Percutaneous Mitral Valve Repair: Outcome Improvement with Operator Experience and a Second-Generation Device
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Post-Procedural Care
2.3. Endpoints and Definitions
2.4. Statistical Analysis
3. Results
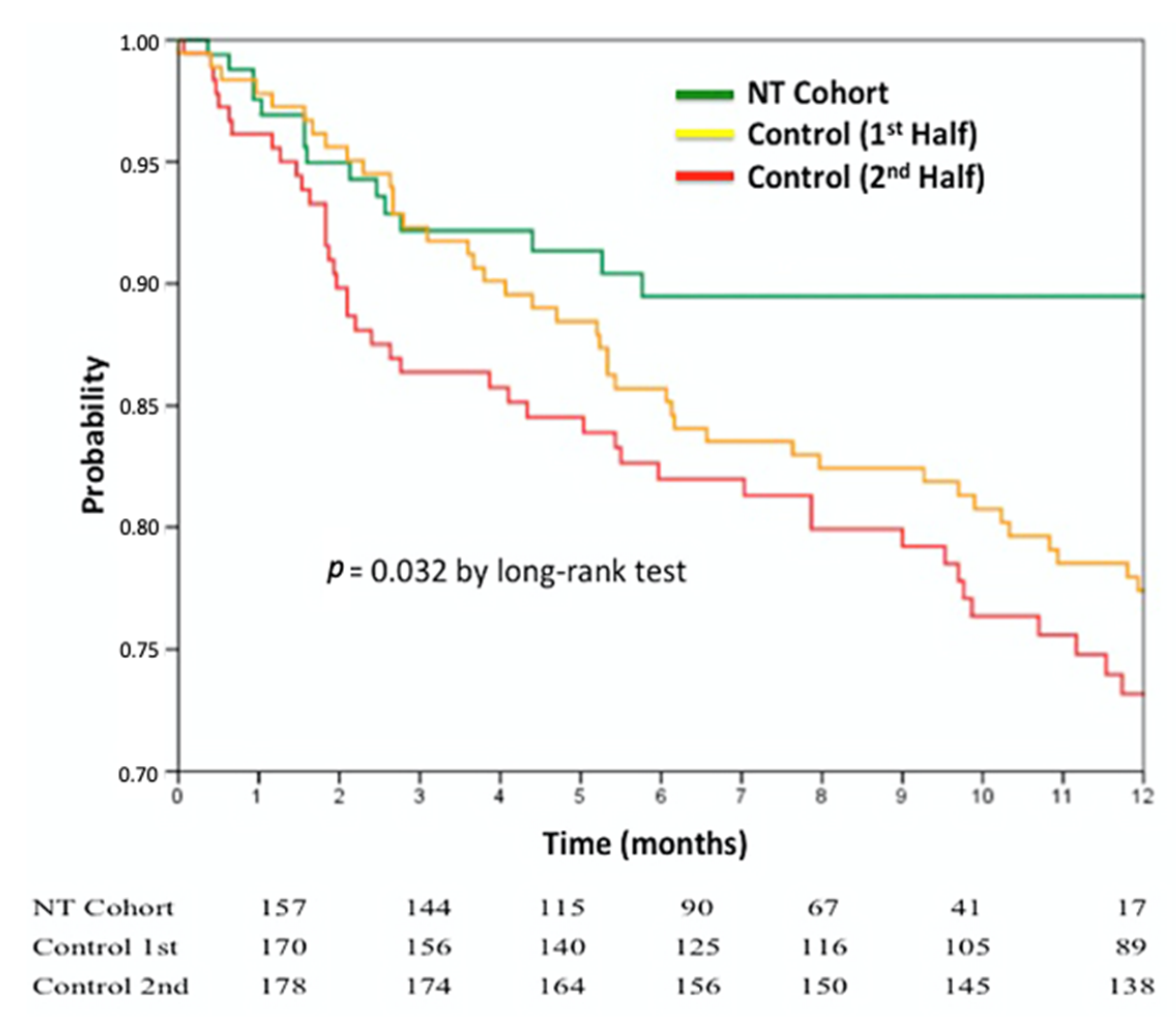
3.1. Clinical Follow-Up
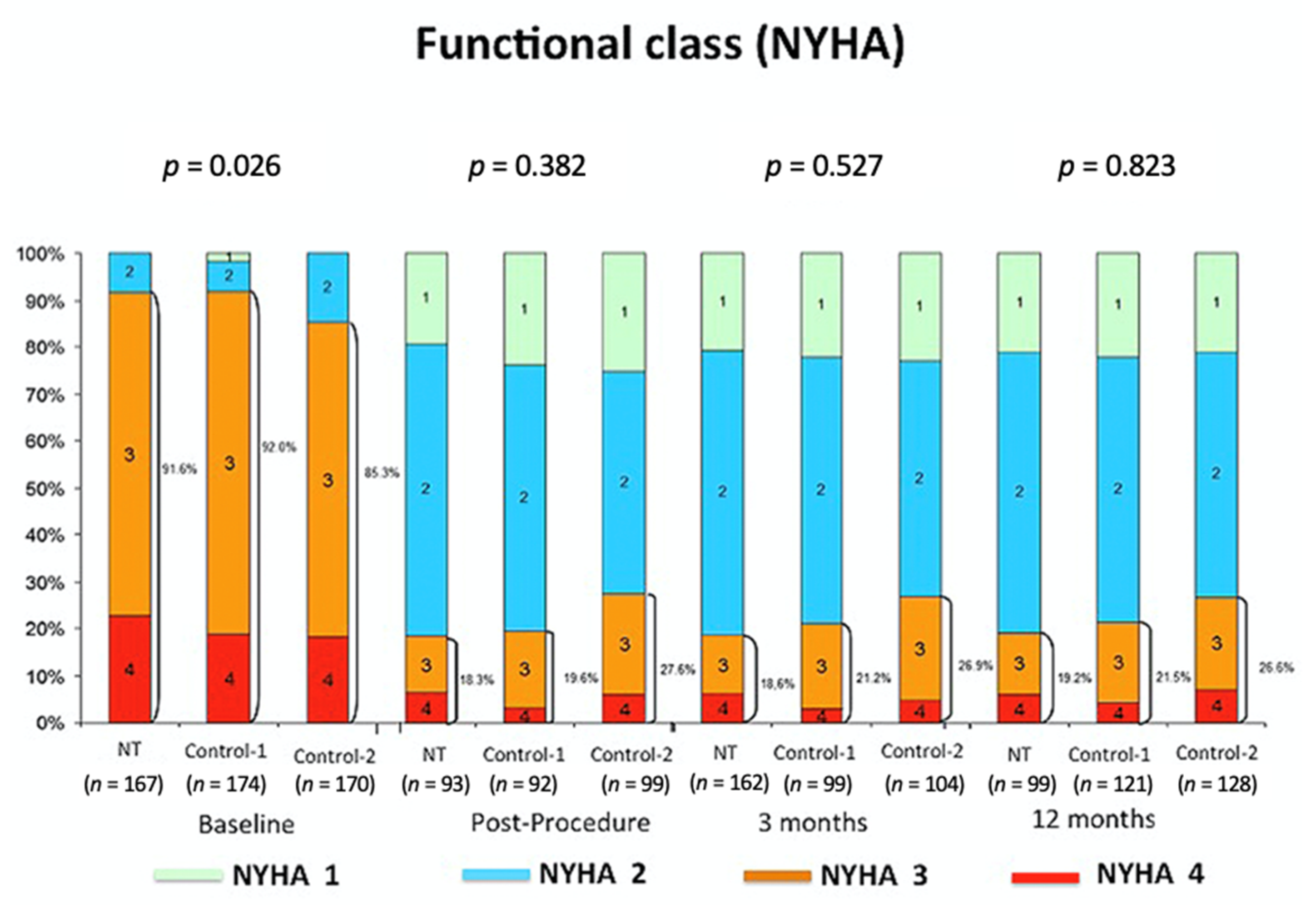
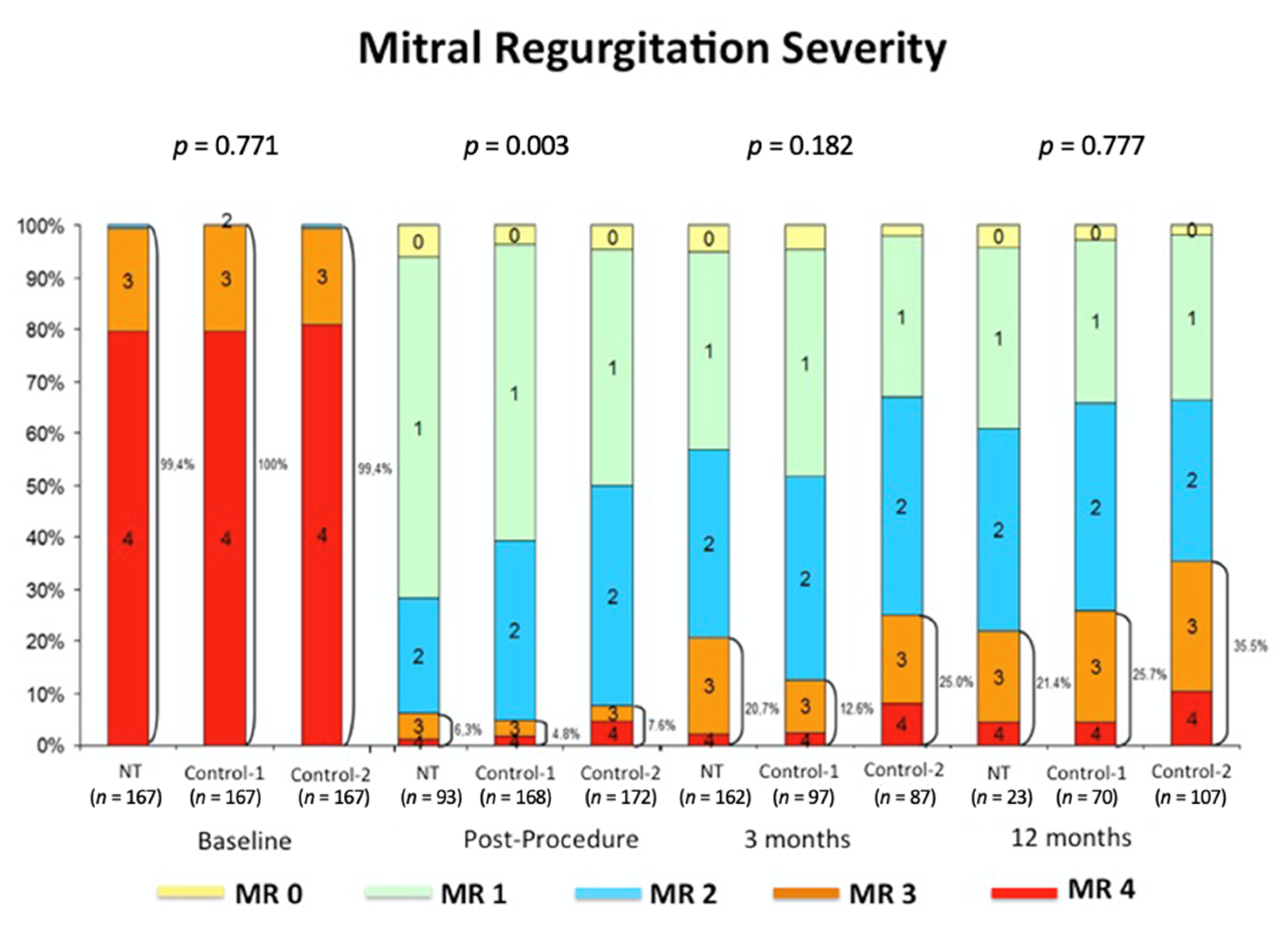
3.2. Echocardiographic Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feldman, T.; Kar, S.; Elmariah, S.; Smart, S.C.; Trento, A.; Siegel, R.J.; Apruzzese, P.; Fail, P.; Rinaldi, M.J.; Smalling, R.W.; et al. Randomized Comparison of Percutaneous Repair and Surgery for Mitral Regurgitation: 5-Year Results of EVEREST II. J. Am. Coll. Cardiol. 2015, 66, 2844–2854. [Google Scholar] [CrossRef] [PubMed]
- Feldman, T.; Foster, E.; Glower, D.D.; Kar, S.; Rinaldi, M.J.; Fail, P.S.; Smalling, R.W.; Siegel, R.; Rose, G.A.; Engeron, E.; et al. Percutaneous repair or surgery for mitral regurgitation. N. Engl. J. Med. 2011, 364, 1395–1406. [Google Scholar] [CrossRef] [PubMed]
- Grasso, C.; Capodanno, D.; Scandura, S.; Cannata, S.; Immè, S.; Mangiafico, S.; Pistritto, A.; Ministeri, M.; Barbanti, M.; Caggegi, A.; et al. One- and Twelve-Month Safety and Efficacy Outcomes of Patients Undergoing Edge-to-Edge Percutaneous Mitral Valve Repair (from the GRASP Registry). Am. J. Cardiol. 2013, 111, 1482–1487. [Google Scholar] [CrossRef] [PubMed]
- Baldus, S.; Schillinger, W.; Franzen, O.; Bekeredjian, R.; Sievert, H.; Schofer, J.; Kuck, K.-H.; Konorza, T.; Möllmann, H.; Hehrlein, C.; et al. MitraClip therapy in daily clinical practice: Initial results from the German transcatheter mitral valve interventions (TRAMI) registry. Eur. J. Hear. Fail. 2012, 14, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Maisano, F.; Franzen, O.; Baldus, S.; Schäfer, U.; Hausleiter, J.; Butter, C.; Ussia, G.P.; Sievert, H.; Richardt, G.; Widder, J.D.; et al. Percutaneous mitral valve interventions in the real world: Early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandomized post-approval study of the MitraClip therapy in Europe. J. Am. Coll. Cardiol. 2013, 62, 1052–1061. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, G.; Estevez-Loureiro, R.; Franzen, O.; Tamburino, C.; Vanderheyden, M.; Lüscher, T.F.; Moat, N.; Price, S.; Dall’Ara, G.; Winter, R.; et al. Percutaneous mitral valve edge-to-edge repair: In-hospital results and 1-year follow-up of 628 patients of the 2011-2012 Pilot European Sentinel Registry. J. Am. Coll. Cardiol. 2014, 64, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Carrasco-Chinchilla, F.; Arzamendi, D.; Romero, M.; de Carlos, F.G.; Alonso-Briales, J.H.; Li, C.H.; Mesa, M.D.; Arnold, R.; Frutos, A.M.S.; Pan, M.; et al. Initial experience of percutaneous treatment of mitral regurgitation with MitraClip(R) therapy in Spain. Rev. Esp. Cardiol. 2014, 67, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Obadia, J.F.; Messika-Zeitoun, D.; Leurent, G.; Iung, B.; Bonnet, G.; Piriou, N.; Lefèvre, T.; Piot, C.; Rouleau, F.; Carrié, D.; et al. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. N. Engl. J. Med. 2018, 379, 2297–2306. [Google Scholar] [CrossRef]
- Stone, G.W.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; Whisenant, B.; Grayburn, P.A.; Rinaldi, M.; Kapadia, S.R.; et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N. Engl. J. Med. 2018, 379, 2307–2318. [Google Scholar] [CrossRef] [PubMed]
- Kalbacher, D.; Schäfer, U.; Bardeleben, R.S.V.; Eggebrecht, H.; Sievert, H.; Nickenig, G.; Butter, C.; May, A.E.; Bekeredjian, R.; Ouarrak, T.; et al. Long-term outcome, survival and predictors of mortality after MitraClip therapy: Results from the German Transcatheter Mitral Valve Interventions (TRAMI) registry. Int. J. Cardiol. 2019, 277, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Grasso, C.; Ince, H. The MitraClip system: Strategies for optimal patient selection and optimised results. EuroIntervention 2016, 12. [Google Scholar] [CrossRef] [PubMed]
- Kebler, M.J.; Whörle, J.; Rpttbauer, W.; Markovic, S. Procedural and Clinical Results of the New Mitraclip NT after Percutaneous Edge to Edge Repair of Mitral Valve Regurgitation. Int. J. Cardiovac. Res. 2018, 7. [Google Scholar] [CrossRef]
- Godino, C.; Scotti, A.; Taramasso, M.; Adamo, M.; Russo, M.; Chiarito, M.; Melillo, F.; Beneduce, A.; Pivato, C.A.; Arrigoni, L.; et al. Two-year cardiac mortality after MitraClip treatment of functional mitral regurgitation in ischemic and non-ischemic dilated cardiomyopathy. Int. J. Cardiol. 2018, 269, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Keßler, M.; Seeger, J.; Muche, R.; Wöhrle, J.; Rottbauer, W.; Markovic, S. Predictors of rehospitalization after percutaneous edge-to-edge mitral valve repair by MitraClip implantation. Eur. J. Heart Fail. 2019, 21, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Hamm, K.; Zacher, M.; Hautmann, M.; Gietzen, F.; Halbfaß, P.; Kerber, S.; Diegeler, A.; Schieffer, B.; Barth, S. Influence of experience on procedure steps, safety, and functional results in edge to edge mitral valve repair-a single center study. Catheter. Cardiovasc. Interv. 2016, 90, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Ledwoch, J.; Franke, J.; Baldus, S.; Schillinger, W.; Bekeredjian, R.; Boekstegers, P.; Hink, U.; Kuck, K.-H.; Ouarrak, T.; Möllmann, H.; et al. Impact of the learning curve on outcome after transcatheter mitral valve repair: Results from the German Mitral Valve Registry. Clin. Res. Cardiol. 2014, 103, 930–937. [Google Scholar] [CrossRef] [PubMed]
| Total N = 545 | Control-1 N = 182 | Control-2 N = 183 | NT Cohort N = 180 | p | |
|---|---|---|---|---|---|
| Age | 72.7 ± 10.8 | 70.1 ± 11.5 | 73.9 ± 9.4 | 74.2 ± 10.9 | <0.001 |
| Gender male (n (%)) | 385 (70.6) | 139 (76.4) | 131 (71.6) | 115 (63.9) | 0.031 |
| BMI (kg/m2) (n = 526/171/355) | 27.2 ± 4.7 | 27.4 ± 5.0 | 26.6 ± 4.4 | 27.5 ± 4.5 | 0.154 |
| BSA (n = 526/171/355) | 1.81 ± 0.19 | 1.83 ± 0.21 | 1.80 ± 0.19 | 1.80 ± 0.18 | 0.104 |
| Hypertension | 373 (68.4) | 118 (64.8) | 126 (68.9) | 129 (71.7) | 0.372 |
| Diabetes mellitus | 181 (33.2) | 55 (30.2) | 63 (34.4) | 63 (35.0) | 0.570 |
| COPD | 119 (21.8) | 43 (23.6) | 38 (20.8) | 38 (21.1) | 0.771 |
| Atrial fibrillation | 300 (55.0) | 88 (48.4) | 101 (55.2) | 111 (61.7) | 0.039 |
| Coronary artery disease | 280 (51.4) | 29 (15.9) | 32 (17.5) | 99 (55.0) | 0.870 |
| Recent myocardial infarction (<90 days) | 29 (5.3) | 6 (3.3) | 10 (5.5) | 13 (7.2) | 0.249 |
| Coronary artery bypass graft | 89 (16.3) | 29 (15.9) | 32 (17.5) | 28 (15.6) | 0.870 |
| Previous percutaneous intervention | 189 (34.7) | 58 (31.9) | 65 (35.5) | 66 (36.7) | 0.605 |
| STS score | 4.3 (2.1–7.5) | 3.8 (1.5–6.7) | 4.2(2.2–7.5) | 4.7 (3.0–8.3) | 0.020 |
| LVEF, % | 39.1 ± 15.8 | 36.9 ± 15.3 | 39.6 ± 16.0 | 38.3 ± 15.7 | 0.071 |
| sPAP | 52 (41–62) | 53 (42–65) | 54 (44–61) | 50 (40–62) | 0.413 |
| LVEDV (mL) | 76 (51–151) | 87 (58–182) | 73 (49–141) | 83 (55–155) | 0.173 |
| Regurgitant orifice area (mm2) | 25.3 ± 26.3 | 28.9 ± 26.3 | 25.1 ± 26.7 | 21.5 ± 25.7 | 0.248 |
| NYHA functional Class | 0.026 | ||||
| 3 (0.6) | 0 | 3 (1.7) | 0 | |
| 50 (9.8) | 25 (14.7) | 11 (6.3) | 14 (8.4) | |
| 356 (69.7) | 114 (67.1) | 127 (73.0) | 115 (68.9) | |
| 102 (20.0) | 31 (18.2) | 33 (19.0) | 38 (22.8) | |
| MR severity (n = 496/162/334) | 0.771 | ||||
| 0 | 0 | 0 | 0 | |
| 0 | 0 | 0 | 0 | |
| 2 (0.4) | 1 (0.6) | 0 | 1 (0.6) | |
| 97 (19.6) | 31 (18.6) | 34 (20.4) | 32 (19.8) | |
| 397 (80.0) | 135 (80.8) | 133 (79.6) | 129 (79.6) | |
| MR etiology | 0.003 | ||||
| 333 (66.5) | 126 (75.0) | 118 (69.0) | 89 (54.9) | |
| 97 (19.4) | 26 (15.5) | 29 (17.0) | 42 (25.9) | |
| 71 (14.2) | 16 (9.5) | 24 (14.0) | 31 (18.1) |
| Total N = 545 | Control-1 N = 182 | Control-2 N = 183 | NT Cohort N = 180 | p | |
|---|---|---|---|---|---|
| Procedural success | 454 (93.6) | 155 (85.2) | 156 (85.2) | 143 (93.7) | 0.237 |
| Number of clips (mean ± SD) | 1.47 ± 0.71 | 1.65 ± 0.71 | 1.54 ± 0.66 | 1.36 ± 0.61 | <0.001 |
| Device time (min) | 80 (60–100) | 100 (60–150) | 80 (60–100) | 60 (45–92) | <0.001 |
| Procedural time (min) | 131 (106–180) | 150 (120–240) | 120 (100–173) | 120 (100–163) | <0.001 |
| MR pre clip | 0.221 | ||||
| 0 | 0 | 0 | 0 | |
| 0 | 0 | 0 | 0 | |
| 1 (0.2) | 1 (0.6) | 0 | 0 | |
| 106 (21.2) | 28 (16.4) | 40 (23.8) | 38 (23.5) | |
| 394 (78.6) | 142 (83.0) | 128 (76.2) | 124 (76.5) | |
| MR post clip | 0.003 | ||||
| 24 (4.8) | 8 (4.7) | 6 (3.6) | 10 (6.3) | |
| 278 (55.7) | 78 (45.3) | 96 (57.1) | 104 (65.4) | |
| 166 (33.3) | 73 (42.4) | 58 (34.5) | 35 (22.0) | |
| 18 (3.6) | 5 (2.9) | 5 (3.0) | 8 (5.0) | |
| 13 (2.6) | 8 (4.7) | 3 (1.8) | 2 (1.3) | |
| 0.61 ± 1.16 | 0.57 ± 1.33 | 0.60 ± 1.16 | 0.71 ± 1.17 | 0.349 |
| 2.29 ± 1.82 | 2.27 ± 1.71 | 2.19 ± 1.86 | 2.52 ± 1.74 | 0.056 |
| Total N = 545 | Control-1 N = 182 | Control-2 N = 183 | NT Cohort N = 180 | p | |
|---|---|---|---|---|---|
| Partial or total clip detachment | 8 (1.7) | 2 (1.2) | 3 (2.0) | 3 * (1.9) | 0.837 |
| Cordal rupture | 7 (1.5) | 2 (1.2) | 2 (1.3) | 3 (1.9) | 0.857 |
| Cordal entrapment | 5 (1.1) | 2 (1.2) | 2 (1.3) | 1 (0.6) | 0.810 |
| Femoral pseudoaneurysm | 7 (1.5) | 3 (1.8) | 2 (1.3) | 2 (1.3) | 0.903 |
| Femoral arteriovenous istula | 4 (0.8) | 2 (1.2) | 1 (0.6) | 1 (0.6) | 0.819 |
| Transfusion | 27 (5.7) | 11 (6.7) | 10 (6.5) | 6 (3.9) | 0.501 |
| Vascular surgery | 2 (0.4) | 1 (0.6) | 1 (0.7) | 0 | 0.999 |
| Pericardial effusion | 12 (2.5) | 7 (4.3) | 1 (0.6) | 4 (2.6) | 0.025 |
| 8 (1.7) | 4 (2.4) | 0 | 4 (2.6) | |
| 3 (0.6) | 3 (1.8) | 0 | 0 | |
| 1 (0.2) | 0 | 1 (0.6) | 0 | |
| Air embolism | 5 (1.1) | 0 | 2 (1.3) | 3 (1.9) | 0.112 |
| In-hospital death | 11 (2.3) | 5 (3.0) | 5 (3.1) | 1 (0.7) | 0.199 |
| Length of stay (days) | 4 (2–7) | 5 (3–7) | 4 (2–6) | 3 (2–6) | 0.016 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freixa, X.; Estévez-Loureiro, R.; Carrasco-Chinchilla, F.; Millán, X.; Amat-Santos, I.; Regueiro, A.; Nombela-Franco, L.; Pascual, I.; Cid, B.; López-Mínguez, J.R.; et al. Percutaneous Mitral Valve Repair: Outcome Improvement with Operator Experience and a Second-Generation Device. J. Clin. Med. 2021, 10, 734. https://doi.org/10.3390/jcm10040734
Freixa X, Estévez-Loureiro R, Carrasco-Chinchilla F, Millán X, Amat-Santos I, Regueiro A, Nombela-Franco L, Pascual I, Cid B, López-Mínguez JR, et al. Percutaneous Mitral Valve Repair: Outcome Improvement with Operator Experience and a Second-Generation Device. Journal of Clinical Medicine. 2021; 10(4):734. https://doi.org/10.3390/jcm10040734
Chicago/Turabian StyleFreixa, Xavier, Rodrigo Estévez-Loureiro, Fernando Carrasco-Chinchilla, Xavier Millán, Ignacio Amat-Santos, Ander Regueiro, Luis Nombela-Franco, Isaac Pascual, Belen Cid, José Ramón López-Mínguez, and et al. 2021. "Percutaneous Mitral Valve Repair: Outcome Improvement with Operator Experience and a Second-Generation Device" Journal of Clinical Medicine 10, no. 4: 734. https://doi.org/10.3390/jcm10040734
APA StyleFreixa, X., Estévez-Loureiro, R., Carrasco-Chinchilla, F., Millán, X., Amat-Santos, I., Regueiro, A., Nombela-Franco, L., Pascual, I., Cid, B., López-Mínguez, J. R., Hernández-Antolín, R. A., Cruz-González, I., Andraka, L., Goicolea, J., Ruíz-Quevedo, V., Díez, J. L., Berenguer, A., Baz, J. A., Pan, M., ... Arzamendi, D. (2021). Percutaneous Mitral Valve Repair: Outcome Improvement with Operator Experience and a Second-Generation Device. Journal of Clinical Medicine, 10(4), 734. https://doi.org/10.3390/jcm10040734









