Associations of Body Mass Index with Ventilation Management and Clinical Outcomes in Invasively Ventilated Patients with ARDS Related to COVID-19—Insights from the PRoVENT-COVID Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethics
2.3. Study Registration
2.4. Inclusion and Exclusion Criteria
2.5. Collected Data, and Patient Classification
2.6. Endpoints
2.7. Statistical Analysis
3. Results
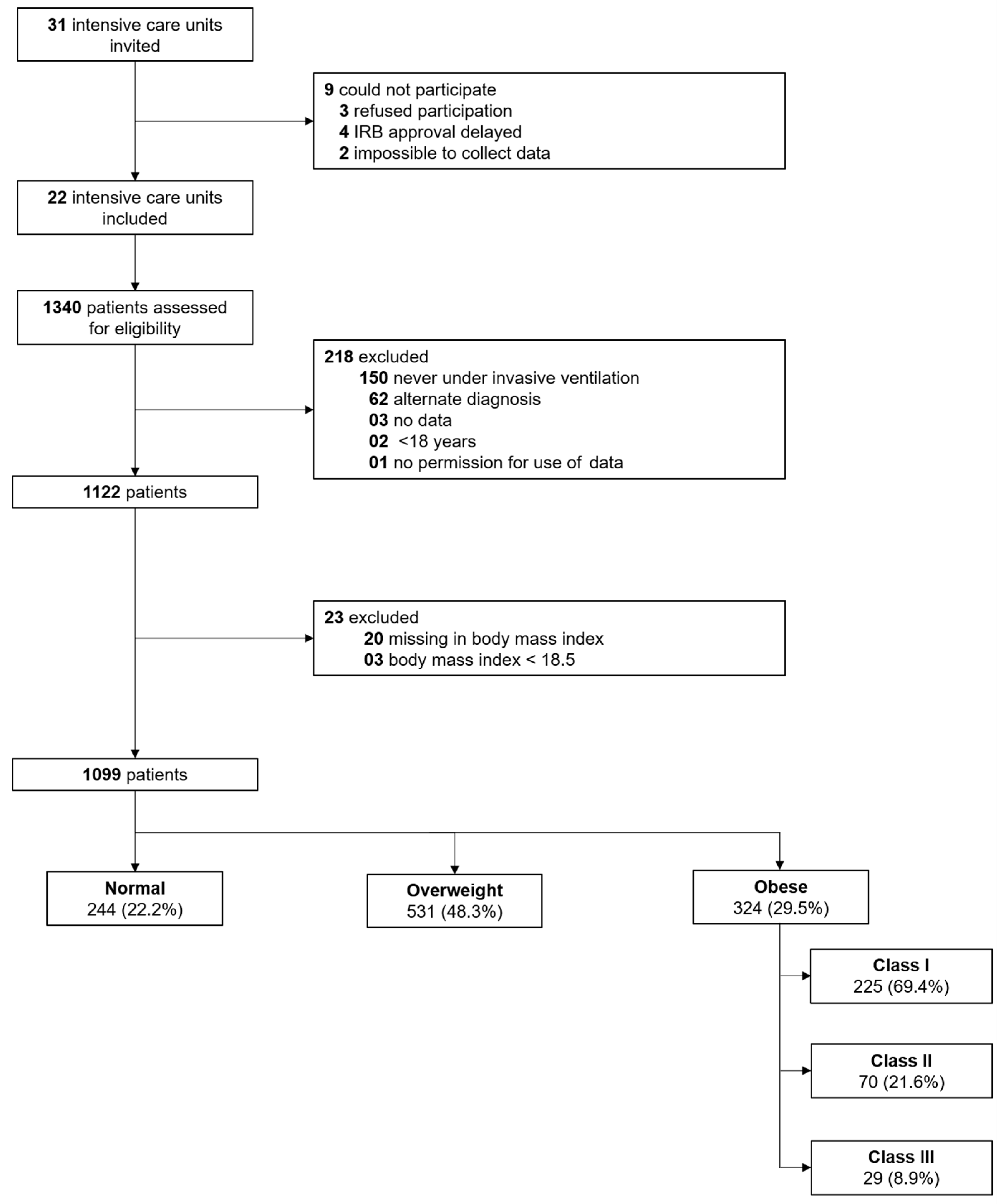
3.1. Participating ICUs and Patients Enrolled
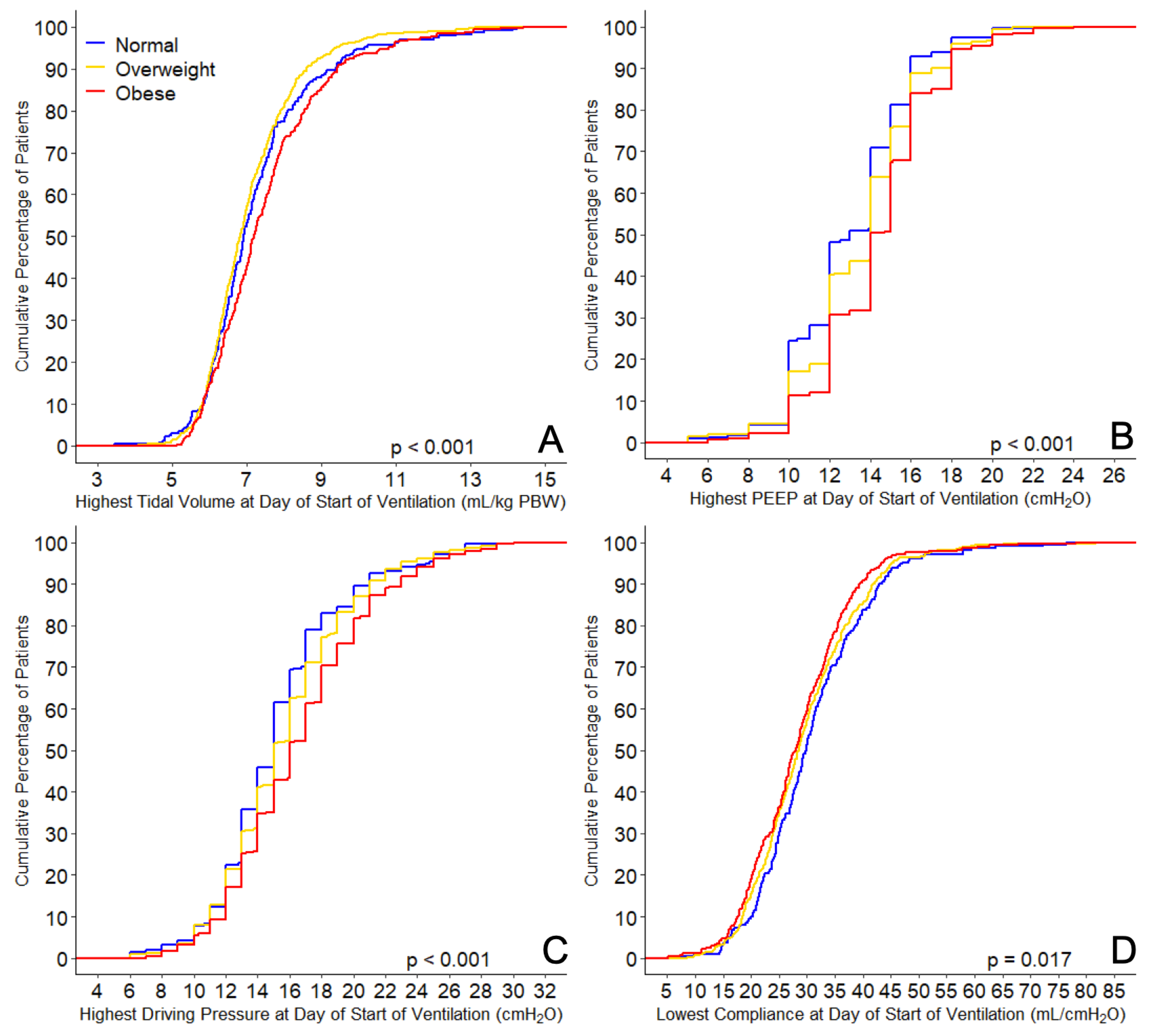
3.2. Ventilatory Support and Adjunctive Therapies
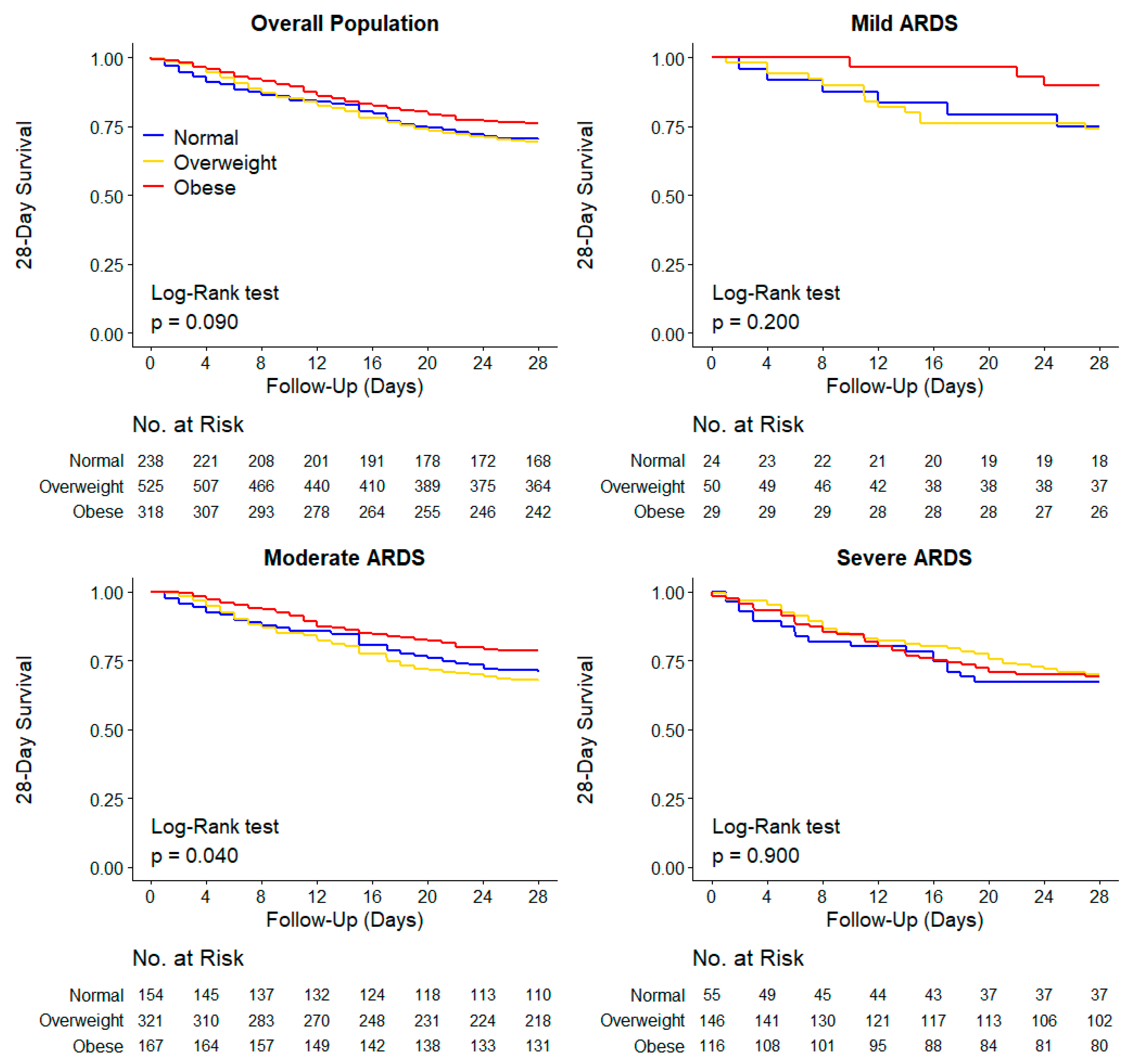
3.3. Patient Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sattar, N.; McInnes, I.B.; McMurray, J.J.V. Obesity Is a Risk Factor for Severe COVID-19 Infection: Multiple Potential Mechanisms. Circulation 2020, 142, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Goodman, K.E.; Magder, L.S.; Baghdadi, J.D.; Pineles, L.; Levine, A.R.; Perencevich, E.N.; Harris, A.D. Impact of Sex and Metabolic Comorbidities on COVID-19 Mortality Risk Across Age Groups: 66,646 Inpatients Across 613 U.S. Hospitals. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef]
- Lighter, J.; Phillips, M.; Hochman, S.; Sterling, S.; Johnson, D.; Francois, F.; Stachel, A. Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission. Clin. Infect. Dis. 2020, 71, 896–897. [Google Scholar] [CrossRef] [PubMed]
- Simonnet, A.; Chetboun, M.; Poissy, J.; Raverdy, V.; Noulette, J.; Duhamel, A.; Labreuche, J.; Mathieu, D.; Pattou, F.; Jourdain, M. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity (Silver Spring) 2020, 28, 1195–1199. [Google Scholar] [CrossRef] [PubMed]
- Brower, R.G.; Matthay, M.A.; Morris, A.; Schoenfeld, D.; Thompson, B.T.; Wheeler, A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 2000, 342, 1301–1308. [Google Scholar] [PubMed]
- Amato, M.B.; Meade, M.O.; Slutsky, A.S.; Brochard, L.; Costa, E.L.; Schoenfeld, D.A.; Stewart, T.E.; Briel, M.; Talmor, D.; Mercat, A.; et al. Driving pressure and survival in the acute respiratory distress syndrome. N. Engl. J. Med. 2015, 372, 747–755. [Google Scholar] [CrossRef]
- Constantin, J.M.; Jabaudon, M.; Lefrant, J.Y.; Jaber, S.; Quenot, J.P.; Langeron, O.; Ferrandière, M.; Grelon, F.; Seguin, P.; Ichai, C.; et al. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): A multicentre, single-blind, randomised controlled trial. Lancet Respir. Med. 2019, 7, 870–880. [Google Scholar] [CrossRef]
- Cavalcanti, A.B.; Suzumura, É.A.; Laranjeira, L.N.; Paisani, D.M.; Damiani, L.P.; Guimarães, H.P.; Romano, E.R.; Regenga, M.M.; Taniguchi, L.N.T.; Teixeira, C.; et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA 2017, 318, 1335–1345. [Google Scholar] [PubMed]
- Guérin, C.; Reignier, J.; Richard, J.C.; Beuret, P.; Gacouin, A.; Boulain, T.; Mercier, E.; Badet, M.; Mercat, A.; Baudin, O.; et al. Prone positioning in severe acute respiratory distress syndrome. N. Engl. J. Med. 2013, 368, 2159–2168. [Google Scholar] [CrossRef]
- Ball, L.; Serpa Neto, A.; Pelosi, P. Obesity and survival in critically ill patients with acute respiratory distress syndrome: A paradox within the paradox. Crit. Care 2017, 21, 114. [Google Scholar] [CrossRef]
- Boers, N.S.; Botta, M.; Tsonas, A.M.; Algera, A.G.; Pillay, J.; Dongelmans, D.A.; Horn, J.; Vlaar, A.P.J.; Hollmann, M.W.; Bos, L.D.J.; et al. PRactice of VENTilation in Patients with Novel Coronavirus Disease (PRoVENT-COVID): Rationale and protocol for a national multicenter observational study in The Netherlands. Ann. Transl. Med. 2020, 8, 1251. [Google Scholar] [CrossRef] [PubMed]
- Botta, M.; Tsonas, A.M.; Pillay, J.; Boers, L.S.; Algera, A.G.; Bos, L.D.J.; Dongelmans, D.A.; Hollmann, M.W.; Horn, J.; Vlaar, A.P.J.; et al. Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): A national, multicentre, observational cohort study. Lancet Respir Med. 2020, 9, 139–148. [Google Scholar] [CrossRef]
- Available online: https://sites.google.com/view/provent-covid/provent-covid (accessed on 11 February 2021).
- Yehya, N.; Harhay, M.O.; Curley, M.A.Q.; Schoenfeld, D.A.; Reeder, R.W. Reappraisal of Ventilator-Free Days in Critical Care Research. Am. J. Respir. Crit. Care Med. 2019, 200, 828–836. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [PubMed]
- O’Brien, J.M., Jr.; Welsh, C.H.; Fish, R.H.; Ancukiewicz, M.; Kramer, A.M. Excess body weight is not independently associated with outcome in mechanically ventilated patients with acute lung injury. Ann. Intern. Med. 2004, 140, 338–345. [Google Scholar] [CrossRef]
- Anzueto, A.; Frutos-Vivar, F.; Esteban, A.; Bensalami, N.; Marks, D.; Raymondos, K.; Apezteguía, C.; Arabi, Y.; Hurtado, J.; González, M.; et al. Influence of body mass index on outcome of the mechanically ventilated patients. Thorax 2011, 66, 66–73. [Google Scholar] [CrossRef]
- Kalra, S.S.; Siuba, M.; Panitchote, A.; Mireles-Cabodevila, E.; Chatburn, R.L.; Krishnan, S.; Duggal, A. Higher Class of Obesity Is Associated With Delivery of Higher Tidal Volumes in Subjects With ARDS. Respir. Care 2020, 65, 1519–1526. [Google Scholar] [CrossRef]
- Kress, J.P.; Pohlman, A.S.; Alverdy, J.; Hall, J.B. The impact of morbid obesity on oxygen cost of breathing (VO(2RESP)) at rest. Am. J. Respir. Crit. Care Med. 1999, 160, 883–886. [Google Scholar] [CrossRef]
- De Jong, A.; Chanques, G.; Jaber, S. Mechanical ventilation in obese ICU patients: From intubation to extubation. Crit. Care 2017, 21, 63. [Google Scholar] [CrossRef]
- De Jong, A.; Verzilli, D.; Jaber, S. ARDS in Obese Patients: Specificities and Management. Crit. Care 2019, 23, 74. [Google Scholar] [CrossRef] [PubMed]
- Guérin, C.; Albert, R.K.; Beitler, J.; Gattinoni, L.; Jaber, S.; Marini, J.J.; Munshi, L.; Papazian, L.; Pesenti, A.; Vieillard-Baron, A.; et al. Prone position in ARDS patients: Why, when, how and for whom. Intensive Care Med. 2020, 46, 2385–2396. [Google Scholar] [CrossRef] [PubMed]
- Malik, P.; Patel, U.; Patel, K.; Martin, M.; Shah, C.; Mehta, D.; Malik, F.A.; Sharma, A. Obesity a predictor of outcomes of COVID-19 hospitalized patients-A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 1188–1193. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Li, Z.; Yang, T.; Wang, M.; Xi, X. Is body mass index associated with outcomes of mechanically ventilated adult patients in intensive critical units? A systematic review and meta-analysis. PLoS ONE 2018, 13, e0198669. [Google Scholar] [CrossRef]
- Ni, Y.N.; Luo, J.; Yu, H.; Wang, Y.W.; Hu, Y.H.; Liu, D.; Liang, B.M.; Liang, Z.A. Can body mass index predict clinical outcomes for patients with acute lung injury/acute respiratory distress syndrome? A meta-analysis. Crit. Care 2017, 21, 36. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Tonetti, T.; Protti, A.; Langer, T.; Girardis, M.; Bellani, G.; Laffey, J.; Carrafiello, G.; Carsana, L.; Rizzuto, C.; et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: A multicentre prospective observational study. Lancet Respir. Med. 2020, 8, 1201–1208. [Google Scholar] [CrossRef]
- Mostaghim, A.; Sinha, P.; Bielick, C.; Knudsen, S.; Beeram, I.; White, L.F.; Apovian, C.; Sagar, M.; Hochberg, N.S. Clinical outcomes and inflammatory marker levels in patients with Covid-19 and obesity at an inner-city safety net hospital. PLoS ONE 2020, 15, e0243888. [Google Scholar] [CrossRef]
- De Jong, A.; Wrigge, H.; Hedenstierna, G.; Gattinoni, L.; Chiumello, D.; Frat, J.P.; Ball, L.; Schetz, M.; Pickkers, P.; Jaber, S. How to ventilate obese patients in the ICU. Intensive Care Med. 2020, 46, 2423–2435. [Google Scholar] [CrossRef] [PubMed]
| Normal (n = 244) | Overweight (n = 531) | Obese (n = 324) | p Value | |
|---|---|---|---|---|
| Age, years | 67.0 (60.0–73.0) | 66.0 (59.0–73.0) | 61.0 (53.0–70.0) | <0.001 |
| Male gender—no (%) | 186 (76.2) | 407 (76.6) | 209 (64.5) | <0.001 |
| Body mass index, kg/m2 | 23.9 (22.9–24.6) | 27.3 (26.2–28.5) | 32.9 (31.2–35.9) | <0.001 |
| Transferred under invasive ventilation | 51 (20.9) | 82 (15.4) | 59 (18.2) | 0.160 |
| Days between intubation and admission | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.583 |
| Use of non-invasive ventilation—no (%) | 15 (6.8) | 45 (9.4) | 24 (8.1) | 0.517 |
| Duration of non-invasive ventilation, hours | 5.5 (2.0–48.0) | 8.0 (2.0–15.1) | 7.5 (2.0–14.8) | 0.803 |
| Chest CT scan performed—no (%) | 83/232 (35.8) | 169/509 (33.2) | 103/314 (32.8) | 0.738 |
| Lung parenchyma affected—no (%) | 0.839 | |||
| 0% | 3/84 (3.6) | 6/172 (3.5) | 5/103 (4.9) | |
| 25% | 32/84 (38.1) | 51/172 (29.7) | 33/103 (32.0) | |
| 50% | 26/84 (31.0) | 52/172 (30.2) | 28/103 (27.2) | |
| 75% | 20/84 (23.8) | 53/172 (30.8) | 29/103 (28.2) | |
| 100% | 3/84 (3.6) | 10/172 (5.8) | 8/103 (7.8) | |
| Chest X-ray performed—no (%) | 127/149 (85.2) | 289/334 (86.5) | 175/204 (85.8) | 0.907 |
| Quadrants affected—no (%) | 0.068 | |||
| 1 | 14/126 (11.1) | 21/291 (7.2) | 7/173 (4.0) | |
| 2 | 24/126 (19.0) | 67/291 (23.0) | 48/173 (27.7) | |
| 3 | 37/126 (29.4) | 72/291 (24.7) | 55/173 (31.8) | |
| 4 | 51/126 (40.5) | 131/291 (45.0) | 63/173 (36.4) | |
| Severity of ARDS—no (%) | 0.028 | |||
| Mild | 24/239 (10.0) | 51/523 (9.7) | 29/318 (9.1) | |
| Moderate | 157/239 (65.7) | 326/523 (62.3) | 171/318 (53.8) | |
| Severe | 58/239 (24.3) | 146/523 (27.9) | 118/318 (37.1) | |
| Co-existing disorders—no (%) | ||||
| Hypertension | 74 (30.3) | 186 (35.0) | 114 (35.2) | 0.383 |
| Heart failure | 9 (3.7) | 31 (5.8) | 8 (2.5) | 0.058 |
| Diabetes | 41 (16.8) | 115 (21.7) | 90 (27.8) | 0.007 |
| Chronic kidney disease | 8 (3.3) | 31 (5.8) | 8 (2.5) | 0.045 |
| Baseline creatinine, µmol/L * | 77.0 (61.0–98.0) | 78.0 (64.0–97.0) | 76.0 (62.8–97.0) | 0.767 |
| Liver cirrhosis | 0 (0.0) | 2 (0.4) | 1 (0.3) | 0.999 |
| Chronic obstructive pulmonary disease | 20 (8.2) | 41 (7.7) | 24 (7.4) | 0.934 |
| Active hematological neoplasia | 5 (2.0) | 10 (1.9) | 1 (0.3) | 0.091 |
| Active solid neoplasia | 6 (2.5) | 14 (2.6) | 7 (2.2) | 0.967 |
| Neuromuscular disease | 2 (0.8) | 3 (0.6) | 3 (0.9) | 0.728 |
| Immunosuppression | 9 (3.7) | 8 (1.5) | 7 (2.2) | 0.165 |
| Previous medication—no (%) | ||||
| Systemic steroids | 10 (4.1) | 17 (3.2) | 11 (3.4) | 0.786 |
| Inhalation steroids | 21 (8.6) | 58 (10.9) | 45 (13.9) | 0.137 |
| Angiotensin converting enzyme inhibitor | 33 (13.5) | 93 (17.5) | 60 (18.5) | 0.250 |
| Angiotensin II receptor blocker | 24 (9.8) | 57 (10.7) | 44 (13.6) | 0.318 |
| Beta-blockers | 40 (16.4) | 98 (18.5) | 71 (21.9) | 0.235 |
| Insulin | 14 (5.7) | 38 (7.2) | 26 (8.0) | 0.590 |
| Metformin | 29 (11.9) | 77 (14.5) | 65 (20.1) | 0.021 |
| Statins | 70 (28.7) | 155 (29.2) | 100 (30.9) | 0.826 |
| Calcium channel blockers | 47 (19.3) | 79 (14.9) | 67 (20.7) | 0.067 |
| Vital signs at the day of start of ventilation | ||||
| Heart rate, bpm ** | 84.0 (71.5–97.0) | 84.0 (73.0–97.1) | 86.0 (76.9–98.0) | 0.130 |
| Mean arterial pressure, mmHg ** | 78.7 (73.0–86.0) | 80.0 (73.5–87.5) | 82.0 (75.7–89.5) | 0.002 |
| Laboratory tests at the day of start of ventilation | ||||
| pH ** | 7.36 (7.30–7.41) | 7.37 (7.32–7.41) | 7.36 (7.31–7.41) | 0.700 |
| Worst PaO2/FiO2, mmHg *** | 130.0 (101.0–166.9) | 125.0 (98.5–162.4) | 114.6 (87.6–146.0) | 0.001 |
| PaCO2, mmHg ** | 44.5 (39.5–51.3) | 44.3 (38.8–49.6) | 44.6 (39.8–51.0) | 0.356 |
| Lactate mmol/L ** | 1.2 (0.9–1.5) | 1.2 (1.0–1.4) | 1.1 (0.9–1.4) | 0.132 |
| Organ support at the day of start of ventilation—no (%) | ||||
| Continuous sedation | 231/243 (95.1) | 506/530 (95.5) | 316 (97.5) | 0.213 |
| Inotropic or vasopressor | 192/243 (79.0) | 412/530 (77.7) | 241 (74.4) | 0.377 |
| Vasopressor | 192/243 (79.0) | 412/530 (77.7) | 240 (74.1) | 0.328 |
| Inotropic | 18/243 (7.4) | 17/530 (3.2) | 10 (3.1) | 0.022 |
| Fluid balance, mL | 696.7 (29.0–1441.0) | 515.8 (7.3–1239.3) | 449.0 (-15.0–1299.9) | 0.171 |
| Urine output, mL | 692.5 (333.8–1116.2) | 647.5 (350.0–1145.0) | 705.0 (395.0–1115.0) | 0.500 |
| Ventilation support at the day of start of ventilation | ||||
| Assisted ventilation—no (%) | 73/243 (30.0) | 161/527 (30.6) | 84 (25.9) | 0.328 |
| Tidal volume, mL/kg PBW ** | 6.4 (5.9–6.9) | 6.4 (5.9–7.0) | 6.6 (5.9–7.5) | < 0.001 |
| PEEP, cmH2O ** | 12.0 (10.0–14.0) | 12.7 (11.0–14.5) | 14.0 (12.0–15.0) | < 0.001 |
| Peak pressure, cmH2O ** | 25.2 (22.8–28.9) | 26.6 (23.5–29.3) | 28.0 (25.3–31.0) | < 0.001 |
| Driving pressure, cmH2O ** | 13.0 (11.2–15.3) | 13.7 (12.0–16.0) | 14.5 (12.5–17.0) | < 0.001 |
| Mechanical power, J/min ** | 18.1 (14.7–21.6) | 18.2 (15.3–21.9) | 19.4 (15.8–23.5) | 0.014 |
| Compliance, mL/cmH2O ** | 36.2 (28.7–45.1) | 33.4 (26.8–41.1) | 31.9 (26.0–38.1) | < 0.001 |
| Total respiratory rate, mpm ** | 21.7 (19.3–24.0) | 21.7 (19.8–24.0) | 22.0 (19.2–24.0) | 0.921 |
| Minute ventilation, L/min | 9.8 (8.5–11.4) | 9.6 (8.4–11.2) | 9.7 (8.3–11.2) | 0.556 |
| Minute ventilation corrected, mL/kg/min PBW | 137.2 (122.3–157.5) | 138.3 (122.4–157.3) | 141.3 (125.7–164.1) | 0.053 |
| FiO2 ** | 0.54 (0.45–0.65) | 0.57 (0.47–0.66) | 0.60 (0.52–0.71) | <0.001 |
| etCO2, mmHg ** | 35.7 (32.0–40.7) | 36.5 (32.4–41.6) | 38.4 (34.6–43.8) | <0.001 |
| Rescue therapy at the day of start of ventilation—no (%) | ||||
| Prone positioning | 61/241 (25.3) | 161/522 (30.8) | 104/317 (32.8) | 0.142 |
| Duration, hours | 9.0 (6.0–14.0) | 8.0 (4.0–13.5) | 8.0 (3.1–13.0) | 0.138 |
| Recruitment maneuver | 3/197 (1.5) | 12/434 (2.8) | 5/268 (1.9) | 0.641 |
| ECMO | 1/241 (0.4) | 0/523 (0.0) | 3/318 (0.9) | 0.066 |
| Use of NMBA | 54/243 (22.2) | 154/529 (29.1) | 89 (27.5) | 0.128 |
| Duration, hours | 0.0 (0.0–0.0) | 0.0 (0.0–8.0) | 0.0 (0.0–8.0) | 0.182 |
| Normal (n = 244) | Overweight (n = 531) | Obese (n = 324) | p Value | |
|---|---|---|---|---|
| 28-day mortality—no. (%) | 71/238 (29.8) | 162/525 (30.9) | 76/318 (23.9) | 0.082 |
| Ventilator-free days at day 28, days | 2.0 (0.0–18.0) | 0.0 (0.0–15.0) | 6.0 (0.0–17.0) | 0.088 |
| Duration of ventilation, days | 13.0 (7.0–23.0) | 15.0 (8.0–24.0) | 14.0 (9.0–22.8) | 0.206 |
| In survivors at day 28, days | 14.0 (8.0–27.0) | 16.0 (10.0–30.0) | 16.0 (10.0–26.0) | 0.192 |
| Tracheostomy—no (%) | 47/241 (19.5) | 86/527 (16.3) | 53/322 (16.5) | 0.517 |
| Thromboembolic complications—no (%) | 80 (32.8) | 146 (27.5) | 88 (27.2) | 0.258 |
| Pulmonary embolism | 64 (26.2) | 112 (21.1) | 70 (21.6) | 0.263 |
| Deep vein thrombosis | 12 (4.9) | 29 (5.5) | 14 (4.3) | 0.776 |
| Ischemic stroke | 9 (3.7) | 15 (2.8) | 6 (1.9) | 0.401 |
| Myocardial infarction | 5 (2.0) | 9 (1.7) | 2 (0.6) | 0.261 |
| Systemic arterial embolism | 2 (0.8) | 1 (0.2) | 1 (0.3) | 0.349 |
| Acute kidney injury—no (%) | 104 (42.6) | 235/529 (44.4) | 149/322 (46.3) | 0.689 |
| Need for RRT—no (%) | 40 (16.4) | 103 (19.4) | 58 (17.9) | 0.610 |
| Need of rescue therapy—no (%) * | 168/241 (69.7) | 393/526 (74.7) | 245/321 (76.3) | 0.191 |
| Prone positioning | 124/241 (51.5) | 300/527 (56.9) | 188/322 (58.4) | 0.232 |
| Recruitment maneuver | 9/200 (4.5) | 36/440 (8.2) | 18/271 (6.6) | 0.239 |
| Use of NMBA | 95 (38.9) | 266 (50.1) | 166 (51.2) | 0.006 |
| ECMO | 1/241 (0.4) | 6/525 (1.1) | 5/318 (1.6) | 0.415 |
| ICU length of stay, days | 14.0 (8.0–26.0) | 16.0 (9.0–26.0) | 15.0 (10.0–26.0) | 0.302 |
| In survivors, days | 15.5 (9.3–29.0) | 18.0 (11.0–31.0) | 17.0 (11.0–28.0) | 0.379 |
| Hospital length of stay, days | 23.0 (13.0–37.3) | 23.0 (13.0–36.0) | 25.0 (16.8–37.0) | 0.219 |
| In survivors, days | 29.0 (18.0–44.5) | 30.0 (20.0–45.8) | 29.0 (21.0–42.0) | 0.682 |
| ICU mortality—no (%) | 76/238 (31.9) | 186/519 (35.8) | 85/313 (27.2) | 0.034 |
| Hospital mortality—no (%) | 80/224 (35.7) | 191/490 (39.0) | 87/290 (30.0) | 0.041 |
| 90-day mortality—no (%) | 82/219 (37.4) | 201/492 (40.9) | 91/285 (31.9) | 0.046 |
| Effect Estimate (95% CI) | p Value | |
|---|---|---|
| 28-day mortality | ||
| Body mass index category | ||
| Normal | 1 (Reference) | |
| Overweight | 1.10 (0.83 to 1.47) | 0.500 |
| Obese | 0.89 (0.63 to 1.25) | 0.510 |
| ICU mortality | ||
| Body mass index category | ||
| Normal | 1 (Reference) | |
| Overweight | OR, 1.39 (0.96 to 2.00) | 0.079 |
| Obese | OR, 1.07 (0.69 to 1.65) | 0.753 |
| Hospital mortality | ||
| Body mass index category | ||
| Normal | 1 (Reference) | |
| Overweight | OR, 1.38 (0.95 to 2.00) | 0.090 |
| Obese | OR, 1.05 (0.68 to 1.64) | 0.817 |
| 90-day mortality | ||
| Body mass index category | ||
| Normal | 1 (Reference) | |
| Overweight | HR, 1.16 (0.89 to 1.52) | 0.270 |
| Obese | HR, 1.00 (0.72 to 1.38) | 0.999 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schavemaker, R.; Schultz, M.J.; Lagrand, W.K.; van Slobbe-Bijlsma, E.R.; Serpa Neto, A.; Paulus, F.; for the PRoVENT–COVID; Collaborative Group. Associations of Body Mass Index with Ventilation Management and Clinical Outcomes in Invasively Ventilated Patients with ARDS Related to COVID-19—Insights from the PRoVENT-COVID Study. J. Clin. Med. 2021, 10, 1176. https://doi.org/10.3390/jcm10061176
Schavemaker R, Schultz MJ, Lagrand WK, van Slobbe-Bijlsma ER, Serpa Neto A, Paulus F, for the PRoVENT–COVID, Collaborative Group. Associations of Body Mass Index with Ventilation Management and Clinical Outcomes in Invasively Ventilated Patients with ARDS Related to COVID-19—Insights from the PRoVENT-COVID Study. Journal of Clinical Medicine. 2021; 10(6):1176. https://doi.org/10.3390/jcm10061176
Chicago/Turabian StyleSchavemaker, Renée, Marcus J. Schultz, Wim K. Lagrand, Eline R. van Slobbe-Bijlsma, Ary Serpa Neto, Frederique Paulus, for the PRoVENT–COVID, and Collaborative Group. 2021. "Associations of Body Mass Index with Ventilation Management and Clinical Outcomes in Invasively Ventilated Patients with ARDS Related to COVID-19—Insights from the PRoVENT-COVID Study" Journal of Clinical Medicine 10, no. 6: 1176. https://doi.org/10.3390/jcm10061176
APA StyleSchavemaker, R., Schultz, M. J., Lagrand, W. K., van Slobbe-Bijlsma, E. R., Serpa Neto, A., Paulus, F., for the PRoVENT–COVID, & Collaborative Group. (2021). Associations of Body Mass Index with Ventilation Management and Clinical Outcomes in Invasively Ventilated Patients with ARDS Related to COVID-19—Insights from the PRoVENT-COVID Study. Journal of Clinical Medicine, 10(6), 1176. https://doi.org/10.3390/jcm10061176







