Lifestyle and Psychological Factors of Women with Pregnancy Intentions Who Become Pregnant: Analysis of a Longitudinal Cohort of Australian Women
Abstract
1. Introduction
2. Method
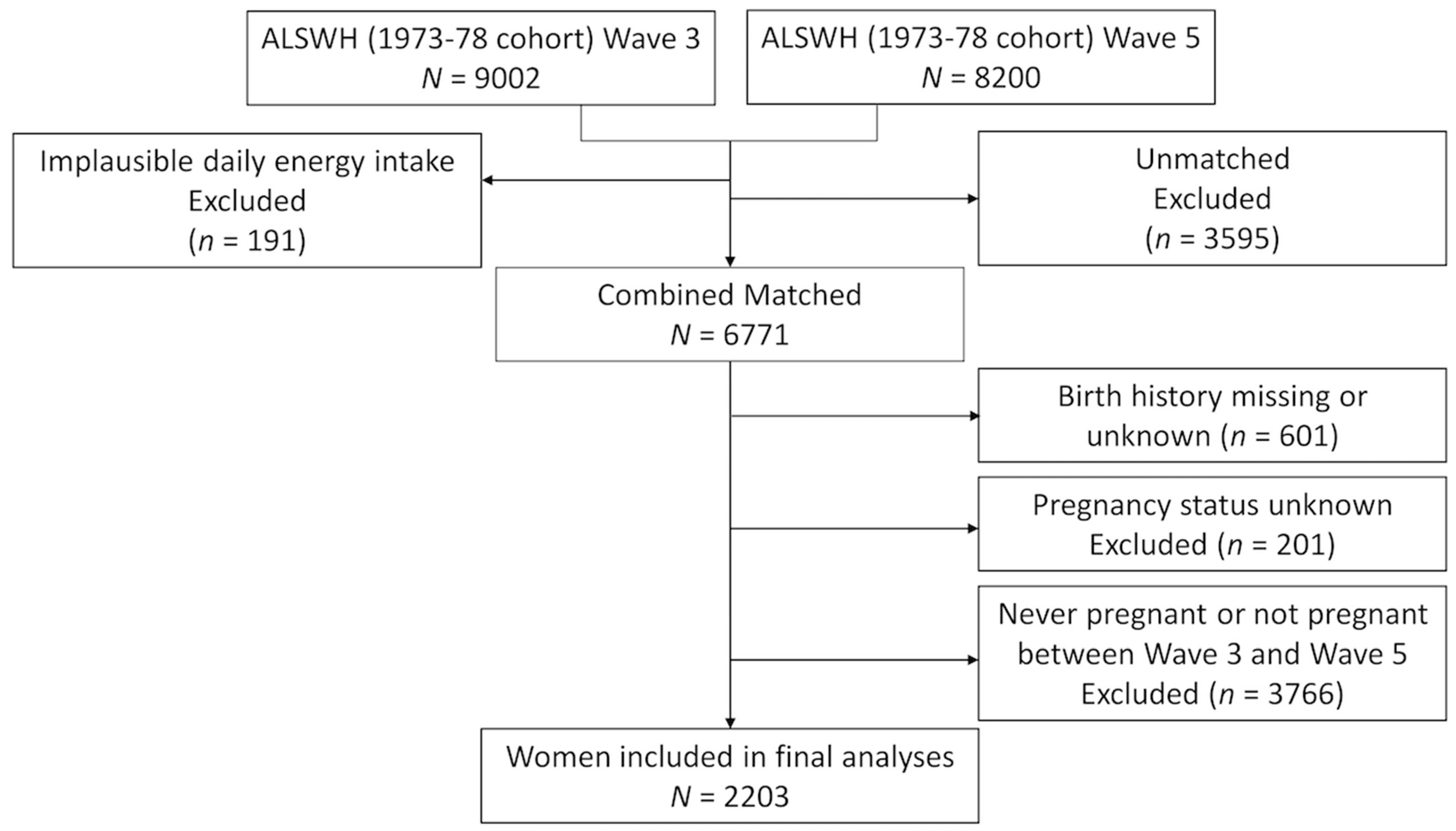
2.1. Study Population
2.2. Measures
2.2.1. Pregnancy Intentions
2.2.2. Demographic and Anthropometric Variables
2.2.3. Lifestyle Factors
2.2.4. Psychological Factors
2.3. Statistical Analyses
3. Results
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.; Boyle, J.A.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; Rode, L.; et al. Association of Gestational Weight Gain With Maternal and Infant Outcomes: A Systematic Review and Meta-analysis. JAMA 2017, 317, 2207–2225. [Google Scholar] [CrossRef]
- Institute of Medicine; National Research Council. Weight Gain During Pregnancy: Reexamining the Guidelines—Report Brief; Institute of Medicine: Washington, DC, USA, 2009. [Google Scholar]
- American College of Obstetricians and Gynecologists. Comittee Opinion No. 804: Physical Activity and Exercise During Pregnancy and the Postpartum Period. Obstet. Gynecol. 2020, 135, e178–e188. [Google Scholar] [CrossRef]
- Yao, D.; Chang, Q.; Wu, Q.-J.; Gao, S.-Y.; Zhao, H.; Liu, Y.-S.; Jiang, Y.-T.; Zhao, Y.-H. Relationship Between Maternal Central Obesity and the Risk of Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis of Cohort Studies. J. Diabetes Res. 2020, 2020, 6303820. [Google Scholar] [CrossRef]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the Women at Risk of Antenatal Anxiety and Depression: A Systematic Review. J. Affect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.; McPhie, S.; Fuller-Tyszkiewicz, M.; Gillman, M.W.; Skouteris, H. Psychological Health and Lifestyle Management Preconception and in Pregnancy. Semin. Reprod. Med. 2016, 34, 121–128. [Google Scholar] [CrossRef]
- Chivers, B.R.; Boyle, J.A.; Lang, A.Y.; Teede, H.J.; Moran, L.J.; Harrison, C.L. Preconception Health and Lifestyle Behaviours of Women Planning a Pregnancy: A Cross-Sectional Study. J. Clin. Med. 2020, 9, 1701. [Google Scholar] [CrossRef]
- Hall, J.A.; Benton, L.; Copas, A.; Stephenson, J. Pregnancy Intention and Pregnancy Outcome: Systematic Review and Meta-Analysis. Matern. Child Health J. 2017, 21, 670–704. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.S.; Balkhair, T.; Ohlsson, A.; Beyene, J.; Scott, F.; Frick, C. Intention to Become Pregnant and Low Birth Weight and Preterm Birth: A Systematic Review. Matern. Child Health J. 2011, 15, 205–216. [Google Scholar] [CrossRef]
- Hill, B.; Ling, M.; Mishra, G.; Moran, L.J.; Teede, H.J.; Bruce, L.; Skouteris, H. Lifestyle and Psychological Factors Associated with Pregnancy Intentions: Findings from a Longitudinal Cohort Study of Australian Women. Int. J. Environ. Res. Public Health 2019, 16, 5094. [Google Scholar] [CrossRef] [PubMed]
- Malek, L.; Umberger, W.; Makrides, M.; Zhou, S.J. Adherence to the Australian Dietary Guidelines During Pregnancy: Evidence from a National Study. Public Health Nutr. 2015, 19, 1155–1163. [Google Scholar] [CrossRef]
- Nkrumah, I.; North, M.; Kothe, E.; Chai, T.L.; Pirotta, S.; Lim, S.; Hill, B. The Relationship Between Pregnancy Intentions and Diet or Physical Activity Behaviors in the Preconception and Antenatal Periods: A Systematic Review and Meta-Analysis. J. Midwifery Womens Health 2020, 65, 660–680. [Google Scholar] [CrossRef]
- Stephenson, J.; Heslehurst, N.; Hall, J.; Schoenaker, D.A.J.M.; Hutchinson, J.; Cade, J.E.; Poston, L.; Barrett, G.; Crozier, S.R.; Barker, M.; et al. Before the Beginning: Nutrition and Lifestyle in the Preconception Period and its Importance for Future Health. Lancet 2018, 391, 1830–1841. [Google Scholar] [CrossRef]
- Brown, W.J.; Bryson, L.; Byles, J.E.; Dobson, A.J.; Lee, C.; Mishra, G.; Schofield, M. Women’s Health Australia: Recruitment for a National Longitudinal Cohort Study. Women Health 1999, 28, 23–40. [Google Scholar] [CrossRef]
- Lee, C.; Dobson, A.J.; Brown, W.J.; Bryson, L.; Byles, J.; Warner-Smith, P.; Young, A.F. Cohort Profile: The Australian Longitudinal Study on Women’s Health. Int. J. Epidemiol. 2005, 34, 987–991. [Google Scholar] [CrossRef]
- Dobson, A.J.; Hockey, R.; Brown, W.J.; Byles, J.E.; Loxton, D.J.; McLaughlin, D.; Tooth, L.R.; Mishra, G.D. Cohort Profile Update: Australian Longitudinal Study on Women’s Health. Int. J. Epidemiol. 2015, 44, 1547–1547f. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Armstrong, T.; Bauman, A.E.; Davies, J. Physical Activity Patterns of Australian Adults: Results of the 1999 National Physical Activity Survey; Australian Institute of Health and Welfare: Canberra, Australia, 2000. Available online: https://www.aihw.gov.au/reports/physical-activity/physical-activity-patterns-of-australian-adults/contents/table-of-contents (accessed on 1 December 2020).
- Dorney, E.; Black, K. Preconception Care. Aust. J. Gen. Pract. 2018, 47, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Hodge, A.; Patterson, A.J.; Brown, W.J.; Ireland, P.; Giles, G. The Anti Cancer Council of Victoria FFQ: Relative Validity of Nutrient Intakes Compared with Weighed Food Records in Young to Middle-Aged Women in a Study of Iron Supplementation. Aust. N. Z. J. Public Health 2000, 24, 576–583. [Google Scholar] [CrossRef] [PubMed]
- McNaughton, S.A.; Ball, K.; Crawford, D.; Mishra, G.D. An Index of Diet and Eating Patterns is a Valid Measure of Diet Quality in an Australian Population. J. Nutr. 2008, 138, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Kellett, E.; Smith, A.; Schmerlaib, Y. The Australian Guide to Healthy Eating; Commonwealth Department of Health and Family Services: Canberra, Australia, 1998.
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for Depression in Well Older Adults: Evaluation of a Short Form of the CES-D. Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Taft, A.J.; Watson, L.F. Depression and Termination of Pregnancy (Induced Abortion) in a National Cohort of Young Australian Women: The Confounding Effect of Women’s Experience of Violence. BMC Public Health 2008, 8, 75. [Google Scholar] [CrossRef]
- Bell, S.; Lee, C. Development of the Perceived Stress Questionnaire for Young Women. Psychol. Health Med. 2002, 7, 189–201. [Google Scholar] [CrossRef]
- Green-Raleigh, K.; Lawrence, J.M.; Chen, H.; Devine, O.; Prue, C. Pregnancy Planning Status and Health Behaviors Among Nonpregnant Women in a California Managed Health Care Organization. Perspect Sex. Reprod. Health 2005, 37, 179–183. [Google Scholar] [CrossRef]
- Chuang, C.H.; Hillemeier, M.M.; Dyer, A.-M.; Weisman, C.S. The Relationship Between Pregnancy Intention and Preconception Health Behaviors. Prev. Med. 2011, 53, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.; Kandel, P.; Hill, B.; Hills, S.; Dunbar, J.; Skouteris, H. Practice Nurses and Providing Preconception Care to Women in Australia: A Qualitative Study. Aust. J. Prim. Health 2020. [Google Scholar] [CrossRef] [PubMed]
- The Royal Australian College of General Practitioners. Guidelines for Preventive Activities in General Practice; The Royal Australian College of General Practitioners: East Melbourne, Austrilia, 2016. [Google Scholar]
- McPhie, S.; Skouteris, H.; Millar, L.; Olsson, C.; Campbell, K.; van der Pligt, P.; Dodd, J.; Hill, B. Preconception Weight Management: An Untapped Area of Women’s Health. Aust. J. Prim. Health 2017, 23, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.; Bergmeier, H.; McPhie, S.; Fuller-Tyszkiewicz, M.; Teede, H.; Forster, D.; Spiliotis, B.E.; Hills, A.P.; Skouteris, H. Is Parity a Risk Factor for Excessive Weight Gain During Pregnancy and Postpartum Weight Retention? A Systematic Review and Meta-Analysis. Obes. Rev. 2017, 18, 755–764. [Google Scholar] [CrossRef]
- Hillemeier, M.M.; Weisman, C.S.; Chuang, C.; Downs, D.S.; McCall-Hosenfeld, J.; Camacho, F. Transition to Overweight or Obesity Among Women of Reproductive Age. J. Women’s Health (2002) 2011, 20, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Corder, K.; Winpenny, E.M.; Foubister, C.; Guagliano, J.M.; Hartwig, X.M.; Love, R.; Clifford Astbury, C.; van Sluijs, E.M.F. Becoming a Parent: A Systematic Review and Meta-Analysis of Changes in BMI, Diet, and Physical Activity. Obes. Rev. 2020, 21, e12959. [Google Scholar] [CrossRef]
- Menting, M.D.; Mintjens, S.; van de Beek, C.; Frick, C.J.; Ozanne, S.E.; Limpens, J.; Roseboom, T.J.; Hooijmans, C.R.; van Deutekom, A.W.; Painter, R.C. Maternal Obesity in Pregnancy Impacts Offspring Cardiometabolic Health: Systematic Review and Meta-Analysis of Animal Studies. Obes. Rev. 2019, 20, 675–685. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Insufficient Physical Activity; AIHW: Canberra, Australia, 2019. Available online: https://www.aihw.gov.au/reports/risk-factors/insufficient-physical-activity (accessed on 1 December 2020).
- National Health and Medical Research Council. Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013. Available online: https://www.health.gov.au/resources/publications/the-australian-dietary-guidelines (accessed on 1 December 2020).
- Department of Health. Australia’s Physical Activity and Sedentary Behaviour Guidelines; Australian Government: Canberra, Australia, 2014. Available online: https://www.health.gov.au/health-topics/exercise-and-physical-activity (accessed on 1 December 2020).
- Glanz, K.; Rimer, B.K.; Viswanath, K. (Eds.) Health Behaviour and Health Education: Theory, Research and Practice, 4th ed.; John Wiley & Sons, Inc.: San Francisco, CA, USA, 2008; ISBN 978-0-7879-9614-7. [Google Scholar]
- Hill, B. Expanding our Understanding and Use of the Ecological Systems Theory Model for the Prevention of Maternal Obesity: A New Socioecological Framework. Obes. Rev. 2020, 1–7. [Google Scholar] [CrossRef]
- Abajobir, A.A.; Maravilla, J.C.; Alati, R.; Najman, J.M. A Systematic Review and Meta-Analysis of the Association Between Unintended Pregnancy and Perinatal Depression. J. Affect. Disord. 2016, 192, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Lagadec, N.; Steinecker, M.; Kapassi, A.; Magnier, A.M.; Chastang, J.; Robert, S.; Gaouaou, N.; Ibanez, G. Factors Influencing the Quality of Life of Pregnant Women: A Systematic Review. BMC Pregnancy Childbirth 2018, 18, 455. [Google Scholar] [CrossRef]
- Underwood, L.; Waldie, K.E.; D’Souza, S.; Peterson, E.R.; Morton, S.M. A Longitudinal Study of Pre-pregnancy and Pregnancy Risk Factors Associated with Antenatal and Postnatal Symptoms of Depression: Evidence from Growing Up in New Zealand. Matern. Child Health J. 2017, 21, 915–931. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.; Hall, J.; Skouteris, H.; Currie, S. Defining Preconception: Exploring the Concept of a Preconception Population. BMC Pregnancy Childbirth 2020, 20, 280. [Google Scholar] [CrossRef] [PubMed]
- Bearak, J.; Popinchalk, A.; Alkema, L.; Sedgh, G. Global, Regional, and Subregional Trends in Unintended Pregnancy and its Outcomes from 1990 to 2014: Estimates from a Bayesian Hierarchical Model. Lancet Glob. Health 2018, 6, e380–e389. [Google Scholar] [CrossRef]
- Brown, W.J.; Kabir, E.; Clark, B.K.; Gomersall, S.R. Maintaining a Healthy BMI: Data From a 16-Year Study of Young Australian Women. Am. J. Prev. Med. 2016, 51, e165–e178. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total Sample N = 2203 | Aspiration N = 2097 | Reached Aspiration N = 106 | p-Value | |||
|---|---|---|---|---|---|---|---|
| Value n (%) or Mean (SD) | N | Value n (%) or Mean (SD) | N | Value n (%) or Mean (SD) | N | ||
| Age (years, continuous) | 27.5 (1.42) | 2203 | 27.4 (1.42) | 2097 | 27.9 (1.41) | 106 | <0.001 |
| Highest level of education | 2161 | 2055 | 106 | ||||
| No formal education/high school | 378 (17.5) | 353 (17.2) | 25 (23.6) | 0.234 | |||
| Trade/diploma | 501(23.2) | 479 (23.3) | 22 (20.7) | ||||
| Degree | 1282 (59.3) | 1223 (59.5) | 59 (55.7) | ||||
| Country of birth | 2190 | 2084 | 106 | ||||
| Australian born | 2022 (92.3) | 1929 (92.6) | 93 (87.7) | 0.111 | |||
| Other English-speaking background | 96 (4.4) | 90 (4.3) | 6 (5.7) | ||||
| Other, Asia Europe | 72 (3.3) | 65 (3.1) | 7 (6.6) | ||||
| Average household income (AUD) | 1854 | 1779 | 75 | ||||
| <$26,000 | 78 (4.2) | 75 (4.2) | 3 (4.0) | 0.483 | |||
| $26,000 to $77,999 | 839 (45.2) | 800 (44.9) | 39 (52.0) | ||||
| ≥$78,000 | 973 (50.5) | 904 (50.8) | 33 (44.0) | ||||
| Employment | 2089 | 1987 | 102 | ||||
| No Paid work | 126 (6.0) | 121(6.1) | 5 (4.9) | 0.623 | |||
| Paid work | 1963 (94.0) | 1866 (93.9) | 97 (95.1) | ||||
| Marital status | 2198 | 2092 | 106 | ||||
| Not married or de facto | 769 (35.0) | 711 (34.0) | 58 (54.7) | <0.001 | |||
| Married or de facto | 1429 (65.0) | 1381 (66.0) | 48 (45.3) | ||||
| Gravidity | 2203 | 2097 | 106 | ||||
| None | 2048 (92.9) | 1945 (92.7) | 103 (97.2) | 0.083 | |||
| One and above | 155 (7) | 152 (7.2) | 3 (2.8) | ||||
| Body Mass Index | 2141 | 2036 | 105 | ||||
| Underweight | 85 (4.0) | 81 (4.0) | 4 (3.8) | 0.301 | |||
| Normal | 1448 (67.6) | 1381 (67.8) | 67 (63.8) | ||||
| Overweight | 414 (19.3) | 395 (19.4) | 19 (18.1) | ||||
| Obese | 194 (9.1) | 179 (8.8) | 15 (14.3) | ||||
| Physical activity | 2191 | 2085 | 106 | ||||
| Sedentary (<40 metmins) | 131 (6.0) | 122 (5.8) | 9 (8.5) | 0.488 | |||
| Low (41–600 metmins) | 772 (35.2) | 739 (35.4) | 33 (33.1) | ||||
| Moderate (601–1200 metmins) | 546 (24.9) | 522 (25.0) | 24 (22.6) | ||||
| High (>1201 metmins) | 742 (33.9) | 702 (33.7) | 40 (37.7) | ||||
| Diet quality (DGI score, continuous) | 78.1 (10.8) | 2178 | 78 (10.8) | 2074 | 78.9 (10.9) | 104 | 0.399 |
| Sedentary behaviour (hours, continuous) | 6.6 (2.7) | 2107 | 6.6 (2.7) | 2006 | 6.6 (2.9) | 101 | 0.964 |
| Alcohol intake | 2198 | 2092 | 106 | ||||
| Never | 107 (4.9) | 98 (4.7) | 9 (8.5) | 0.076 | |||
| Any | 2091 (95.1) | 1994 (95.3) | 97 (91.5) | ||||
| Smoking status | 2194 | 2088 | 106 | ||||
| Never or ex-smoker | 1795 (81.8) | 1711 (81.9) | 84 (79.2) | 0.482 | |||
| Current smoker | 399 (18.2) | 377 (18.1) | 22 (20.7) | ||||
| Depressive symptoms | 2176 | 2071 | 105 | ||||
| No | 1760 (80.9) | 1681 (81.2) | 79 (75.2) | 0.132 | |||
| Yes | 416 (19.1) | 390 (18.8) | 26 (24.8) | ||||
| Anxiety symptoms | 2196 | 2090 | 106 | ||||
| No | 1109 (50.5) | 1055 (50.5) | 54 (50.9) | 0.926 | |||
| Yes | 1087 (49.5) | 1035 (49.5) | 52 (49.1) | ||||
| Stress (score, continuous) | 0.82 (0.48) | 2199 | 0.82 (0.47) | 2094 | 0.87 (0.59) | 105 | 0.363 |
| Variable | Bivariable | Multivariable | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | AOR | 95% CI | p-Value | |
| Age (continuous) | 0.8 | 0.69–0.91 | 0.001 | 0.7 | 0.60–0.88 | 0.001 |
| Education | ||||||
| No formal/high school | 1 | 1 | ||||
| Trade/diploma | 1.5 | 0.86–2.78 | 0.150 | 0.9 | 0.39–2.11 | 0.823 |
| Degree | 1.5 | 0.91–2.38 | 0.119 | 1.1 | 0.51–0.81 | 0.808 |
| Employment status | ||||||
| No paid work | 1.0 | 1.0 | ||||
| Paid work | 0.8 | 0.32–1.99 | 0.624 | 0.7 | 0.16–3.0 | 0.623 |
| Annual household income (AUD$) | ||||||
| <$25,999 | 1.0 | 1.0 | ||||
| $26,000–$77,999 | 0.8 | 0.25–2.72 | 0.746 | 0.7 | 0.16–3.31 | 0.690 |
| ≥$78,000 | 1.1 | 0.33–3.66 | 0.882 | 0.8 | 0.18–3.90 | 0.822 |
| Marital Status | ||||||
| Not married or de facto | 1.0 | 1.0 | ||||
| Married or de facto | 2.3 | 1.58–3.48 | <0.001 | 2.6 | 1.50–4.42 | 0.001 |
| Gravidity | ||||||
| None | 1.0 | 1.0 | ||||
| One and above | 2.7 | 0.84–2.56 | 0.095 | 4.5 | 0.59–34.99 | 0.146 |
| BMI Category | ||||||
| Underweight | 1.0 | 0.35–2.76 | 0.973 | 1.0 | 0.24–4.58 | 0.950 |
| Normal weight | 1.0 | 1.0 | ||||
| Overweight | 1.0 | 0.60–1.70 | 0.974 | 0.8 | 0.44–1.60 | 0.598 |
| Obese | 0.6 | 0.32–1.04 | 0.065 | 0.4 | 0.20–0.89 | 0.024 |
| Physical activity | ||||||
| Sedentary (<40 metmins) | 1.0 | 1.0 | ||||
| Low (41–600 metmins | 1.7 | 0.77–3.54 | 0.196 | 1.3 | 0.42–4.0 | 0.661 |
| Moderate (601–1200 metmins) | 1.6 | 0.73–3.54 | 0.241 | 1.3 | 0.39–4.23 | 0.679 |
| High (>1201 metmins) | 1.3 | 0.61–2.74 | 0.499 | 0.8 | 0.27–2.63 | 0.771 |
| Sedentary behaviour (sitting time) (continuous) | 1.0 | 0.93–1.08 | 0.964 | 1.0 | 0.89–1.08 | 0.672 |
| Diet quality (continuous) | 1.0 | 0.97–1.01 | 0.399 | 1.0 | 0.97–1.01 | 0.390 |
| Alcohol intake | ||||||
| None | 1.0 | 1.0 | ||||
| Any | 1.9 | 0.93–3.85 | 0.080 | 2.6 | 0.99–6.63 | 0.051 |
| Smoking | ||||||
| Never or ex-smoker | 1.0 | 1.0 | ||||
| Current smoker | 0.8 | 0.52–1.36 | 0.483 | 1.0 | 0.50–2.00 | 0.995 |
| Depressive symptoms, Yes | 0.7 | 0.45–1.11 | 0.133 | 0.7 | 0.35–1.57 | 0.423 |
| Anxiety symptoms, Yes | 1.0 | 0.69–1.51 | 0.926 | 1.2 | 0.68–2.28 | 0.478 |
| Stress (continuous) | 0.8 | 0.56–1.23 | 0.363 | 1.1 | 0.55–2.05 | 0.859 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hill, B.; Awoke, M.A.; Bergmeier, H.; Moran, L.J.; Mishra, G.D.; Skouteris, H. Lifestyle and Psychological Factors of Women with Pregnancy Intentions Who Become Pregnant: Analysis of a Longitudinal Cohort of Australian Women. J. Clin. Med. 2021, 10, 725. https://doi.org/10.3390/jcm10040725
Hill B, Awoke MA, Bergmeier H, Moran LJ, Mishra GD, Skouteris H. Lifestyle and Psychological Factors of Women with Pregnancy Intentions Who Become Pregnant: Analysis of a Longitudinal Cohort of Australian Women. Journal of Clinical Medicine. 2021; 10(4):725. https://doi.org/10.3390/jcm10040725
Chicago/Turabian StyleHill, Briony, Mamaru A. Awoke, Heidi Bergmeier, Lisa J. Moran, Gita D. Mishra, and Helen Skouteris. 2021. "Lifestyle and Psychological Factors of Women with Pregnancy Intentions Who Become Pregnant: Analysis of a Longitudinal Cohort of Australian Women" Journal of Clinical Medicine 10, no. 4: 725. https://doi.org/10.3390/jcm10040725
APA StyleHill, B., Awoke, M. A., Bergmeier, H., Moran, L. J., Mishra, G. D., & Skouteris, H. (2021). Lifestyle and Psychological Factors of Women with Pregnancy Intentions Who Become Pregnant: Analysis of a Longitudinal Cohort of Australian Women. Journal of Clinical Medicine, 10(4), 725. https://doi.org/10.3390/jcm10040725








