The Loop Tenodesis Procedure—From Biomechanics to First Clinical Results
Abstract
1. Introduction
2. Materials and Methods
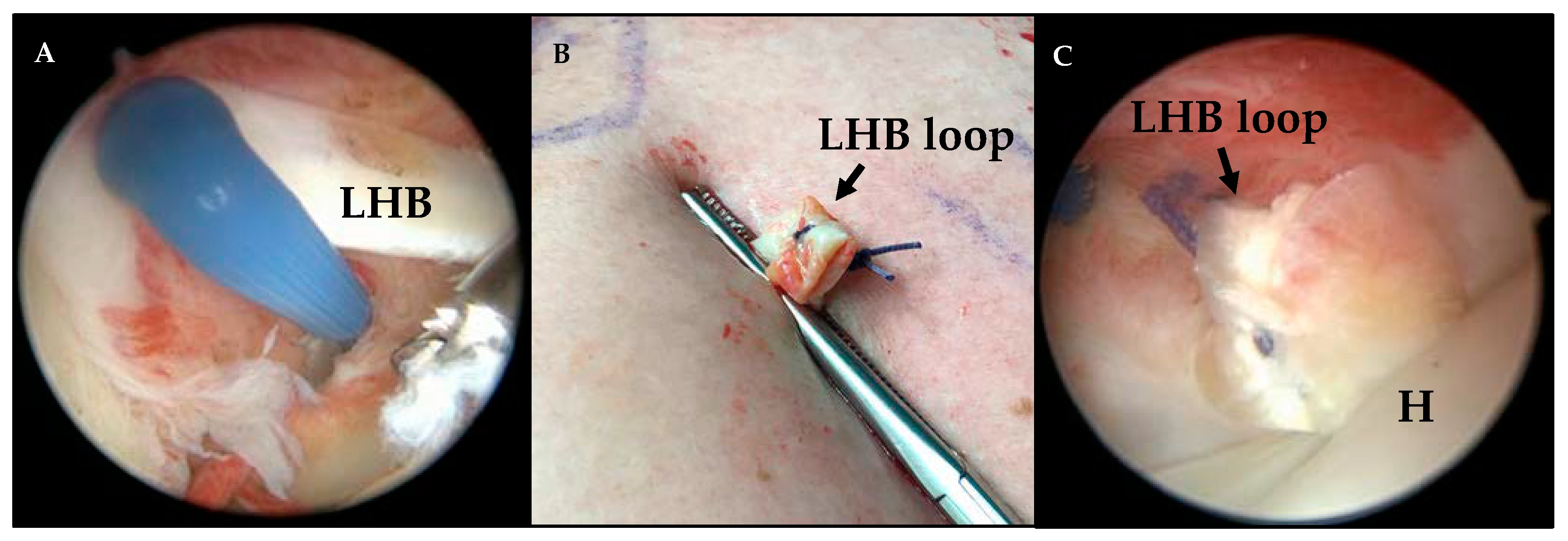
2.1. Surgical Technique
2.2. Postoperative Rehabilitation and Treatment
2.3. Functional Evaluation
2.4. Structural Evaluation
2.5. Statistical Evaluation
3. Results
3.1. Intraoperative Findings and Concomitant Procedures
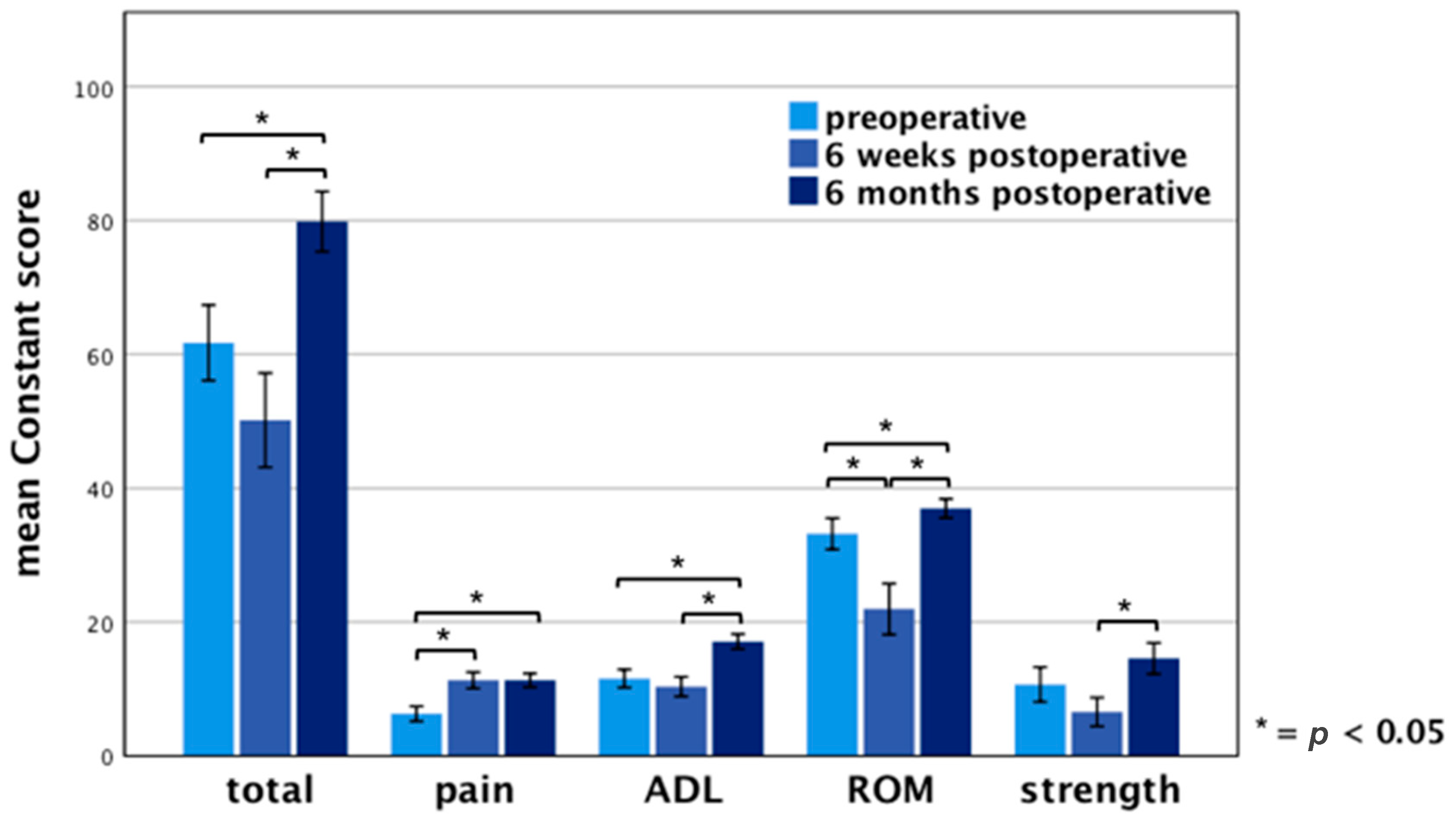
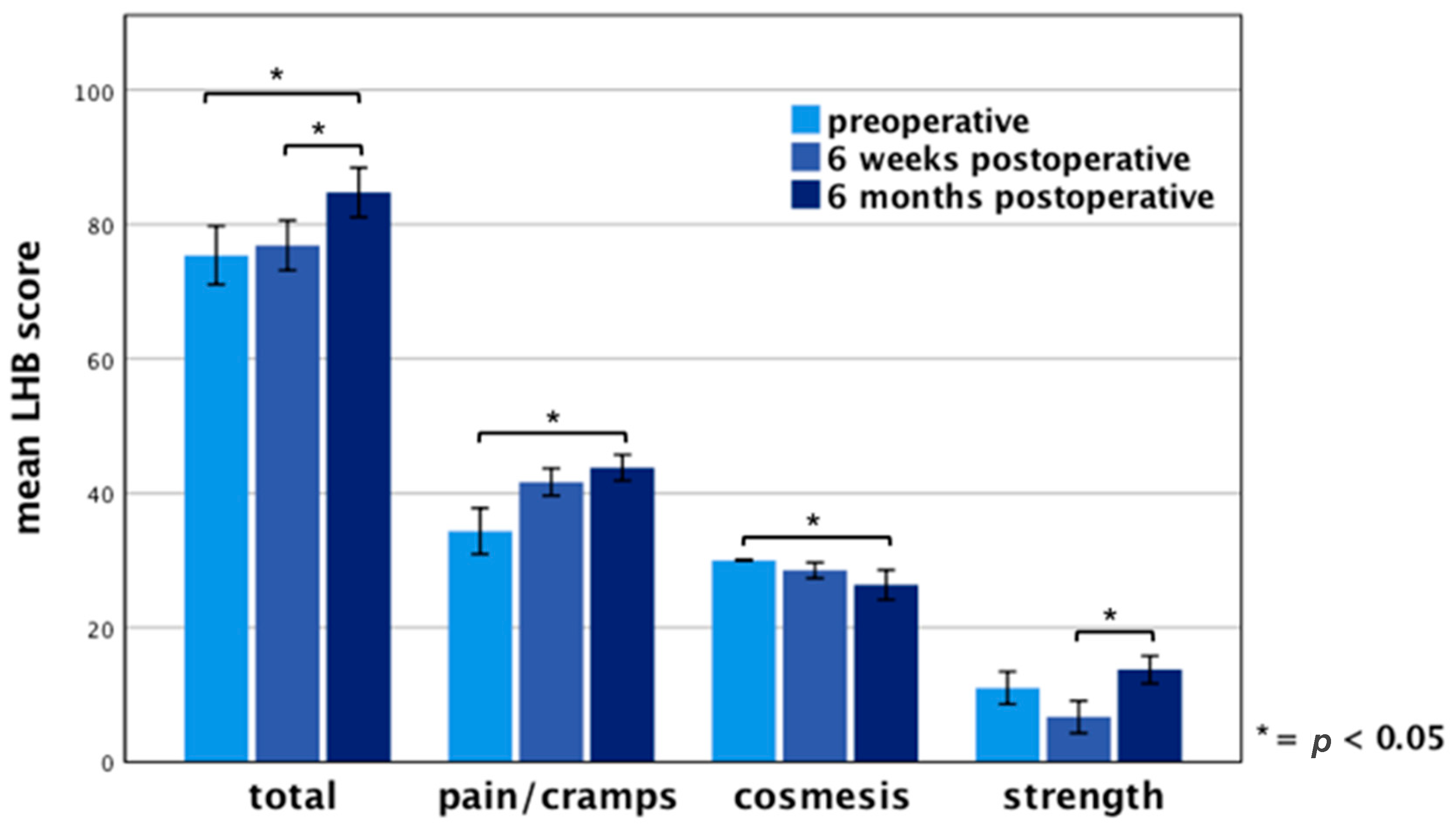
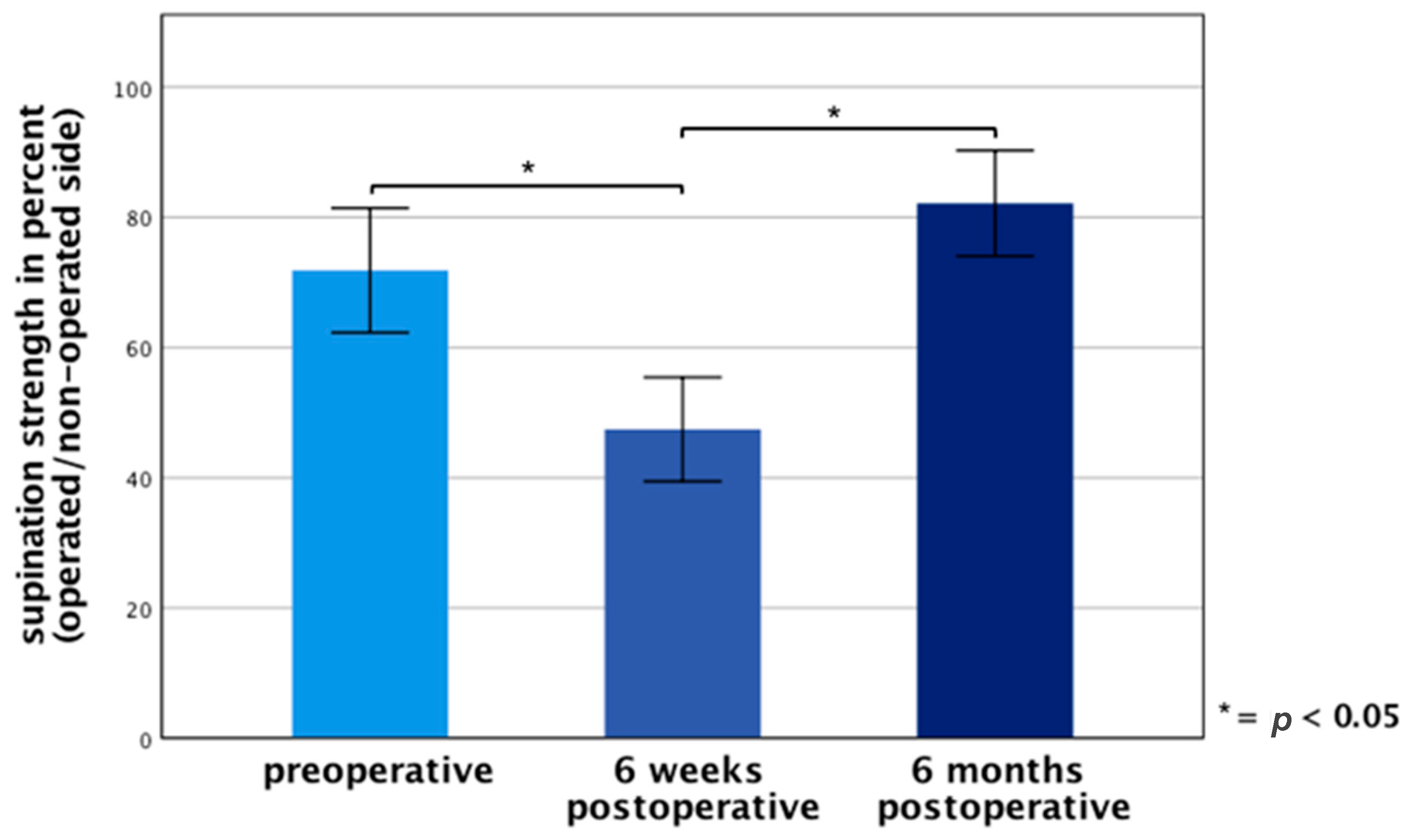
3.2. Functional Results
3.3. Structural Evaluation
4. Discussion
5. Conclusions
Outlook: All-Inside Loop Tenodesis Technique
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sethi, N.; Wright, R.; Yamaguchi, K. Disorders of the long head of the biceps tendon. J. Should. Elb. Surg. 1999, 8, 644–654. [Google Scholar] [CrossRef]
- Szabó, I.; Boileau, P.; Walch, G. The proximal biceps as a pain generator and results of tenotomy. Sports Med. Arthrosc. Rev. 2008, 16, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Mazzocca, A.D.; Bicos, J.; Santangelo, S.; Romeo, A.A.; Arciero, R.A. The biomechanical evaluation of four fixation techniques for proximal biceps tenodesis. Arthrosc. J. Arthrosc. Relat. Surg. 2005, 21, 1296–1306. [Google Scholar] [CrossRef] [PubMed]
- Romeo, A.A.; Mazzocca, A.D.; Tauro, J.C. Arthroscopic biceps tenodesis. Arthrosc. J. Arthrosc. Relat. Surg. 2004, 20, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Kerschbaum, M.; Maziak, N.; Scheuermann, M.; Scheibel, M. Arthroscopic tenodesis or tenotomy of the long head of the biceps tendon in preselected patients: Does it make a difference? Der Orthop. 2017, 46, 215–221. [Google Scholar] [CrossRef] [PubMed]
- The, B.; Brutty, M.; Wang, A.; Campbell, P.T.; Halliday, M.J.C.; Ackland, T.R. Long-term functional results and isokinetic strength evaluation after arthroscopic tenotomy of the long head of biceps tendon. Int. J. Should. Surg. 2014, 8, 76. [Google Scholar] [CrossRef]
- Slenker, N.R.; Lawson, K.; Ciccotti, M.G.; Dodson, C.C.; Cohen, S.B. Biceps tenotomy versus tenodesis: Clinical outcomes. Arthrosc. J. Arthrosc. Relat. Surg. 2012, 28, 576–582. [Google Scholar] [CrossRef]
- Na, Y.; Zhu, Y.; Shi, Y.; Ren, Y.; Zhang, T.; Liu, W.; Han, C. A meta-analysis comparing tenotomy or tenodesis for lesions of the long head of the biceps tendon with concomitant reparable rotator cuff tears. J. Orthop. Surg. Res. 2019, 14, 370. [Google Scholar] [CrossRef]
- Scheibel, M.; Schröder, R.-J.; Chen, J.; Bartsch, M. Arthroscopic soft tissue tenodesis versus bony fixation anchor tenodesis of the long head of the biceps tendon. Am. J. Sports Med. 2011, 39, 1045–1052. [Google Scholar] [CrossRef]
- Nho, S.J.; Reiff, S.N.; Verma, N.N.; Slabaugh, M.A.; Mazzocca, A.D.; Romeo, A.A. Complications associated with subpectoral biceps tenodesis: Low rates of incidence following surgery. J. Should. Elb. Surg. 2010, 19, 764–768. [Google Scholar] [CrossRef]
- Brady, P.C.; Narbona, P.; Adams, C.R.; Huberty, D.; Parten, P.; Hartzler, R.U.; Arrigoni, P.; Burkhart, S.S. Arthroscopic proximal biceps tenodesis at the articular margin: Evaluation of outcomes, complications, and revision rate. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Koch, B.S.; Burks, R.T. Failure of biceps tenodesis with interference screw fixation. Arthrosc. J. Arthrosc. Relat. Surg. 2012, 28, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Kerschbaum, M.; Weiss, I.; Mayr, A.; Pfeifer, C.; Nerlich, M.; Greiner, S. The Arthroscopic Loop Tenodesis Procedure: An Implant-Free Technique to Treat Long Biceps Tendon Pathologies. Arthrosc. Tech. 2019, 8, e503–e506. [Google Scholar] [CrossRef] [PubMed]
- Kerschbaum, M.; Voss, A.; Pfeifer, C.; Weiss, I.; Mayr, A.; Alt, V.; Greiner, S.; Grechenig, S. Novel implant-free loop Tenodesis vs. simple Tenotomy of the long biceps tendon—A biomechanical investigation. BMC Musculoskelet. Disord. 2019, 20, 522. [Google Scholar] [CrossRef]
- Constant, C.R.; Murley, A.H. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Kerschbaum, M.; Arndt, L.; Bartsch, M.; Chen, J.; Gerhardt, C.; Scheibel, M. Using the LHB score for assessment of LHB pathologies and LHB surgery: A prospective study. Arch. Orthop. Trauma Surg. 2016, 136, 469–475. [Google Scholar] [CrossRef]
- Ge, H.; Zhang, Q.; Sun, Y.; Li, J.; Sun, L.; Cheng, B. Tenotomy or Tenodesis for the Long Head of Biceps Lesions in Shoulders: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0121286. [Google Scholar] [CrossRef]
- Galasso, O.; Gasparini, G.; Benedetto, M.D.; Familiari, F.; Castricini, R. Tenotomy versus Tenodesis in the treatment of the long head of biceps brachii tendon lesions. BMC Musculoskelet. Disord. 2012, 13, 205. [Google Scholar] [CrossRef]
- Koh, K.H.; Ahn, J.H.; Kim, S.M.; Yoo, J.C. Treatment of biceps tendon lesions in the setting of rotator cuff tears: Prospective cohort study of tenotomy versus tenodesis. Am. J. Sports Med. 2010, 38, 1584–1590. [Google Scholar] [CrossRef]
- Frost, A.; Zafar, M.S.; Maffulli, N. Tenotomy versus tenodesis in the management of pathologic lesions of the tendon of the long head of the biceps brachii. Am. J. Sports Med. 2009, 37, 828–833. [Google Scholar] [CrossRef]
- Kerschbaum, M.; Scheuermann, M.; Gerhardt, C.; Scheibel, M. Arthroscopic knotless suprapectoral tenodesis of the long head of biceps: Clinical and structural results. Arch. Orthop. Trauma Surg. 2016, 136, 1135–1142. [Google Scholar] [PubMed]
- Zabrzyński, J.; Paczesny, Ł.; Łapaj, Ł.; Zabrzyńska, A.; Szwedowski, D. The surgical treatment of the long head of biceps tendon and the autotenodesis phenomenon: An ultrasound and arthroscopic study. Folia Morphol. 2020, 79, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Zabrzyński, J.; Paczesny, Ł.; Łapaj, Ł.; Grzanka, D.; Szukalski, J. Is the inflammation process absolutely absent in tendinopathy of the long head of the biceps tendon? Histopathologic study of the long head of the biceps tendon after arthroscopic treatment. Pol. J. Pathol. 2017, 68, 315–325. [Google Scholar]
- Lim, T.K.; Moon, E.S.; Koh, K.H.; Yoo, J.C. Patient-related factors and complications after arthroscopic tenotomy of the long head of the biceps tendon. Am. J. Sports Med. 2011, 39, 783–789. [Google Scholar] [PubMed]
- Walch, G.; Edwards, T.B.; Boulahia, A.; Nové-Josserand, L.; Neyton, L.; Szabo, I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: Clinical and radiographic results of 307 cases. J. Should. Elb. Surg. 2005, 14, 238–246. [Google Scholar]
- Osbahr, D.C.; Diamond, A.B.; Speer, K.P. The cosmetic appearance of the biceps muscle after long-head tenotomy versus tenodesis. Arthrosc. J. Arthrosc. Relat. Surg. 2002, 18, 483–487. [Google Scholar]
- Zabrzyński, J.; Huri, G.; Gryckiewicz, S.; Çetik, R.M.; Szwedowski, D.; Łapaj, Ł.; Gagat, M.; Paczesny, Ł. Biceps Tenodesis Versus Tenotomy with Fast Rehabilitation Protocol—A Functional Perspective in Chronic Tendinopathy. J. Clin. Med. 2020, 9, 3938. [Google Scholar] [CrossRef]
- Kerschbaum, M.; Alt, V.; Pfeifer, C. The All-Inside Arthroscopic Loop Tenodesis Procedure to Treat Long Head of Biceps Tendon Pathologies. Arthrosc. Tech. 2019, 8, e1551–e1554. [Google Scholar]
| Sex | ||
| Female | n | 11 |
| Male | n | 26 |
| Age (years) | Mean ± SD | 52.0 ± 6.9 |
| BMI (kg/m2) | Mean ± SD | 28.6 ± 3.8 |
| Operated side | ||
| Right shoulder | n | 23 |
| Left shoulder | n | 14 |
| Dominant side affected | n | 24 |
| Intraoperative Findings of LHB Pathologies | ||
|---|---|---|
| Partial LHB tear | n | 37 |
| Tendinitis | n | 12 |
| Pulley lesion | n | 35 |
| SLAP lesion | n | 1 |
| Concomitant surgeries | ||
| Rotator cuff repair | n | 37 |
| ASAD | n | 37 |
| ARAC | n | 1 |
| Upperarm Deformity | Patient-Dependent | Examiner-Dependent | |
|---|---|---|---|
| mild | n | 2 | 11 |
| moderate | n | 2 | 2 |
| severe | n | 1 | 1 |
| total | n | 5 | 14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riedl, M.; Mayr, A.; Greiner, S.; Pfeifer, C.; Weiss, I.; Forchhammer, L.; Alt, V.; Kerschbaum, M. The Loop Tenodesis Procedure—From Biomechanics to First Clinical Results. J. Clin. Med. 2021, 10, 432. https://doi.org/10.3390/jcm10030432
Riedl M, Mayr A, Greiner S, Pfeifer C, Weiss I, Forchhammer L, Alt V, Kerschbaum M. The Loop Tenodesis Procedure—From Biomechanics to First Clinical Results. Journal of Clinical Medicine. 2021; 10(3):432. https://doi.org/10.3390/jcm10030432
Chicago/Turabian StyleRiedl, Moritz, Agnes Mayr, Stefan Greiner, Christian Pfeifer, Isabella Weiss, Lina Forchhammer, Volker Alt, and Maximilian Kerschbaum. 2021. "The Loop Tenodesis Procedure—From Biomechanics to First Clinical Results" Journal of Clinical Medicine 10, no. 3: 432. https://doi.org/10.3390/jcm10030432
APA StyleRiedl, M., Mayr, A., Greiner, S., Pfeifer, C., Weiss, I., Forchhammer, L., Alt, V., & Kerschbaum, M. (2021). The Loop Tenodesis Procedure—From Biomechanics to First Clinical Results. Journal of Clinical Medicine, 10(3), 432. https://doi.org/10.3390/jcm10030432







