Differences in the Clinical Picture in Women with a Depressive Episode in the Course of Unipolar and Bipolar Disorder
Abstract
1. Introduction
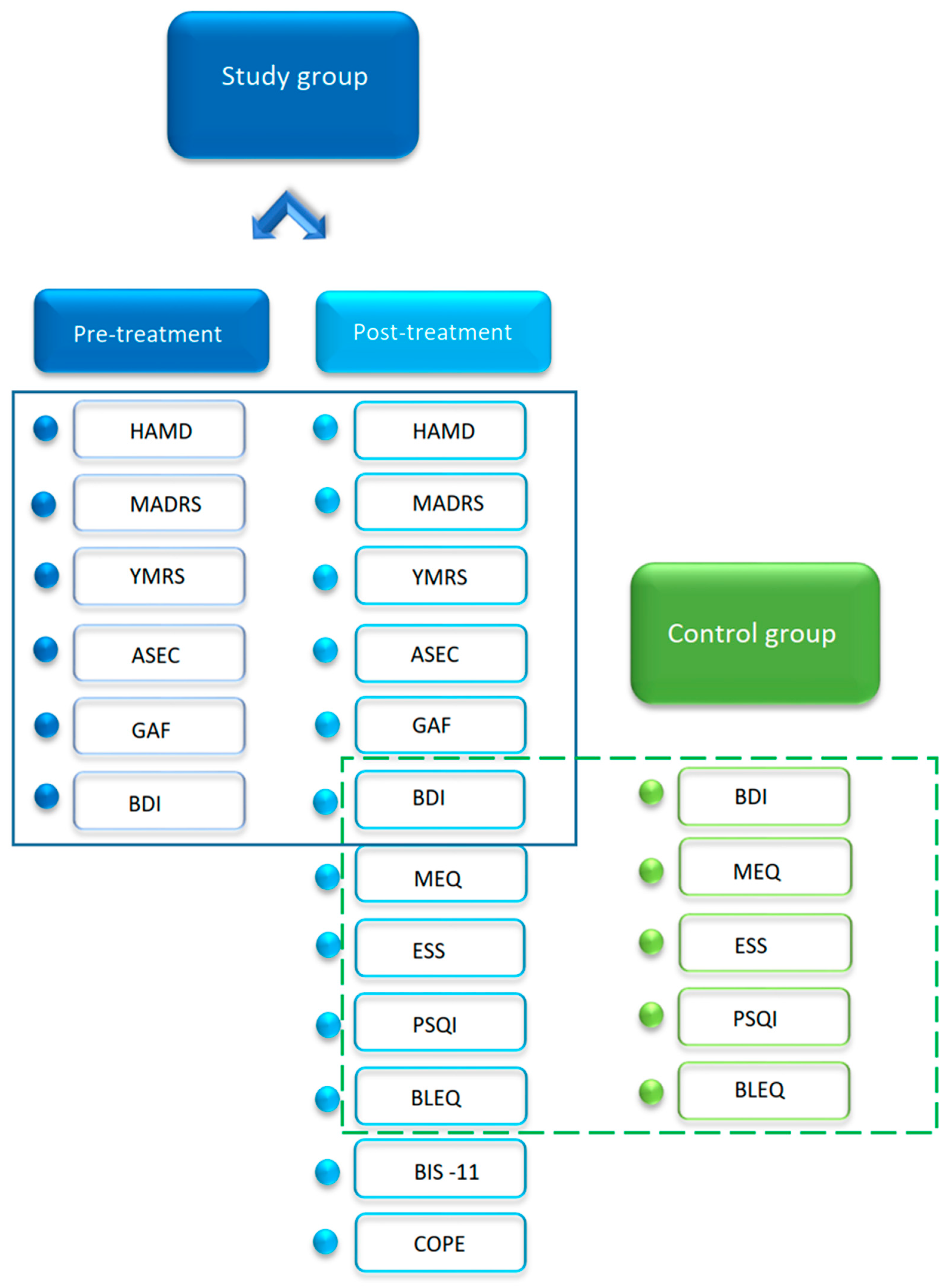
2. Materials and Methods
2.1. Participants
2.2. Statistical Analyses
3. Results
3.1. Sample Characteristics Including Social Status and Basic Clinical Data
3.2. Depressive Symptoms Severity in the Pre- and Post-Treatment State
3.3. Analysis the Group of Medications Taken in the Pre- and Post-Treatment State
3.4. Assessment of Global Functioning in the Pre- and Post-Treatment State
3.5. Laboratory Findings
3.6. Sleep Quality and Chronotype Analysis in BP, UP and CG
3.7. Impulsivity Assessment in BP and UP
3.8. Stressful Life Events before the Relapse
3.9. Coping with Stress Assessment in BP and UP in Comparison to Literature CG
3.10. Antidepressant Side-Effect Before and After Treatment
4. Discussion
4.1. BP Patients Struggle More with Social Relationships Than UP Subjects
4.2. Evening Chronotype and Daytime Difficulties Are Common
4.3. BP Patients Are More Impulsive Than UP Subjects
4.4. Relationship Problems Are More Likely to Trigger Episode in BP, Whereas UP Patients More Often Have a Relapse after Bereavement
4.5. Affective Disorder Patients Use Behavioral Disengagement Strategy
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Depression and Other Common Mental Disorders: Global Health Estimates; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Ozcelik, M.; Sahbaz, C. Clinical Evaluation of Biological Rhythm Domains in Patients with Major Depression. Braz. J. Psychiatry 2020, 42, 258–263. [Google Scholar] [CrossRef]
- Blairy, S.; Linotte, S.; Souery, D.; Papadimitriou, G.N.; Dikeos, D.; Lerer, B.; Kaneva, R.; Milanova, V.; Serretti, A.; Mendlewicz, J.; et al. Social Adjustment and Self-Esteem of Bipolar Patients: A Multicentric Study. J. Affect. Disord. 2004, 79, 97–103. [Google Scholar] [CrossRef]
- Yatham, L.N.; Lecrubier, Y.; Fieve, R.R.; Davis, K.H.; Harris, S.D.; Krishnan, A.A. Quality of Life in Patients with Bipolar I Depression: Data from 920 Patients. Bipolar Disord. 2004, 6, 379–385. [Google Scholar] [CrossRef]
- Elgie, R.; Morselli, P.L. Social Functioning in Bipolar Patients: The Perception and Perspective of Patients, Relatives and Advocacy Organizations—A Review. Bipolar Disord. 2007, 9, 144–157. [Google Scholar] [CrossRef]
- Ghaemi, S.N.; Boiman, E.E.; Goodwin, F.K. Diagnosing Bipolar Disorder and the Effect of Antidepressants: A Naturalistic Study. J. Clin. Psychiatry 2000, 61, 804–808. [Google Scholar] [CrossRef]
- Lish, J.D.; Dime-Meenan, S.; Whybrow, P.C.; Price, R.A.; Hirschfeld, R.M. The National Depressive and Manic-Depressive Association (Dmda) Survey of Bipolar Members. J. Affect. Disord. 1994, 31, 281–294. [Google Scholar] [CrossRef]
- Goldberg, J.F. The Economic and Social Burden of Bipolar Disorder: A Review; Copyright John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2002; Volume 5, pp. 441–501. [Google Scholar]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime Prevalence and Age-of-Onset Distributions of Dsm-Iv Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Forty, L.; Smith, D.; Jones, L.; Jones, I.; Caesar, S.; Cooper, C.; Fraser, C.; Gordon-Smith, K.; Hyde, S.; Craddock, N.; et al. Clinical Differences between Bipolar and Unipolar Depression. Br. J. Psychiatry 2008, 192, 388–389. [Google Scholar] [CrossRef]
- Angst, J.; Cui, L.; Swendsen, J.; Rothen, S.; Cravchik, A.; Kessler, R.C.; Merikangas, K.R. Major Depressive Disorder with Subthreshold Bipolarity in the National Comorbidity Survey Replication. Am. J. Psychiatry 2010, 167, 1194–1201. [Google Scholar] [CrossRef]
- Zimmermann, P.; Bruckl, T.; Nocon, A.; Pfister, H.; Lieb, R.; Wittchen, H.U.; Holsboer, F.; Angst, J. Heterogeneity of Dsm-Iv Major Depressive Disorder as a Consequence of Subthreshold Bipolarity. Arch. Gen. Psychiatry 2009, 66, 1341–1352. [Google Scholar] [CrossRef] [PubMed]
- Suominen, K.; Mantere, O.; Valtonen, H.; Arvilommi, P.; Leppamaki, S.; Isometsa, E. Gender Differences in Bipolar Disorder Type I and Ii. Acta Psychiatr. Scand. 2009, 120, 464–473. [Google Scholar] [CrossRef]
- Essau, C.A.; Lewinsohn, P.M.; Seeley, J.R.; Sasagawa, S. Gender Differences in the Developmental Course of Depression. J. Affect. Disord. 2010, 127, 185–190. [Google Scholar] [CrossRef]
- Vega, P.; Barbeito, S.; Ruiz de Azua, S.; Martinez-Cengotitabengoa, M.; Gonzalez-Ortega, I.; Saenz, M.; Gonzalez-Pinto, A. Bipolar Disorder Differences between Genders: Special Considerations for Women. Womens Health 2011, 7, 663–674. [Google Scholar] [CrossRef]
- Labonte, B.; Engmann, O.; Purushothaman, I.; Menard, C.; Wang, J.; Tan, C.; Scarpa, J.R.; Moy, G.; Loh, Y.-H.; Nestler, E.J.; et al. Sex-Specific Transcriptional Signatures in Human Depression. Nat. Med. 2017, 23, 1102–1111. [Google Scholar] [CrossRef]
- APA. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), 4th ed.; APA: Washington, DC, USA, 2000. [Google Scholar]
- First, M.B.; Spitzer, R.L.; Gibbon, M. Structured Clinical Interview for DSM-IV-Tr Axis I Disorders, Clinical Trials Version (SCID-Ct); New York State Psychiatric Institute, Biometrics Research: New York, NY, USA, 2007. [Google Scholar]
- Craddock, M.; Asherson, P.; Owen, M.J.; Williams, J.; McGuffin, P.; Farmer, A.E. Concurrent Validity of the Opcrit Diagnostic System. Comparison of Opcrit Diagnoses with Consensus Best-Estimate Lifetime Diagnoses. Br. J. Psychiatry 1996, 169, 58–63. [Google Scholar] [CrossRef]
- Hamilton, M. A Rating Scale for Depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, S.A.; Asberg, M. A New Depression Scale Designed to Be Sensitive to Change. Br. J. Psychiatry 1979, 134, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Young, R.C.; Biggs, J.T.; Ziegler, V.E.; Meyer, D.A. A Rating Scale for Mania: Reliability, Validity and Sensitivity. Br. J. Psychiatry 1978, 133, 429–435. [Google Scholar] [CrossRef]
- Uher, R.; Farmer, A.; Henigsberg, N.; Rietschel, M.; Mors, O.; Maier, W.; Kozel, D.; Hauser, J.; Souery, D.; Aitchison, K.J.; et al. Adverse Reactions to Antidepressants. Br. J. Psychiatry 2009, 195, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Earley, W.; Durgam, S.; Lu, K.; Ruth, A.; Nemeth, G.; Laszlovszky, I.; Yatham, L.N. Clinically Relevant Response and Remission Outcomes in Cariprazine-Treated Patients with Bipolar I Disorder. J. Affect. Disord. 2018, 226, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An Inventory for Measuring Depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Lopuszanska, M.; Szklarska, A.; Jankowska, E.A. Assessment of Severity of Depressive Symptoms Using the Polish Version Ia of Beck Depression Inventory in Healthy Men, Inhabitants of Wroclaw. Psychiatr. Pol. 2013, 47, 1001–1009. [Google Scholar] [PubMed]
- Patton, J.H.; Stanford, M.S.; Barratt, E.S. Factor Structure of the Barratt Impulsiveness Scale. J. Clin. Psychol. 1995, 51, 768–774. [Google Scholar] [CrossRef]
- Horne, J.A.; Ostberg, O. A Self-Assessment Questionnaire to Determine Morningness-Eveningness in Human Circadian Rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar] [PubMed]
- Pracki, T.W.M.; Pracka, D.; Dmitrzak-Węglarz, M.; Augustyńska, B. Measuring the Chronotype in Polish Population. Med. Biol. Sci. 2014, 28, 47–53. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Johns, M.W. A New Method for Measuring Daytime Sleepiness: The Epworth Sleepiness Scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing Coping Strategies: A Theoretically Based Approach. J. Pers. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef] [PubMed]
- Juczyński, Z.; Ogińska-Bulik, N. COPE—Wielowymiarowy Inwentarz Do Pomiaru Radzenia Sobie Ze Stresem; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2009. [Google Scholar]
- Brugha, T.; Bebbington, P.; Tennant, C.; Hurry, J. The List of Threatening Experiences: A Subset of 12 Life Event Categories with Considerable Long-Term Contextual Threat. Psychol. Med. 1985, 15, 189–194. [Google Scholar] [CrossRef]
- Bech, P. Rating Scales in Depression: Limitations and Pitfalls. Dialogues Clin. Neurosci. 2006, 8, 207–215. [Google Scholar]
- Maust, D.; Cristancho, M.; Gray, L.; Rushing, S.; Tjoa, C.; Thase, M.E. Psychiatric Rating Scales. Handb. Clin. Neurol. 2012, 106, 227–237. [Google Scholar]
- Stanford, M.S.; Dougherty, D.M.; Lake, S.L.; Anderson, N.E.; Patton, J.H. Fifty Years of the Barratt Impulsiveness Scale: An Update and Review. Personal. Individ. Differ. 2009, 47, 385–395. [Google Scholar] [CrossRef]
- Juczyński, Z.; Ogińska-Bulik, N. Narzędzia Pomiaru Stresu I Radzenia Sobie Ze Stresem; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2012. [Google Scholar]
- Walid, M.S. Which Neuropsychiatric Disorder Is More Associated with Divorce? J. Divorce Remarriage 2011, 52, 220–224. [Google Scholar] [CrossRef]
- Morselli, P.L.; Elgie, R.; Cesana, B.M. Gamian-Europe/Beam Survey Ii: Cross-National Analysis of Unemployment, Family History, Treatment Satisfaction and Impact of the Bipolar Disorder on Life Style. Bipolar Disord. 2004, 6, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, J.F.; Harrow, M. Consistency of Remission and Outcome in Bipolar and Unipolar Mood Disorders: A 10-Year Prospective Follow-Up. J. Affect. Disord. 2004, 81, 123–131. [Google Scholar] [CrossRef]
- Goldberg, J.F.; Harrow, M. A 15-Year Prospective Follow-up of Bipolar Affective Disorders: Comparisons with Unipolar Nonpsychotic Depression. Bipolar Disord. 2011, 13, 155–163. [Google Scholar] [CrossRef]
- Shippee, N.D.; Shah, N.D.; Williams, M.D.; Moriarty, J.P.; Frye, M.A.; Ziegenfuss, J.Y. Differences in Demographic Composition and in Work, Social, and Functional Limitations among the Populations with Unipolar Depression and Bipolar Disorder: Results from a Nationally Representative Sample. Health Qual. Life Outcomes 2011, 9, 90. [Google Scholar] [CrossRef] [PubMed]
- Glahn, D.C.; Bearden, C.E.; Bowden, C.L.; Soares, J.C. Reduced Educational Attainment in Bipolar Disorder. J. Affect. Disord. 2006, 92, 309–312. [Google Scholar] [CrossRef]
- Dmitrzak-Weglarz, M.; Pawlak, J.; Wilkosc, M.; Miechowicz, I.; Maciukiewicz, M.; Ciarkowska, W.; Zaremba, D.; Hauser, J. Chronotype and Sleep Quality as a Subphenotype in Association Studies of Clock Genes in Mood Disorders. Acta Neurobiol. Exp. 2016, 76, 32–42. [Google Scholar] [CrossRef]
- Mume, C.O. Excessive Daytime Sleepiness among Depressed Patients. Libyan J. Med. 2010, 5, 4626. [Google Scholar] [CrossRef]
- Peluso, M.A.; Hatch, J.P.; Glahn, D.C.; Monkul, E.S.; Sanches, M.; Najt, P.; Bowden, C.L.; Barratt, E.S.; Soares, J.C. Trait Impulsivity in Patients with Mood Disorders. J. Affect. Disord. 2007, 100, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, J.; Busch, K.A.; Jacobs, D.; Kravitz, H.M.; Fogg, L. Suicide: A Four-Pathway Clinical-Biochemical Model. Ann. N. Y. Acad. Sci. 1997, 836, 288–301. [Google Scholar] [CrossRef]
- Allen, T.J.; Moeller, F.G.; Rhoades, H.M.; Cherek, D.R. Impulsivity and History of Drug Dependence. Drug Alcohol Depend. 1998, 50, 137–145. [Google Scholar] [CrossRef]
- Swann, A.C.; Dougherty, D.M.; Pazzaglia, P.J.; Pham, M.; Moeller, F.G. Impulsivity: A Link between Bipolar Disorder and Substance Abuse. Bipolar Disord. 2004, 6, 204–212. [Google Scholar] [CrossRef]
- Ozten, M.; Erol, A. Impulsivity Differences between Bipolar and Unipolar Depression. Indian J. Psychiatry 2019, 61, 156–160. [Google Scholar]
- Hosang, G.M.; Korszun, A.; Jones, L.; Jones, I.; McGuffin, P.; Farmer, A.E. Life-Event Specificity: Bipolar Disorder Compared with Unipolar Depression. Br. J. Psychiatry 2012, 201, 458–465. [Google Scholar] [CrossRef]
- Engel-Yeger, B.; Gonda, X.; Muzio, C.; Rinosi, G.; Pompili, M.; Amore, M.; Serafini, G. Sensory Processing Patterns, Coping Strategies, and Quality of Life among Patients with Unipolar and Bipolar Disorders. Braz. J. Psychiatry 2016, 38, 207–215. [Google Scholar] [CrossRef]
- Coulston, C.M.; Bargh, D.M.; Tanious, M.; Cashman, E.L.; Tufrey, K.; Curran, G.; Kuiper, S.; Morgan, H.; Lampe, L.; Malhi, G.S. Is Coping Well a Matter of Personality? A Study of Euthymic Unipolar and Bipolar Patients. J. Affect. Disord. 2013, 145, 54–61. [Google Scholar] [CrossRef]
- Fletcher, K.; Parker, G.B.; Manicavasagar, V. Coping Profiles in Bipolar Disorder. Compr. Psychiatry 2013, 54, 1177–1184. [Google Scholar] [CrossRef]
- Arnold, L.M. Gender Differences in Bipolar Disorder. Psychiatr. Clin. N. Am. 2003, 26, 595–620. [Google Scholar] [CrossRef]
- Azorin, J.M.; Belzeaux, R.; Kaladjian, A.; Adida, M.; Hantouche, E.; Lancrenon, S.; Fakra, E. Risks Associated with Gender Differences in Bipolar I Disorder. J. Affect. Disord. 2013, 151, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Study Group | Control Group | p-Value | BP | UP | p-Value |
|---|---|---|---|---|---|---|
| Female, N | 79 | 67 | 0.3206 ƚ | 43 | 34 | 0.3051 ƚ |
| Age, years: mean [SD] | 42.23 [15.06] | 42.46 [11.41] | 0.8599 | 41.33 [14.24] | 43.31 [16.12] | 0.6226 |
| Education, years: mean [SD] | 13.65 [2.78] | 15.81 [2.15] | <0.0001 | 13.39 [2.84] | 13.97 [2.71] | 0.2969 |
| Marital status, N [%] | ||||||
| single | 25 [34.24] | 17 [25.37] | 0.2170 ƚ | 15 [37.50] | 10 [30.30] | 0.3173 ƚ |
| married | 30 [41.10] | 47 [68.66] | 0.0527 ƚ | 13 [32.50] | 17 [51.51] | 0.4652 ƚ |
| divorced | 13 [17.81] | 3 [4.48] | 0.0124 ƚ | 10 [25.00] | 3 [9.09] | 0.0522 ƚ |
| widow | 5 [6.85] | 1 [1.49] | 0.1025 ƚ | 2 [5.00] | 3 [9.09] | 0.6547 ƚ |
| Occupation before disorder, N [%] | ||||||
| employed | 30 [75.00] | 20 [64.52] | 0.1573 ƚ | |||
| unemployed | 10 [25.00] | 11 [35.48] | 0.8273 ƚ | |||
| Current occupation, N [%] | ||||||
| employed (full or part-time work) | 27 [37.50] | 65 [97.01] | <0.0001 ƚ | 12 [30.00] | 15 [46.87] | 0.5637 ƚ |
| student | 11 [15.28] | 0 [0] | 0.0009 ƚ | 7 [17.50] | 4 [12.50] | 0.3657 ƚ |
| unemployed or disable (including ‘retired’) | 34 [47.22] | 2 [2.99] | 0.0001 ƚ | 21 [52.50] | 13 [40.63] | 0.1701 ƚ |
| Family history of psychiatric disorders, N [%] | 50 [67.57] | 0 [0] | <0.0001 ƚ | 32 [78.05] | 18 [54.55] | 0.0477 ƚ |
| Age of onset: mean [SD]) | 28 [9.60] | 35 [14.8] | 0.0295 | |||
| Duration of hospitalization, weeks: mean [SD] | 7.20 [3.68] | 5.7 [2.18] | 0.1603 | |||
| Number of hospitalizations: mean [SD] | 5.60 [7.57] | 2.00 [2.26] | 0.0004 |
| Measure | Bipolar Disorder | Unipolar Disorder | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Treatment | Post-Treatment | p-Value | Pre-Treatment | Post-Treatment | p-Value | |||||
| Mean | SD | Mean | SD | Wilcoxon Test | Mean | SD | Mean | SD | Wilcoxon Test | |
| Hamilton Rating Scale for Depression–17 | 26.03 | 8.23 | 3.39 | 2.42 | <0.0001 | 25.51 | 6.10 | 3.85 | 3.09 | <0.0001 |
| Montgomery-Asberg Depression Rating Scale | 28.53 | 6.37 | 4.82 | 4.08 | 0.0003 | 31.80 | 6.73 | 3.80 | 3.16 | 0.0051 |
| Young Mania Rating Scale | 1.39 | 1.86 | 0.29 | 0.90 | 0.0029 | 0.93 | 1.62 | 0.03 | 0.19 | 0.0077 |
| Global Assessment of Functioning scale | 46.64 | 9.72 | 76.50 | 9.32 | 0.0010 | 46.89 | 14.12 | 79.00 | 4.90 | 0.0077 |
| Number of psychotropic medications taken | 4.45 | 2.05 | 5.39 | 2.91 | 0.0058 | 3.32 | 2.15 | 4.71 | 2.97 | 0.0019 |
| Beck Depression Inventory | 35.39 | 8.64 | 8.82 | 8.56 | <0.0001 | 31.04 | 13.41 | 10.73 | 10.35 | <0.0001 |
| Compared Groups | Control Group | Bipolar Patients | Unipolar Patients | p-Value of Kruskal–Wallis Test | Post-Hoc Dunn Test p- and z-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Mean | SD | Mean | SD | Mean | SD | CG vs. BP | CG vs. UP | BP vs. UP | ||
| Sleep duration | 0.6269 | 0.8499 | 0.2222 | 0.5774 | 0.1481 | 0.6015 | 0.0008 | 0.1059 | 0.0244 | 1.0000 | |
| (2.1050) | (2.6470) | (0.4539) | |||||||||
| Sleep disturbances | 0.8955 | 0.4650 | 1.0769 | 0.3922 | 1.0370 | 0.1925 | 0.0899 | 0.6338 | 0.9445 | 1.0000 | |
| (1.2501) | (1.0051) | (0.2173) | |||||||||
| Sleep latency | 0.7761 | 0.7349 | 1.3333 | 0.8771 | 1.7037 | 0.7753 | 0.0000 | 0.0246 | 0.0000 | 0.4468 | |
| (2.6437) | (4.3670) | (1.4433) | |||||||||
| Daytime dysfunction | 1.0000 | 0.5505 | 1.2400 | 1.0520 | 1.2963 | 0.8234 | 0.2492 | 1.0000 | 0.4527 | 1.0000 | |
| (0.7583) | (1.4364) | (0.5394) | |||||||||
| Habitual sleep efficiency | 0.3582 | 0.6898 | 0.4074 | 0.7971 | 0.6296 | 0.8389 | 0.1355 | 1.0000 | 0.3454 | 0.6475 | |
| (0.0977) | (1.5755) | (1.2377) | |||||||||
| Sleep quality | 0.8955 | 0.6064 | 0.7778 | 0.6405 | 1.0000 | 0.6794 | 0.4717 | 1.0000 | 1.0000 | 0.9061 | |
| (0.7081) | (0.5241) | (1.0321) | |||||||||
| Medicine-induced sleep | 0.2388 | 0.7196 | 1.0370 | 1.1923 | 1.5926 | 1.4212 | 0.0000 | 0.0134 | 0.0002 | 1.0000 | |
| (2.8422) | (3.9887) | (0.9603) | |||||||||
| PSQI | 4.7910 | 2.5198 | 6.1600 | 3.6019 | 7.4074 | 3.0415 | 0.0007 | 0.3160 | 0.0005 | 0.2626 | |
| (1.6195) | (3.7453) | (1.7085) | |||||||||
| Chronotyp | 1.9104 | 0.7330 | 1.6667 | 0.7338 | 1.4800 | 0.7141 | 0.0255 | 0.5132 | 0.0489 | 1.0000 | |
| (1.3687) | (2.4024) | (0.9044) | |||||||||
| ESS | 7.5970 | 3.0254 | 7.5556 | 4.2547 | 5.9167 | 4.4027 | 0.0890 | 1.0000 | 0.0941 | 0.2868 | |
| (0.1951) | (2.1523) | (1.6665) | |||||||||
| BP | Type of Questionnaire and Thematic Issues | HAMD | BDI | PSQI | ||||
|---|---|---|---|---|---|---|---|---|
| Intermittent, Shallow Sleep | Premature Waking Up | Premature Waking Up | Sleep Disturbances | Medicine Induced Sleep | Daytime Dysfunction | Total Score | ||
| OPCRIT | reduced need for sleep | −0.2877 | −0.0376 | 0.3238 | 0.0751 | 0.1119 | −0.1507 | 0.1268 |
| difficulty falling asleep | 0.4373 | −0.0234 | −0.0698 | −0.0652 | 0.1830 | −0.2387 | −0.0291 | |
| waking up at night | 0.4227 | 0.0384 | 0.0499 | −0.0602 | 0.0000 | −0.2169 | −0.2285 | |
| premature waking up | 0.2486 | 0.5411 | 0.4242 | 0.1780 | 0.0338 | −0.3745 | −0.0145 | |
| excessive sleepiness | −0.2509 | −0.2982 | −0.1462 | −0.2221 | −0.0192 | 0.4026 | −0.0702 | |
| UP | Type of Questionnaire and Thematic Issues | HAMD | BDI | PSQI | ||||
| Intermittent, Shallow Sleep | Premature Waking Up | Premature Waking Up | Sleep Disturbances | Medicine Induced Sleep | Daytime Dysfunction | Total Score | ||
| OPCRIT | reduced need for sleep | 0.1062 | −0.0262 | 0.0689 | 0.4703 | −0.1530 | 0.0072 | −0.1819 |
| difficulty falling asleep | 0.3887 | 0.1809 | 0.4259 | 0.1504 | 0.1363 | −0.2852 | 0.1197 | |
| waking up at night | 0.1916 | 0.1681 | 0.5965 | 0.0993 | 0.3362 | −0.1123 | 0.2333 | |
| premature waking up | 0.1648 | 0.5663 | 0.4524 | 0.2296 | 0.6643 | −0.2935 | 0.4936 | |
| excessive sleepiness | −0.1419 | 0.0090 | −0.0235 | 0.1248 | 0.3317 | 0.3850 | 0.1753 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bilska, K.; Pawlak, J.; Kapelski, P.; Narożna, B.; Zakowicz, P.; Szczepankiewicz, A.; Skibińska, M.; Dmitrzak-Węglarz, M. Differences in the Clinical Picture in Women with a Depressive Episode in the Course of Unipolar and Bipolar Disorder. J. Clin. Med. 2021, 10, 676. https://doi.org/10.3390/jcm10040676
Bilska K, Pawlak J, Kapelski P, Narożna B, Zakowicz P, Szczepankiewicz A, Skibińska M, Dmitrzak-Węglarz M. Differences in the Clinical Picture in Women with a Depressive Episode in the Course of Unipolar and Bipolar Disorder. Journal of Clinical Medicine. 2021; 10(4):676. https://doi.org/10.3390/jcm10040676
Chicago/Turabian StyleBilska, Karolina, Joanna Pawlak, Paweł Kapelski, Beata Narożna, Przemysław Zakowicz, Aleksandra Szczepankiewicz, Maria Skibińska, and Monika Dmitrzak-Węglarz. 2021. "Differences in the Clinical Picture in Women with a Depressive Episode in the Course of Unipolar and Bipolar Disorder" Journal of Clinical Medicine 10, no. 4: 676. https://doi.org/10.3390/jcm10040676
APA StyleBilska, K., Pawlak, J., Kapelski, P., Narożna, B., Zakowicz, P., Szczepankiewicz, A., Skibińska, M., & Dmitrzak-Węglarz, M. (2021). Differences in the Clinical Picture in Women with a Depressive Episode in the Course of Unipolar and Bipolar Disorder. Journal of Clinical Medicine, 10(4), 676. https://doi.org/10.3390/jcm10040676







