Correlation between Electrophysiological Change and Facial Function in Parotid Surgery Patients
Abstract
:1. Introduction
2. Materials and Methods
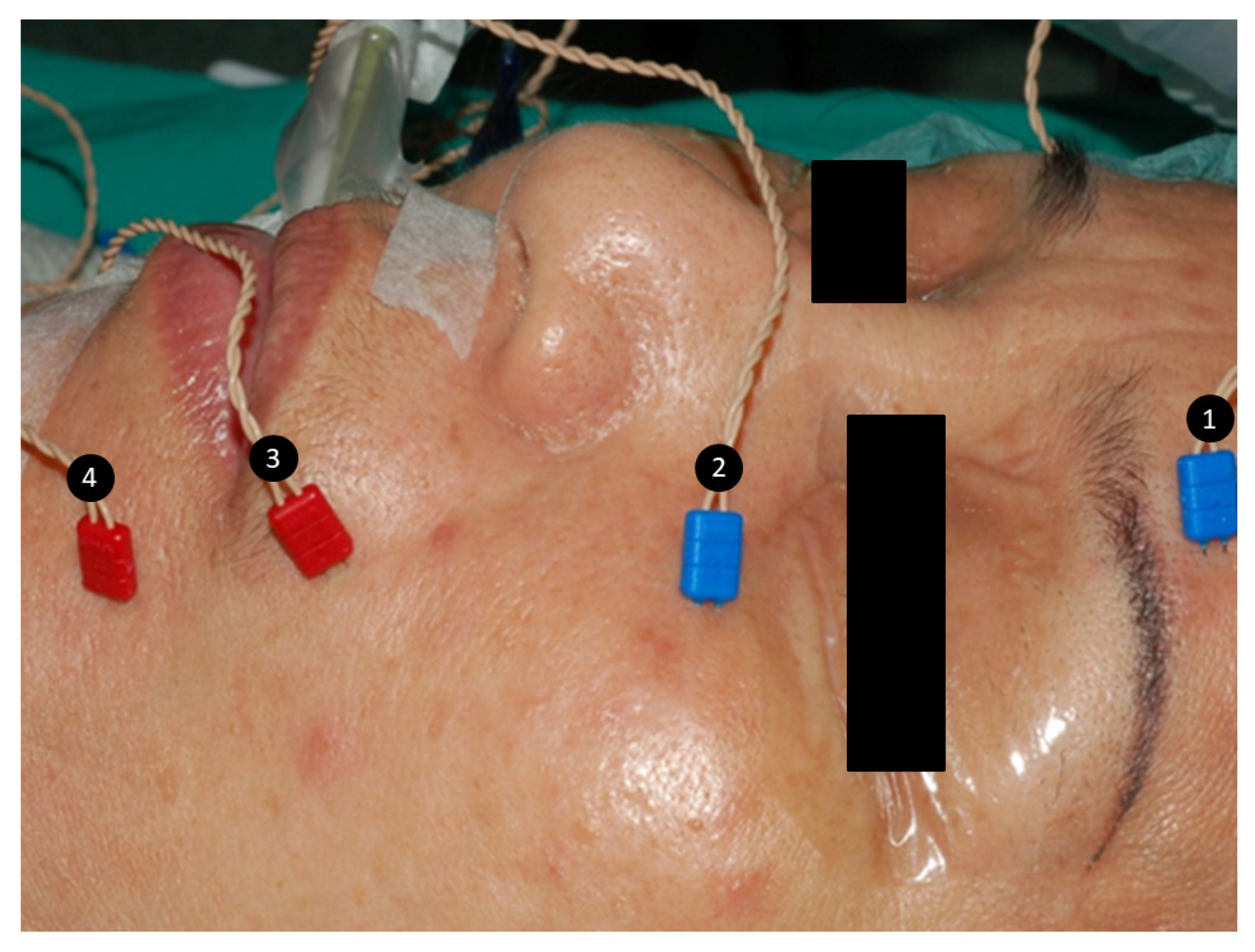
2.1. General Anesthesia and Facial Nerve Monitoring Setup
2.2. Evaluation of FN Function before and after FN Branch Dissection
2.3. Assessment of Facial Function
3. Results
4. Discussion
- (1)
- The lack of a control group, good statistical analysis, detailed data regarding type of parotidectomy, tumor size, tumor location and extent of parotid resection and FN dissection were the major shortcoming of this study. However, this study was focused on the change of EMG amplitude and the risk of facial dysfunction after facial nerve dissection with our standard FNM procedure and facial function grading system. Our results showed that regional facial weakness occurred in 13 of 16 signals (81%) with >50% amplitude decrease. An amplitude decrease >50% in an FN branch is associated with a high incidence of dysfunction in the corresponding facial region.
- (2)
- Defining an unchanged amplitude after FN dissection is difficult. On each channel, some difference of EMG amplitude was observed between two consecutive stimulations. Therefore, an EMG amplitude change of ±10% may be interpreted as a normal variation of the monitoring system.
- (3)
- This study focused on cases with integral continuity of FN branches after parotid tumor resection. Future studies should investigate the outcomes after intraoperative transection of FN branch.
- (4)
- The cases with large amplitude decrease were limited, although the results showed a high incidence of facial dysfunction in the signals with amplitude decrease >50%. Further study with large volume in multiple centers is necessary.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Brien, C.J. Current management of benign parotid tumors—The role of limited superficial parotidectomy. Head Neck 2003, 25, 946–952. [Google Scholar] [CrossRef]
- Terrell, J.E.; Kileny, P.R.; Yian, C.; Esclamado, R.M.; Bradford, C.R.; Pillsbury, M.S.; Wolf, G.T. Clinical outcome of continuous facial nerve monitoring during primary parotidectomy. Arch. Otolaryngol.—Head Neck Surg. 1997, 123, 1081–1087. [Google Scholar] [CrossRef] [PubMed]
- Eisele, D.W.; Wang, S.J.; Orloff, L.A. Electrophysiologic facial nerve monitoring during parotidectomy. Head Neck 2010, 32, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Dulguerov, P.; Marchal, F.; Lehmann, W. Postparotidectomy facial nerve paralysis: Possible etiologic factors and results with routine facial nerve monitoring. Laryngoscope 1999, 109, 754–762. [Google Scholar] [CrossRef]
- Guntinas-Lichius, O.; Gabriel, B.; Peter Klussmann, J. Risk of facial palsy and severe Frey’s syndrome after conservative parotidectomy for benign disease: Analysis of 610 operations. Acta Oto-Laryngol. 2006, 126, 1104–1109. [Google Scholar] [CrossRef] [PubMed]
- Mehle, M.E.; Kraus, D.H.; Wood, B.G.; Benninger, M.S.; Eliachar, I.; Levine, H.L.; Tucker, H.M.; Lavertu, P. Facial nerve morbidity following parotid surgery for benign disease: The Cleveland Clinic Foundation experience. Laryngoscope 1993, 103, 386–388. [Google Scholar] [CrossRef] [PubMed]
- Bron, L.P.; O’Brien, C.J. Facial nerve function after parotidectomy. Arch. Otolaryngol.—Head Neck Surg. 1997, 123, 1091–1096. [Google Scholar] [CrossRef]
- Witt, R.L. Facial nerve function after partial superficial parotidectomy: An 11-year review (1987–1997). Otolaryngol. Head Neck Surg. 1999, 121, 210–213. [Google Scholar] [CrossRef]
- Mra, Z.; Komisar, A.; Blaugrund, S.M. Functional facial nerve weakness after surgery for benign parotid tumors: A multivariate statistical analysis. Head Neck 1993, 15, 147–152. [Google Scholar] [CrossRef]
- Anjum, K.; Revington, P.; Irvine, G. Superficial parotidectomy: Antegrade compared with modified retrograde dissections of the facial nerve. Br. J. Oral Maxillofac. Surg. 2008, 46, 433–434. [Google Scholar] [CrossRef]
- Laccourreye, H.; Laccourreye, O.; Cauchois, R.; Jouffre, V.; Ménard, M.; Brasnu, D. Total conservative parotidectomy for primary benign pleomorphic adenoma of the parotid gland: A 25-year experience with 229 patients. Laryngoscope 1994, 104, 1487–1494. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; Kim, B.Y.; Kim, H.; Lee, E.; Park, W.; Choi, S.; Chung, M.K.; Son, Y.-I.; Baek, C.-H.; Jeong, H.-S. Incidence of postoperative facial weakness in parotid tumor surgery: A tumor subsite analysis of 794 parotidectomies. BMC Surg. 2019, 19, 199. [Google Scholar] [CrossRef] [Green Version]
- O’Regan, B.; Bharadwaj, G.; Bhopal, S.; Cook, V. Facial nerve morbidity after retrograde nerve dissection in parotid surgery for benign disease: A 10-year prospective observational study of 136 cases. Br. J. Oral Maxillofac. Surg. 2007, 45, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Graciano, A.J.; Fischer, C.A.; Coelho, G.V.; Steck, J.H.; Paschoal, J.R.; Chone, C.T. Facial nerve dysfunction after superficial parotidectomy with or without continuous intraoperative electromyographic neuromonitoring: A prospective randomized pilot study. Eur. Arch. Oto-Rhino-Laryngol. 2018, 275, 2861–2868. [Google Scholar] [CrossRef]
- Ballivet-de Régloix, S.; Grinholtz-Haddad, J.; Maurin, O.; Genestier, L.; Lisan, Q.; Pons, Y. Facial nerve monitoring during parotidectomy: A two-center retrospective study. Iran. J. Otorhinolaryngol. 2016, 28, 255. [Google Scholar]
- Grosheva, M.; Klussmann, J.P.; Grimminger, C.; Wittekindt, C.; Beutner, D.; Pantel, M.; Volk, G.F.; Guntinas-Lichius, O. Electromyographic facial nerve monitoring during parotidectomy for benign lesions does not improve the outcome of postoperative facial nerve function: A prospective two-center trial. Laryngoscope 2009, 119, 2299–2305. [Google Scholar] [CrossRef]
- Witt, R.L. Facial nerve monitoring in parotid surgery: The standard of care? Otolaryngol.—Head Neck Surg. 1998, 119, 468–470. [Google Scholar] [CrossRef]
- Savvas, E.; Hillmann, S.; Weiss, D.; Koopmann, M.; Rudack, C.; Alberty, J. Association between facial nerve monitoring with postoperative facial paralysis in parotidectomy. JAMA Otolaryngol.—Head Neck Surg. 2016, 142, 828–833. [Google Scholar] [CrossRef] [Green Version]
- Sood, A.J.; Houlton, J.J.; Nguyen, S.A.; Gillespie, M.B. Facial nerve monitoring during parotidectomy: A systematic review and meta-analysis. Otolaryngol.—Head Neck Surg. 2015, 152, 631–637. [Google Scholar] [CrossRef]
- Ozturk, K.; Akyildiz, S.; Gode, S.; Turhal, G.; Gursan, G.; Kirazli, T. The effect of partial superficial parotidectomy on amplitude, latency and threshold of facial nerve stimulation. Arch. Oto-Rhino-Laryngol. 2016, 273, 1527–1531. [Google Scholar] [CrossRef] [PubMed]
- Sajisevi, M. Indications for Facial Nerve Monitoring During Parotidectomy. Otolaryngol. Clin. N. Am. 2021, 54, 489–496. [Google Scholar] [CrossRef]
- Chiesa-Estomba, C.M.; Larruscain-Sarasola, E.; Lechien, J.R.; Mouawad, F.; Calvo-Henriquez, C.; Diom, E.S.; Ramirez, A.; Ayad, T. Facial nerve monitoring during parotid gland surgery: A systematic review and meta-analysis. Arch. Oto-Rhino-Laryngol. 2021, 278, 933–943. [Google Scholar] [CrossRef]
- Meier, J.D.; Wenig, B.L.; Manders, E.C.; Nenonene, E.K. Continuous intraoperative facial nerve monitoring in predicting postoperative injury during parotidectomy. Laryngoscope 2006, 116, 1569–1572. [Google Scholar] [CrossRef]
- Guntinas-Lichius, O.; Eisele, D.W. Facial nerve monitoring. In Salivary Gland Neoplasms; Karger Publishers: Basel, Switzerland, 2016; Volume 78, pp. 46–52. [Google Scholar]
- Mamelle, E.; Bernat, I.; Pichon, S.; Granger, B.; Sain-Oulhen, C.; Lamas, G.; Tankéré, F. Supramaximal stimulation during intraoperative facial nerve monitoring as a simple parameter to predict early functional outcome after parotidectomy. Acta Oto-Laryngol. 2013, 133, 779–784. [Google Scholar] [CrossRef]
- Behm, D.; Whittle, J.; Button, D.; Power, K. Intermuscle differences in activation. Muscle Nerve 2002, 25, 236–243. [Google Scholar] [CrossRef]
- Roberts, T.J.; Gabaldón, A.M. Interpreting muscle function from EMG: Lessons learned from direct measurements of muscle force. Integr. Comp. Biol. 2008, 48, 312–320. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.-Y.; Chang, C.-P.; Hung, C.-L.; Hung, C.-J.; Huang, S.-M. Traction Injury of Recurrent Laryngeal Nerve during Thyroidectomy. World J. Surg. 2020, 44, 402–407. [Google Scholar] [CrossRef]
- Wu, C.-W.; Dionigi, G.; Sun, H.; Liu, X.; Kim, H.Y.; Hsiao, P.-J.; Tsai, K.-B.; Chen, H.-C.; Chen, H.-Y.; Chang, P.-Y. Intraoperative neuromonitoring for the early detection and prevention of RLN traction injury in thyroid surgery: A porcine model. Surgery 2014, 155, 329–339. [Google Scholar] [CrossRef]
- Chiang, F.-Y.; Lu, I.-C.; Kuo, W.-R.; Lee, K.-W.; Chang, N.-C.; Wu, C.-W. The mechanism of recurrent laryngeal nerve injury during thyroid surgery—The application of intraoperative neuromonitoring. Surgery 2008, 143, 743–749. [Google Scholar] [CrossRef]
- Chiang, F.-Y.; Lee, K.-W.; Chen, H.-C.; Chen, H.-Y.; Lu, I.-C.; Kuo, W.-R.; Hsieh, M.-C.; Wu, C.-W. Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J. Surg. 2010, 34, 223–229. [Google Scholar] [CrossRef]
- Yuan, Q.; Wu, G.; Hou, J.; Liao, X.; Liao, Y.; Chiang, F.-Y. Correlation between electrophysiological changes and outcomes of vocal cord function in 1764 recurrent laryngeal nerves with visual integrity during thyroidectomy. Thyroid 2020, 30, 739–745. [Google Scholar] [CrossRef]
- Wu, C.-W.; Hao, M.; Tian, M.; Dionigi, G.; Tufano, R.P.; Kim, H.Y.; Jung, K.Y.; Liu, X.; Sun, H.; Lu, I.-C. Recurrent laryngeal nerve injury with incomplete loss of electromyography signal during monitored thyroidectomy—Evaluation and outcome. Langenbeck’s Arch. Surg. 2017, 402, 691–699. [Google Scholar] [CrossRef]
- House, W. Facial nerve grading system. Otolaryngol. Head Neck Surg. 1985, 93, 184–193. [Google Scholar] [CrossRef]
- Burres, S.; Fisch, U. The comparison of facial grading systems. Arch. Otolaryngol.—Head Neck Surg. 1986, 112, 755–758. [Google Scholar] [CrossRef]
- Murty, G.E.; Diver, J.P.; Kelly, P.J.; O’Donoghue, G.; Bradley, P.J. The Nottingham System: Objective assessment of facial nerve function in the clinic. Otolaryngol.—Head Neck Surg. 1994, 110, 156–161. [Google Scholar] [CrossRef]
- Croxson, G.; May, M.; Mester, S.J. Grading facial nerve function: House-Brackmann versus Burres-Fisch methods. Am. J. Otol. 1990, 11, 240–246. [Google Scholar]
- O’Reilly, B.F.; Soraghan, J.J.; McGrenary, S.; He, S. Objective method of assessing and presenting the House-Brackmann and regional grades of facial palsy by production of a facogram. Otol. Neurotol. 2010, 31, 486–491. [Google Scholar] [CrossRef]
- Stodulski, D.; Skorek, A.; Mikaszewski, B.; Wiśniewski, P.; Stankiewicz, C. Facial nerve grading after parotidectomy. Arch. Oto-Rhino-Laryngol. 2015, 272, 2445–2450. [Google Scholar] [CrossRef] [Green Version]
- Ross, B.G.; Fradet, G.; Nedzelski, J.M. Development of a sensitive clinical facial grading system. Otolaryngol.—Head Neck Surg. 1996, 114, 380–386. [Google Scholar] [CrossRef]
- Mencke, T.; Echternach, M.; Kleinschmidt, S.; Lux, P.; Barth, V.; Plinkert, P.K.; Fuchs-Buder, T. Laryngeal morbidity and quality of tracheal intubationa randomized controlled trial. J. Am. Soc. Anesthesiol. 2003, 98, 1049–1056. [Google Scholar] [CrossRef]
- Lu, I.-C.; Chang, P.-Y.; Su, M.-P.; Chen, P.-N.; Chen, H.-Y.; Chiang, F.-Y.; Wu, C.-W. The feasibility of sugammadex for general anesthesia and facial nerve monitoring in patients undergoing parotid surgery. Kaohsiung J. Med Sci. 2017, 33, 400–404. [Google Scholar] [CrossRef]
- Lu, I.-C.; Tsai, C.-J.; Wu, C.-W.; Cheng, K.-I.; Wang, F.-Y.; Tseng, K.-Y.; Chiang, F.-Y. A comparative study between 1 and 2 effective doses of rocuronium for intraoperative neuromonitoring during thyroid surgery. Surgery 2011, 149, 543–548. [Google Scholar] [CrossRef]



| Characteristics of Patients | 112 Patients (448 NBAR) |
|---|---|
| Pathologic reports | |
| Benign | 105 patients |
| Malignant | 7 patients |
| Sex | |
| Female | 51 patients |
| Male | 61 patients |
| Age (Mean ± SD) | 49.7 ± 13.9 years |
| Surgical extent | |
| Superficial parotidectomy | 89 patients |
| Superficial and deep parotidectomy | 23 patients |
| Transection facial nerve injury | 0 NBAR |
| Mean EMG amplitude (F2/F1 signals) | |
| Channel 1 | 983 ± 545/986 ± 592 µV |
| Channel 2 | 1289 ± 905/1264 ± 940 µV |
| Channel 3 | 1395 ± 961/1462 ± 922 µV |
| Channel 4 | 1542 ± 907/1680 ± 986 µV |
| Comparisons of F2 and F1 signal amplitudes | |
| Unchanged | 223 (50%) NBAR |
| Increased | 105 (23%) NBAR |
| Decreased | 120 (27%) NBAR |
| Abnormal regional facial function | |
| Unchanged/Increased signal amplitude | 0 of 328 (0.0%) NBAR |
| Decreased signal amplitude | |
| <50% signal amplitude decrease | 0 of 104 (0.0%) NBAR |
| >50% signal amplitude decrease | 13 of 16 (81.3%) NBAR |
| Procedures | Remarks |
|---|---|
| Grading facial function and photographing the four facial expressions before surgery | Evaluate dynamic movement of individual muscle groups over four separate facial regions by performing four rapid facial expressions |
| General anesthesia and facial nerve monitoring setup | Only a single dose (0.3 mg/kg) of rocuronium is administered during induction of general anesthesia. Four paired subdermal electrodes are inserted into four separate regions to monitor activity of facial muscles innervated by the temporal, zygomatic, buccal, and marginal mandibular branches of FN. |
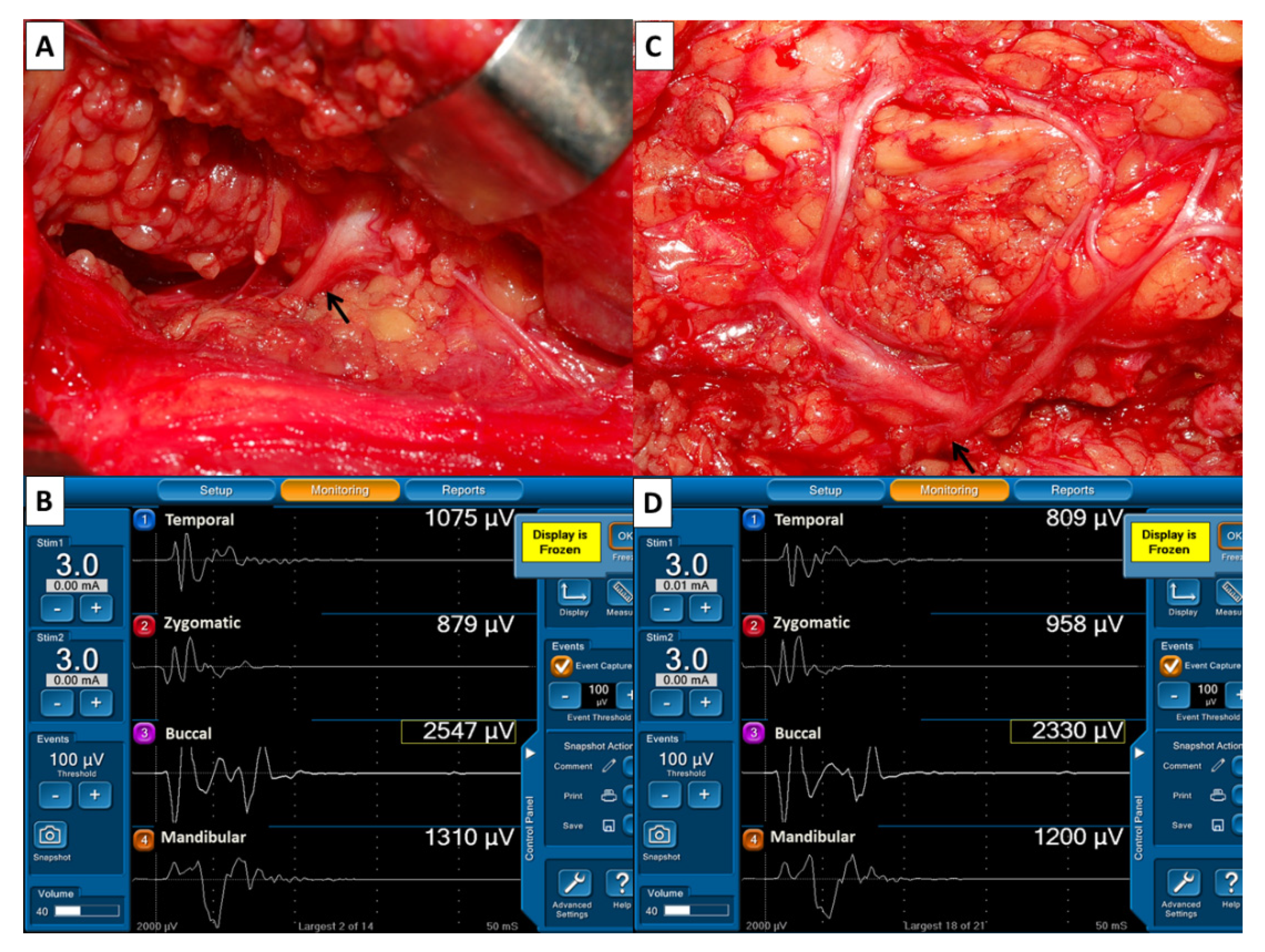
| Pre-dissection EMG (F1 signals) | FN trunk is stimulated with 3 mA when it is first identified |
| Post-dissection EMG (F2 signals) | After dissection of the FN branches, 3 mA is applied to FN trunk |
| Interpretation of EMG signals (F2/F1 ratio) | Unchanged amplitude- amplitude change within ±10% Increased amplitude- amplitude increase >10% Decreased amplitude- amplitude decrease >10% |
| Photographing the exposed FN branches | Confirmation of visual integrity of the FN |
| Grading facial function and photographing the four facial expressions after surgery | If asymmetric facial expression is detected, compare with preoperative recording |
| Degree | Description | Points |
|---|---|---|
| Normal function | A full symmetric dynamic movement of a facial region | 3 |
| Mild dysfunction | A slightly asymmetrical dynamic movement but symmetrical facial expression | 2 |
| Moderate dysfunction | An obvious asymmetrical dynamic movement and asymmetrical facial expression | 1 |
| Severe dysfunction | A complete lack of dynamic movement | 0 |
| Case Number | Age, Sex Side | Branches of Facial Nerve | Amplitude Decrease (%) | Grade of Facial Dysfunction | Pathologic Report |
|---|---|---|---|---|---|
| Case 1 | 74, M Left | Zygomatic | 85% | Normal | Warthin’s tumor |
| Case 2 | 42, F Left | Zygomatic Buccal | 75% 53% | Mild Mild | Pleomorphic adenoma |
| Case 3 | 58, M Right | Buccal | 66% | Mild | Pleomorphic adenoma |
| Case 4 | 47, M Right | Temporal | 53% | Normal | Pleomorphic adenoma |
| Case 5 | 47, F Left | Buccal, Mandibular | 75% 61% | Mild Moderate | Warthin’s tumor |
| Case 6 | 70, F Right | Mandibular | 69% | Mild | Lymphoepithelial cyst |
| Case 7 | 67, M Left | Mandibular | 68% | Moderate | Warthin’s tumor |
| Case 8 | 55, M Right | Zygomatic | 70% | Normal | Hemangioma |
| Case 9 | 39, F Right | Buccal Mandibular | 62% 73% | Mild Moderate | Myoepithelioma |
| Case 10 | 53, M Left | Mandibular | 63% | Mild | Warthin’s tumor |
| Case 11 | 38, F Right | Mandibular | 61% | Moderate | Oncocytoma |
| Case 12 | 48, M Left | Mandibular | 82% | Moderate | Salivary duct carcinoma |
| Case 13 | 54, M Right | Mandibular | 90% | Moderate | Warthin’s tumor |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiang, F.-Y.; Wang, C.-C.; Wu, C.-W.; Lu, I.-C.; Chang, P.-Y.; Lin, Y.-C.; Lien, C.-F.; Wang, C.-C.; Huang, T.-Y.; Hwang, T.-Z. Correlation between Electrophysiological Change and Facial Function in Parotid Surgery Patients. J. Clin. Med. 2021, 10, 5730. https://doi.org/10.3390/jcm10245730
Chiang F-Y, Wang C-C, Wu C-W, Lu I-C, Chang P-Y, Lin Y-C, Lien C-F, Wang C-C, Huang T-Y, Hwang T-Z. Correlation between Electrophysiological Change and Facial Function in Parotid Surgery Patients. Journal of Clinical Medicine. 2021; 10(24):5730. https://doi.org/10.3390/jcm10245730
Chicago/Turabian StyleChiang, Feng-Yu, Chih-Chun Wang, Che-Wei Wu, I-Cheng Lu, Pi-Ying Chang, Yi-Chu Lin, Ching-Feng Lien, Chien-Chung Wang, Tzu-Yen Huang, and Tzer-Zen Hwang. 2021. "Correlation between Electrophysiological Change and Facial Function in Parotid Surgery Patients" Journal of Clinical Medicine 10, no. 24: 5730. https://doi.org/10.3390/jcm10245730
APA StyleChiang, F.-Y., Wang, C.-C., Wu, C.-W., Lu, I.-C., Chang, P.-Y., Lin, Y.-C., Lien, C.-F., Wang, C.-C., Huang, T.-Y., & Hwang, T.-Z. (2021). Correlation between Electrophysiological Change and Facial Function in Parotid Surgery Patients. Journal of Clinical Medicine, 10(24), 5730. https://doi.org/10.3390/jcm10245730







