Influence of Physical Activity on Pain, Depression and Quality of Life of Patients in Palliative Care: A Proof-of-Concept Study
Abstract
1. Introduction
2. Materials and Methods
- Independence of the patient
- Mobilization of the patient, so as to be independent
- Education of the patient and the caregiver in the field of physical adaptation techniques
- ○
- Self-movement
- ○
- Training within the immediate environment
- ○
- Independence in eating
- ○
- Independence in using the toilet
- ○
- Use of the telephone
- ○
- Use of multimedia receivers
- Safeguarding techniques used to minimize the likelihood of falls, such as:
- ○
- Adapting the apartment and the immediate environment for the safe movement of the palliative person
- ○
- Safe falling techniques
- Use of rehabilitation equipment and orthopedic supplies in safeguarding patients
- ○
- Education of the patient in the field of walking with a support
- ○
- Education of the patient in the field of moving around in a wheelchair, including overcoming architectural barriers
- ○
- Use of mechanical equipment for patient transfer
- ○
- Education on how to equip the dwelling with handrails, railings, handles, non-slip mats, shower chairs etc.
- ○
- Education in the field of equipping the patient with the necessary aids to perform basic and complex everyday activities, as well as activities related to leisure time and rest
- Relaxation techniques
- ○
- Education with basic elements of autogenic training and yoga
- Shaping the environment of palliative patients
- Overcoming architectural barriers
- Counseling in the field of medical and rehabilitation services in mobilization of patients
- Creating conditions for independent physical rehabilitation
- ○
- Education in basic respiratory exercises, and stretching exercises depending on the patient’s current condition
- ○
- Education in creating a home rehabilitation space
- Psychological support in overcoming their own and external limitations
- Organization of free time of a palliative patient
- Integration with the environment and its impact on the quality of life of palliative care patients
- Adaptation of a palliative patient to function in changing life conditions
- Quality of life and acceptance of the disease
Statistical Analysis
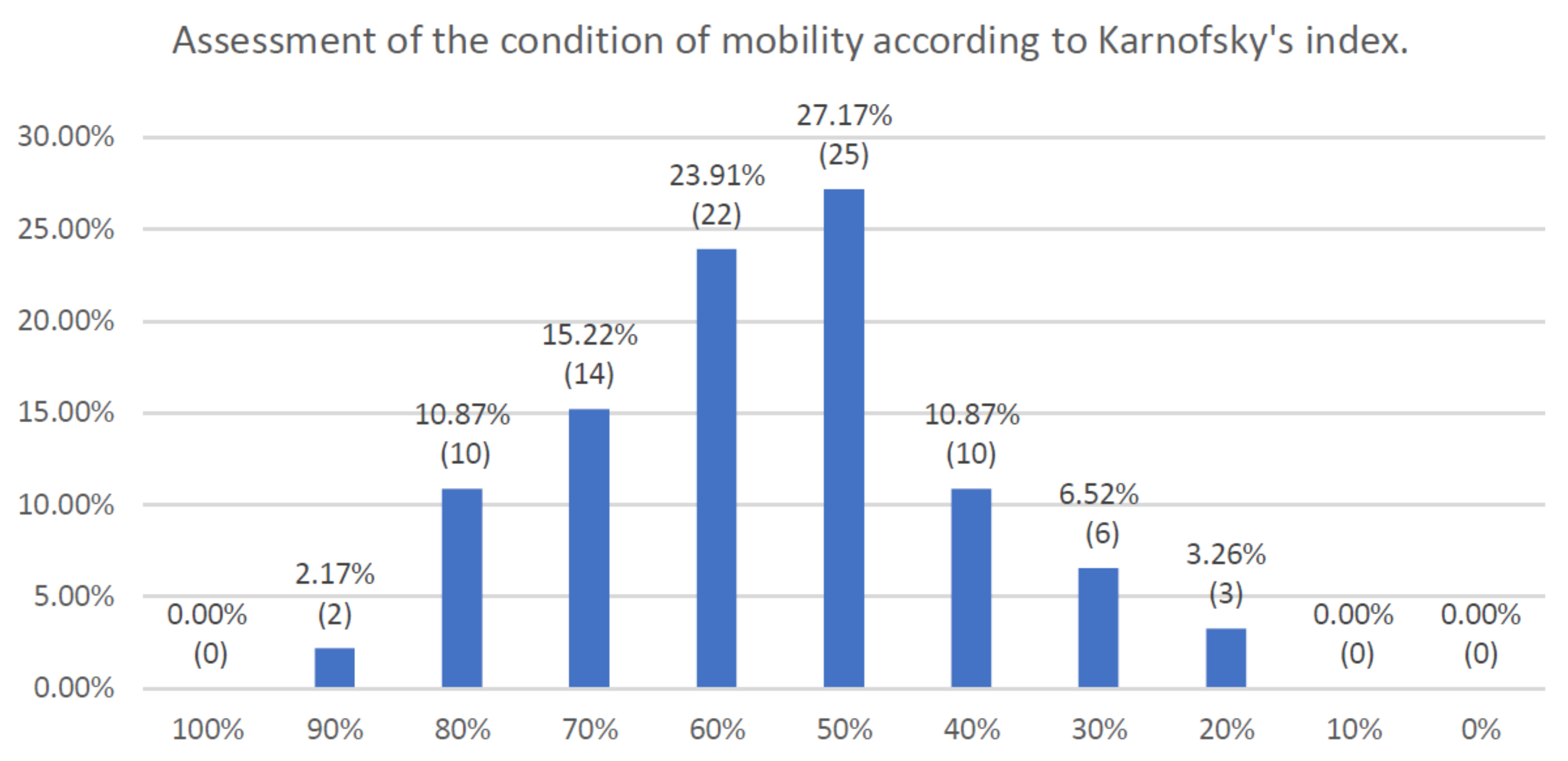
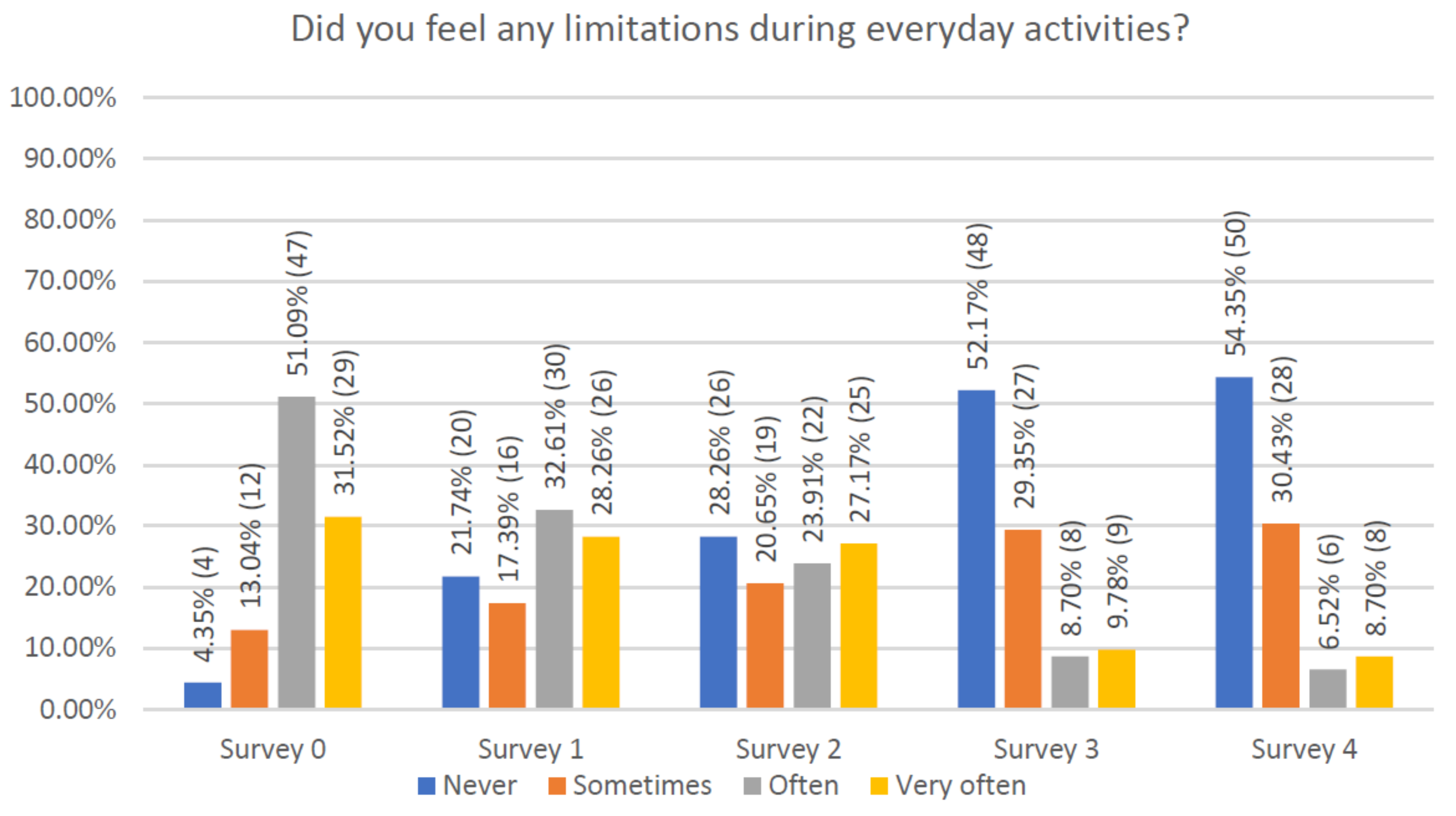
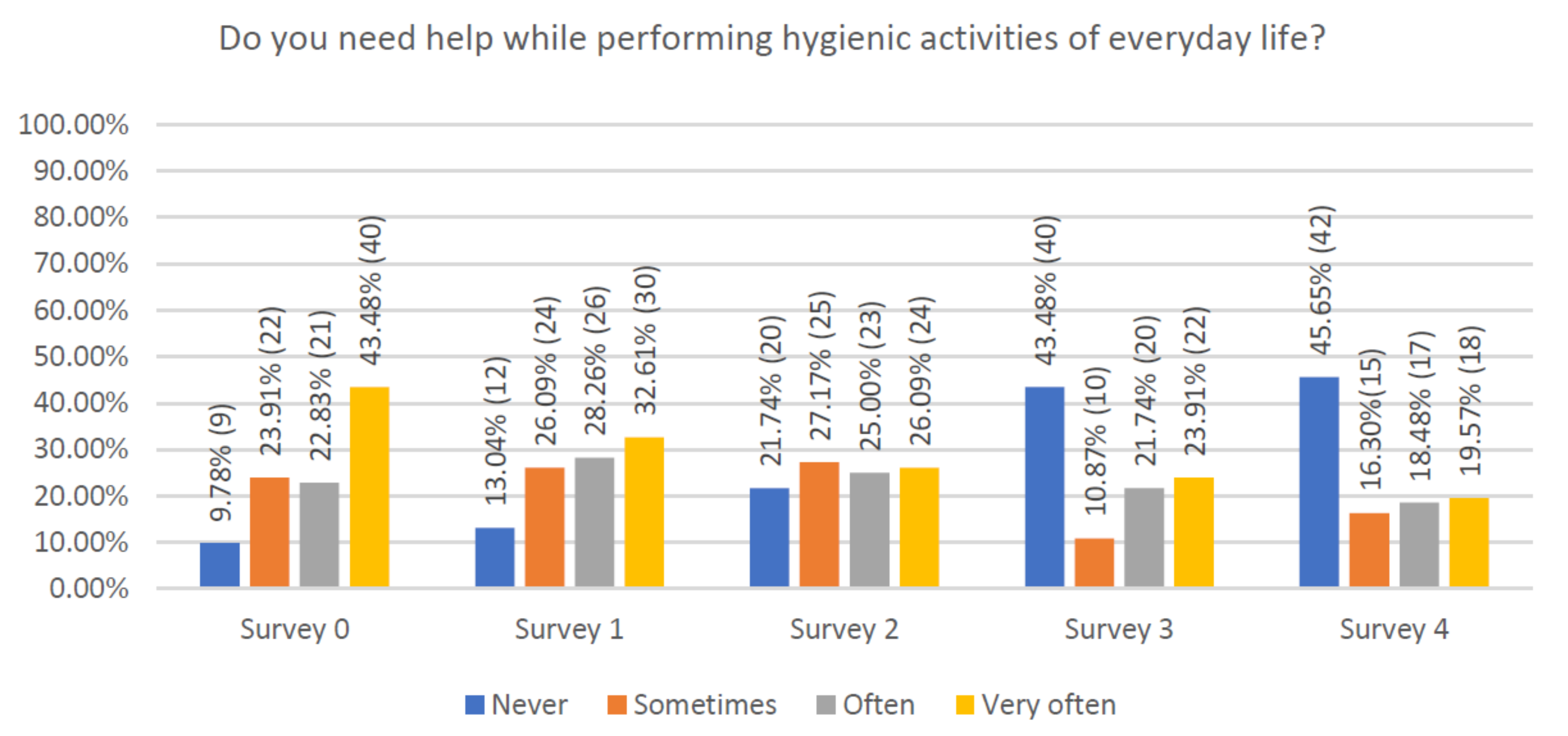
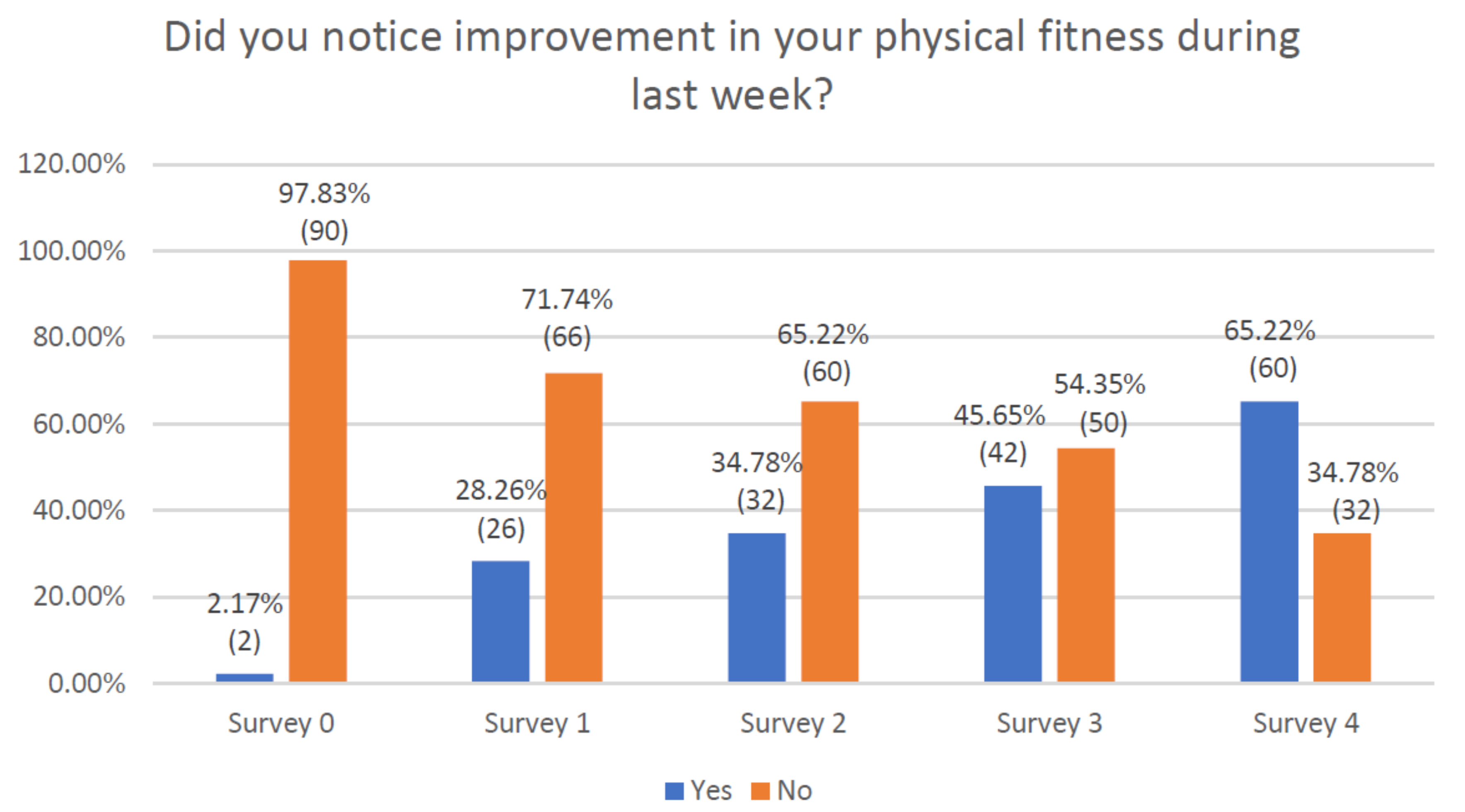
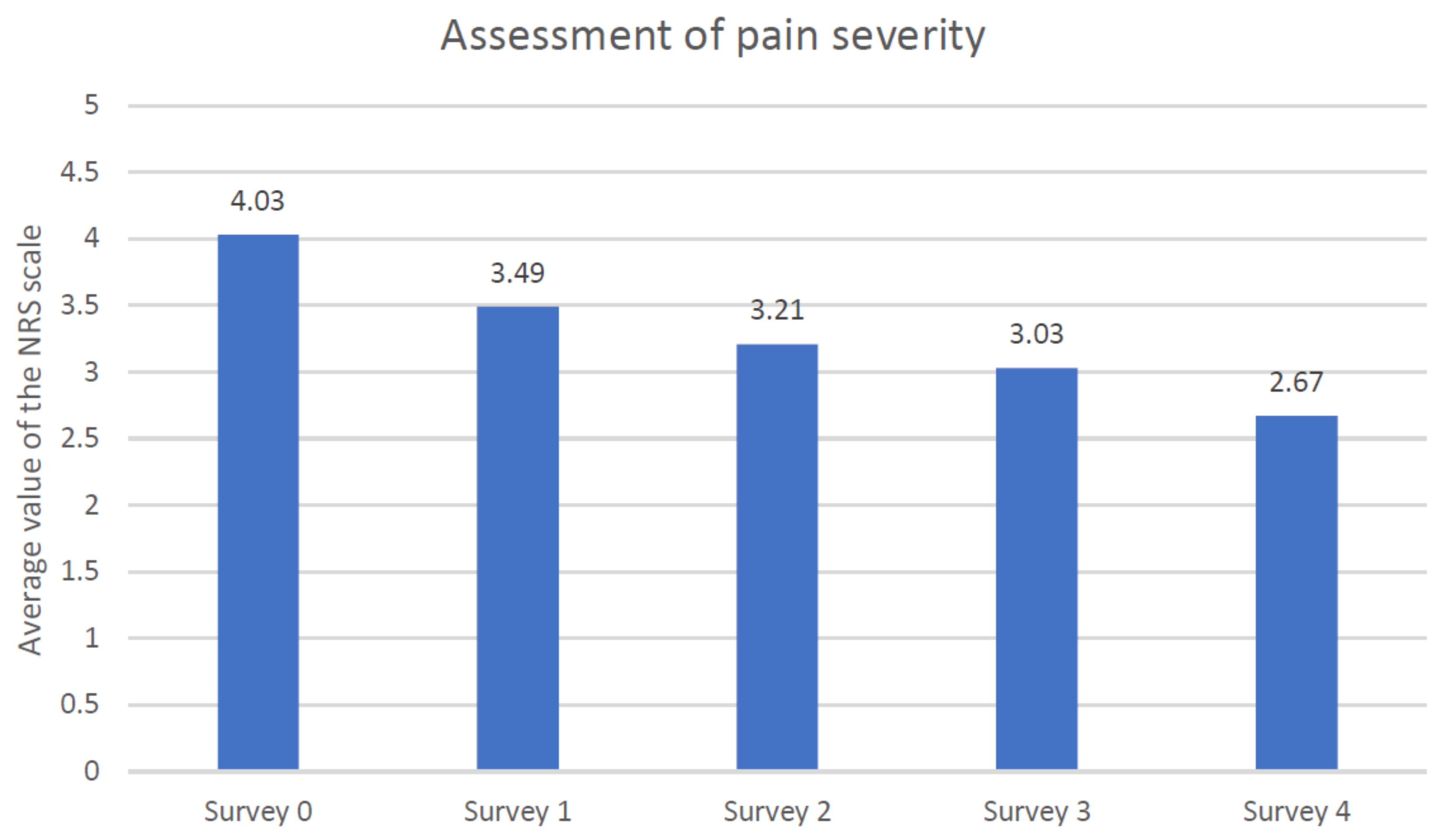
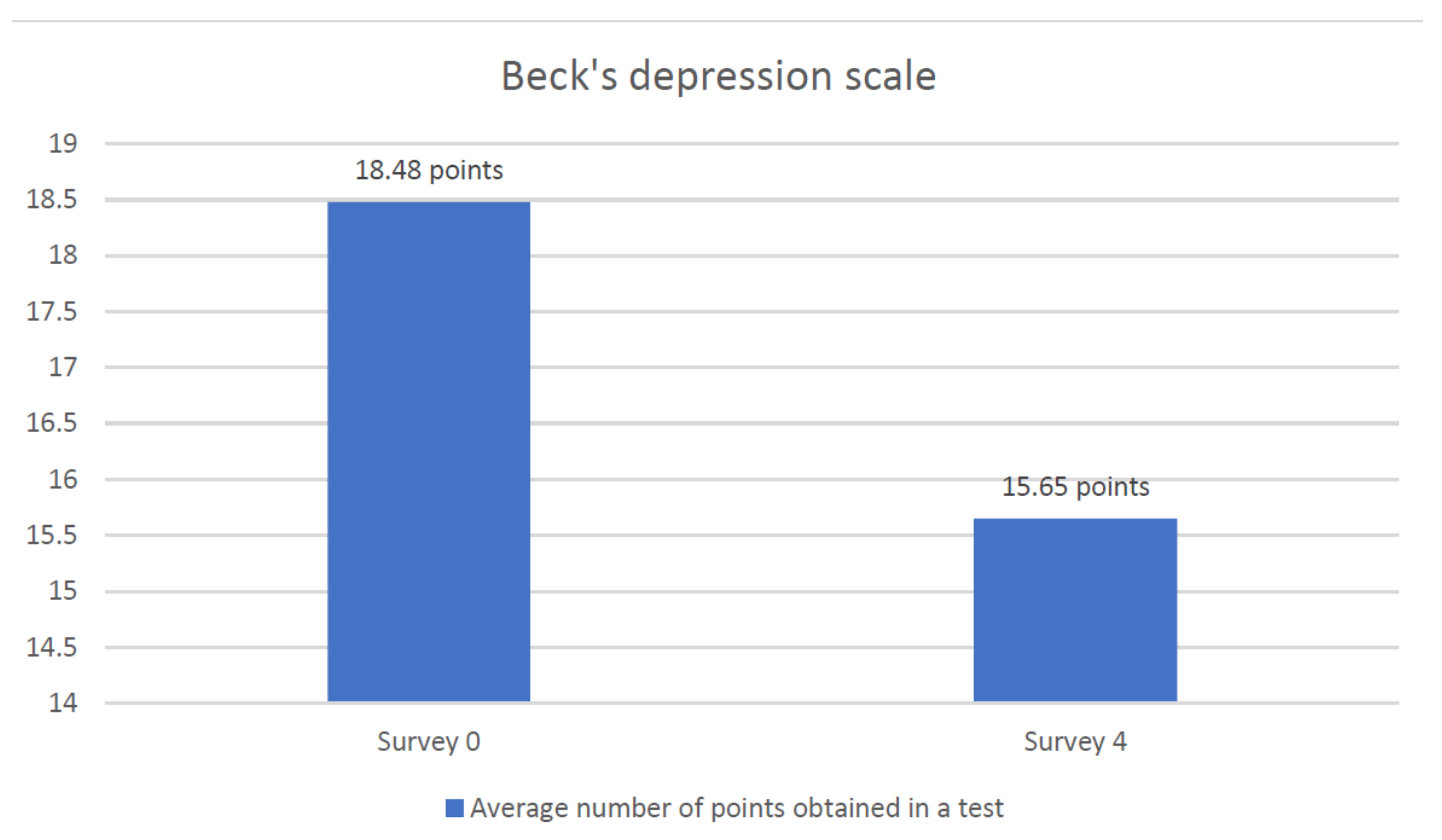
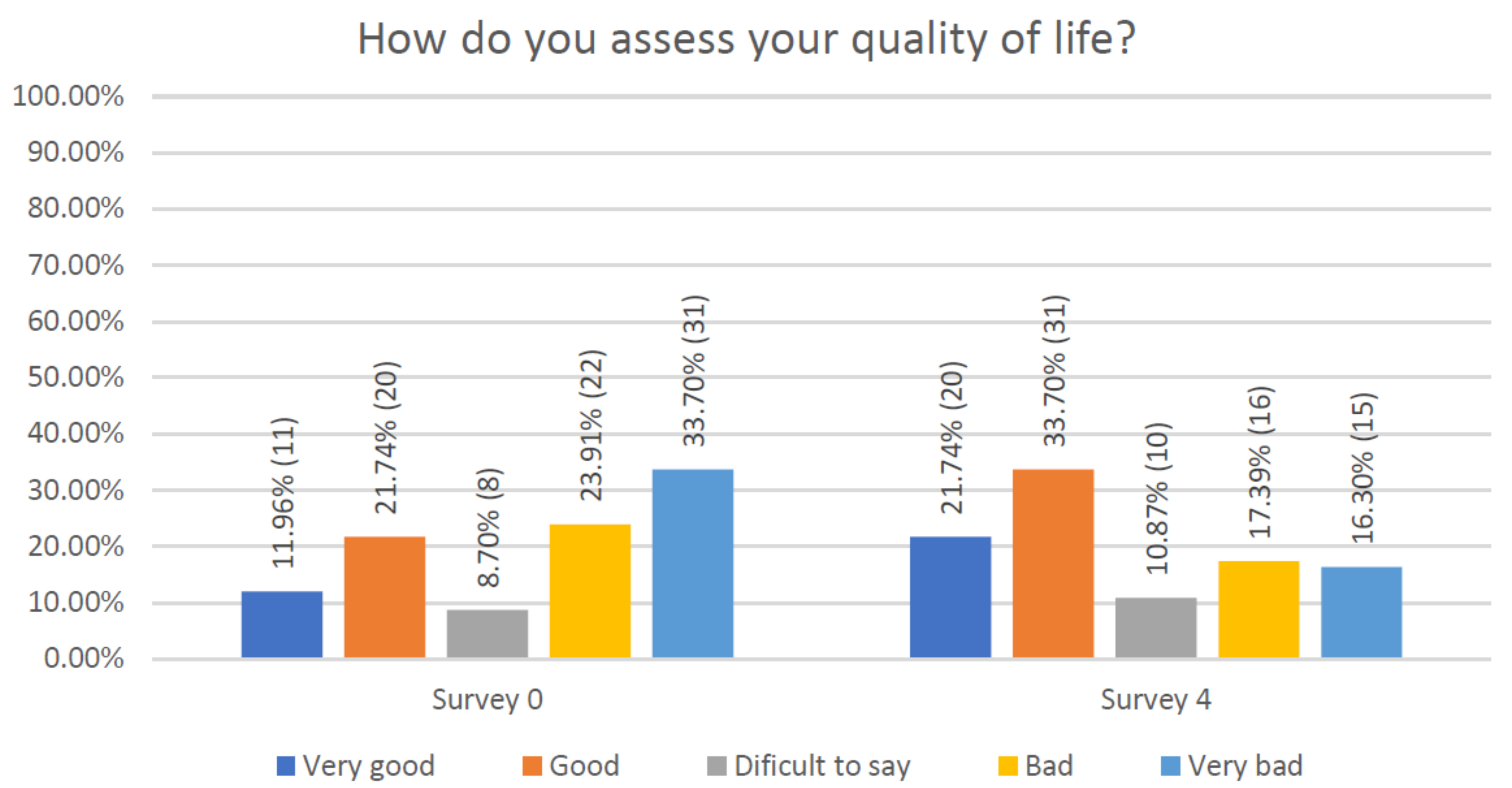
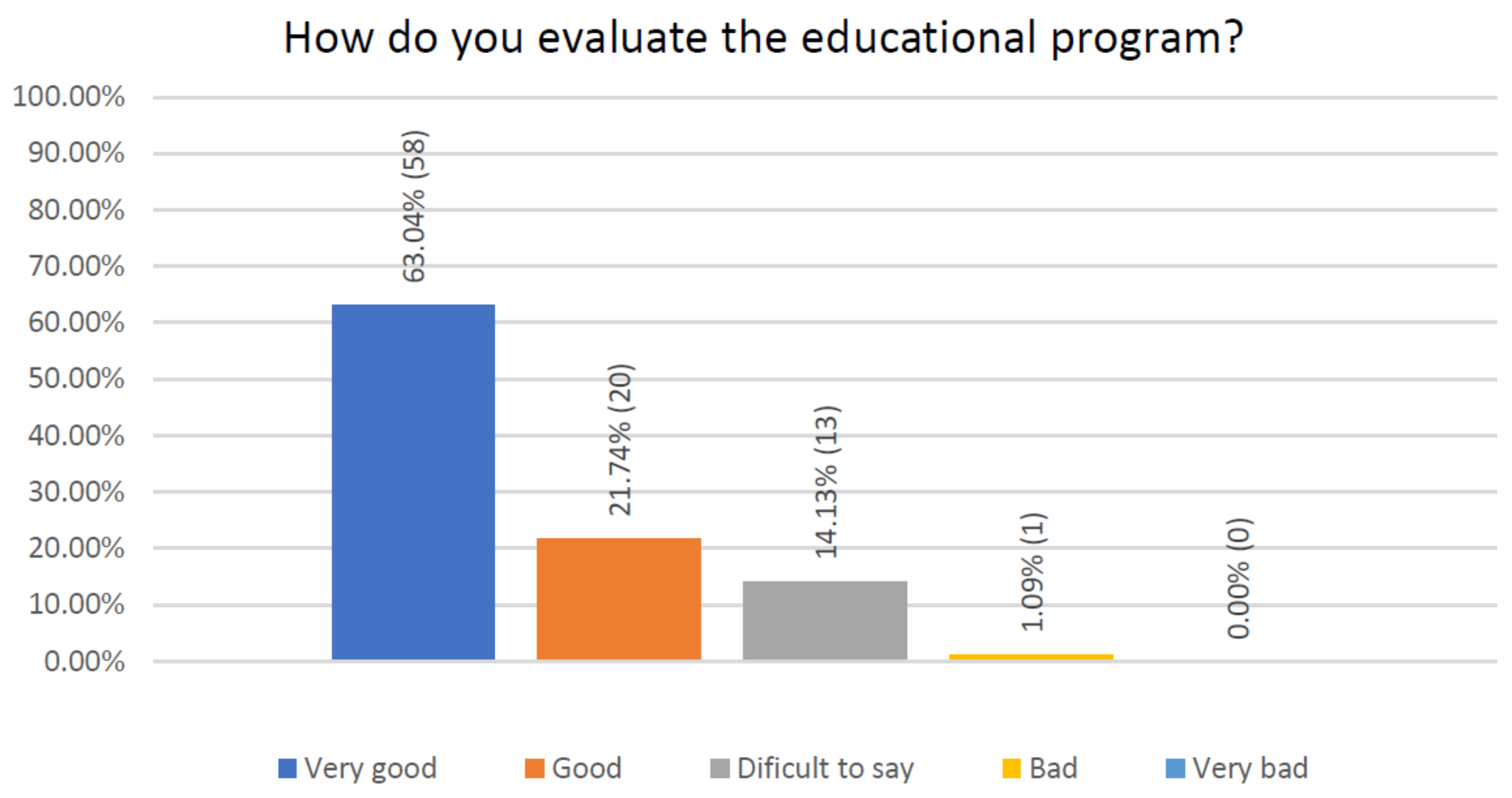
3. Results
4. Discussion
Limitations and Strengths
5. Conclusions
- Palliative patients often or very often experience limitations in the performance of daily activities.
- The examined group of respondents in the majority of cases lead a limited lifestyle and report problems in the sphere of independence, even performing basic activities of everyday life.
- After completing the educational program for a useful physical activity, the majority of patients declared a reduction of limitations in routine everyday activities.
- The derived effect was an increase in the quality of life of the examined group of palliative patients, including reduction of pain and mood improvement.
- The original educational program for physical activity generated a positive response among patients in palliative care, both in a hospice or at home, and their caregivers.
- The implementation of this project in the everyday management of palliative care patients would need little additional efforts, in terms of personnel, and would provide good results, if those obtained with this pilot study are confirmed by further studies.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. The World Health Organization Quality of Life (WHOQOL). 2012. Available online: https://www.who.int/healthinfo/survey/whoqol-qualityoflife/en/ (accessed on 25 April 2020).
- Panzini, R.G.; Mosqueiro, B.P.; Zimpel, R.R.; Bandeira, D.R.; Rocha, N.S.; Fleck, M.P. Quality-of-life and spirituality. Int. Rev. Psychiatry 2017, 29, 263–282. [Google Scholar] [CrossRef] [PubMed]
- Van Loon, M.S.; Van Leeuwen, K.M.; Ostelo, R.W.J.G.; Bosmans, J.E.; Widdershoven, G.A.M. Quality of life in a broader perspective: Does ASCOT reflect the capability approach? Qual. Life Res. 2017, 27, 1181–1189. [Google Scholar] [CrossRef] [PubMed]
- Counted, V.; Possamai, A.; Meade, T. Relational spirituality and quality of life 2007 to 2017: An integrative research review. Heal. Qual. Life Outcomes 2018, 16, 1–18. [Google Scholar] [CrossRef] [PubMed]
- De Walden-Gałuszko, K.; Ciałkowska-Rysz, A. Medycyna Paliatywna, 1st ed.; Państwowy Zakład Wydawnictw Lekarskich: Warszawa, Poland, 2015. [Google Scholar]
- Ciałkowska-Rysz, A.; Dzierżanowski, T. Medycyna Paliatywna, 1st ed.; Termedia: Poznań, Poland, 2019. [Google Scholar]
- Harden, K.; Price, D.; Duffy, E.; Galunas, L.; Rodgers, C. Palliative Care: Improving Nursing Knowledge, Attitudes, and Behaviors. Clin. J. Oncol. Nurs. 2017, 21, E232–E238. [Google Scholar] [CrossRef] [PubMed]
- WHO Definition of Palliative Care. Available online: http://www.who.int/cancer/palliative/definition/en/ (accessed on 21 December 2012).
- Drop, B.; Barańska, A.; Firlej, E.; Janiszewska, M.; Jędrych, M. Palliative care and the growing health needs of older people in Poland. J. Educ. Health Sport 2017, 7, 959–968. [Google Scholar]
- IASP Terminology. Available online: https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698#Pain (accessed on 8 January 2021).
- Mehta, A.; Chan, L.S. Understanding of the Concept of "Total Pain". J. Hosp. Palliat. Nurs. 2008, 10, 26–32. [Google Scholar] [CrossRef]
- Langley, P.; Müller-Schwefe, G.; Nicolaou, A.; Liedgens, H.; Pergolizzi, J.; Varrassi, G. The societal impact of pain in the European Union: Health-related quality of life and healthcare resource utilization. J. Med. Econ. 2010, 13, 571–581. [Google Scholar] [CrossRef] [PubMed]
- Paterniani, A.; Sperati, F.; Esposito, G.; Cognetti, G.; Pulimeno, A.M.L.; Rocco, G.; Diamanti, P.; Bertini, L.; Baldeschi, G.C.; Varrassi, G.; et al. Quality of life and disability of chronic non-cancer pain in adults patients attending pain clinics: A prospective, multicenter, observational study. Appl. Nurs. Res. 2020, 56, 151332. [Google Scholar] [CrossRef] [PubMed]
- Varrassi, G.; De Conno, F.; Orsi, L.; Puntillo, F.; Sotgiu, G.; Zeppetella, J.; Zucco, F. Cancer Pain Management: An Italian Delphi Survey from the Rational Use of Analgesics (RUA) Group. J. Pain Res. 2020, 13, 979–986. [Google Scholar] [CrossRef] [PubMed]
- Antonucci, L.A.; Taurino, A.; Laera, D.; Taurisano, P.; Losole, J.; Lutricuso, S.; Abbatantuono, C.; Giglio, M.; De Caro, M.F.; Varrassi, G.; et al. An Ensemble of Psychological and Physical Health Indices Discriminates Between Individuals with Chronic Pain and Healthy Controls with High Reliability: A Machine Learning Study. Pain Ther. 2020, 9, 601–614. [Google Scholar] [CrossRef] [PubMed]
- Liampas, A.; Rekatsina, M.; Vadalouca, A.; Paladini, A.; Varrassi, G.; Zis, P. Non-Pharmacological Management of Painful Peripheral Neuropathies: A Systematic Review. Adv. Ther. 2020, 37, 4096–4106. [Google Scholar] [CrossRef] [PubMed]
- Zis, P.; Varrassi, G.; Vadalouka, A.; Paladini, A. Psychological Aspects and Quality of Life in Chronic Pain. Pain Res. Manag. 2019, 2019, 8346161. [Google Scholar] [CrossRef] [PubMed]
- Miniszewska, J.; Chrystowska-Jabłońska, B. Strategia radzenia sobie z chorobą nowotworową a jakość życia. Psychoonkologia 2002, 6, 89–94. [Google Scholar]
- Tabassum, S.; Sheetal, K.; Joginder, Y.; Shalu, T.; Khumanshi, Y.; Pinky, T. Role and importance of Physiotherapy during Palliative Care in India: A Review. World J. Res. Rev. 2018, 7, 1–8. [Google Scholar]
- McTiernan, A.; Friedenreich, C.M.; Katzmarzyk, P.T.; Powell, K.E.; Macko, R.; Buchner, D.; Pescatello, L.S.; Bloodgood, B.; Tennant, B.; Vaux-Bjerke, A.; et al. Physical activity in cancer prevention and survival: A systematic review. Med. Sci. Sports Exerc. 2019, 51, 1252–1261. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, J.; Dewey, H.; Thrift, A.; Donnan, G. Inactive and alone: Physical activity within the first 14 days of acute stroke unit care. Stroke 2004, 35, 1005–1009. [Google Scholar] [CrossRef] [PubMed]
- López-Sendín, N.; Alburquerque-Sendín, F.; Cleland, J.A.; Fernández-de-las-Peñas, C. Effects of Physical Therapy on Pain and Mood in Patients with Terminal Cancer: A Pilot Randomized Clinical Trial. J. Altern. Complement. Med. 2012, 18, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Pyszora, A.; Budzyński, J.; Wójcik, A.; Prokop, A.; Krajnik, M. Physiotherapy programme reduces fatigue in patients with advanced cancer receiving palliative care: Randomized controlled trial. Support. Care Cancer 2017, 25, 2899–2908. [Google Scholar] [CrossRef] [PubMed]
- McGrillen, K.; McCorry, N.K. A physical exercise programme for palliative care patients in a clinical setting: Observations and preliminary findings. Prog. Palliat. Care 2014, 22, 352–357. [Google Scholar] [CrossRef]



| Variable | Average | Minimum | Maximum | SD |
|---|---|---|---|---|
| Age | 66.47 | 41.00 | 90.00 | 9.55 |
| Body Mass | 57.05 | 40.00 | 90.00 | 12.72 |
| Height | 162.57 | 148.00 | 186.00 | 9.73 |
| BMI | 21.50 | 15.63 | 35.16 | 3.87 |
| Men | Women | ||||
|---|---|---|---|---|---|
| Pathology | N | % | Pathology | N | % |
| Malignant Cancer of Bronchi and Lung | 12 | 13.04% | Malignant Cancer of Bronchi and Lung | 19 | 20.65% |
| Stomach Cancer | 9 | 9.78% | Breast Cancer | 16 | 17.39% |
| Prostate Cancer | 6 | 6.52% | Colon Cancer | 9 | 9.78% |
| Colon Cancer | 3 | 3.26% | Cancer of Liver and Bile Duct | 5 | 5.43% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Myrcik, D.; Statowski, W.; Trzepizur, M.; Paladini, A.; Corli, O.; Varrassi, G. Influence of Physical Activity on Pain, Depression and Quality of Life of Patients in Palliative Care: A Proof-of-Concept Study. J. Clin. Med. 2021, 10, 1012. https://doi.org/10.3390/jcm10051012
Myrcik D, Statowski W, Trzepizur M, Paladini A, Corli O, Varrassi G. Influence of Physical Activity on Pain, Depression and Quality of Life of Patients in Palliative Care: A Proof-of-Concept Study. Journal of Clinical Medicine. 2021; 10(5):1012. https://doi.org/10.3390/jcm10051012
Chicago/Turabian StyleMyrcik, Dariusz, Wojciech Statowski, Magdalena Trzepizur, Antonella Paladini, Oscar Corli, and Giustino Varrassi. 2021. "Influence of Physical Activity on Pain, Depression and Quality of Life of Patients in Palliative Care: A Proof-of-Concept Study" Journal of Clinical Medicine 10, no. 5: 1012. https://doi.org/10.3390/jcm10051012
APA StyleMyrcik, D., Statowski, W., Trzepizur, M., Paladini, A., Corli, O., & Varrassi, G. (2021). Influence of Physical Activity on Pain, Depression and Quality of Life of Patients in Palliative Care: A Proof-of-Concept Study. Journal of Clinical Medicine, 10(5), 1012. https://doi.org/10.3390/jcm10051012







