Quality of Recovery after Laparoscopic Cholecystectomy Following Neuromuscular Blockade Reversal with Neostigmine or Sugammadex: A Prospective, Randomized, Controlled Trial
Abstract
1. Introduction
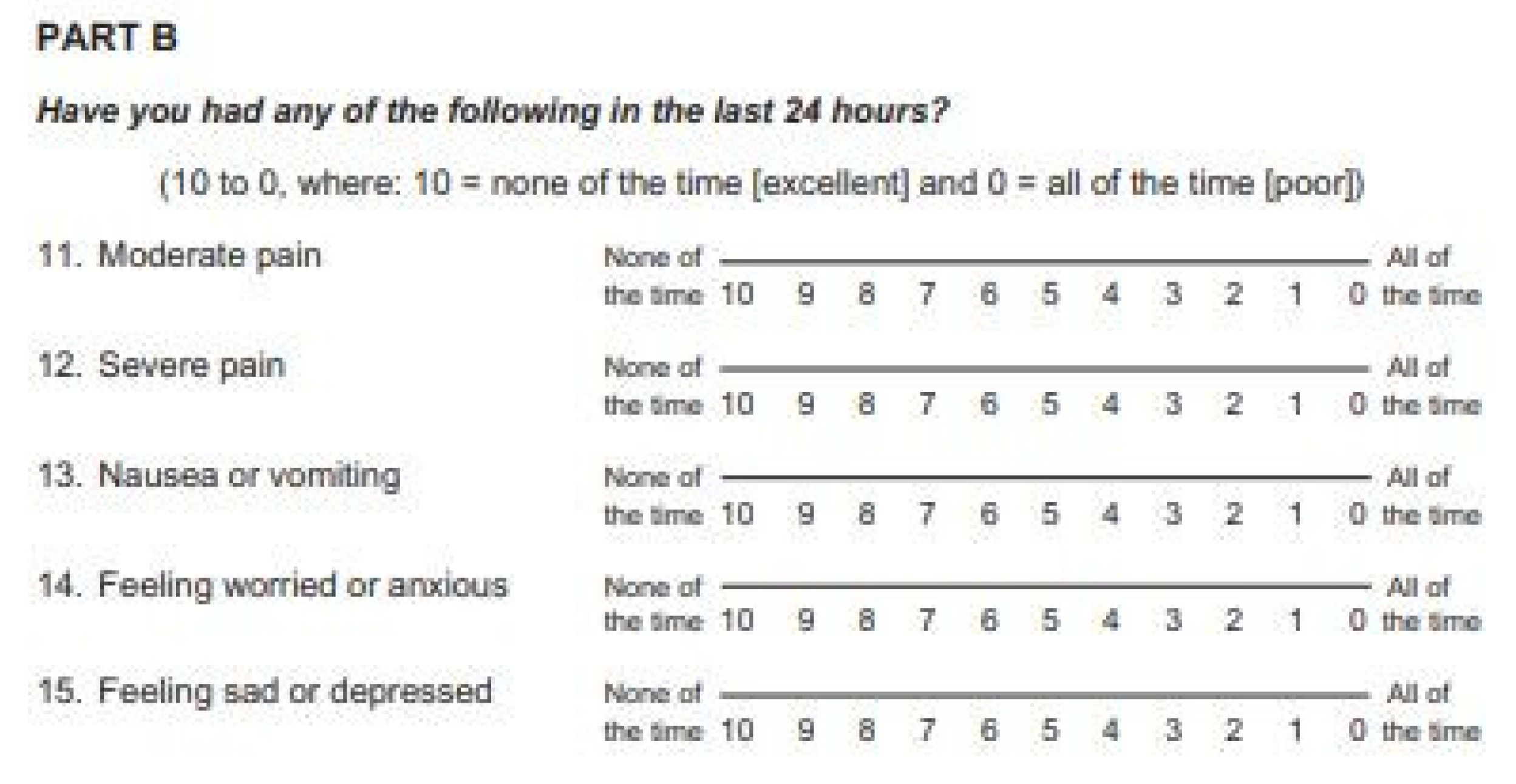
2. Materials and Methods
Statistical Analyses
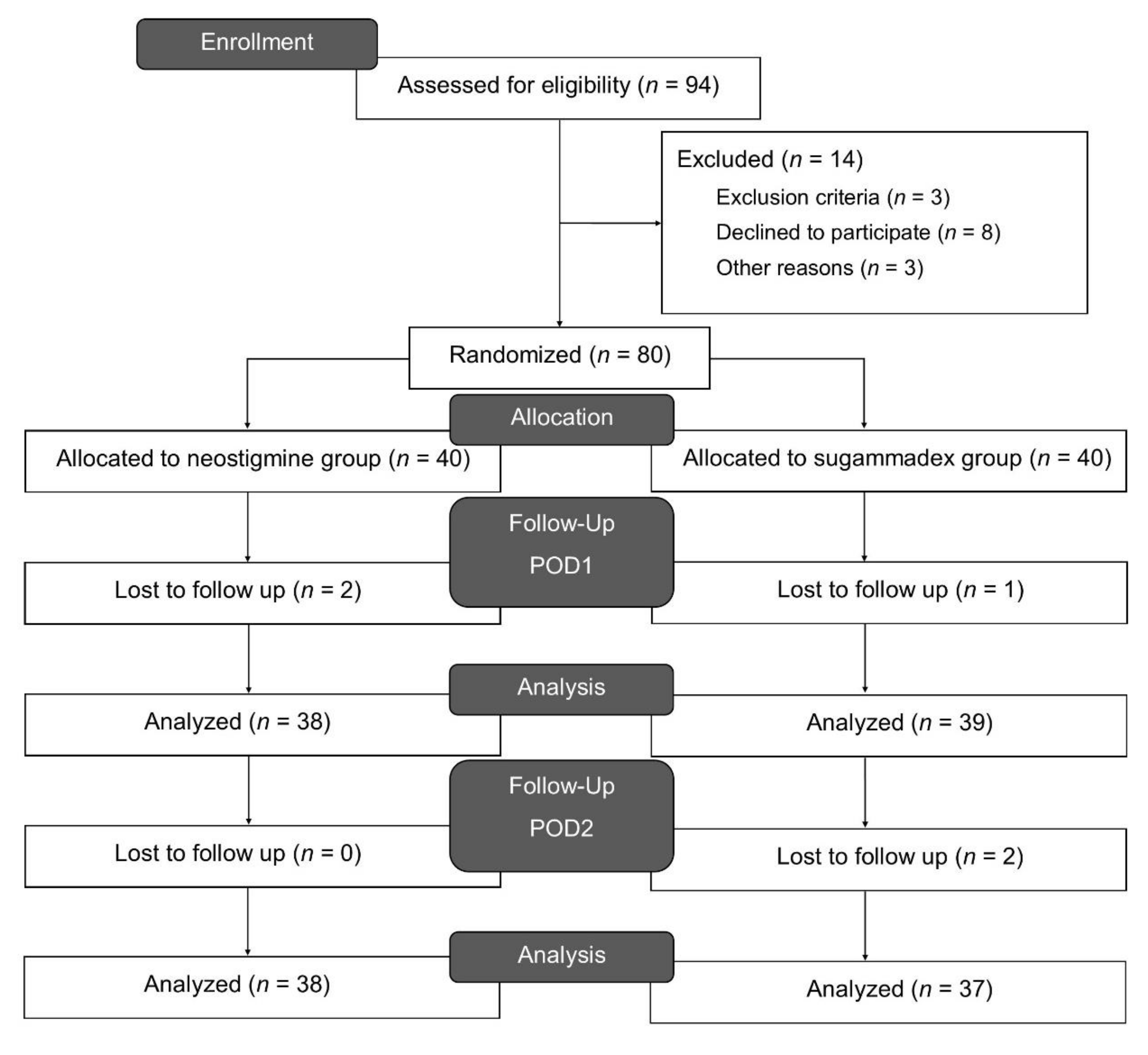
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
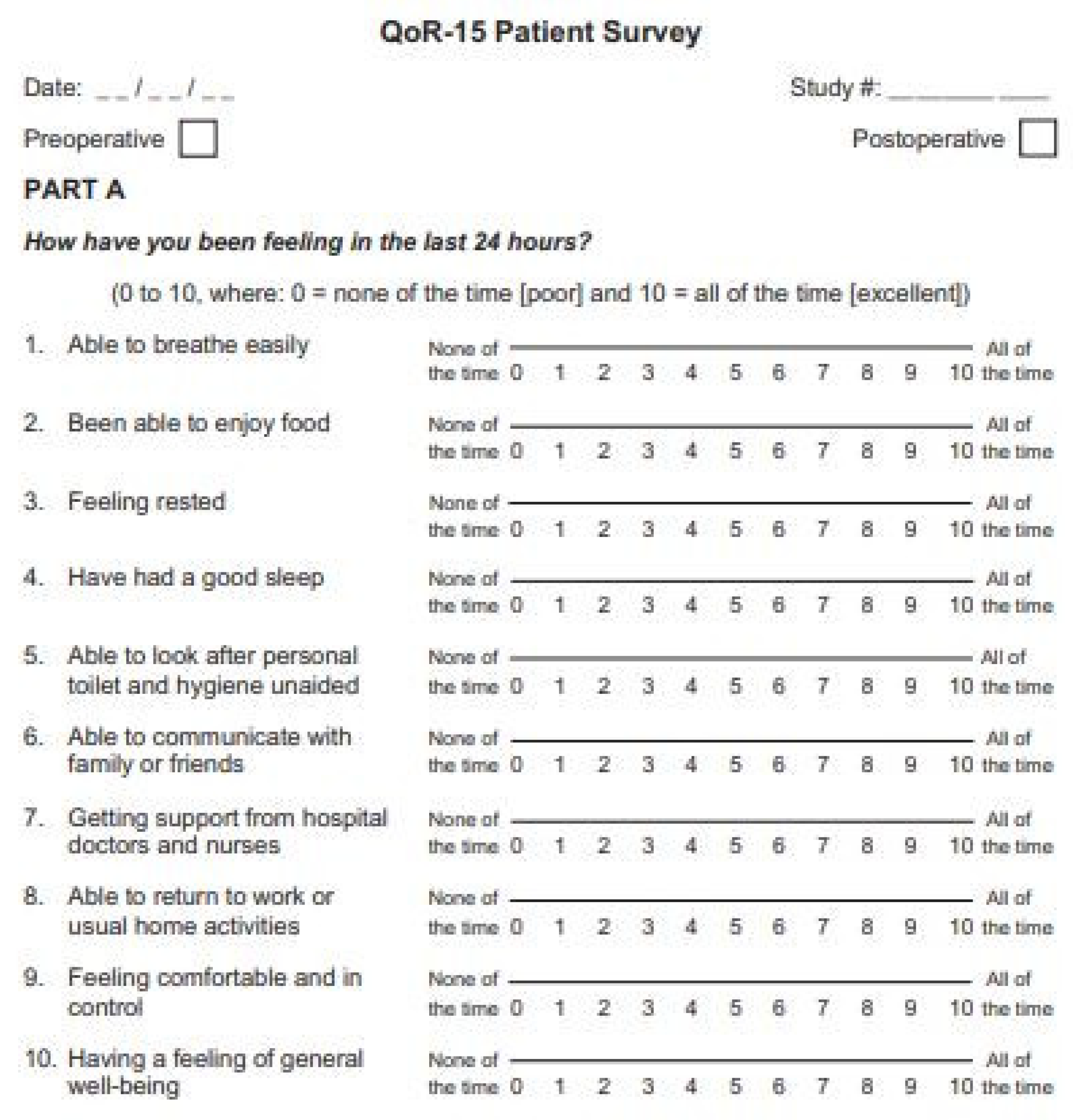
Appendix A
| 1. | Able to breathe easy |
| 2. | Been able to enjoy food |
| 3. | Feeling rested |
| 4. | Have had a good sleep |
| 5. | Able to look after personal toilet and hygiene unaided |
| 6. | Able to communicate with family or friends |
| 7. | Getting support from hospital doctors and nurse |
| 8. | Able to return to work or usual home activities |
| 9. | Feeling comfortable and in control |
| 10. | Having a feeling of general well-being |
| 11. | Moderate pain |
| 12. | Severe pain |
| 13. | Nausea or vomiting |
| 14. | Feeling worried or anxious |
| 15. | Feeling sad or depressed |
Appendix B
Appendix C
| Neostigmine | Sugammadex | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Preop n = 38 | POD1 n = 38 | POD2 n = 38 | Preop n = 39 | POD1 n = 39 | POD2 n = 37 | Preop | POD1 | POD2 | |
| Physical comfort | |||||||||
| Breath | 9.7 ± 0.7 | 8.2 ± 2.7 | 8.7 ± 2.4 | 9.6 ± 1.0 | 7.5 ± 2.6 | 9.4 ± 1.0 | 0.73 | 0.21 | 0.11 |
| Eat | 8.0 ± 3.3 | 5.2 ± 4.0 | 7.0 ± 3.0 | 8.9 ± 2.1 | 5.1 ± 3.9 | 7.7 ± 2.5 | 0.19 | 0.84 | 0.31 |
| Rest | 8.8 ± 2.0 | 5.7 ± 3.3 | 7.9 ± 2.6 | 9.3 ± 1.4 | 6.4 ± 3.0 | 8.5 ± 1.5 | 0.20 | 0.33 | 0.21 |
| Sleep | 8.3 ± 2.3 | 5.9 ± 3.2 | 7.7 ± 2.6 | 8.3 ± 2.1 | 6.1 ± 3.0 | 8.5 ± 1.4 | 0.97 | 0.86 | 0.13 |
| Nausea | 8.1 ± 2.9 | 7.1 ± 3.5 | 7.8 ± 3.2 | 8.9 ± 2.5 | 6.7 ± 3.4 | 7.7 ± 3.0 | 0.21 | 0.56 | 0.93 |
| Physical independence | |||||||||
| Wash | 9.3 ± 1.5 | 6.2 ± 3.6 | 8.2 ± 2.5 | 9.6 ± 1.0 | 6.1 ± 3.6 | 8.3 ± 1.9 | 0.35 | 0.82 | 0.79 |
| Work | 8.7 ± 2.7 | 3.0 ± 3.5 | 5.9 ± 3.5 | 8.8 ± 2.4 | 3.8 ± 3.5 | 6.1 ± 3.0 | 0.12 | 0.30 | 0.72 |
| Pain | |||||||||
| Moderate pain | 7.1 ± 3.1 | 3.2 ± 3.0 | 6.1 ± 2.6 | 8.0 ± 2.3 | 3.6 ± 3.0 | 5.5 ± 2.3 | 0.16 | 0.51 | 0.34 |
| Severe pain | 8.3 ± 2.8 | 4.9 ± 2.9 | 7.1 ± 3.2 | 8.6 ± 2.3 | 5.0 ± 3.1 | 7.1 ± 2.2 | 0.67 | 0.94 | 0.96 |
| Psychological support | |||||||||
| Talk | 9.5 ± 1.1 | 7.3 ± 3.0 | 8.7 ± 2.2 | 9.6 ± 1.1 | 7.4 ± 2.9 | 9.0 ± 1.6 | 0.58 | 0.92 | 0.45 |
| Help | 9.6 ± 1.0 | 9.0 ± 2.0 | 9.1 ± 2.0 | 9.7 ± 0.6 | 9.1 ± 1.8 | 9.0 ± 2.0 | 0.39 | 0.77 | 0.78 |
| Emotional state | |||||||||
| Emotion | 9.2 ± 1.4 | 7.7 ± 2.8 | 8.5 ± 2.4 | 9.3 ± 1.3 | 8.4 ± 1.9 | 9.0 ± 1.3 | 0.62 | 0.17 | 0.22 |
| Well-being | 8.7 ± 2.0 | 5.8 ± 3.0 | 7.6 ± 2.7 | 8.5 ± 1.6 | 5.9 ± 2.7 | 8.1 ± 1.6 | 0.68 | 0.87 | 0.31 |
| Anxiety | 7.7 ± 2.5 | 7.1 ± 3.2 | 8.2 ± 2.9 | 83 ± 2.3 | 6.8 ± 3.1 | 8.9 ± 1.7 | 0.32 | 0.72 | 0.22 |
| Depression | 8.5 ± 2.3 | 8.0 ± 2.5 | 7.8 ± 3.1 | 8.3 ± 2.2 | 7.4 ± 2.8 | 9.0 ± 1.5 | 0.71 | 0.30 | 0.41 |
| Total | 129.3 ± 25.2 | 94.4 ± 30.7 | 116.3 ± 31.1 | 133.6 ± 16.5 | 95.5 ± 27.7 | 122 ± 17.3 | 0.38 | 0.87 | 0.33 |
References
- Myles, P.S.; Weitkamp, B.; Jones, K.; Melick, J.; Hensen, S. Validity and reliability of a postoperative quality of recovery score: The QoR-40. Br. J. Anaesth. 2000, 84, 11–15. [Google Scholar] [CrossRef]
- Gornall, B.; Myles, P.; Smith, C.; Burke, J.; Leslie, K.; Pereira, M.; Bost, J.; Kluivers, K.; Nilsson, U.; Tanaka, Y.; et al. Measurement of quality of recovery using the QoR-40: A quantitative systematic review. Br. J. Anaesth. 2013, 111, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Mittal, G. Pain Management after Laparoscopic Cholecystectomy-A Randomized Prospective Trial of Low Pressure and Standard Pressure Pneumoperitoneum. J. Clin. Diagn.Res. 2014, 8, 92–94. [Google Scholar] [CrossRef]
- Wallace, D.H.; Serpell, M.G.; Baxter, J.N.; O’Dwyer, P.J. Randomized trial of different insufflation pressures for laparoscopic cholecystectomy. Br. J. Surg. 1997, 84, 455–458. [Google Scholar]
- Arslan, M.; Çiçek, R.; Kalender, H.Ü.; Yilmaz, H. Preventing Postoperative Nausea and Vomiting After Laparoscopic Cholecystectomy: A Prospective, Randomized, Double-Blind Study. Curr Ther Res. Clin. Exp. 2011, 72, 1–12. [Google Scholar] [CrossRef]
- Hristovska, A.-M.; Duch, P.; Allingstrup, M.; Afshari, A. Efficacy and safety of Sugammadex versus Neostigmine in reversing neuromuscular blockade in adults. Acta Anaesthesiol. Scand. 2017, 8, CD012763. [Google Scholar] [CrossRef] [PubMed]
- Kirmeier, E.; Eriksson, L.I.; Lewald, H.; Fagerlund, M.J.; Hoeft, A.; Hollmann, M.; Meistelman, C.; Hunter, J.M.; Ulm, K.; Blobner, M.; et al. Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): A multicentre, prospective observational study. Lancet Respir. Med. 2019, 7, 129–140. [Google Scholar] [CrossRef]
- Kheterpal, S.; Vaughn, M.T.; Dubovoy, T.Z.; Shah, N.J.; Bash, L.D.; Colquhoun, D.A.; Shanks, A.M.; Mathis, M.R.; Soto, R.G.; Bardia, A.; et al. Sugammadex versus Neostigmine for Reversal of Neuromuscular Blockade and Postoperative Pulmonary Complications (STRONGER). Anesthesiology 2020, 132, 1371–1381. [Google Scholar] [CrossRef]
- Oh, T.K.; Oh, A.-Y.; Ryu, J.-H.; Koo, B.-W.; Song, I.-A.; Nam, S.W.; Jee, H.-J. Retrospective analysis of 30-day unplanned readmission after major abdominal surgery with reversal by sugammadex or neostigmine. Br. J. Anaesth. 2019, 122, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.D. Miller’s Anesthesia, 9th ed.; Glopper, M.A., Cohen, N.H., Eriksson, L.I., Fleisher, L.A., Leslie, K., Wiener-Kronish, J.P., Eds.; Elsevier: Philadelphia, PA, USA, 2015; Volume 1, pp. 846–847. [Google Scholar]
- Lee, J.H.; Kim, D.; Seo, D.; Son, J.-S.; Kim, D.-C. Validity and reliability of the Korean version of the Quality of Recovery-40 questionnaire. Korean J. Anesthesiol. 2018, 71, 467–475. [Google Scholar] [CrossRef]
- Yoon, S.; Joo, H.; Oh, Y.M.; Lee, J.; Bahk, J.-H.; Lee, H.-J. Validation and clinical utility of the Korean version of the Quality of Recovery-15 with enhanced recovery after surgery: A prospective observational cohort study. Br. J. Anaesth. 2020, 125, 614–621. [Google Scholar] [CrossRef] [PubMed]
- Myles, P.S.; Myles, D.B.; Galagher, W.; Chew, C.; MacDonald, N.; Dennis, A. Minimal Clinically Important Difference for Three Quality of Recovery Scales. Anesthesiology 2016, 125, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Herrera, F.J.; Wong, J.; Chung, F. A Systematic Review of Postoperative Recovery Outcomes Measurements After Ambulatory Surgery. Anesth. Analg. 2007, 105, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Stark, P.A.; Myles, P.S.; Burke, J.A. Development and psychometric evaluation of a postoperative quality of recovery score: The QoR-15. Anesthesiology 2013, 118, 1332–1340. [Google Scholar] [CrossRef]
- Kleif, J.; Waage, J.; Christensen, K.B.; Gögenur, I. Systematic review of the QoR-15 score, a patient- reported outcome measure measuring quality of recovery after surgery and anaesthesia. Brit. J. Anaesth. 2018, 120, 28–36. [Google Scholar] [CrossRef]
- Kim, N.Y.; Koh, J.C.; Lee, K.-Y.; Kim, S.S.; Hong, J.H.; Nam, H.J.; Bai, S.-J. Influence of reversal of neuromuscular blockade with sugammadex or neostigmine on postoperative quality of recovery following a single bolus dose of rocuronium: A prospective, randomized, double-blinded, controlled study. J. Clin. Anesthesia 2019, 57, 97–102. [Google Scholar] [CrossRef]
- Amorim, P.; Lagarto, F.; Gomes, B.; Esteves, S.; Bismarck, J.; Rodrigues, N.; Nogueira, M. Neostigmine vs. sugammadex: Observational cohort study comparing the quality of recovery using the Postoperative Quality Recovery Scale. Acta Anaesthesiol. Scand. 2014, 58, 1101–1110. [Google Scholar] [CrossRef]
- Murphy, G.S.; Szokol, J.W.; Marymont, J.H.; Greenberg, S.B.; Avram, M.J.; Vender, J.S. Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesthesia Analg. 2008, 107, 130–137. [Google Scholar] [CrossRef]
- Sauer, M.; Stahn, A.; Soltesz, S.; Noeldge-Schomburg, G.; Mencke, T. The influence of residual neuromuscular block on the incidence of critical respiratory events. A randomised, prospective, placebo-controlled trial. Eur. J. Anaesthesiol. 2011, 28, 842–848. [Google Scholar] [CrossRef]
- Lee, Y.-J.; Oh, A.-Y.; Koo, B.-W.; Han, J.; Park, J.-H.; Hong, J.-P.; Seo, K.-S. Postoperative residual neuromuscular blockade after reversal based on a qualitative peripheral nerve stimulator response. Eur. J. Anaesthesiol. 2020, 37, 196–202. [Google Scholar] [CrossRef]
- Schepens, T.; Cammu, G.; Saldien, V.; De Neve, N.; Jorens, P.G.; Foubert, L.; Vercauteren, M. Electromyographic activity of the diaphragm during neostigmine or sugammadex-enhanced recovery after neuromuscular blockade with rocuronium: A randomised controlled study in healthy volunteers. Eur. J. Anaesthesiol. 2015, 32, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Cammu, G.; Schepens, T.; De Neve, N.; Wildemeersch, D.; Foubert, L.; Jorens, P.G. Diaphragmatic and intercostal electromyographic activity during neostigmine, sugammadex and neostigmine-sugammadex-enhanced recovery after neuromuscular blockade: A randomised controlled volunteer study. Eur. J. Anaesthesiol. 2017, 34, 8–15. [Google Scholar] [CrossRef]
- Buchanan, F.F.; Myles, P.S.; Cicuttini, F. Effect of patient sex on general anaesthesia and recovery. Br. J. Anaesth. 2011, 106, 832–839. [Google Scholar] [CrossRef]
- Scott, A.J.; Mason, S.E.; Langdon, A.J.; Patel, B.; Mayer, E.; Moorthy, K.; Purkayastha, S. Prospective Risk Factor Analysis for the Development of Post-operative Urinary Retention Following Ambulatory General Surgery. World J. Surg. 2018, 42, 3874–3879. [Google Scholar] [CrossRef]
- Selius, B.A.; Subedi, R. Urinary retention in adults: Diagnosis and initial management. Am. Fam Physician 2008, 77, 643–650. [Google Scholar] [PubMed]
- Cha, J.-E.; Park, S.W.; Choi, Y.I.; Oh, I.D.; Kang, H.Y.; Lee, S.H.; Choi, J.-H. Sugammadex use can decrease the incidence of post-operative urinary retention by avoiding anticholinergics: A retrospective study. Anesth. Pain Med. 2018, 13, 40–46. [Google Scholar] [CrossRef]
| Neostigmine, n = 38 | Sugammadex, n = 39 | |
|---|---|---|
| Age (years) | 51.3 ± 11.5 | 54.1 ± 10.7 |
| Weight (kg) | 69.1 ± 12.5 | 68.1 ± 15.5 |
| Height (cm) | 164.5 ± 9.1 | 166.6 ± 8.6 |
| Sex; male | 18 (47.4%) | 22 ± 56.4% |
| Operation time (min) | 41.2 ± 19.2 | 43.0 ± 21.2 |
| Anesthesia time (min) | 58.3 ± 22.2 | 63.6 ± 22.6 |
| Diagnosis | ||
| Chronic cholecystitis | 16 (42.1%) | 23 (59%) |
| Acute cholecystitis | 12 (31.6%) | 10 (25.6%) |
| Acute pancreatitis | 2 (5.3%) | 0 (0%) |
| GB Polyp | 6 (15.8%) | 5 (12.8%) |
| GB Adenomatosis | 1 (2.6%) | 1 (2.6%) |
| GB stone | 1 (2.6%) | 0 (0%) |
| ASA physical status | ||
| 1 | 18 (47.4%) | 15 (38.5%) |
| 2 | 18 (47.4%) | 19 (48.7%) |
| 3 | 2 (5.3%) | 5 (12.8%) |
| Hypertension | 12 (31.6%) | 9 (23.1%) |
| Diabetes mellitus | 4 (10.5%) | 6 (15.4%) |
| Coronary artery disease | 3 (7.9%) | 8 (20.5%) |
| Cerebral vascular disease | 1 (2.6%) | 2 (5.1%) |
| Cancer | 6 (15.8%) | 10 (25.6%) |
| Neostigmine, n = 38 | Sugammadex, n = 39 | p-Value | |
|---|---|---|---|
| Modified Aldrete score | 7.5 ± 0.6 | 7.4 ± 0.5 | 0.48 |
| PACU stay (min) | 27.7 ± 8.7 | 29.8 ± 9.4 | 0.32 |
| Pain score (NRS) | |||
| 30 min | 6.5 ± 1.4 | 6.6 ± 1.2 | 0.76 |
| 6 h | 3.6 ± 1.1 | 3.4 ± 1.0 | 0.41 |
| 24 h | 3.0 ± 0.7 | 2.9 ± 0.6 | 0.22 |
| Rescue analgesics * | 3.2 ± 1.9 | 3.3 ± 1.2 | 0.79 |
| Morphine equivalent dose (mg) | 14.5 ± 7.3 | 15.6 ± 6.2 | 0.46 |
| Rescue anti-emetics * | 0.4 ± 0.7 | 0.4 ± 0.7 | 0.92 |
| Urinary retention | 6 (15.8%) | 1 (2.6%) | 0.04 † |
| Length of hospital stay (days) | 3.5 ± 0.95 | 3.7 ± 1.0 | 0.29 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, J.; Oh, A.-Y.; Jeon, Y.-T.; Koo, B.-W.; Kim, B.Y.; Kim, D.; Hwang, I. Quality of Recovery after Laparoscopic Cholecystectomy Following Neuromuscular Blockade Reversal with Neostigmine or Sugammadex: A Prospective, Randomized, Controlled Trial. J. Clin. Med. 2021, 10, 938. https://doi.org/10.3390/jcm10050938
Han J, Oh A-Y, Jeon Y-T, Koo B-W, Kim BY, Kim D, Hwang I. Quality of Recovery after Laparoscopic Cholecystectomy Following Neuromuscular Blockade Reversal with Neostigmine or Sugammadex: A Prospective, Randomized, Controlled Trial. Journal of Clinical Medicine. 2021; 10(5):938. https://doi.org/10.3390/jcm10050938
Chicago/Turabian StyleHan, Jiwon, Ah-Young Oh, Yong-Tae Jeon, Bon-Wook Koo, Bo Young Kim, Donghyun Kim, and Insung Hwang. 2021. "Quality of Recovery after Laparoscopic Cholecystectomy Following Neuromuscular Blockade Reversal with Neostigmine or Sugammadex: A Prospective, Randomized, Controlled Trial" Journal of Clinical Medicine 10, no. 5: 938. https://doi.org/10.3390/jcm10050938
APA StyleHan, J., Oh, A.-Y., Jeon, Y.-T., Koo, B.-W., Kim, B. Y., Kim, D., & Hwang, I. (2021). Quality of Recovery after Laparoscopic Cholecystectomy Following Neuromuscular Blockade Reversal with Neostigmine or Sugammadex: A Prospective, Randomized, Controlled Trial. Journal of Clinical Medicine, 10(5), 938. https://doi.org/10.3390/jcm10050938






