The Effect of Exoskeletal-Assisted Walking on Spinal Cord Injury Bowel Function: Results from a Randomized Trial and Comparison to Other Physical Interventions
Abstract
1. Introduction
2. Experimental Section
2.1. Recruitment
2.2. Protocol
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
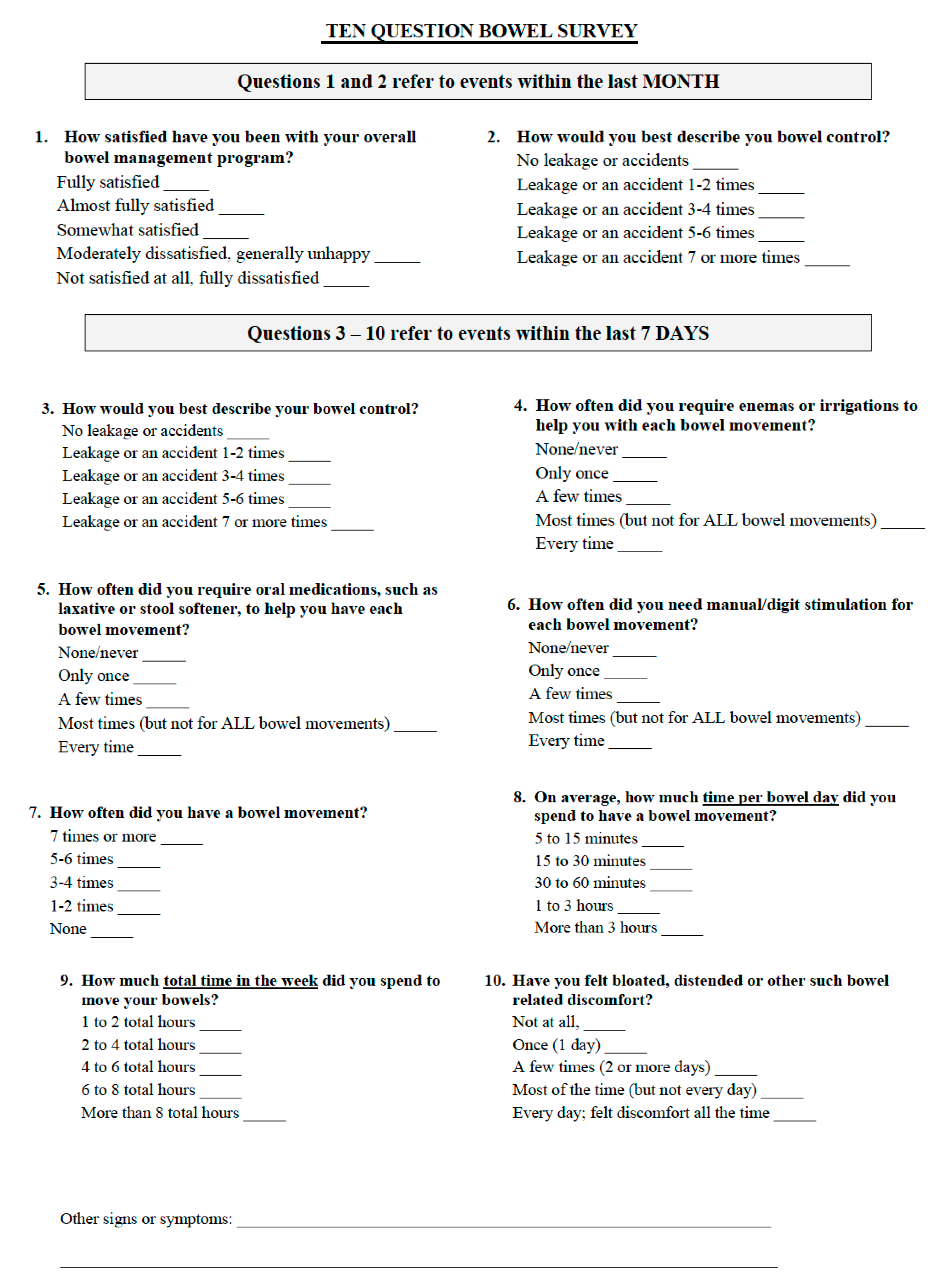
Appendix A
References
- Korsten, M.A.; Fajardo, N.R.; Rosman, A.S.; Creasey, G.H.; Spungen, A.M.; Bauman, W.A. Difficulty with evacuation after spinal cord injury: Colonic motility during sleep and effects of abdominal wall stimulation. J. Rehabil. Res. Dev. 2004, 41, 95–100. [Google Scholar] [CrossRef]
- Adriaansen, J.J.; Van Asbeck, F.W.; Van Kuppevelt, D.; Snoek, G.J.; Post, M.W. Outcomes of Neurogenic Bowel Management in Individuals Living With a Spinal Cord Injury for at Least 10 Years. Arch. Phys. Med. Rehabil. 2015, 96, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Faaborg, P.M.; Christensen, P.; Finnerup, N.; Laurberg, S.; Krogh, K. The pattern of colorectal dysfunction changes with time since spinal cord injury. Spinal Cord 2007, 46, 234–238. [Google Scholar] [CrossRef]
- Rasmussen, M.M.; Krogh, K.; Clemmensen, D.; Bluhme, H.; Rawashdeh, Y.; Christensen, P. Colorectal transport during defecation in participants with supraconal spinal cord injury. Spinal Cord 2013, 51, 683–687. [Google Scholar] [CrossRef][Green Version]
- Hanson, R.W.; Franklin, M.R. Sexual loss in relation to other functional losses for spinal cord injured males. Arch. Phys. Med. Rehabil. 1976, 57, 291–293. [Google Scholar]
- Steins, S.A.; Bergman, S.B.; Goetz, L.L. Neurogenic bowel dysfunction after spinal cord injury: Clinical evaluation and rehabiliative management. Arch. Phys. Med. Rehabil. 1997, 78, S86–S100. [Google Scholar] [CrossRef]
- Eng, J.J.; Levins, S.M.; Townson, A.F.; Mah-Jones, D.; Bremner, J.; Huston, G. Use of Prolonged Standing for Individuals With Spinal Cord Injuries. Phys. Ther. 2001, 81, 1392–1399. [Google Scholar] [CrossRef]
- Kwok, S.; Harvey, L.A.; Glinsky, J.V.; Bowden, J.L.; Coggrave, M.; Tussler, D. Does regular standing improve bowel function in people with spinal cord injury? A randomised crossover trial. Spinal Cord 2015, 53, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Krogh, K.; Christensen, P.; Sabroe, S.; Laurberg, S. Neurogenic bowel dysfunction score. Spinal Cord 2005, 44, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Agachan, F.; Chen, T.; Pfeifer, J.; Reissman, P.; Wexner, S.D. A constipation scoring system to simplify evaluation and management of constipated patients. Dis. Colon Rectum 1996, 39, 681–685. [Google Scholar] [CrossRef] [PubMed]
- Vaizey, C.J.; Carapeti, E.; Cahill, J.A.; Kamm, M.A. Prospective comparison of faecal incontinence grading systems. Gut 1999, 44, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Bi, L.; Triadafilopoulos, G. Exercise and gastrointestinal function and disease: An evidence-based review of risks and benefits. Clin. Gastroenterol. Hepatol. 2003, 1, 345–355. [Google Scholar] [CrossRef]
- Moses, F.M. The Effect of Exercise on the Gastrointestinal Tract1. Sports Med. 1990, 9, 159–172. [Google Scholar] [CrossRef] [PubMed]
- De Schryver, A.M.; Keulemans, Y.C.; Peters, H.P.; Akkermans, L.M.; Smout, A.J.; De Vries, W.R.; Van Berge-Henegouen, G.P. Effects of regular physical activity on defecation pattern in middle-aged patients complaining of chronic constipation. Scand. J. Gastroenterol. 2005, 40, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Oettle, G.J. Effect of moderate exercise on bowel habit. Gut 1991, 32, 941–944. [Google Scholar] [CrossRef] [PubMed]
- Morrison, S.A.; Lorenz, D.; Eskay, C.P.; Forrest, G.F.; Basso, D.M. Longitudinal Recovery and Reduced Costs After 120 Sessions of Locomotor Training for Motor Incomplete Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2018, 99, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Hubscher, C.H.; Herrity, A.N.; Williams, C.S.; Montgomery, L.R.; Willhite, A.M.; Angeli, C.A.; Harkema, S.J. Improvements in bladder, bowel and sexual outcomes following task-specific locomotor training in human spinal cord injury. PLoS ONE 2018, 13, e0190998. [Google Scholar] [CrossRef]
- Chun, A.; Asselin, P.K.; Knezevic, S.; Kornfeld, S.; Bauman, W.A.; Korsten, M.A.; Harel, N.Y.; Huang, V.; Spungen, A.M. Changes in bowel function following exoskeletal-assisted walking in persons with spinal cord injury: An observational pilot study. Spinal Cord 2020, 58, 459–466. [Google Scholar] [CrossRef]
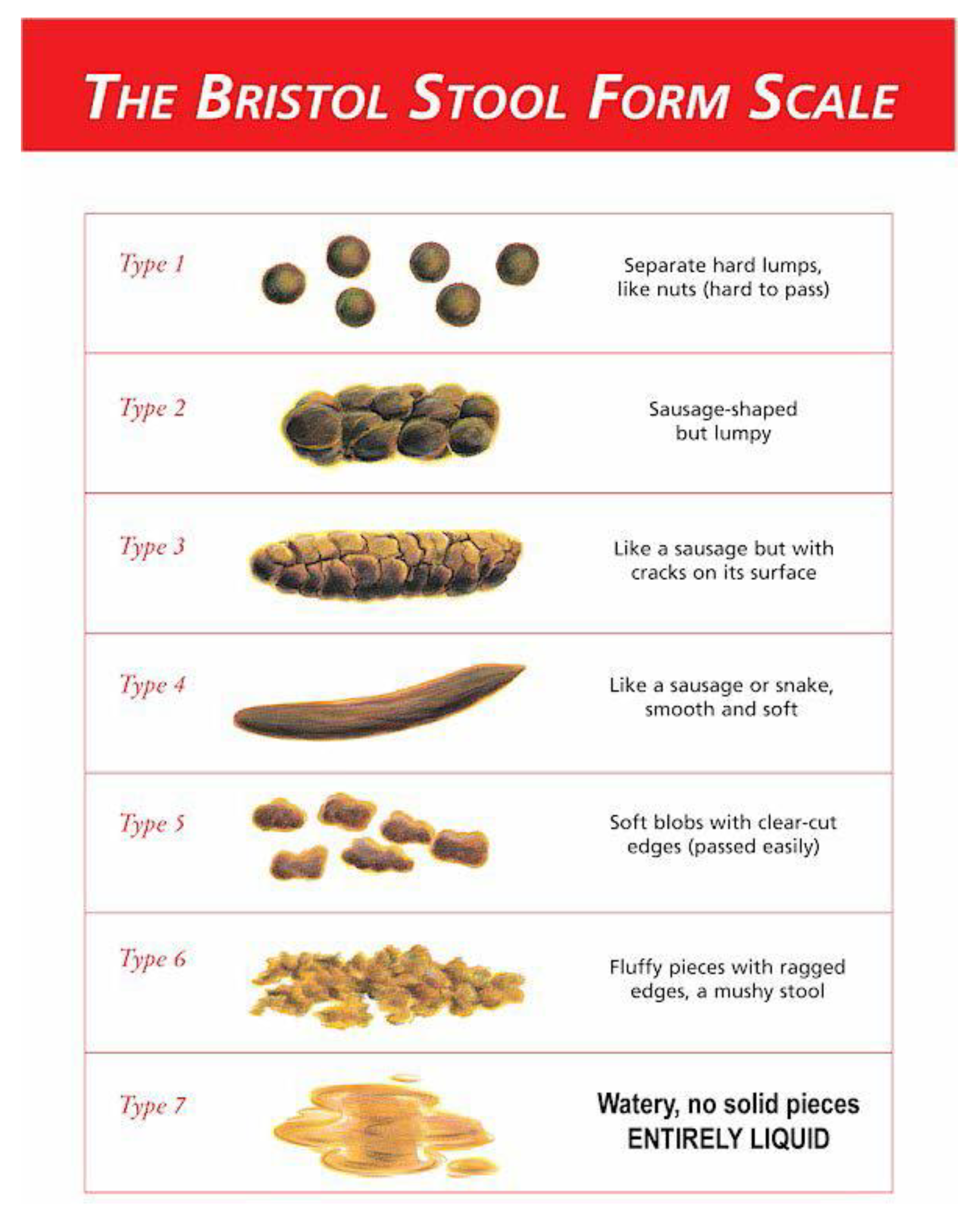
- Perez, M.M.; Martinez, A.B. The Bristol scale—A useful system to assess stool form? Rev. Esp. Enferm. Dig. 2009, 101, 305–311. [Google Scholar]
- Fineberg, D.B.; Asselin, P.; Harel, N.Y.; Agranova-Breyter, I.; Kornfeld, S.D.; Bauman, W.A.; Spungen, A.M. Vertical ground reaction force-based analysis of powered exoskeleton-assisted walking in persons with motor-complete paraplegia. J. Spinal Cord Med. 2013, 36, 313–321. [Google Scholar] [CrossRef]
- Hong, E.; Gorman, P.H.; Forrest, G.F.; Asselin, P.K.; Knezevic, S.; Scott, W.; Wojciehowski, S.B.; Kornfeld, S.; Spungen, A.M. Mobility Skills With Exoskeletal-Assisted Walking in Persons With SCI: Results From a Three Center Randomized Clinical Trial. Front. Robot. AI 2020, 7. [Google Scholar] [CrossRef]
- Esquenazi, A.; Talaty, M.; Packel, A.; Saulino, M. The ReWalk Powered Exoskeleton to Restore Ambulatory Function to Individuals with Thoracic-Level Motor-Complete Spinal Cord Injury. Am. J. Phys. Med. Rehabil. 2012, 91, 911–921. [Google Scholar] [CrossRef]
- Zeilig, G.; Weingarden, H.; Zwecker, M.; Dudkiewicz, I.; Bloch, A.; Esquenazi, A. Safety and tolerance of the ReWalk exoskeleton suit for ambulation by people with complete spinal cord injury: A pilot study. J. Spinal Cord Med. 2012, 35, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Palermo, A.E.; Maher, J.L.; Baunsgaard, C.B.; Nash, M.S. Clinician-Focused Overview of Bionic Exoskeleton Use After Spinal Cord Injury. Top. Spinal Cord Inj. Rehabil. 2017, 23, 234–244. [Google Scholar] [CrossRef] [PubMed]
- Lynch, A.C.; Wong, C.; Anthony, A.; Dobbs, B.R.; Frizelle, F.A. Bowel dysfunction following spinal cord injury: A description of bowel function in a spinal cord-injured population and comparison with age and gender matched controls. Spinal Cord 2000, 38, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Blake, M.R.; Raker, J.M.; Whelan, K. Validity and reliability of the Bristol Stool Form Scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment. Pharmacol. Ther. 2016, 44, 693–703. [Google Scholar] [CrossRef]
- Tulsky, D.S.; Kisala, P.A.; Victorson, D.; Tate, D.; Heinemann, A.W.; Amtmann, D.; Cella, D. Developing a Contemporary Patient-Reported Outcomes Measure for Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2011, 92 (Suppl. 10), S44–S51. [Google Scholar] [CrossRef]
- Tulsky, D.S.; Kisala, P.A. The Spinal Cord Injury—Quality of Life (SCI-QOL) measurement system: Development, psychometrics, and item bank calibration. J. Spinal Cord Med. 2015, 38, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Tulsky, D.S.; Kisala, P.A.; Tate, D.G.; Spungen, A.M.; Kirshblum, S.C. Development and psychometric characteristics of the SCI-QOL Bladder Management Difficulties and Bowel Management Difficulties item banks and short forms and the SCI-QOL Bladder Complications scale. J. Spinal Cord Med. 2015, 38, 288–302. [Google Scholar] [CrossRef]

| Category | Frequency Reported | Pre-EAW | Post-EAW | Percent of Participants Improved |
|---|---|---|---|---|
| Enema, oral medication and/or manual digital stimulation needed for each bowel evacuation in the past week | Never to a few times | 57% | 63% | 12% |
| Most to every time | 41% | 35% | ||
| Average bowel evacuation time needed per bowel day during the past week | 5 to 60 min | 80% | 92% | 24% |
| >1 to 3 h | 18% | 6% | ||
| Average bowel evacuation time needed in the past week | 1 to 6 h | 80% | 92% | 24% |
| >6 to 8 h | 16% | 6% |
| Category | Exoskeletal-Assisted Walking (EAW) Phase (n = 50) | Usual Activity (UA) Phase (n = 49) | EAW vs. UA Diff (p Value) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Paired T-Test (p) | Pre–Post Diff | Pre | Post | Paired T-Test (p) | Pre–Post Diff | ||
| All (n = 49) (± SD) | 49.7 (8.7) | 48.4 (9.2) | 0.207 | −1.3 (7.1) | 50.8 (8.6) | 49.3 (9.2) | 0.071 | −1.5 (5.8) | 0.88 |
| (range) | 36.1–79.4 | 36.1–74.4 | 36.1–75.0 | 36.1–79.4 | |||||
| EAW first (n = 24) | 49.9 (8.4) | 50.4 (8.3) | 0.292 | 0.5 (7.4) | 50.4 (8.3) | 49.1 (9.5) | 0.292 | −1.3 (5.8) | 0.46 |
| UA first (n = 25) | 49.5 (9.0) | 46.5 (9.8) | 0.028 | −3.0 (6.5) | 51.2 (8.9) | 49.5 (9.1) | 0.145 | −1.8 (5.8) | 0.54 |
| DOI > 2.0 y (n = 26) | 51.0 (9.5) | 48.8 (10.2) | 0.144 | −2.2 (7.3) | 52.0 (9.4) | 50.9 (9.6) | 0.299 | −1.1 (5.4) | 0.60 |
| DOI ≤ 2.0 y (n = 23) | 47.9. (7.6) | 47.5 (8.3) | 0.823 | −0.4 (6.9) | 49.1 (7.5) | 47.0 (8.5) | 0.143 | −2.0 (6.2) | 0.51 |
| Male (n = 38) | 50.1 (9.1) | 47.6(9.8) | 0.041 | −2.5 (7.1) | 50.8 (9.0) | 49.5 (9.3) | 0.109 | −1.3 (5.0) | 0.49 |
| Female (n = 11) | 48.5 (6.5) | 51.2 (5.3) | 0.108 | 2.8 (4.9) | 50.8 (6.3) | 48.6 (8.3) | 0.398 | −2.1 (7.7) | 0.23 |
| Complete (n = 31) | 51.6 (9.3) | 49.9 (9.6) | 0.243 | −1.7 (7.8) | 52.1 (9.1) | 51.4 (9.7) | 0.489 | −0.7 (5.7) | 0.65 |
| Incomplete (n = 18) | 46.5 (6.6) | 45.9 (8.1) | 0.642 | −0.6 (5.8) | 48.6 (7.4) | 45.7 (7.0) | 0.047 | −2.9 (5.8) | 0.32 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gorman, P.H.; Forrest, G.F.; Asselin, P.K.; Scott, W.; Kornfeld, S.; Hong, E.; Spungen, A.M. The Effect of Exoskeletal-Assisted Walking on Spinal Cord Injury Bowel Function: Results from a Randomized Trial and Comparison to Other Physical Interventions. J. Clin. Med. 2021, 10, 964. https://doi.org/10.3390/jcm10050964
Gorman PH, Forrest GF, Asselin PK, Scott W, Kornfeld S, Hong E, Spungen AM. The Effect of Exoskeletal-Assisted Walking on Spinal Cord Injury Bowel Function: Results from a Randomized Trial and Comparison to Other Physical Interventions. Journal of Clinical Medicine. 2021; 10(5):964. https://doi.org/10.3390/jcm10050964
Chicago/Turabian StyleGorman, Peter H., Gail F. Forrest, Pierre K. Asselin, William Scott, Stephen Kornfeld, Eunkyoung Hong, and Ann M. Spungen. 2021. "The Effect of Exoskeletal-Assisted Walking on Spinal Cord Injury Bowel Function: Results from a Randomized Trial and Comparison to Other Physical Interventions" Journal of Clinical Medicine 10, no. 5: 964. https://doi.org/10.3390/jcm10050964
APA StyleGorman, P. H., Forrest, G. F., Asselin, P. K., Scott, W., Kornfeld, S., Hong, E., & Spungen, A. M. (2021). The Effect of Exoskeletal-Assisted Walking on Spinal Cord Injury Bowel Function: Results from a Randomized Trial and Comparison to Other Physical Interventions. Journal of Clinical Medicine, 10(5), 964. https://doi.org/10.3390/jcm10050964





