The Association between Bisphenol A, Steroid Hormones, and Selected MicroRNAs Levels in Seminal Plasma of Men with Infertility
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Semen Analysis
2.3. BPA Measurement from the Seminal Plasma Samples
2.4. Biochemical Analyses
2.5. Total RNA Isolation
2.6. MicroRNA Analysis
2.7. Statistical Analysis
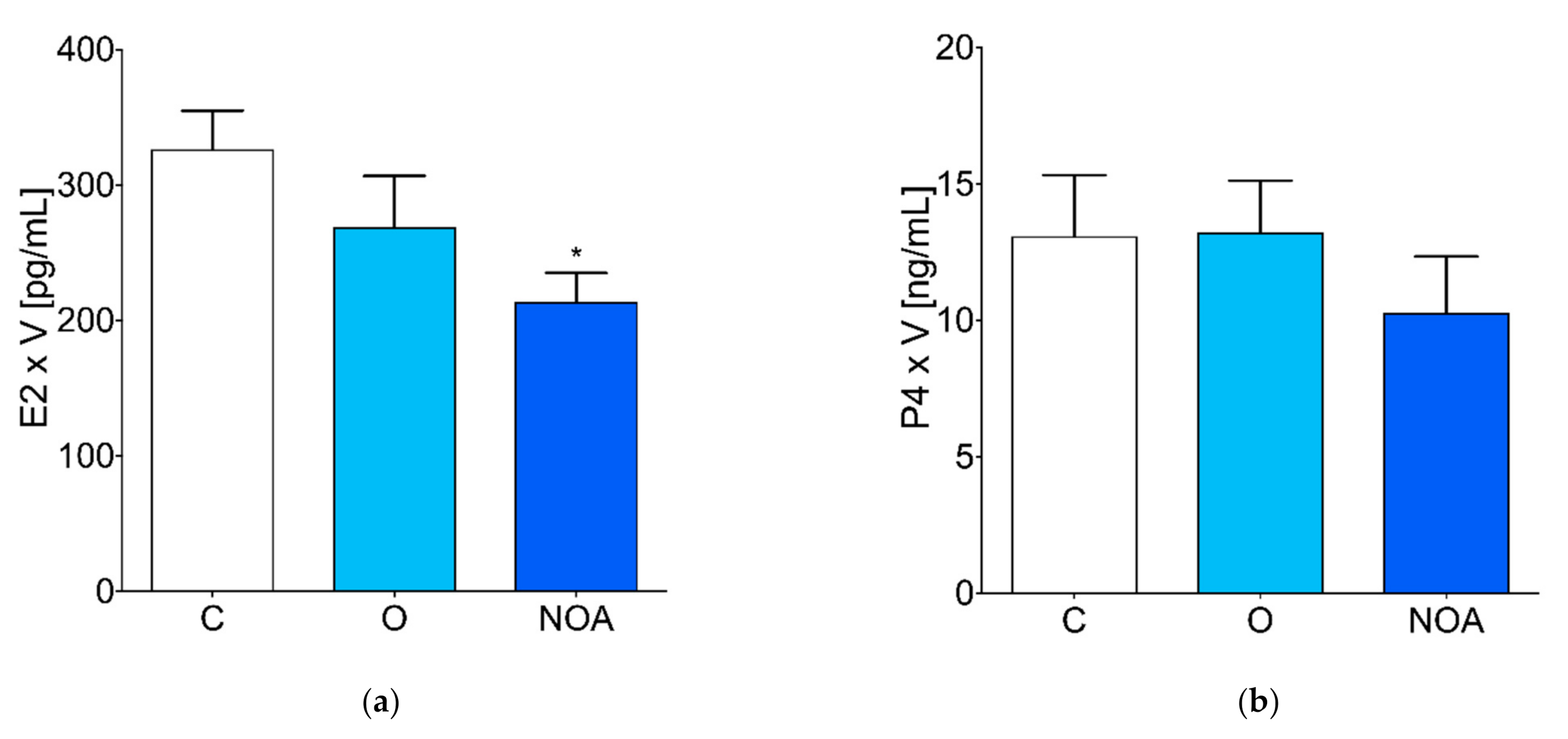
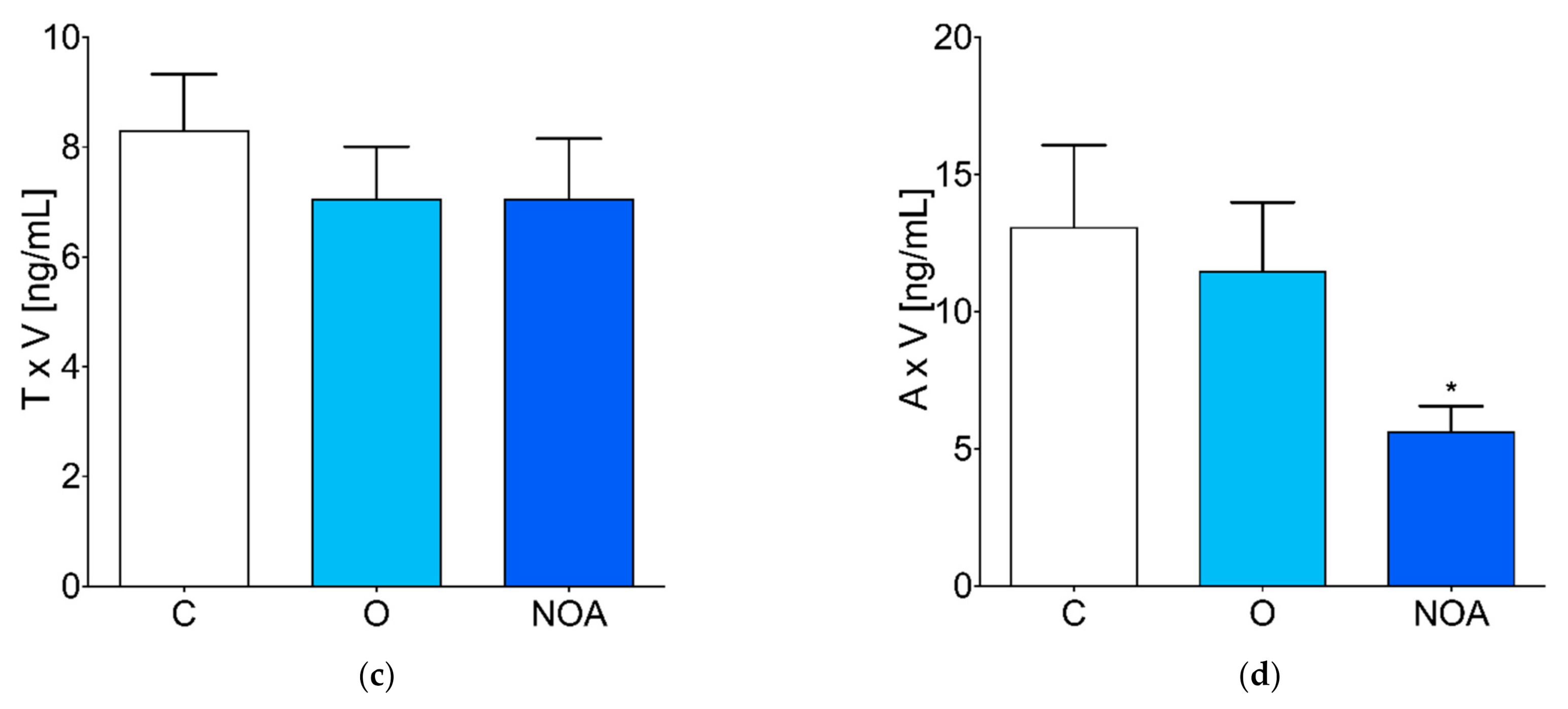
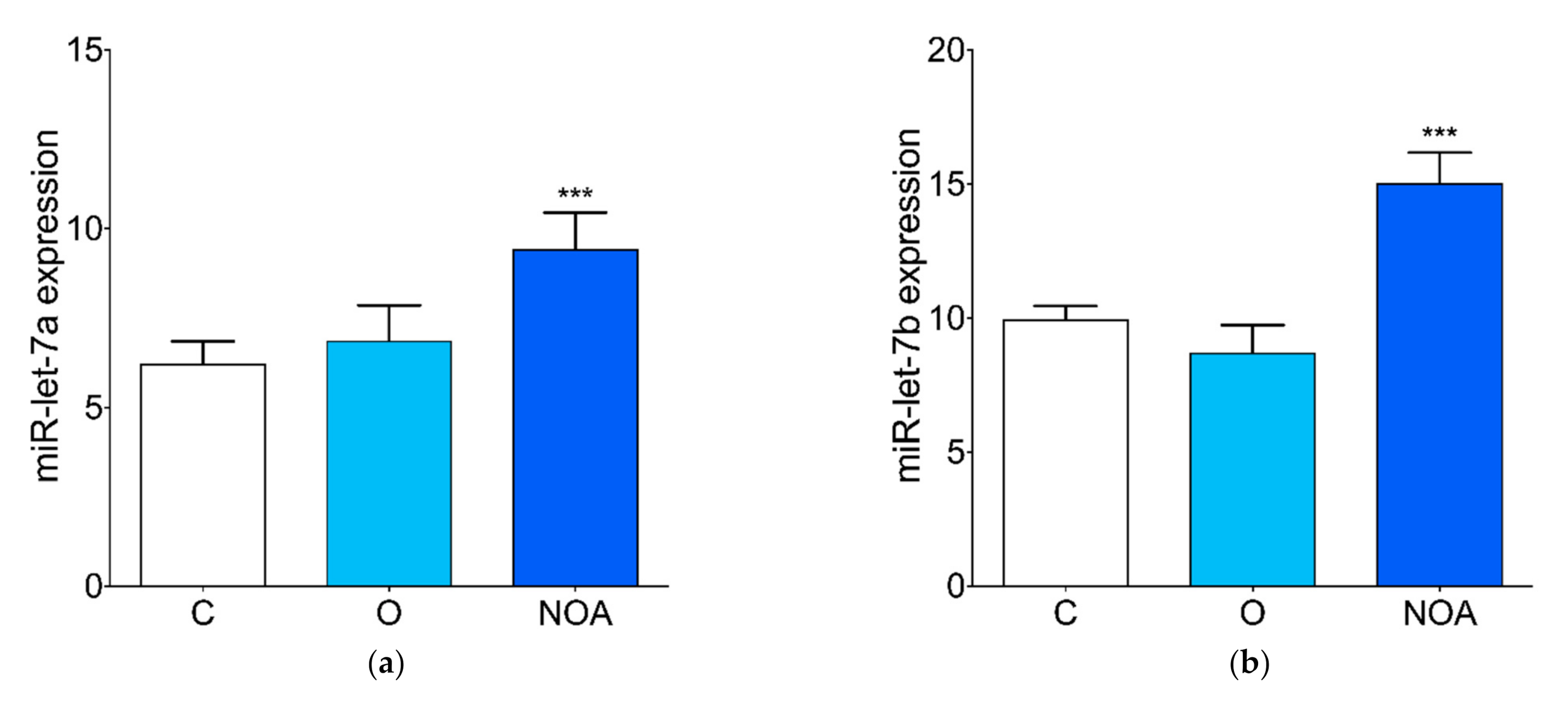
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sharpe, R.M.; Irvine, D.S. How Strong Is the Evidence of a Link between Environmental Chemicals and Adverse Effects on Human Reproductive Health? BMJ 2004, 328, 447–451. [Google Scholar] [CrossRef] [Green Version]
- Rochester, J.R. Bisphenol A and Human Health: A Review of the Literature. Reprod. Toxicol. 2013, 42, 132–155. [Google Scholar] [CrossRef]
- Vandenberg, L.N.; Hauser, R.; Marcus, M.; Olea, N.; Welshons, W.V. Human Exposure to Bisphenol A (BPA). Reprod. Toxicol. 2007, 24, 139–177. [Google Scholar] [CrossRef] [PubMed]
- Toner, F.; Allan, G.; Dimond, S.S.; Waechter, J.M.; Beyer, D. In Vitro Percutaneous Absorption and Metabolism of Bisphenol A (BPA) through Fresh Human Skin. Toxicol. Vitr. 2018, 47, 147–155. [Google Scholar] [CrossRef]
- Hines, C.J.; Jackson, M.V.; Christianson, A.L.; Clark, J.C.; Arnold, J.E.; Pretty, J.R.; Deddens, J.A. Air, Hand Wipe, and Surface Wipe Sampling for Bisphenol A (BPA) among Workers in Industries that Manufacture and Use BPA in the United States. J. Occup. Environ. Hyg. 2017, 14, 882–897. [Google Scholar] [CrossRef] [PubMed]
- Ikezuki, Y.; Tsutsumi, O.; Takai, Y.; Kamei, Y.; Taketani, Y. Determination of Bisphenol A Concentrations in Human Biological Fluids Reveals Significant Early Prenatal Exposure. Hum. Reprod. 2002, 17, 2839–2841. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vitku, J.; Sosvorova, L.; Chlupacova, T.; Hampl, R.; Hill, M.; Sobotka, V.; Heracek, J.; Bicikova, M.; Stárka, L. Differences in Bisphenol A and Estrogen Levels in the Plasma and Seminal Plasma of Men with Different Degrees of Infertility. Physiol. Res. 2015, 64, S303–S311. [Google Scholar] [CrossRef]
- Lukasiewicz, M.; Czerniecki, J.; Ponikwicka-Tyszko, D.; Sztachelska, M.; Hryniewicka, M.; Nalewajko-Sieliwoniuk, E.; Wiczkowski, W.; Banaszewska, B.; Milewski, R.; Toppari, J.; et al. Placenta Is Capable of Protecting the Male Fetus from Exposure to Environmental Bisphenol A. Expo. Health 2020, 13, 1–14. [Google Scholar] [CrossRef]
- LaRocca, J.; Boyajian, A.; Brown, C.; Smith, S.D.; Hixon, M. Effects of In Utero Exposure to Bisphenol A or Diethylstilbestrol on the Adult Male Reproductive System. Birth Defects Res. Part B Dev. Reprod. Toxicol. 2011, 92, 526–533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, P.; Wang, X.; Chang, F.; Bai, Y.; Li, Y.; Zhou, R.; Chen, L. Low Dose Bisphenol A Impairs Spermatogenesis by Suppressing Reproductive Hormone Production and Promoting Germ Cell Apoptosis in Adult Rats. J. Biomed. Res. 2013, 27, 135–144. [Google Scholar] [CrossRef]
- Mendiola, J.; Jørgensen, N.; Andersson, A.-M.; Calafat, A.M.; Ye, X.; Redmon, J.B.; Drobnis, E.Z.; Wang, C.; Sparks, A.; Thurston, S.W.; et al. Are Environmental Levels of Bisphenol A Associated with Reproductive Function in Fertile Men? Environ. Health Perspect. 2010, 118, 1286–1291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, D.-K.; Zhou, Z.; Miao, M.; He, Y.; Wang, J.; Ferber, J.; Herrinton, L.J.; Gao, E.; Yuan, W. Urine Bisphenol-A (BPA) Level in Relation to Semen Quality. Fertil. Steril. 2011, 95, 625–630.e4. [Google Scholar] [CrossRef]
- Lassen, T.H.; Frederiksen, H.; Jensen, T.K.; Petersen, J.H.; Joensen, U.N.; Main, K.M.; Skakkebaek, N.E.; Juul, A.; Jørgensen, N.; Andersson, A.-M. Urinary Bisphenol A Levels in Young Men: Association with Reproductive Hormones and Semen Quality. Environ. Health Perspect. 2014, 122, 478–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galloway, T.; Cipelli, R.; Guralnik, J.; Ferrucci, L.; Bandinelli, S.; Corsi, A.M.; Money, C.; McCormack, P.; Melzer, D. Daily Bisphenol A Excretion and Associations with Sex Hormone Concentrations: Results from the InCHIANTI Adult Population Study. Environ. Health Perspect. 2010, 118, 1603–1608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meeker, J.D.; Calafat, A.M.; Hauser, R. Urinary Bisphenol A Concentrations in Relation to Serum Thyroid and Reproductive Hormone Levels in Men from an Infertility Clinic. Environ. Sci. Technol. 2010, 44, 1458–1463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Q.; Miao, M.; Ran, M.; Ding, L.; Bai, L.; Wu, T.; Yuan, W.; Gao, E.; Wang, J.; Li, G.; et al. Serum Bisphenol-A concentration and Sex Hormone Levels in Men. Fertil. Steril. 2013, 100, 478–482. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, W.; Wu, K.; Wang, Y.; Zhu, H.; Deng, Z.; Peng, L.; Zhu, G. Association of Serum Bisphenol-A Concentration and Male Reproductive Function among Exposed Workers. Arch. Environ. Contam. Toxicol. 2014, 68, 38–45. [Google Scholar] [CrossRef]
- Kim, E.J.; Lee, D.; Chung, B.C.; Pyo, H.; Lee, J. Association between Urinary Levels of Bisphenol-A and Estrogen Metabolism in Korean Adults. Sci. Total Environ. 2014, 470–471, 1401–1407. [Google Scholar] [CrossRef]
- Nakamura, D.; Yanagiba, Y.; Duan, Z.; Ito, Y.; Okamura, A.; Asaeda, N.; Tagawa, Y.; Li, C.; Taya, K.; Zhang, S.-Y. Bisphenol A May Cause Testosterone Reduction by Adversely Affecting Both Testis and Pituitary Systems Similar to Estradiol. Toxicol. Lett. 2010, 194, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Gould, J.C.; Leonard, L.S.; Maness, S.C.; Wagner, B.L.; Conner, K.; Zacharewski, T.; Safe, S.; McDonnell, D.P.; Gaido, K.W. Bisphenol A Interacts with the Estrogen Receptor α in a Distinct Manner from Estradiol. Mol. Cell. Endocrinol. 1998, 142, 203–214. [Google Scholar] [CrossRef]
- Alonso-Magdalena, P.; Ropero, A.B.; Soriano, S.; García-Arévalo, M.; Ripoll, C.; Fuentes, E.; Quesada, I.; Nadal, Á. Bisphenol-A Acts as a Potent Estrogen via Non-Classical Estrogen Triggered Pathways. Mol. Cell. Endocrinol. 2012, 355, 201–207. [Google Scholar] [CrossRef]
- Lee, H.J.; Chattopadhyay, S.; Gong, E.-Y.; Ahn, R.S.; Lee, K. Antiandrogenic Effects of Bisphenol A and Nonylphenol on the Function of Androgen Receptor. Toxicol. Sci. 2003, 75, 40–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okada, H.; Tokunaga, T.; Liu, X.; Takayanagi, S.; Matsushima, A.; Shimohigashi, Y. Direct Evidence Revealing Structural Elements Essential for the High Binding Ability of Bisphenol A to Human Estrogen-Related Receptor-γ. Environ. Health Perspect. 2008, 116, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, K.; Tagami, T.; Akamizu, T.; Usui, T.; Saijo, M.; Kanamoto, N.; Hataya, Y.; Shimatsu, A.; Kuzuya, H.; Nakao, K. Thyroid Hormone Action Is Disrupted by Bisphenol A as an Antagonist. J. Clin. Endocrinol. Metab. 2002, 87, 5185–5190. [Google Scholar] [CrossRef]
- Sargis, R.M.; Johnson, D.N.; Choudhury, R.A.; Brady, M.J. Environmental Endocrine Disruptors Promote Adipogenesis in the 3T3-L1 Cell Line through Glucocorticoid Receptor Activation. Obesity 2010, 18, 1283–1288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skinner, M.K. Environmental Epigenomics and Disease Susceptibility. EMBO Rep. 2011, 12, 620–622. [Google Scholar] [CrossRef] [Green Version]
- Tilghman, S.L.; Bratton, M.; Segar, H.C.; Martin, E.C.; Rhodes, L.; Li, M.; McLachlan, J.A.; Wiese, T.E.; Nephew, K.P.; Burow, M.E. Endocrine Disruptor Regulation of MicroRNA Expression in Breast Carcinoma Cells. PLoS ONE 2012, 7, e32754. [Google Scholar] [CrossRef] [PubMed]
- Berezikov, E. Evolution of MicroRNA Diversity and Regulation in Animals. Nat. Rev. Genet. 2011, 12, 846–860. [Google Scholar] [CrossRef]
- Bartel, D.P. MicroRNAs: Target Recognition and Regulatory Functions. Cell 2009, 136, 215–233. [Google Scholar] [CrossRef] [Green Version]
- Salas-Huetos, A.; James, E.R.; Aston, K.I.; Carrell, D.T.; Jenkins, T.G.; Yeste, M. The Role of miRNAs in Male Human Reproduction: A Systematic Review. Andrology 2019, 8, 7–26. [Google Scholar] [CrossRef] [Green Version]
- Mokánszki, A.; Molnár, Z.; Tóthné, E.V.; Bodnár, B.; Jakab, A.; Bálint, B.L.; Balogh, I. Altered MicroRNAs Expression Levels of Sperm and Seminal Plasma in Patients with Infertile Ejaculates Compared with Normozoospermic Males. Hum. Fertil. 2019, 23, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Katchy, A.; Williams, C. Expression Profiles of Estrogen-Regulated MicroRNAs in Breast Cancer Cells. In Estrogen Receptors. Methods in Molecular Biology; Humana Press: New York, NY, USA, 2016; Volume 1366, pp. 373–393. [Google Scholar] [CrossRef] [Green Version]
- Schraml, E.; Hackl, M.; Grillari, J. MicroRNAs and Toxicology: A Love Marriage. Toxicol. Rep. 2017, 4, 634–636. [Google Scholar] [CrossRef]
- Kim, J.H.; Cho, Y.H.; Hong, Y.-C. MicroRNA Expression in Response to Bisphenol A Is Associated with High Blood Pressure. Environ. Int. 2020, 141, 105791. [Google Scholar] [CrossRef]
- Bhat-Nakshatri, P.; Wang, G.; Collins, N.R.; Thomson, M.J.; Geistlinger, T.R.; Carroll, J.S.; Brown, M.; Hammond, S.; Srour, E.F.; Liu, Y.; et al. Estradiol-Regulated MicroRNAs Control Estradiol Response in Breast Cancer Cells. Nucleic Acids Res. 2009, 37, 4850–4861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sørensen, A.; Wissing, M.L.; Englund, A.L.M.; Dalgaard, L. MicroRNA Species in Follicular Fluid Associating with Polycystic Ovary Syndrome and Related Intermediary Phenotypes. J. Clin. Endocrinol. Metab. 2016, 101, 1579–1589. [Google Scholar] [CrossRef] [Green Version]
- Manfo, F.P.T.; Jubendradass, R.; Nantia, E.A.; Moundipa, P.F.; Mathur, P.P. Adverse Effects of Bisphenol A on Male Reproductive Function. In Reviews of Environmental Contamination and Toxicology Volume 228. Reviews of Environmental Contamination and Toxicology (Continuation of Residue Reviews); Springer: Cham, Switzerland, 2013; pp. 57–82. [Google Scholar] [CrossRef]
- Vitku, J.; Heracek, J.; Sosvorova, L.; Hampl, R.; Chlupacova, T.; Hill, M.; Sobotka, V.; Bicikova, M.; Stárka, L. Associations of Bisphenol A and Polychlorinated Biphenyls with Spermatogenesis and Steroidogenesis in Two Biological Fluids from MEN Attending an Infertility Clinic. Environ. Int. 2016, 89–90, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Li, D.-K.; Zhou, Z.; Miao, M.; He, Y.; Qing, D.; Wu, T.; Wang, J.; Weng, X.; Ferber, J.; Herrinton, L.J.; et al. Relationship Between Urine Bisphenol-A Level and Declining Male Sexual Function. J. Androl. 2010, 31, 500–506. [Google Scholar] [CrossRef]
- Meeker, J.D.; Yang, T.; Ye, X.; Calafat, A.M.; Hauser, R. Urinary Concentrations of Parabens and Serum Hormone Levels, Semen Quality Parameters, and Sperm DNA Damage. Environ. Health Perspect. 2011, 119, 252–257. [Google Scholar] [CrossRef] [Green Version]
- Goldstone, A.E.; Chen, Z.; Perry, M.J.; Kannan, K.; Louis, G.M. Urinary Bisphenol A and Semen Quality, the LIFE Study. Reprod. Toxicol. 2015, 51, 7–13. [Google Scholar] [CrossRef]
- La Rocca, C.; Tait, S.; Guerranti, C.; Busani, L.; Ciardo, F.; Bergamasco, B.; Perra, G.; Mancini, F.R.; Marci, R.; Bordi, G.; et al. Exposure to Endocrine Disruptors and Nuclear Receptors Gene Expression in Infertile and Fertile Men from Italian Areas with Different Environmental Features. Int. J. Environ. Res. Public Health 2015, 12, 12426–12445. [Google Scholar] [CrossRef] [Green Version]
- Lian, J.; Zhang, X.; Tian, H.; Liang, N.; Wang, Y.; Liang, C.; Li, X.; Sun, F. Altered MicroRNA Expression in Patients with Non-Obstructive Azoospermia. Reprod. Biol. Endocrinol. 2009, 7, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.; Yang, C.; Chen, X.; Yao, B.; Yang, C.; Zhu, C.; Li, L.; Wang, J.; Li, X.; Shao, Y.; et al. Altered Profile of Seminal Plasma MicroRNAs in the Molecular Diagnosis of Male Infertility. Clin. Chem. 2011, 57, 1722–1731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, W.; Hu, Z.; Qin, Y.; Dong, J.; Dai, J.; Lu, C.; Zhang, W.; Shen, H.; Xia, Y.; Wang, X. Seminal Plasma MicroRNAs: Potential Biomarkers for Spermatogenesis Status. Mol. Hum. Reprod. 2012, 18, 489–497. [Google Scholar] [CrossRef]
- Jung, Y.H.; Gupta, M.K.; Shin, J.Y.; Uhm, S.J.; Lee, H.T. MicroRNA Signature in Testes-Derived Male Germ-Line Stem Cells. Mol. Hum. Reprod. 2010, 16, 804–810. [Google Scholar] [CrossRef]
- Zhou, R.; Wang, R.; Qin, Y.; Ji, J.; Xu, M.; Wu, W.; Chen, M.; Wu, D.; Song, L.; Shen, H.; et al. Mitochondria-Related miR-151a-5p Reduces Cellular ATP Production by Targeting CYTB in Asthenozoospermia. Sci. Rep. 2015, 5, 17743. [Google Scholar] [CrossRef] [Green Version]
- Muñoz, X.; Mata, A.; Bassas, L.; Larriba, S. Altered miRNA Signature of Developing Germ-Cells in Infertile Patients Relates to the Severity of Spermatogenic Failure and Persists in Spermatozoa. Sci. Rep. 2015, 5, 17991. [Google Scholar] [CrossRef] [Green Version]
- Veiga-Lopez, A.; Luense, L.J.; Christenson, L.K.; Padmanabhan, V. Developmental Programming: Gestational Bisphenol-A Treatment Alters Trajectory of Fetal Ovarian Gene Expression. Endocrinology 2013, 154, 1873–1884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, S.; Mutlu, L.; Zhou, Y.; Taylor, H.S. Aromatase Inhibitor Regulates Let-7 Expression and Let-7f-Induced Cell Migration in Endometrial Cells from Women with Endometriosis. Fertil. Steril. 2016, 106, 673–680. [Google Scholar] [CrossRef] [Green Version]


| Characteristics | Control (n = 50) | Oligoasthenotera-Tozoospermia (n = 46) | Azoospermia (n = 20) | p-Value |
| Age (years) | 31.30 ± 0.77 | 31.36 ± 0.86 | 31.20 ± 1.22 | 0.966 |
| BMI | 23.92 ± 0.35 | 23.69 ± 0.34 | 23.3 ± 0.52 | 0.608 |
| Volume | 4.01 ± 0.17 | 4.32 ± 0.32 | 3.75 ± 0.26 | 0.675 |
| Sperm concentration (×106/mL) | 42.56 ± 4.93 | 5.60 ± 0.72 | 0 | 0.0001 |
| Total sperm concentration | 165.85 ± 19.80 | 21.28 ± 2.85 | 0 | 0.0001 |
| Total motility (%) | 74.02 ± 1.83 | 49.03 ± 3.02 | 0 | 0.0001 |
| Progressive motility (%) | 51.45 ± 2.04 | 28.84 ± 2.54 | 0 | 0.0001 |
| Normal morphology (%) | 12.20 ± 1.26 | 3.72 ± 0.04 | 0 | 0.0001 |
| BPA | ||
|---|---|---|
| Parameter | r | p-value |
| Sperm concentration | −0.232 | 0.01 |
| Total sperm concentration | −0.22 | 0.02 |
| Total motility | −0.148 | 0.11 |
| Progressive motility | −0.068 | 0.47 |
| Normal morphology | −0.193 | 0.04 |
| E2 | −0.146 | 0.12 |
| P4 | −0.061 | 0.51 |
| T | −0.001 | 0.99 |
| A | −0.125 | 0.18 |
| miR-let-7a | 0.189 | 0.04 |
| miR-let-7b | 0.105 | 0.26 |
| miR-let-7c | 0.249 | 0.007 |
| miR-518f | −0.236 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palak, E.; Lebiedzińska, W.; Anisimowicz, S.; Sztachelska, M.; Pierzyński, P.; Wiczkowski, W.; Żelazowska-Rutkowska, B.; Niklińska, G.N.; Ponikwicka-Tyszko, D.; Wołczyński, S. The Association between Bisphenol A, Steroid Hormones, and Selected MicroRNAs Levels in Seminal Plasma of Men with Infertility. J. Clin. Med. 2021, 10, 5945. https://doi.org/10.3390/jcm10245945
Palak E, Lebiedzińska W, Anisimowicz S, Sztachelska M, Pierzyński P, Wiczkowski W, Żelazowska-Rutkowska B, Niklińska GN, Ponikwicka-Tyszko D, Wołczyński S. The Association between Bisphenol A, Steroid Hormones, and Selected MicroRNAs Levels in Seminal Plasma of Men with Infertility. Journal of Clinical Medicine. 2021; 10(24):5945. https://doi.org/10.3390/jcm10245945
Chicago/Turabian StylePalak, Ewelina, Weronika Lebiedzińska, Sławomir Anisimowicz, Maria Sztachelska, Piotr Pierzyński, Wiesław Wiczkowski, Beata Żelazowska-Rutkowska, Gabriella Nicole Niklińska, Donata Ponikwicka-Tyszko, and Sławomir Wołczyński. 2021. "The Association between Bisphenol A, Steroid Hormones, and Selected MicroRNAs Levels in Seminal Plasma of Men with Infertility" Journal of Clinical Medicine 10, no. 24: 5945. https://doi.org/10.3390/jcm10245945
APA StylePalak, E., Lebiedzińska, W., Anisimowicz, S., Sztachelska, M., Pierzyński, P., Wiczkowski, W., Żelazowska-Rutkowska, B., Niklińska, G. N., Ponikwicka-Tyszko, D., & Wołczyński, S. (2021). The Association between Bisphenol A, Steroid Hormones, and Selected MicroRNAs Levels in Seminal Plasma of Men with Infertility. Journal of Clinical Medicine, 10(24), 5945. https://doi.org/10.3390/jcm10245945






