ECMO in Cardiac Arrest: A Narrative Review of the Literature
Abstract
1. Introduction
2. Methods
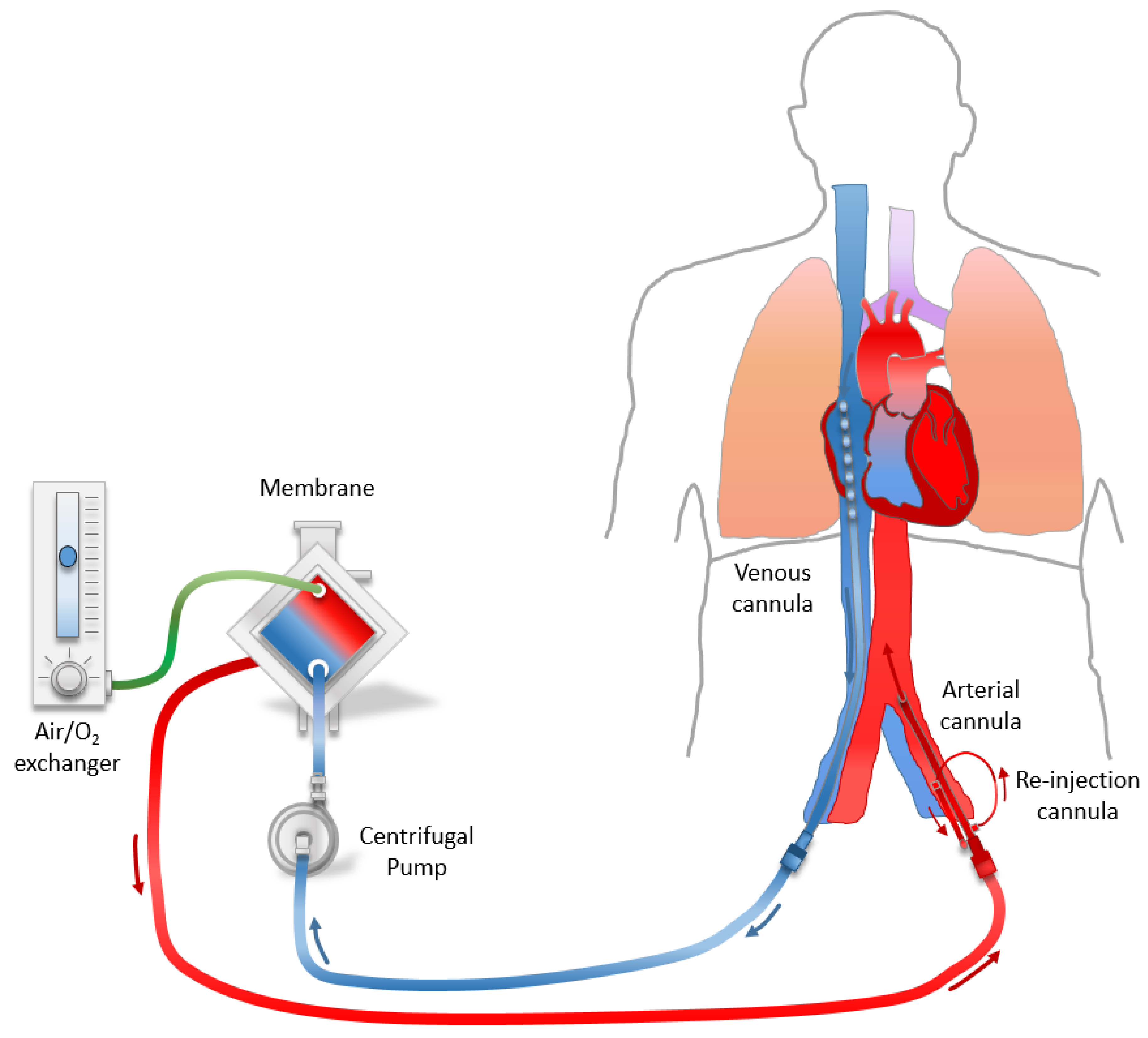
3. Place of Implementation of the ECPR
4. Equipment and Technique for Setting Up ECPR
5. Patient Selection Process
6. Patients Management after ECPR
7. Neurological Outcomes
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Wong, C.X.; Brown, A.; Lau, D.H.; Chugh, S.S.; Albert, C.M.; Kalman, J.M.; Sanders, P. Epidemiology of Sudden Cardiac Death: Global and Regional Perspectives. Heart Lung Circ. 2019, 28, 6–14. [Google Scholar] [CrossRef]
- Yan, S.; Gan, Y.; Jiang, N.; Wang, R.; Chen, Y.; Luo, Z.; Zong, Q.; Chen, S.; Lv, C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: A systematic review and meta-analysis. Crit Care 2020, 24, 61. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.S.; Lin, J.W.; Yu, H.Y.; Ko, W.J.; Jerng, J.S.; Chang, W.T.; Chen, W.J.; Huang, S.C.; Chi, N.H.; Wang, C.H.; et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: An observational study and propensity analysis. Lancet 2008, 372, 554–561. [Google Scholar] [CrossRef]
- Wengenmayer, T.; Rombach, S.; Ramshorn, F.; Biever, P.; Bode, C.; Duerschmied, D.; Staudacher, D.L. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit. Care 2017, 21, 157. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, T.; Morimura, N.; Nagao, K.; Asai, Y.; Yokota, H.; Nara, S.; Hase, M.; Tahara, Y.; Atsumi, T.; Group, S.-J.S. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: A prospective observational study. Resuscitation 2014, 85, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Le Guen, M.; Nicolas-Robin, A.; Carreira, S.; Raux, M.; Leprince, P.; Riou, B.; Langeron, O. Extracorporeal life support following out-of-hospital refractory cardiac arrest. Crit. Care 2011, 15, R29. [Google Scholar] [CrossRef]
- Kagawa, E.; Inoue, I.; Kawagoe, T.; Ishihara, M.; Shimatani, Y.; Kurisu, S.; Nakama, Y.; Dai, K.; Takayuki, O.; Ikenaga, H.; et al. Assessment of outcomes and differences between in- and out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal life support. Resuscitation 2010, 81, 968–973. [Google Scholar] [CrossRef]
- Danial, P.; Hajage, D.; Nguyen, L.S.; Mastroianni, C.; Demondion, P.; Schmidt, M.; Bougle, A.; Amour, J.; Leprince, P.; Combes, A.; et al. Percutaneous versus surgical femoro-femoral veno-arterial ECMO: A propensity score matched study. Intensive Care Med. 2018, 44, 2153–2161. [Google Scholar] [CrossRef]
- Bellezzo, J.M.; Shinar, Z.; Davis, D.P.; Jaski, B.E.; Chillcott, S.; Stahovich, M.; Walker, C.; Baradarian, S.; Dembitsky, W. Emergency physician-initiated extracorporeal cardiopulmonary resuscitation. Resuscitation 2012, 83, 966–970. [Google Scholar] [CrossRef]
- Lamhaut, L.; Hutin, A.; Puymirat, E.; Jouan, J.; Raphalen, J.H.; Jouffroy, R.; Jaffry, M.; Dagron, C.; An, K.; Dumas, F.; et al. A Pre-Hospital Extracorporeal Cardio Pulmonary Resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: An observational study and propensity analysis. Resuscitation 2017, 117, 109–117. [Google Scholar] [CrossRef]
- Megarbane, B.; Leprince, P.; Deye, N.; Resiere, D.; Guerrier, G.; Rettab, S.; Theodore, J.; Karyo, S.; Gandjbakhch, I.; Baud, F.J. Emergency feasibility in medical intensive care unit of extracorporeal life support for refractory cardiac arrest. Intensive Care Med. 2007, 33, 758–764. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Deballon, I.; Hornby, L.; Shemie, S.D.; Bhanji, F.; Guadagno, E. Extracorporeal resuscitation for refractory out-of-hospital cardiac arrest in adults: A systematic review of international practices and outcomes. Resuscitation 2016, 101, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Tonna, J.E.; Johnson, N.J.; Greenwood, J.; Gaieski, D.F.; Shinar, Z.; Bellezo, J.M.; Becker, L.; Shah, A.P.; Youngquist, S.T.; Mallin, M.P.; et al. Practice characteristics of Emergency Department extracorporeal cardiopulmonary resuscitation (eCPR) programs in the United States: The current state of the art of Emergency Department extracorporeal membrane oxygenation (ED ECMO). Resuscitation 2016, 107, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Poppe, M.; Weiser, C.; Holzer, M.; Sulzgruber, P.; Datler, P.; Keferbock, M.; Zeiner, S.; Lobmeyr, E.; van Tulder, R.; Ziegler, A.; et al. The incidence of “load&go” out-of-hospital cardiac arrest candidates for emergency department utilization of emergency extracorporeal life support: A one-year review. Resuscitation 2015, 91, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.H.; Chou, N.K.; Becker, L.B.; Lin, J.W.; Yu, H.Y.; Chi, N.H.; Hunag, S.C.; Ko, W.J.; Wang, S.S.; Tseng, L.J.; et al. Improved outcome of extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest—A comparison with that for extracorporeal rescue for in-hospital cardiac arrest. Resuscitation 2014, 85, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Bougouin, W.; Dumas, F.; Lamhaut, L.; Marijon, E.; Carli, P.; Combes, A.; Pirracchio, R.; Aissaoui, N.; Karam, N.; Deye, N.; et al. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: A registry study. Eur. Heart J. 2019, 41, 1–11. [Google Scholar] [CrossRef]
- Longo, U.G.; Ciuffreda, M.; D’Andrea, V.; Mannering, N.; Locher, J.; Denaro, V. All-polyethylene versus metal-backed tibial component in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3620–3636. [Google Scholar] [CrossRef]
- Atkinson, T.M.; Ohman, E.M.; O’Neill, W.W.; Rab, T.; Cigarroa, J.E.; Interventional Scientific Council of the American College of Cardiology. A Practical Approach to Mechanical Circulatory Support in Patients Undergoing Percutaneous Coronary Intervention: An Interventional Perspective. JACC Cardiovasc. Interv. 2016, 9, 871–883. [Google Scholar] [CrossRef]
- Garan, A.R.; Kirtane, A.; Takayama, H. Redesigning Care for Patients with Acute Myocardial Infarction Complicated by Cardiogenic Shock: The “Shock Team”. JAMA Surg. 2016, 151, 684–685. [Google Scholar] [CrossRef]
- Tchantchaleishvili, V.; Hallinan, W.; Massey, H.T. Call for Organized Statewide Networks for Management of Acute Myocardial Infarction-Related Cardiogenic Shock. JAMA Surg. 2015, 150, 1025–1026. [Google Scholar] [CrossRef]
- Garan, A.R.; Eckhardt, C.; Takeda, K.; Topkara, V.K.; Clerkin, K.; Fried, J.; Masoumi, A.; Demmer, R.T.; Trinh, P.; Yuzefpolskaya, M.; et al. Predictors of survival and ability to wean from short-term mechanical circulatory support device following acute myocardial infarction complicated by cardiogenic shock. Eur. Heart J. Acute Cardiovasc. Care 2018, 7, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Muller, G.; Flecher, E.; Lebreton, G.; Luyt, C.E.; Trouillet, J.L.; Brechot, N.; Schmidt, M.; Mastroianni, C.; Chastre, J.; Leprince, P.; et al. The ENCOURAGE mortality risk score and analysis of long-term outcomes after VA-ECMO for acute myocardial infarction with cardiogenic shock. Intensive Care Med. 2016, 42, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Baratto, F.; Pappalardo, F.; Oloriz, T.; Bisceglia, C.; Vergara, P.; Silberbauer, J.; Albanese, N.; Cireddu, M.; D’Angelo, G.; Di Prima, A.L.; et al. Extracorporeal Membrane Oxygenation for Hemodynamic Support of Ventricular Tachycardia Ablation. Circ. Arrhythm Electrophysiol. 2016, 9, e004492. [Google Scholar] [CrossRef] [PubMed]
- Brunner, M.E.; Siegenthaler, N.; Shah, D.; Licker, M.J.; Cikirikcioglu, M.; Brochard, L.; Bendjelid, K.; Giraud, R. Extracorporeal membrane oxygenation support as bridge to recovery in a patient with electrical storm related cardiogenic shock. Am. J. Emerg. Med. 2013, 31, 467.e1–467.e6. [Google Scholar] [CrossRef] [PubMed]
- Guglin, M.; Zucker, M.J.; Bazan, V.M.; Bozkurt, B.; El Banayosy, A.; Estep, J.D.; Gurley, J.; Nelson, K.; Malyala, R.; Panjrath, G.S.; et al. Venoarterial ECMO for Adults: JACC Scientific Expert Panel. J. Am. Coll. Cardiol. 2019, 73, 698–716. [Google Scholar] [CrossRef]
- Rosenzweig, E.B.; Brodie, D.; Abrams, D.C.; Agerstrand, C.L.; Bacchetta, M. Extracorporeal membrane oxygenation as a novel bridging strategy for acute right heart failure in group 1 pulmonary arterial hypertension. ASAIO J. 2014, 60, 129–133. [Google Scholar] [CrossRef]
- Banfi, C.; Pozzi, M.; Siegenthaler, N.; Brunner, M.E.; Tassaux, D.; Obadia, J.F.; Bendjelid, K.; Giraud, R. Veno-venous extracorporeal membrane oxygenation: Cannulation techniques. J. Thorac. Dis. 2016, 8, 3762–3773. [Google Scholar] [CrossRef]
- Barbaro, R.P.; Odetola, F.O.; Kidwell, K.M.; Paden, M.L.; Bartlett, R.H.; Davis, M.M.; Annich, G.M. Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am. J. Respir. Crit. Care Med. 2015, 191, 894–901. [Google Scholar] [CrossRef]
- Broman, L.M.; Holzgraefe, B.; Palmer, K.; Frenckner, B. The Stockholm experience: Interhospital transports on extracorporeal membrane oxygenation. Crit. Care 2015, 19, 278. [Google Scholar] [CrossRef]
- Noah, M.A.; Peek, G.J.; Finney, S.J.; Griffiths, M.J.; Harrison, D.A.; Grieve, R.; Sadique, M.Z.; Sekhon, J.S.; McAuley, D.F.; Firmin, R.K.; et al. Referral to an extracorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A(H1N1). JAMA 2011, 306, 1659–1668. [Google Scholar] [CrossRef]
- Peek, G.J.; Mugford, M.; Tiruvoipati, R.; Wilson, A.; Allen, E.; Thalanany, M.M.; Hibbert, C.L.; Truesdale, A.; Clemens, F.; Cooper, N.; et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): A multicentre randomised controlled trial. Lancet 2009, 374, 1351–1363. [Google Scholar] [CrossRef]
- Moret, M.; Banfi, C.; Sartorius, D.; Fumeaux, T.; Leeman-Refondini, C.; Sologashvili, T.; Reuse, J.; Nowicki, B.; Mamode-Premdjee, J.; Tassaux, D.; et al. [“Mobile” ECMO]. Rev. Med. Suisse 2014, 10, 2368–2374. [Google Scholar]
- Benzoni, E.; Terrosu, G.; Bresadola, V.; Cerato, F.; Cojutti, A.; Milan, E.; Dado, G.; Bresadola, F. Analysis of clinical outcomes and prognostic factors of neoadjuvant chemoradiotherapy combined with surgery: Intraperitoneal versus extraperitoneal rectal cancer. Eur. J. Cancer Care (Engl.) 2006, 15, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators; Davies, A.; Jones, D.; Bailey, M.; Beca, J.; Bellomo, R.; Blackwell, N.; Forrest, P.; Gattas, D.; Granger, E.; et al. Extracorporeal Membrane Oxygenation for 2009 Influenza A(H1N1) Acute Respiratory Distress Syndrome. JAMA 2009, 302, 1888–1895. [Google Scholar] [CrossRef]
- Patroniti, N.; Zangrillo, A.; Pappalardo, F.; Peris, A.; Cianchi, G.; Braschi, A.; Iotti, G.A.; Arcadipane, A.; Panarello, G.; Ranieri, V.M.; et al. The Italian ECMO network experience during the 2009 influenza A(H1N1) pandemic: Preparation for severe respiratory emergency outbreaks. Intensive Care Med. 2011, 37, 1447–1457. [Google Scholar] [CrossRef]
- Lamhaut, L.; Jouffroy, R.; Soldan, M.; Phillipe, P.; Deluze, T.; Jaffry, M.; Dagron, C.; Vivien, B.; Spaulding, C.; An, K.; et al. Safety and feasibility of prehospital extra corporeal life support implementation by non-surgeons for out-of-hospital refractory cardiac arrest. Resuscitation 2013, 84, 1525–1529. [Google Scholar] [CrossRef]
- Abrams, D.; Garan, A.R.; Abdelbary, A.; Bacchetta, M.; Bartlett, R.H.; Beck, J.; Belohlavek, J.; Chen, Y.S.; Fan, E.; Ferguson, N.D.; et al. Position paper for the organization of ECMO programs for cardiac failure in adults. Intensive Care Med. 2018, 44, 717–729. [Google Scholar] [CrossRef]
- Banfi, C.; Pozzi, M.; Brunner, M.E.; Rigamonti, F.; Murith, N.; Mugnai, D.; Obadia, J.F.; Bendjelid, K.; Giraud, R. Veno-arterial extracorporeal membrane oxygenation: An overview of different cannulation techniques. J. Thorac. Dis. 2016, 8, E875–E885. [Google Scholar] [CrossRef]
- Giraud, R.; Banfi, C.; Bendjelid, K. Echocardiography should be mandatory in ECMO venous cannula placement. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 1429–1430. [Google Scholar] [CrossRef]
- Arroyo, D.; Bendjelid, K.; Robert-Ebadi, H.; Rigamonti, F.; Siegenthaler, N.; Giraud, R. Suspected Arterial Vasospasm in Femoro-Femoral Venoarterial Extracorporeal Life Support. ASAIO J. 2017, 63, e35–e38. [Google Scholar] [CrossRef]
- Conseil Francais de Reanimation, C.; Societe Francaise D’anesthesie et de, R.; Societe Francaise de, C.; Societe Francaise de Chirurgie Thoracique et, C.; Societe Francaise de Medecine, D.U.; Societe Francaise de, P.; Groupe Francophone de Reanimation et D’urgence, P.; Societe Francaise de, P.; Societe de Reanimation de Langue, F. Guidelines for indications for the use of extracorporeal life support in refractory cardiac arrest. French Ministry of Health. Ann. Fr. Anesth. Reanim. 2009, 28, 182–190. [Google Scholar] [CrossRef]
- Kim, S.J.; Jung, J.S.; Park, J.H.; Park, J.S.; Hong, Y.S.; Lee, S.W. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patients with out-of-hospital cardiac arrest: A propensity-matched study. Crit. Care 2014, 18, 535. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, J.C.; Frisch, A.; Rittenberger, J.C.; Callaway, C.W. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: When should we change to novel therapies? Circulation 2013, 128, 2488–2494. [Google Scholar] [CrossRef] [PubMed]
- Martinell, L.; Nielsen, N.; Herlitz, J.; Karlsson, T.; Horn, J.; Wise, M.P.; Unden, J.; Rylander, C. Early predictors of poor outcome after out-of-hospital cardiac arrest. Crit. Care 2017, 21, 96. [Google Scholar] [CrossRef]
- Soar, J.; Nolan, J.P.; Bottiger, B.W.; Perkins, G.D.; Lott, C.; Carli, P.; Pellis, T.; Sandroni, C.; Skrifvars, M.B.; Smith, G.B.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015, 95, 100–147. [Google Scholar] [CrossRef]
- Goto, T.; Morita, S.; Kitamura, T.; Natsukawa, T.; Sawano, H.; Hayashi, Y.; Kai, T. Impact of extracorporeal cardiopulmonary resuscitation on outcomes of elderly patients who had out-of-hospital cardiac arrests: A single-centre retrospective analysis. BMJ Open 2018, 8, e019811. [Google Scholar] [CrossRef]
- Johnson, N.J.; Acker, M.; Hsu, C.H.; Desai, N.; Vallabhajosyula, P.; Lazar, S.; Horak, J.; Wald, J.; McCarthy, F.; Rame, E.; et al. Extracorporeal life support as rescue strategy for out-of-hospital and emergency department cardiac arrest. Resuscitation 2014, 85, 1527–1532. [Google Scholar] [CrossRef]
- Lorusso, R.; Cariou, A.; Flaatten, H. The dilemma of patient age in decision-making for extracorporeal life support in cardiopulmonary resuscitation. Intensive Care Med. 2019, 45, 542–544. [Google Scholar] [CrossRef]
- Pozzi, M.; Armoiry, X.; Achana, F.; Koffel, C.; Pavlakovic, I.; Lavigne, F.; Fellahi, J.L.; Obadia, J.F. Extracorporeal Life Support for Refractory Cardiac Arrest: A 10-Year Comparative Analysis. Ann. Thorac. Surg. 2019, 107, 809–816. [Google Scholar] [CrossRef]
- Tanguay-Rioux, X.; Grunau, B.; Neumar, R.; Tallon, J.; Boone, R.; Christenson, J. Is initial rhythm in OHCA a predictor of preceding no flow time? Implications for bystander response and ECPR candidacy evaluation. Resuscitation 2018, 128, 88–92. [Google Scholar] [CrossRef]
- Otani, T.; Sawano, H.; Natsukawa, T.; Nakashima, T.; Oku, H.; Gon, C.; Takahagi, M.; Hayashi, Y. Low-flow time is associated with a favorable neurological outcome in out-of-hospital cardiac arrest patients resuscitated with extracorporeal cardiopulmonary resuscitation. J. Crit. Care 2018, 48, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Giraud, R.; Siegenthaler, N.; Schussler, O.; Kalangos, A.; Muller, H.; Bendjelid, K.; Banfi, C. The LUCAS 2 chest compression device is not always efficient: An echographic confirmation. Ann. Emerg. Med. 2015, 65, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Orso, D.; Vetrugno, L.; Federici, N.; Borselli, M.; Spadaro, S.; Cammarota, G.; Bove, T. Mechanical Ventilation Management During Mechanical Chest Compressions. Respir Care 2020. [Google Scholar] [CrossRef] [PubMed]
- Friberg, H.; Rundgren, M. Submersion, accidental hypothermia and cardiac arrest, mechanical chest compressions as a bridge to final treatment: A case report. Scand. J. Trauma Resusc. Emerg. Med. 2009, 17, 7. [Google Scholar] [CrossRef]
- Paal, P.; Gordon, L.; Strapazzon, G.; Brodmann Maeder, M.; Putzer, G.; Walpoth, B.; Wanscher, M.; Brown, D.; Holzer, M.; Broessner, G.; et al. Accidental hypothermia-an update: The content of this review is endorsed by the International Commission for Mountain Emergency Medicine (ICAR MEDCOM). Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 111. [Google Scholar] [CrossRef]
- Bartos, J.A.; Yannopoulos, D. Refractory cardiac arrest: Where extracorporeal cardiopulmonary resuscitation fits. Curr Opin Crit Care 2020, 26, 596–602. [Google Scholar] [CrossRef]
- Rupprecht, L.; Florchinger, B.; Schopka, S.; Schmid, C.; Philipp, A.; Lunz, D.; Muller, T.; Camboni, D. Cardiac decompression on extracorporeal life support: A review and discussion of the literature. ASAIO J. 2013, 59, 547–553. [Google Scholar] [CrossRef]
- Burkhoff, D.; Sayer, G.; Doshi, D.; Uriel, N. Hemodynamics of Mechanical Circulatory Support. J. Am. Coll. Cardiol. 2015, 66, 2663–2674. [Google Scholar] [CrossRef]
- Guirgis, M.; Kumar, K.; Menkis, A.H.; Freed, D.H. Minimally invasive left-heart decompression during venoarterial extracorporeal membrane oxygenation: An alternative to a percutaneous approach. Interact. Cardiovasc. Thorac. Surg. 2010, 10, 672–674. [Google Scholar] [CrossRef]
- Hlavacek, A.M.; Atz, A.M.; Bradley, S.M.; Bandisode, V.M. Left atrial decompression by percutaneous cannula placement while on extracorporeal membrane oxygenation. J. Thorac. Cardiovasc. Surg. 2005, 130, 595–596. [Google Scholar] [CrossRef]
- Koeckert, M.S.; Jorde, U.P.; Naka, Y.; Moses, J.W.; Takayama, H. Impella LP 2.5 for left ventricular unloading during venoarterial extracorporeal membrane oxygenation support. J. Card. Surg. 2011, 26, 666–668. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, S.; Richardson, J.E.; Sakai, T.; Ide, M.; Tanaka, K.A. High mortality associated with intracardiac and intrapulmonary thromboses after cardiopulmonary bypass. J. Anesth. 2012, 26, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Brechot, N.; Combes, A. Ten situations in which ECMO is unlikely to be successful. Intensive Care Med. 2016, 42, 750–752. [Google Scholar] [CrossRef] [PubMed]
- Cevasco, M.; Takayama, H.; Ando, M.; Garan, A.R.; Naka, Y.; Takeda, K. Left ventricular distension and venting strategies for patients on venoarterial extracorporeal membrane oxygenation. J. Thorac. Dis. 2019, 11, 1676–1683. [Google Scholar] [CrossRef]
- Brechot, N.; Demondion, P.; Santi, F.; Lebreton, G.; Pham, T.; Dalakidis, A.; Gambotti, L.; Luyt, C.E.; Schmidt, M.; Hekimian, G.; et al. Intra-aortic balloon pump protects against hydrostatic pulmonary oedema during peripheral venoarterial-extracorporeal membrane oxygenation. Eur. Heart J. Acute Cardiovasc. Care 2018, 7, 62–69. [Google Scholar] [CrossRef]
- Pappalardo, F.; Schulte, C.; Pieri, M.; Schrage, B.; Contri, R.; Soeffker, G.; Greco, T.; Lembo, R.; Mullerleile, K.; Colombo, A.; et al. Concomitant implantation of Impella((R)) on top of veno-arterial extracorporeal membrane oxygenation may improve survival of patients with cardiogenic shock. Eur. J. Heart Fail. 2017, 19, 404–412. [Google Scholar] [CrossRef]
- Russo, J.J.; Aleksova, N.; Pitcher, I.; Couture, E.; Parlow, S.; Faraz, M.; Visintini, S.; Simard, T.; Di Santo, P.; Mathew, R.; et al. Left Ventricular Unloading During Extracorporeal Membrane Oxygenation in Patients with Cardiogenic Shock. J. Am. Coll. Cardiol. 2019, 73, 654–662. [Google Scholar] [CrossRef]
- Lamhaut, L.; Tea, V.; Raphalen, J.H.; An, K.; Dagron, C.; Jouffroy, R.; Jouven, X.; Cariou, A.; Baud, F.; Spaulding, C.; et al. Coronary lesions in refractory out of hospital cardiac arrest (OHCA) treated by extra corporeal pulmonary resuscitation (ECPR). Resuscitation 2018, 126, 154–159. [Google Scholar] [CrossRef]
- Yannopoulos, D.; Bartos, J.A.; Martin, C.; Raveendran, G.; Missov, E.; Conterato, M.; Frascone, R.J.; Trembley, A.; Sipprell, K.; John, R.; et al. Minnesota Resuscitation Consortium’s Advanced Perfusion and Reperfusion Cardiac Life Support Strategy for Out-of-Hospital Refractory Ventricular Fibrillation. J. Am. Heart Assoc. 2016, 5, e003732. [Google Scholar] [CrossRef]
- Hutin, A.; Lamhaut, L.; Lidouren, F.; Kohlhauer, M.; Mongardon, N.; Carli, P.; Berdeaux, A.; Ghaleh, B.; Tissier, R. Early Coronary Reperfusion Facilitates Return of Spontaneous Circulation and Improves Cardiovascular Outcomes after Ischemic Cardiac Arrest and Extracorporeal Resuscitation in Pigs. J. Am. Heart Assoc. 2016, 5. [Google Scholar] [CrossRef]
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.J.; Harjola, V.P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jimenez, D.; et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur. Respir. J. 2019, 54, 1901647. [Google Scholar] [CrossRef] [PubMed]
- Kurnicka, K.; Lichodziejewska, B.; Goliszek, S.; Dzikowska-Diduch, O.; Zdonczyk, O.; Kozlowska, M.; Kostrubiec, M.; Ciurzynski, M.; Palczewski, P.; Grudzka, K.; et al. Echocardiographic Pattern of Acute Pulmonary Embolism: Analysis of 511 Consecutive Patients. J. Am. Soc. Echocardiogr. 2016, 29, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Al-Bawardy, R.; Rosenfield, K.; Borges, J.; Young, M.N.; Albaghdadi, M.; Rosovsky, R.; Kabrhel, C. Extracorporeal membrane oxygenation in acute massive pulmonary embolism: A case series and review of the literature. Perfusion 2019, 34, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Meneveau, N.; Guillon, B.; Planquette, B.; Piton, G.; Kimmoun, A.; Gaide-Chevronnay, L.; Aissaoui, N.; Neuschwander, A.; Zogheib, E.; Dupont, H.; et al. Outcomes after extracorporeal membrane oxygenation for the treatment of high-risk pulmonary embolism: A multicentre series of 52 cases. Eur. Heart J. 2018, 39, 4196–4204. [Google Scholar] [CrossRef] [PubMed]
- Corsi, F.; Lebreton, G.; Brechot, N.; Hekimian, G.; Nieszkowska, A.; Trouillet, J.L.; Luyt, C.E.; Leprince, P.; Chastre, J.; Combes, A.; et al. Life-threatening massive pulmonary embolism rescued by venoarterial-extracorporeal membrane oxygenation. Crit. Care 2017, 21, 76. [Google Scholar] [CrossRef]
- Giraud, R.; Banfi, C.; Siegenthaler, N.; Bendjelid, K. Massive pulmonary embolism leading to cardiac arrest: One pathology, two different ECMO modes to assist patients. J. Clin. Monit. Comput. 2016, 30, 933–937. [Google Scholar] [CrossRef]
- Pavlovic, G.; Banfi, C.; Tassaux, D.; Peter, R.E.; Licker, M.J.; Bendjelid, K.; Giraud, R. Peri-operative massive pulmonary embolism management: Is veno-arterial ECMO a therapeutic option? Acta Anaesthesiol. Scand. 2014, 58, 1280–1286. [Google Scholar] [CrossRef]
- Fletcher-Sandersjoo, A.; Thelin, E.P.; Bartek, J., Jr.; Broman, M.; Sallisalmi, M.; Elmi-Terander, A.; Bellander, B.M. Incidence, Outcome, and Predictors of Intracranial Hemorrhage in Adult Patients on Extracorporeal Membrane Oxygenation: A Systematic and Narrative Review. Front. Neurol. 2018, 9, 548. [Google Scholar] [CrossRef]
- Stub, D.; Bernard, S.; Pellegrino, V.; Smith, K.; Walker, T.; Sheldrake, J.; Hockings, L.; Shaw, J.; Duffy, S.J.; Burrell, A.; et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation 2015, 86, 88–94. [Google Scholar] [CrossRef]
- Nielsen, N.; Wetterslev, J.; Cronberg, T.; Erlinge, D.; Gasche, Y.; Hassager, C.; Horn, J.; Hovdenes, J.; Kjaergaard, J.; Kuiper, M.; et al. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N. Engl. J. Med. 2013, 369, 2197–2206. [Google Scholar] [CrossRef]
- Bartos, J.A.; Grunau, B.; Carlson, C.; Duval, S.; Ripeckyj, A.; Kalra, R.; Raveendran, G.; John, R.; Conterato, M.; Frascone, R.J.; et al. Improved Survival with Extracorporeal Cardiopulmonary Resuscitation Despite Progressive Metabolic Derangement Associated with Prolonged Resuscitation. Circulation 2020, 141, 877–886. [Google Scholar] [CrossRef] [PubMed]
- Kagawa, E.; Dote, K.; Kato, M.; Sasaki, S.; Nakano, Y.; Kajikawa, M.; Higashi, A.; Itakura, K.; Sera, A.; Inoue, I.; et al. Should we emergently revascularize occluded coronaries for cardiac arrest? Rapid-response extracorporeal membrane oxygenation and intra-arrest percutaneous coronary intervention. Circulation 2012, 126, 1605–1613. [Google Scholar] [CrossRef] [PubMed]
- Grunau, B.; Puyat, J.; Wong, H.; Scheuermeyer, F.X.; Reynolds, J.C.; Kawano, T.; Singer, J.; Dick, W.; Christenson, J. Gains of Continuing Resuscitation in Refractory out-of-hospital Cardiac Arrest: A Model-based Analysis to Identify Deaths Due to Intra-arrest Prognostication. Prehosp. Emerg. Care 2018, 22, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Nagao, K.; Nonogi, H.; Yonemoto, N.; Gaieski, D.F.; Ito, N.; Takayama, M.; Shirai, S.; Furuya, S.; Tani, S.; Kimura, T.; et al. Duration of Prehospital Resuscitation Efforts After Out-of-Hospital Cardiac Arrest. Circulation 2016, 133, 1386–1396. [Google Scholar] [CrossRef]
- Reynolds, J.C.; Grunau, B.E.; Elmer, J.; Rittenberger, J.C.; Sawyer, K.N.; Kurz, M.C.; Singer, B.; Proudfoot, A.; Callaway, C.W. Prevalence, natural history, and time-dependent outcomes of a multi-center North American cohort of out-of-hospital cardiac arrest extracorporeal CPR candidates. Resuscitation 2017, 117, 24–31. [Google Scholar] [CrossRef]
- Reynolds, J.C.; Grunau, B.E.; Rittenberger, J.C.; Sawyer, K.N.; Kurz, M.C.; Callaway, C.W. Association Between Duration of Resuscitation and Favorable Outcome After Out-of-Hospital Cardiac Arrest: Implications for Prolonging or Terminating Resuscitation. Circulation 2016, 134, 2084–2094. [Google Scholar] [CrossRef]
- Wang, P.L.; Brooks, S.C. Mechanical versus manual chest compressions for cardiac arrest. Cochrane Database Syst. Rev. 2018, 8, CD007260. [Google Scholar] [CrossRef]
- Nakashima, Y.; Saitoh, T.; Yasui, H.; Ueno, M.; Hotta, K.; Ogawa, T.; Takahashi, Y.; Maekawa, Y.; Yoshino, A. Comparison of Chest Compression Quality Using Wing Boards versus Walking Next to a Moving Stretcher: A Randomized Crossover Simulation Study. J. Clin. Med. 2020, 9, 1584. [Google Scholar] [CrossRef]
- Geocadin, R.G.; Callaway, C.W.; Fink, E.L.; Golan, E.; Greer, D.M.; Ko, N.U.; Lang, E.; Licht, D.J.; Marino, B.S.; McNair, N.D.; et al. Standards for Studies of Neurological Prognostication in Comatose Survivors of Cardiac Arrest: A Scientific Statement From the American Heart Association. Circulation 2019, 140, e517–e542. [Google Scholar] [CrossRef]
- Haywood, K.; Whitehead, L.; Nadkarni, V.M.; Achana, F.; Beesems, S.; Bottiger, B.W.; Brooks, A.; Castren, M.; Ong, M.E.H.; Hazinski, M.F.; et al. COSCA (Core Outcome Set for Cardiac Arrest) in Adults: An Advisory Statement from the International Liaison Committee on Resuscitation. Resuscitation 2018, 127, 147–163. [Google Scholar] [CrossRef]
| Percutaneous ECMO insertion kit |
| Vascular ultrasound probe with sterile protection |
| Echocardiography with Doppler mode |
| ECMO pump compatible with transportation |
| Backup ECMO pump |
| A battery that can last 45 min minimum |
| Clamps for cannulas/circuit |
| Surgery instruments for any hemorrhagic complications |
| Additional light for surgery |
| Heater for ECMO |
| Equipment for in-hospital transportation |
| ECMO pump transportation Cart |
| Emergency bag with all drugs and clamps |
| ECMO already primed available 24 h/24 |
| Vascular Doppler or NIRS to check distal perfusion of the leg |
| Fiberoptic bronchoscope |
| Any device able to unload the left ventricle (IABP, Impella®) |
| Favorable Criteria |
|---|
| Refractory CA with reversible cause |
| Witnessed CA |
| High quality CPR started immediately |
| Age < 70 |
| Initial shockable rhythm |
| EtCO2 > 10 mmHg |
| Signs of life under CPR |
| Reaching hospital < 40 min allowing ECMO initiation < 60 min. (Maximum low-flow < 60 min) |
| Pulse perceived under CPR |
| Unfavorable Criteria |
| CA without any witnesses and/or ignorance of the duration of the no-flow |
| No-flow > 3 min and/or Low-flow > 90 min |
| Poor quality CPR (EtCO2 < 10 mmHg and/or absence of pulse perceived under massage) |
| Non-shockable initial rhythm |
| Major comorbidities |
| Obvious clinical signs of irreversible death (rigidity, lividity) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Charrière, A.; Assouline, B.; Scheen, M.; Mentha, N.; Banfi, C.; Bendjelid, K.; Giraud, R. ECMO in Cardiac Arrest: A Narrative Review of the Literature. J. Clin. Med. 2021, 10, 534. https://doi.org/10.3390/jcm10030534
De Charrière A, Assouline B, Scheen M, Mentha N, Banfi C, Bendjelid K, Giraud R. ECMO in Cardiac Arrest: A Narrative Review of the Literature. Journal of Clinical Medicine. 2021; 10(3):534. https://doi.org/10.3390/jcm10030534
Chicago/Turabian StyleDe Charrière, Amandine, Benjamin Assouline, Marc Scheen, Nathalie Mentha, Carlo Banfi, Karim Bendjelid, and Raphaël Giraud. 2021. "ECMO in Cardiac Arrest: A Narrative Review of the Literature" Journal of Clinical Medicine 10, no. 3: 534. https://doi.org/10.3390/jcm10030534
APA StyleDe Charrière, A., Assouline, B., Scheen, M., Mentha, N., Banfi, C., Bendjelid, K., & Giraud, R. (2021). ECMO in Cardiac Arrest: A Narrative Review of the Literature. Journal of Clinical Medicine, 10(3), 534. https://doi.org/10.3390/jcm10030534







