Leukocyte Immunoglobulin-Like Receptor A3 (LILRA3): A Novel Marker for Lymphoma Development among Patients with Young Onset Sjogren’s Syndrome
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Participants
2.2. DNA Extraction
2.3. Polymerase Chain Reaction (PCR)/LILRA3 Gene Polymorphisms
2.4. Enzyme-Linked Immunosorbent Assay (ELISA)
2.5. Statistical Analysis
3. Results
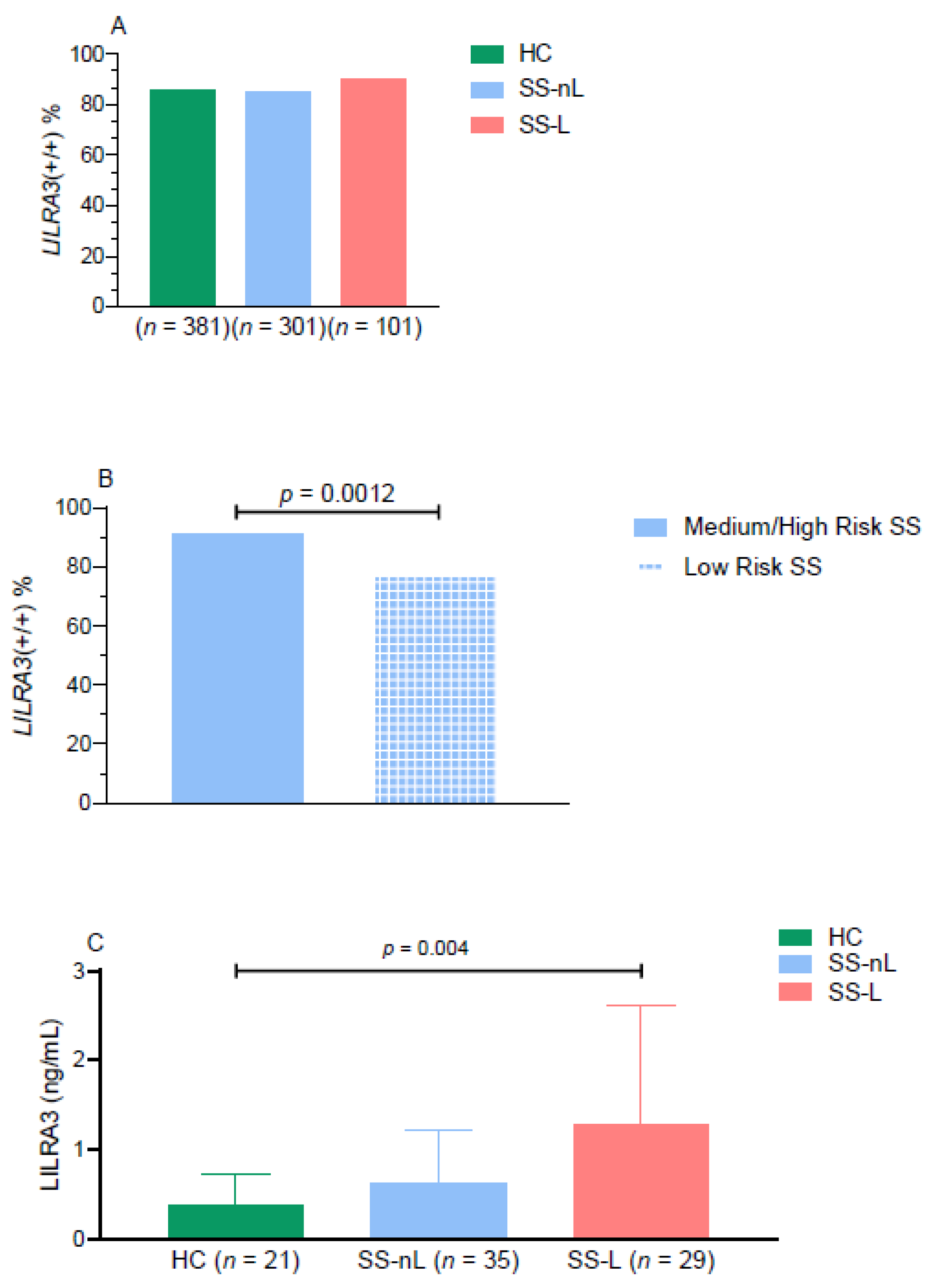
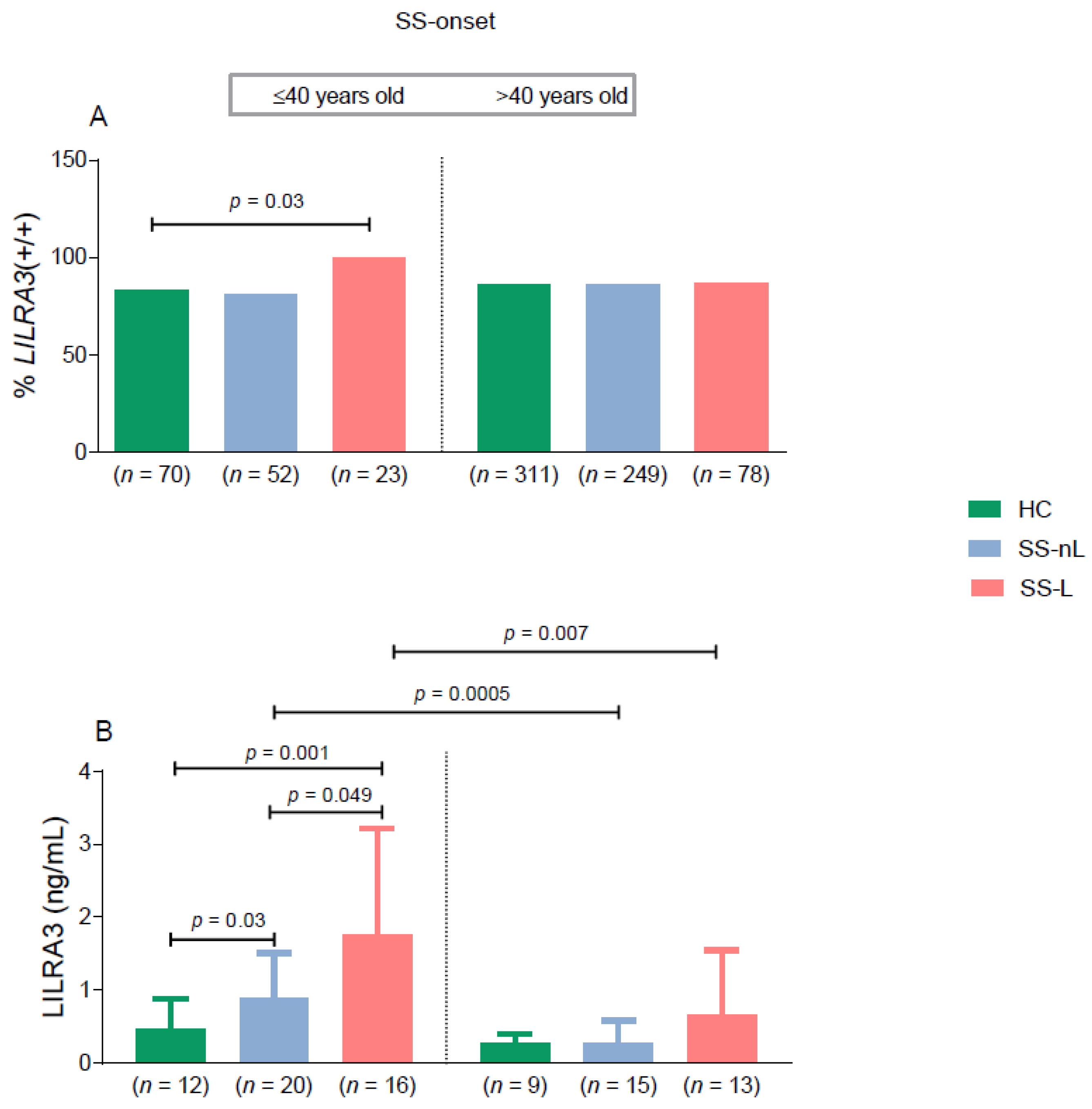
3.1. Prevalence of LILRA3 Genetic Variants in SS Patients and HC
3.2. LILRA3 Serum Protein Levels
3.3. LILRA3 Functional Variant-Clinical and Laboratory Associations
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Qin, B.; Wang, J.; Yang, Z.; Yang, M.; Ma, N.; Huang, F.; Zhong, R. Epidemiology of Primary Sjögren’s Syndrome: A Systematic Review and Meta-Analysis. Ann. Rheum. Dis. 2015, 74, 1983–1989. [Google Scholar] [CrossRef]
- Mavragani, C.P.; Moutsopoulos, H.M. Sjögren Syndrome. Can. Med. Assoc. J. 2014, 186, E579–E586. [Google Scholar] [CrossRef]
- Mavragani, C.P.; Moutsopoulos, H.M. The Geoepidemiology of Sjögren’s Syndrome. Autoimmun. Rev. 2010, 9, A305–A310. [Google Scholar] [CrossRef]
- Skopouli, F.N.; Dafni, U.; Ioannidis, J.P.; Moutsopoulos, H.M. Clinical Evolution, and Morbidity and Mortality of Primary Sjögren’s Syndrome. Semin. Arthritis Rheum. 2000, 29, 296–304. [Google Scholar] [CrossRef]
- Zintzaras, E.; Voulgarelis, M.; Moutsopoulos, H.M. The Risk of Lymphoma Development in Autoimmune Diseases: A Meta-Analysis. Arch. Intern. Med. 2005, 165, 2337–2344. [Google Scholar] [CrossRef] [PubMed]
- Skarlis, C.; Argyriou, E.; Mavragani, C.P. Lymphoma in Sjögren’s Syndrome: Predictors and Therapeutic Options. Curr. Treat. Options Rheumatol. 2020, 6, 1–17. [Google Scholar] [CrossRef]
- Goules, A.V.; Tzioufas, A.G. Lymphomagenesis in Sjögren’s Syndrome: Predictive Biomarkers towards Precision Medicine. Autoimmun. Rev. 2019, 18, 137–143. [Google Scholar] [CrossRef]
- Nezos, A.; Evangelopoulos, M.-E.; Mavragani, C.P. Genetic Contributors and Soluble Mediators in Prediction of Autoimmune Comorbidity. J. Autoimmun. 2019, 104, 102317. [Google Scholar] [CrossRef] [PubMed]
- Kabalak, G.; Dobberstein, S.B.; Matthias, T.; Reuter, S.; The, Y.-H.; Dörner, T.; Schmidt, R.E.; Witte, T. Association of Immunoglobulin-like Transcript 6 Deficiency with Sjögren’s Syndrome. Arthritis Rheum. 2009, 60, 2923–2925. [Google Scholar] [CrossRef] [PubMed]
- Low, H.Z.; Reuter, S.; Topperwien, M.; Dankenbrink, N.; Peest, D.; Kabalak, G.; Stripecke, R.; Schmidt, R.E.; Matthias, T.; Witte, T. Association of the LILRA3 Deletion with B-NHL and Functional Characterization of the Immunostimulatory Molecule. PLoS ONE 2013, 8, e81360. [Google Scholar] [CrossRef]
- Hudson, L.E.; Allen, R.L. Leukocyte Ig-Like Receptors—A Model for MHC Class I Disease Associations. Front. Immunol. 2016, 7, 281. [Google Scholar] [CrossRef]
- Mitchell, A.; Rentero, C.; Endoh, Y.; Hsu, K.; Gaus, K.; Geczy, C.; McNeil, H.P.; Borges, L.; Tedla, N. LILRA5 Is Expressed by Synovial Tissue Macrophages in Rheumatoid Arthritis, Selectively Induces pro-Inflammatory Cytokines and IL-10 and Is Regulated by TNF-Alpha, IL-10 and IFN-Gamma. Eur. J. Immunol. 2008, 38, 3459–3473. [Google Scholar] [CrossRef]
- Brown, D.P.; Jones, D.C.; Anderson, K.J.; Lapaque, N.; Buerki, R.A.; Trowsdale, J.; Allen, R.L. The Inhibitory Receptor LILRB4 (ILT3) Modulates Antigen Presenting Cell Phenotype and, along with LILRB2 (ILT4), Is Upregulated in Response to Salmonella Infection. BMC Immunol. 2009, 10, 56. [Google Scholar] [CrossRef]
- Young, N.T.; Waller, E.C.P.; Patel, R.; Roghanian, A.; Austyn, J.M.; Trowsdale, J. The Inhibitory Receptor LILRB1 Modulates the Differentiation and Regulatory Potential of Human Dendritic Cells. Blood 2008, 111, 3090–3096. [Google Scholar] [CrossRef]
- Brown, D.; Trowsdale, J.; Allen, R. The LILR Family: Modulators of Innate and Adaptive Immune Pathways in Health and Disease. Tissue Antigens 2004, 64, 215–225. [Google Scholar] [CrossRef]
- Jones, D.C.; Roghanian, A.; Brown, D.P.; Chang, C.; Allen, R.L.; Trowsdale, J.; Young, N.T. Alternative MRNA Splicing Creates Transcripts Encoding Soluble Proteins from Most LILR Genes. Eur. J. Immunol. 2009, 39, 3195–3206. [Google Scholar] [CrossRef]
- An, H.; Chandra, V.; Piraino, B.; Borges, L.; Geczy, C.; McNeil, H.P.; Bryant, K.; Tedla, N. Soluble LILRA3, a Potential Natural Antiinflammatory Protein, Is Increased in Patients with Rheumatoid Arthritis and Is Tightly Regulated by Interleukin 10, Tumor Necrosis Factor-Alpha, and Interferon-Gamma. J. Rheumatol. 2010, 37, 1596–1606. [Google Scholar] [CrossRef]
- Torkar, M.; Haude, A.; Milne, S.; Beck, S.; Trowsdale, J.; Wilson, M.J. Arrangement of the ILT Gene Cluster: A Common Null Allele of the ILT6 Gene Results from a 6.7-Kbp Deletion. Eur. J. Immunol. 2000, 30, 3655–3662. [Google Scholar] [CrossRef]
- Hirayasu, K.; Ohashi, J.; Tanaka, H.; Kashiwase, K.; Ogawa, A.; Takanashi, M.; Satake, M.; Jia, G.J.; Chimge, N.-O.; Sideltseva, E.W.; et al. Evidence for Natural Selection on Leukocyte Immunoglobulin-like Receptors for HLA Class I in Northeast Asians. Am. J. Hum. Genet. 2008, 82, 1075–1083. [Google Scholar] [CrossRef]
- Du, Y.; Su, Y.; He, J.; Yang, Y.; Shi, Y.; Cui, Y.; Luo, C.; Wu, X.; Liu, X.; Hu, F.; et al. Impact of the Leucocyte Immunoglobulin-like Receptor A3 (LILRA3) on Susceptibility and Subphenotypes of Systemic Lupus Erythematosus and Sjögren’s Syndrome. Ann. Rheum. Dis. 2015, 74, 2070–2075. [Google Scholar] [CrossRef]
- Du, Y.; Sun, F.; Zhou, M.; Wu, X.; Sun, W.; Jiang, Y.; Cheng, Q.; Chen, X.; Wu, H.; Xue, J. The Expression and Clinical Significance of Different Forms of LILRA3 in Systemic Lupus Erythematosus. Clin. Rheumatol. 2019, 38, 3099–3107. [Google Scholar] [CrossRef] [PubMed]
- Fragkioudaki, S.; Mavragani, C.P.; Moutsopoulos, H.M. Predicting the Risk for Lymphoma Development in Sjogren Syndrome: An Easy Tool for Clinical Use. Medicine (Baltimore) 2016, 95, e3766. [Google Scholar] [CrossRef]
- Quartuccio, L.; Isola, M.; Baldini, C.; Priori, R.; Bartoloni Bocci, E.; Carubbi, F.; Maset, M.; Gregoraci, G.; Della Mea, V.; Salvin, S.; et al. Biomarkers of Lymphoma in Sjögren’s Syndrome and Evaluation of the Lymphoma Risk in Prelymphomatous Conditions: Results of a Multicenter Study. J. Autoimmun. 2014, 51, 75–80. [Google Scholar] [CrossRef]
- Shiboski, C.H.; Shiboski, S.C.; Seror, R.; Criswell, L.A.; Labetoulle, M.; Lietman, T.M.; Rasmussen, A.; Scofield, H.; Vitali, C.; Bowman, S.J.; et al. 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjögren’s Syndrome: A Consensus and Data-Driven Methodology Involving Three International Patient Cohorts. Arthritis Rheumatol. 2017, 69, 35–45. [Google Scholar] [CrossRef]
- Nezos, A.; Makri, P.; Gandolfo, S.; De Vita, S.; Voulgarelis, M.; Crow, M.K.; Mavragani, C.P. TREX1 Variants in Sjogren’s Syndrome Related Lymphomagenesis. Cytokine 2019, 154781. [Google Scholar] [CrossRef]
- Ordóñez, D.; Sánchez, A.J.; Martínez-Rodríguez, J.E.; Cisneros, E.; Ramil, E.; Romo, N.; Moraru, M.; Munteis, E.; López-Botet, M.; Roquer, J.; et al. Multiple Sclerosis Associates with LILRA3 Deletion in Spanish Patients. Genes Immun. 2009, 10, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, A.; Mavragani, C.P.; Nezos, A.; Zintzaras, E.; Quartuccio, L.; De Vita, S.; Koutsilieris, M.; Tzioufas, A.G.; Moutsopoulos, H.M.; Voulgarelis, M. A BAFF Receptor His159Tyr Mutation in Sjögren’s Syndrome-Related Lymphoproliferation. Arthritis Rheumatol. Hoboken NJ 2015, 67, 2732–2741. [Google Scholar] [CrossRef]
- Nezos, A.; Gkioka, E.; Koutsilieris, M.; Voulgarelis, M.; Tzioufas, A.G.; Mavragani, C.P. TNFAIP3 F127C Coding Variation in Greek Primary Sjogren’s Syndrome Patients. J. Immunol. Res. 2018, 2018, 6923213. [Google Scholar] [CrossRef]
- An, H.; Lim, C.; Guillemin, G.J.; Vollmer-Conna, U.; Rawlinson, W.; Bryant, K.; Tedla, N. Serum Leukocyte Immunoglobulin-Like Receptor A3 (LILRA3) Is Increased in Patients with Multiple Sclerosis and Is a Strong Independent Indicator of Disease Severity; 6.7kbp LILRA3 Gene Deletion Is Not Associated with Diseases Susceptibility. PLoS ONE 2016, 11, e0149200. [Google Scholar] [CrossRef]
- Ostuni, P.A.; Ianniello, A.; Sfriso, P.; Mazzola, G.; Andretta, M.; Gambari, P.F. Juvenile Onset of Primary Sjögren’s Syndrome: Report of 10 Cases. Clin. Exp. Rheumatol. 1996, 14, 689–693. [Google Scholar]
- Ramos-Casals, M.; Cervera, R.; Font, J.; García-Carrasco, M.; Espinosa, G.; Reino, S.; Pallarés, L.; Ingelmo, M. Young Onset of Primary Sjögren’s Syndrome: Clinical and Immunological Characteristics. Lupus 1998, 7, 202–206. [Google Scholar] [CrossRef]
- Cimaz, R.; Casadei, A.; Rose, C.; Bartunkova, J.; Sediva, A.; Falcini, F.; Picco, P.; Taglietti, M.; Zulian, F.; Ten Cate, R.; et al. Primary Sjögren Syndrome in the Paediatric Age: A Multicentre Survey. Eur. J. Pediatr. 2003, 162, 661–665. [Google Scholar] [CrossRef]
- Virdee, S.; Greenan-Barrett, J.; Ciurtin, C. A Systematic Review of Primary Sjögren’s Syndrome in Male and Paediatric Populations. Clin. Rheumatol. 2017, 36, 2225–2236. [Google Scholar] [CrossRef] [PubMed]
- Goules, A.V.; Argyropoulou, O.D.; Pezoulas, V.C.; Chatzis, L.; Critselis, E.; Gandolfo, S.; Ferro, F.; Binutti, M.; Donati, V.; Zandonella Callegher, S.; et al. Primary Sjögren’s Syndrome of Early and Late Onset: Distinct Clinical Phenotypes and Lymphoma Development. Front. Immunol. 2020, 11, 594096. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, T. The Nuclear Factor NF-ΚB Pathway in Inflammation. Cold Spring Harb. Perspect. Biol. 2009, 1. [Google Scholar] [CrossRef] [PubMed]
- Tasaki, S.; Suzuki, K.; Nishikawa, A.; Kassai, Y.; Takiguchi, M.; Kurisu, R.; Okuzono, Y.; Miyazaki, T.; Takeshita, M.; Yoshimoto, K.; et al. Multiomic Disease Signatures Converge to Cytotoxic CD8 T Cells in Primary Sjögren’s Syndrome. Ann. Rheum. Dis. 2017, 76, 1458–1466. [Google Scholar] [CrossRef]
- Low, H.Z.; Ahrenstorf, G.; Pommerenke, C.; Habermann, N.; Schughart, K.; Ordóñez, D.; Stripecke, R.; Wilk, E.; Witte, T. TLR8 Regulation of LILRA3 in Monocytes Is Abrogated in Human Immunodeficiency Virus Infection and Correlates to CD4 Counts and Virus Loads. Retrovirology 2016, 13, 15. [Google Scholar] [CrossRef]
- Jung, M.; Sabat, R.; Krätzschmar, J.; Seidel, H.; Wolk, K.; Schönbein, C.; Schütt, S.; Friedrich, M.; Döcke, W.-D.; Asadullah, K.; et al. Expression Profiling of IL-10-Regulated Genes in Human Monocytes and Peripheral Blood Mononuclear Cells from Psoriatic Patients during IL-10 Therapy. Eur. J. Immunol. 2004, 34, 481–493. [Google Scholar] [CrossRef]
- Du, Y.; Cui, Y.; Liu, X.; Hu, F.; Yang, Y.; Wu, X.; Liu, X.; Ma, X.; Zuo, X.; Sheng, Y.; et al. Contribution of Functional LILRA3, but Not Nonfunctional LILRA3, to Sex Bias in Susceptibility and Severity of Anti-Citrullinated Protein Antibody-Positive Rheumatoid Arthritis. Arthritis Rheumatol. Hoboken NJ 2014, 66, 822–830. [Google Scholar] [CrossRef]
- Wang, H.; Wang, Y.; Tang, Y.; Ye, H.; Zhang, X.; Zhou, G.; Lv, J.; Cai, Y.; Li, Z.; Guo, J.; et al. Frequencies of the LILRA3 6.7-Kb Deletion Are Highly Differentiated Among Han Chinese Subpopulations and Involved in Ankylosing Spondylitis Predisposition. Front. Genet. 2019, 10, 869. [Google Scholar] [CrossRef]
- Koch, S.; Goedde, R.; Nigmatova, V.; Epplen, J.T.; Müller, N.; de Seze, J.; Vermersch, P.; Momot, T.; Schmidt, R.E.; Witte, T. Association of Multiple Sclerosis with ILT6 Deficiency. Genes Immun. 2005, 6, 445–447. [Google Scholar] [CrossRef] [PubMed]
| Prevalence of LILRA3 Variants | |||
|---|---|---|---|
| LILRA3 Genotype (n, %) | HC (n = 381) | SS-nL (n = 301) | SS-L (n = 101) |
| (+/+) | 326 (85.6%) | 256 (85.0%) | 91 (90.1%) |
| (+/−) | 54 (14.2%) | 44 (14.7%) | 9 (8.9%) |
| (−/−) | 1 (0.2%) | 1 (0.3%) | 1 (1%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Argyriou, E.; Nezos, A.; Roussos, P.; Venetsanopoulou, A.; Voulgarelis, M.; Boki, K.; Tzioufas, A.G.; Moutsopoulos, H.M.; Mavragani, C.P. Leukocyte Immunoglobulin-Like Receptor A3 (LILRA3): A Novel Marker for Lymphoma Development among Patients with Young Onset Sjogren’s Syndrome. J. Clin. Med. 2021, 10, 644. https://doi.org/10.3390/jcm10040644
Argyriou E, Nezos A, Roussos P, Venetsanopoulou A, Voulgarelis M, Boki K, Tzioufas AG, Moutsopoulos HM, Mavragani CP. Leukocyte Immunoglobulin-Like Receptor A3 (LILRA3): A Novel Marker for Lymphoma Development among Patients with Young Onset Sjogren’s Syndrome. Journal of Clinical Medicine. 2021; 10(4):644. https://doi.org/10.3390/jcm10040644
Chicago/Turabian StyleArgyriou, Evangelia, Adrianos Nezos, Petros Roussos, Aliki Venetsanopoulou, Michael Voulgarelis, Kyriaki Boki, Athanasios G. Tzioufas, Haralampos M. Moutsopoulos, and Clio P. Mavragani. 2021. "Leukocyte Immunoglobulin-Like Receptor A3 (LILRA3): A Novel Marker for Lymphoma Development among Patients with Young Onset Sjogren’s Syndrome" Journal of Clinical Medicine 10, no. 4: 644. https://doi.org/10.3390/jcm10040644
APA StyleArgyriou, E., Nezos, A., Roussos, P., Venetsanopoulou, A., Voulgarelis, M., Boki, K., Tzioufas, A. G., Moutsopoulos, H. M., & Mavragani, C. P. (2021). Leukocyte Immunoglobulin-Like Receptor A3 (LILRA3): A Novel Marker for Lymphoma Development among Patients with Young Onset Sjogren’s Syndrome. Journal of Clinical Medicine, 10(4), 644. https://doi.org/10.3390/jcm10040644






