Clinical Considerations in Orthodontically Forced Eruption for Restorative Purposes
Abstract
1. Introduction
2. Indications
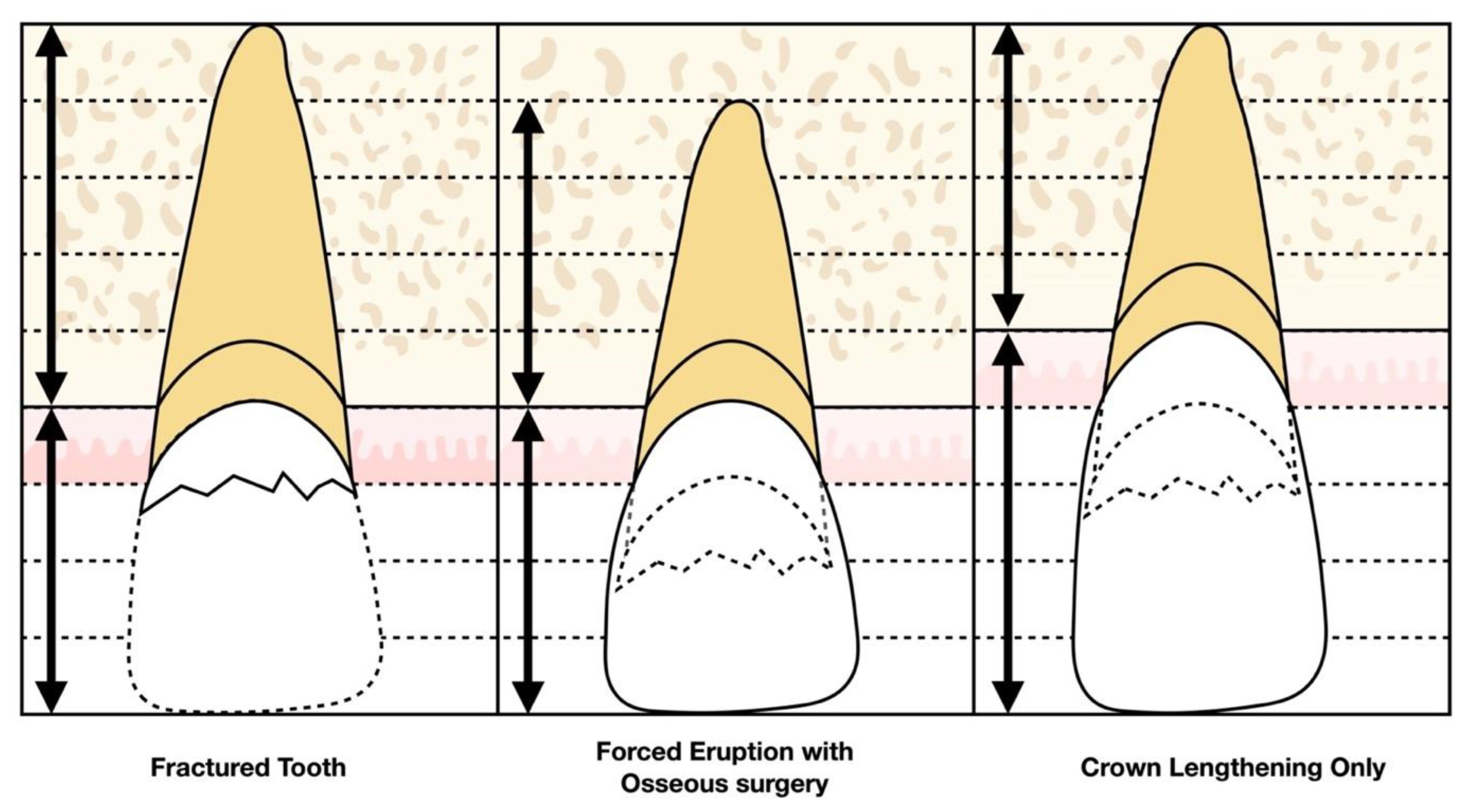
2.1. Ferrule/Crown Lengthening
2.1.1. History
2.1.2. Advantages and Disadvantages
2.1.3. Indications and Contraindications
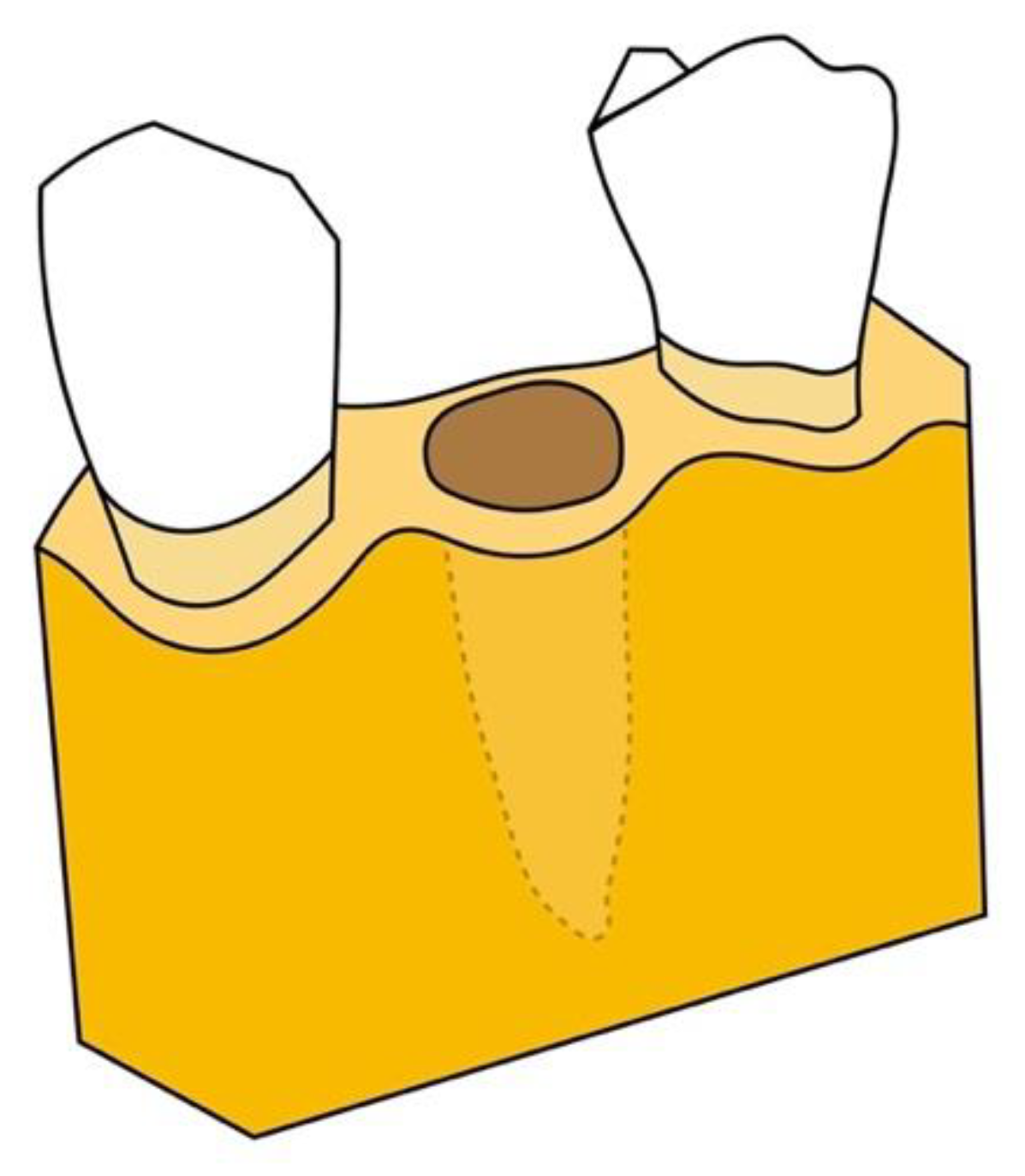
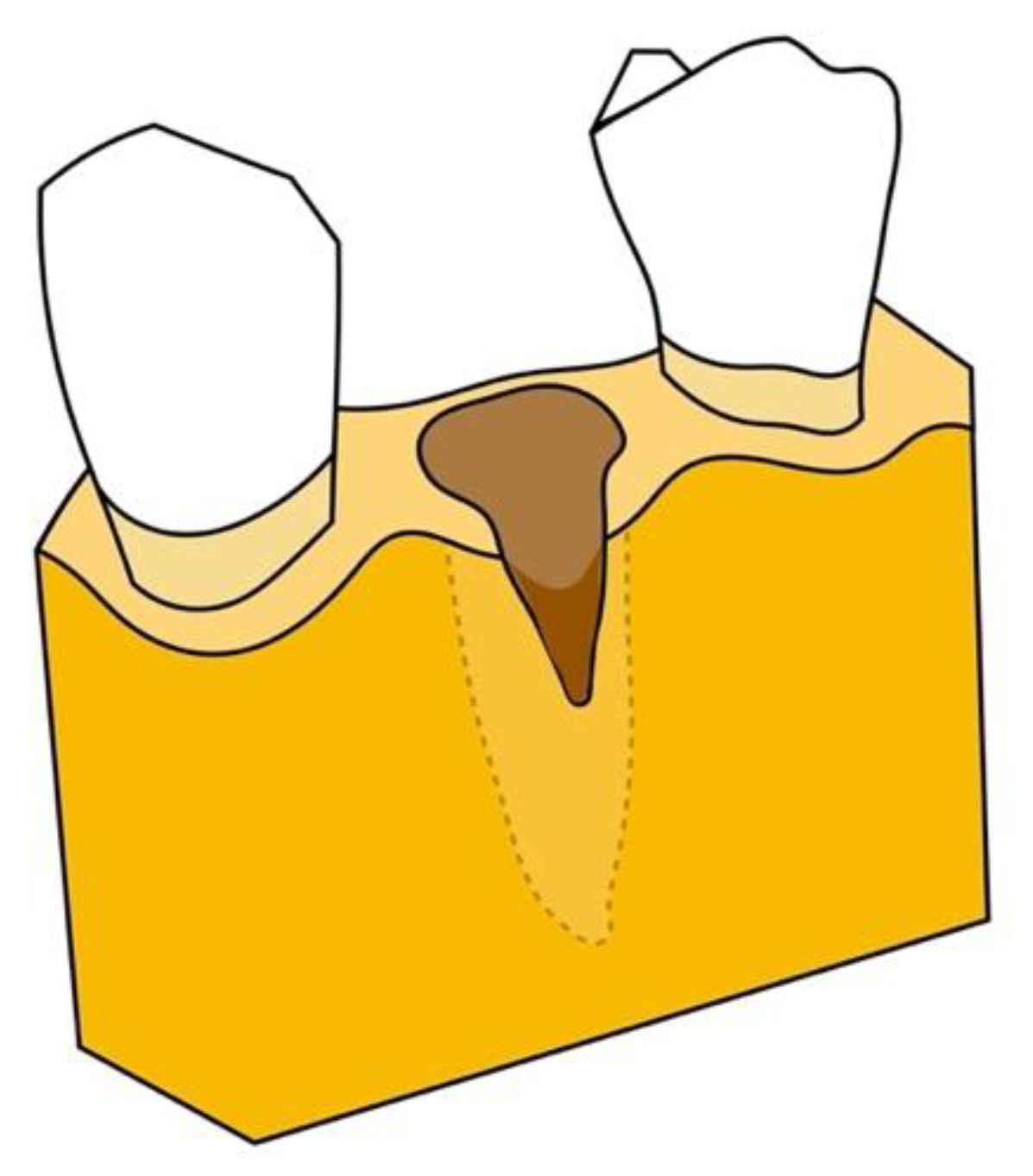
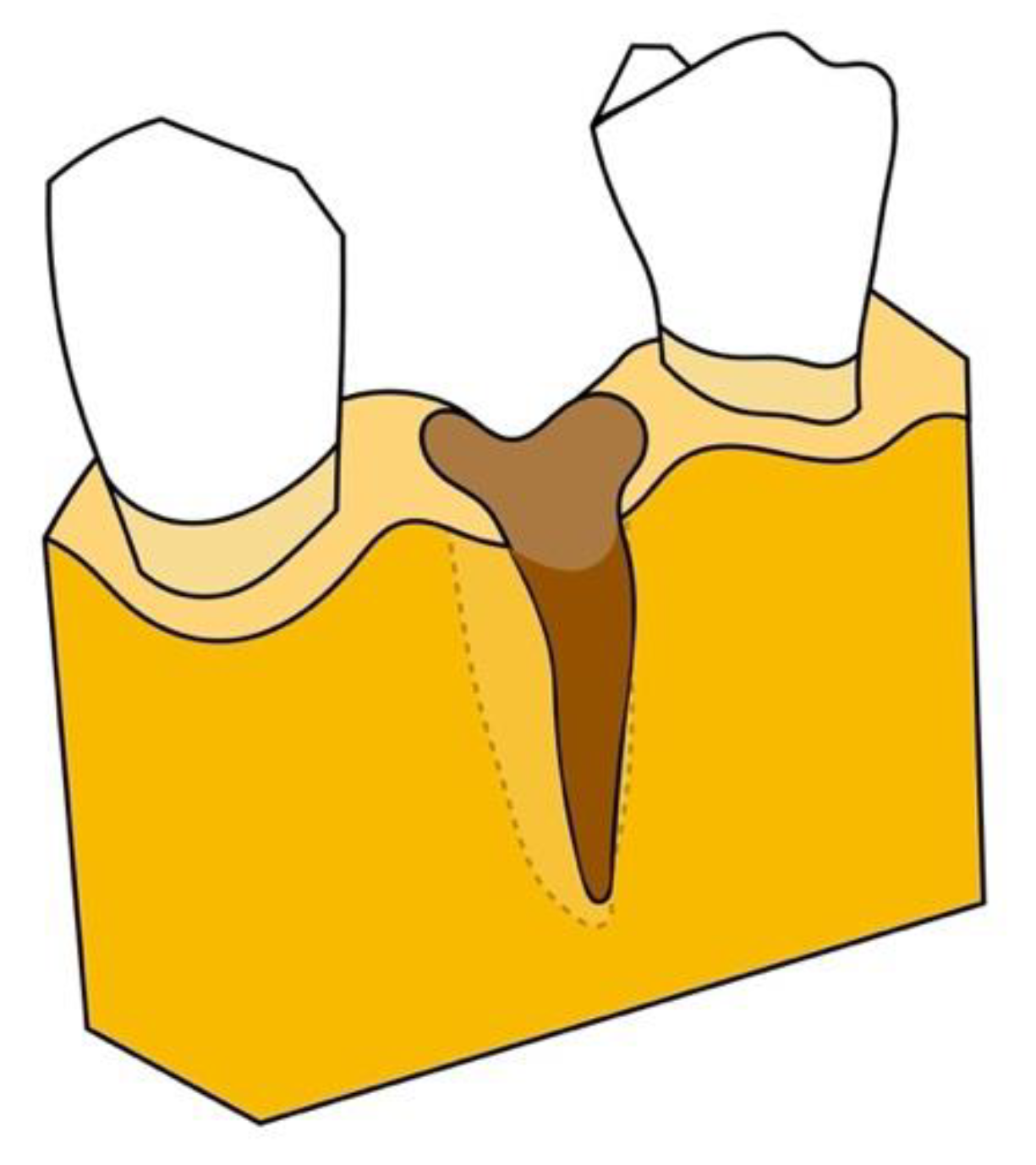
2.2. Implant Site Development
2.2.1. History
2.2.2. Advantages and Disadvantages
2.2.3. Indications and Contraindications
3. Biology of Forced Eruption
4. Methodology and Efficacy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Corruccini, R.S.; Pacciani, E. “Orthodontistry” and dental occlusion in Etruscans. Angle Orthod. 1989, 59, 61–64. [Google Scholar] [PubMed]
- Jacobson, A. DAI: The dental aesthetic index. Am. J. Orthod. Dentofac. Orthop. 1987, 92, 521–522. [Google Scholar] [CrossRef]
- Bach, N.; Baylard, J.-F.; Voyer, R. Orthodontic extrusion: Periodontal considerations and applications. J. Can. Dent. Assoc. 2004, 70, 775–780. [Google Scholar] [PubMed]
- Oppenheim, A. Artificial elongation of teeth. Am. J. Orthod. Oral Surg. 1940, 26, 931–940. [Google Scholar] [CrossRef]
- Heithersay, G.S. Combined endodontic-orthodontic treatment of transverse root fractures in the region of the alveolar crest. Oral Surg. Oral Med. Oral Pathol. 1973, 36, 404–415. [Google Scholar] [CrossRef]
- Brown, I.S. The effect of orthodontic therapy on certain types of periodontal defects. I. Clinical findings. J. Periodontol. 1973, 44, 742–756. [Google Scholar] [CrossRef] [PubMed]
- Ingber, J.S. Forced eruption: Part II. A method of treating nonrestorable teeth--Periodontal and restorative considerations. J. Periodontol. 1976, 47, 203–216. [Google Scholar] [CrossRef] [PubMed]
- Al-Hazaimeh, N.; Gutteridge, D.L. An in vitro study into the effect of the ferrule preparation on the fracture resistance of crowned teeth incorporating prefabricated post and composite core restorations. Int. Endod. J. 2001, 34, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Juloski, J.; Radovic, I.; Goracci, C.; Vulicevic, Z.R.; Ferrari, M. Ferrule effect: A literature review. J. Endod. 2012, 38, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Stankiewicz, N.; Wilson, P. The ferrule effect: A literature review. Int. Endod. J. 2002, 35, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Ingber, J.S. Forced eruption. I. A method of treating isolated one and two wall infrabony osseous defects-rationale and case report. J. Periodontol. 1974, 45, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Pontoriero, R.; Celenza, F., Jr.; Ricci, G.; Carnevale, G. Rapid extrusion with fiber resection: A combined orthodontic-periodontic treatment modality. Int. J. Periodontics Restor. Dent. 1987, 7, 30–43. [Google Scholar]
- Salama, H.; Salama, M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects. Int. J. Periodontics Restor. Dent. 1993, 13. [Google Scholar]
- Esposito, M.; Grusovin, M.G.; Felice, P.; Karatzopoulos, G.; Worthington, H.V.; Coulthard, P. The efficacy of horizontal and vertical bone augmentation procedures for dental implants: A Cochrane systematic review. Evid. Based Pract. Toward Optim. Clin. Outcomes 2010, 195–218. [Google Scholar] [CrossRef]
- Alsahhaf, A.; Att, W. Orthodontic extrusion for pre-implant site enhancement: Principles and clinical guidelines. J. Prosthodont. Res. 2016, 60, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Arun, K.V.; Shreemogana, S. Implant site development using forced eruption: A mini review. J. Indian Orthod. Soc. 2018, 52, 68–73. [Google Scholar] [CrossRef]
- Korayem, M.; Flores-Mir, C.; Nassar, U.; Olfert, K. Implant Site Development by Orthodontic Extrusion A Systematic Review. Angle Orthod. 2008, 78, 752–760. [Google Scholar] [CrossRef]
- Rosen, H.; Partida-Rivera, M. Iatrogenic fracture of roots reinforced with a cervical collar. Oper. Dent. 1986, 11, 46–50. [Google Scholar]
- Sorensen, J.A.; Engelman, M.J. Ferrule design and fracture resistance of endodontically treated teeth. J. Prosthet. Dent. 1990, 63, 529–536. [Google Scholar] [CrossRef]
- Carvalho, C.V.; Bauer, F.P.F.; Romito, G.A.; Pannuti, C.M.; De Micheli, G. Orthodontic extrusion with or without circumferential supracrestal fiberotomy and root planing. Int. J. Periodontics Restor. Dent. 2006, 26, 1–8. [Google Scholar]
- Johnson, G.K.; Sivers, J.E. Forced eruption in crown-lengthening procedures. J. Prosthet. Dent. 1986, 56, 424–427. [Google Scholar] [CrossRef]
- Kozlovsky, A.; Tal, H.; Lieberman, M. Forced eruption combined with gingival fiberotomy. A technique for clinical crown lengthening. J. Clin. Periodontol. 1988, 15, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Van Venrooy, J.R.; Yukna, R.A. Orthodontic extrusion of single-rooted teeth affected with advanced periodontal disease. Am. J. Orthod. 1985, 87, 67–74. [Google Scholar] [CrossRef]
- Minsk, L. Orthodontic tooth extrusion as an adjunct to periodontal therapy. Compend. Contin. Educ. Dent. 2000, 21, 768–770. [Google Scholar]
- Brindis, M.A.; Block, M.S. Orthodontic tooth extrusion to enhance soft tissue implant esthetics. J. Oral Maxillofac. Surg. 2009, 67, 49–59. [Google Scholar] [CrossRef]
- Block, M.S. Dental implants: The last 100 years. J. Oral Maxillofac. Surg. 2018, 76, 11–26. [Google Scholar] [CrossRef] [PubMed]
- Reitan, K. Clinical and histologic observations on tooth movement during and after orthodontic treatment. Am. J. Orthod. 1967, 53, 721–745. [Google Scholar] [CrossRef]
- Rokn, A.R.; Saffarpour, A.; Sadrimanesh, R.; Iranparvar, K.; Mahmoudzadeh, M.; Soolari, A. Implant site development by orthodontic forced eruption of nontreatable teeth: A case report. Open Dent. J. 2012, 6, 99–104. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cochran, D.L. A comparison of endosseous dental implant surfaces. J. Periodontol. 1999, 70, 1523–1539. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.L.; Wong, T.L.; Wong, M.C.; Lang, N.P. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin. Oral Implant Res. 2012, 23, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Chappuis, V.; Engel, O.; Reyes, M.; Shahim, K.; Nolte, L.-P.; Buser, D. Ridge alterations post-extraction in the esthetic zone: A 3D analysis with CBCT. J. Dent. Res. 2013, 92, 195S–201S. [Google Scholar] [CrossRef]
- Kang, P.Y.; Habib, R. Possible Complications With Implant Site Development Utilizing Orthodontic Extrusion: Three Case Reports. Compend. Contin. Educ. Dent. 2019, 40, 292–297. [Google Scholar] [PubMed]
- Simon, J.H.; Lythgoe, J.B.; Torabinejad, M. Clinical and histologic evaluation of extruded endodontically treated teeth in dogs. Oral Surg. Oral Med. Oral Pathol. 1980, 50, 361–371. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.W.; Larson, B.; Sarver, D.M. Contemporary Orthodontics-E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Hochman, M.N.; Chu, S.J.; Tarnow, D.P. Orthodontic extrusion for implant site development revisited: A new classification determined by anatomy and clinical outcomes. Semin. Orthod. 2014, 20, 208–227. [Google Scholar] [CrossRef]
- Kokich, V.G. Esthetics: The orthodontic-periodontic restorative connection. Semin. Orthod. 1996, 2, 21–30. [Google Scholar] [CrossRef]
- Stevens, B.H.; Levine, R.A. Forced eruption: A multidisciplinary approach for form, function, and biologic predictability. Compend. Contin. Educ. Dent. 1998, 19, 994–998. [Google Scholar]
- Nappen, D.; Kohlan, D. Orthodontic extrusion of premolar teeth: An improved technique. J. Prosthet. Dent. 1989, 61, 549–554. [Google Scholar] [CrossRef]
- Amato, F.; Mirabella, A.D.; Macca, U.; Tarnow, D.P. Implant site development by orthodontic forced extraction: A preliminary study. Int. J. Oral Maxillofac. Implant 2012, 27, 411–420. [Google Scholar]
- Berglundh, T.; Marinello, C.; Lindhe, J.; Thilander, B.; Liljenberg, B. Periodontal tissue reactions to orthodontic extrusion: An experimental study in the dog. J. Clin. Periodontol. 1991, 18, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Batenhorst, K.; Bowers, G.; Williams, J., Jr. Tissue changes resulting from facial tipping and extrusion of incisors in monkeys. J. Periodontol. 1974, 45, 660–668. [Google Scholar] [CrossRef] [PubMed]
- Chou, Y.H.; Du, J.K.; Chou, S.T.; Hu, K.F.; Tsai, C.C.; Ho, K.Y.; Wu, Y.M.; Ho, Y.P. An interdisciplinary treatment approach combining orthodontic forced eruption with immediate implant placement to achieve a satisfactory treatment outcome: A case report. Clin. Implant Dent. Relat. Res. 2013, 15, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Somar, M.; Mohadeb, J.V.; Huang, C. Predictability of Orthodontic Forced Eruption in Developing an Implant Site: A Systematic Review. J. Clin. Orthod. 2016, 50, 485–492. [Google Scholar] [PubMed]
- Keceli, H.G.; Guncu, M.B.; Atalay, Z.; Evginer, M.S. Forced eruption and implant site development in the aesthetic zone: A case report. Eur. J. Dent. 2014, 8, 269–275. [Google Scholar] [CrossRef] [PubMed]


| Advantages | Disadvantages |
|---|---|
| Non-invasive | Considerable occlusal reduction |
| Limits involvement of adjacent teeth | Endodontic therapy may be required |
| Preserves supporting bone | Prolonged treatment time |
| Improves esthetics | Minor periodontal surgery may still be indicated |
| Maintains crown-to-root ratio | Additional cost |
| Indications | Contraindications |
|---|---|
| Subgingival or intraosseous caries | Active periodontal inflammation |
| Isolated periodontal defects | Ankylosis |
| Horizontal fractures | Hypercementosis |
| Perforations | Root proximity |
| Internal and external root resorptions | Vertical root fracture |
| Chronic inflammatory lesions | |
| Risk of furcation exposure | |
| Poor crown-to-root ratio | |
| Insufficient prosthetic space |
| Advantages | Disadvantages |
|---|---|
| Non-invasive | Considerable occlusal reduction |
| Limits involvement of adjacent teeth | Endodontic therapy may be required |
| Increases soft and hard tissue volume | Prolonged treatment time |
| Improves esthetics and future emergence profile | Additional cost |
| Improves future crown-to-implant ratio | |
| May obviate additional grafting surgeries |
| Indications | Contraindications |
|---|---|
| Non-restorable teeth | Active periodontal inflammation |
| Large carious lesions | Ankylosis |
| Internal and external root resorptions | Hypercementosis |
| Perforations | Root proximity |
| Diagonal/horizontal fractures | Vertical root fracture |
| Type 1 and Type 2 extraction sites | Chronic inflammatory lesions |
| Type 3 extraction sites |
| Attached Gingiva Connection | Width of Attached Gingiva | Position of MGJ | Width of Soft Tissue | |
|---|---|---|---|---|
| Type 1 | Root and bone | Increases | No change | Increases |
| Type 2 | Root only | No change | Coronal | Increases |
| Type 3 | Neither | No change | No change | No change |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, G.; Yang, M.; Qali, M.; Wang, T.-J.; Li, C.; Chang, Y.-C. Clinical Considerations in Orthodontically Forced Eruption for Restorative Purposes. J. Clin. Med. 2021, 10, 5950. https://doi.org/10.3390/jcm10245950
Huang G, Yang M, Qali M, Wang T-J, Li C, Chang Y-C. Clinical Considerations in Orthodontically Forced Eruption for Restorative Purposes. Journal of Clinical Medicine. 2021; 10(24):5950. https://doi.org/10.3390/jcm10245950
Chicago/Turabian StyleHuang, Grace, Min Yang, Mohammad Qali, Tun-Jan Wang, Chenshuang Li, and Yu-Cheng Chang. 2021. "Clinical Considerations in Orthodontically Forced Eruption for Restorative Purposes" Journal of Clinical Medicine 10, no. 24: 5950. https://doi.org/10.3390/jcm10245950
APA StyleHuang, G., Yang, M., Qali, M., Wang, T.-J., Li, C., & Chang, Y.-C. (2021). Clinical Considerations in Orthodontically Forced Eruption for Restorative Purposes. Journal of Clinical Medicine, 10(24), 5950. https://doi.org/10.3390/jcm10245950







