The Effect of Periprocedural Clinical Factors Related to the Course of STEMI in Men and Women Based on the National Registry of Invasive Cardiology Procedures (ORPKI) between 2014 and 2019
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient and Public Involvement
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- In the present study, procedure-related death occurred more frequently in women with STEMI than men with STEMI.
- Differences in perioperative mortality of women and men were found. The most important elements are smoking and psoriasis.
- Although there are gender differences in peri-procedural conduct in patients with STEMI, the treatment of women and men in the cath lab should be the same and in accordance with the procedures
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vaccarino, V.; Parsons, L.; Every, N.R.; Barron, H.V.; Krumholz, H.M. Sex-Based Differences in Early Mortality after Myocardial Infarction. N. Engl. J. Med. 1999, 341, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Vaccarino, V.; Parsons, L.; Peterson, E.D.; Rogers, W.J.; Kiefe, C.I.; Canto, J. Sex Differences in Mortality After Acute Myocardial Infarction: Changes from 1994 to 2006. Arch. Intern. Med. 2009, 169, 1767–1774. [Google Scholar] [CrossRef] [PubMed]
- Cenko, E.; van der Schaar, M.; Yoon, J.; Manfrini, O.; Vasiljevic, Z.; Vavlukis, M.; Kedev, S.; Miličić, D.; Badimon, L.; Bugiardini, R. Sex-Related Differences in Heart Failure After ST-Segment Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2019, 74, 2379–2389. [Google Scholar] [CrossRef]
- Cenko, E.; Yoon, J.; Kedev, S.; Stankovic, G.; Vasiljevic, Z.; Krljanac, G.; Kalpak, O.; Ricci, B.; Milicic, D.; Manfrini, O.; et al. Sex Differences in Outcomes After STEMI: I: Effect Modification by Treatment Strategy and Age. JAMA Intern. Med. 2018, 178, 632–639. [Google Scholar] [CrossRef]
- Hao, Y.; Liu, J.; Liu, J.; Yang, N.; Smith, S.C., Jr.; Huo, Y.; Fonarow, G.C.; Ge, J.; Taubert, K.A.; Morgan, L.; et al. Sex Differences in In-Hospital Management and Outcomes of Patients with Acute Coronary Syndrome. Circulationaha 2019, 139, 1776–1785. [Google Scholar] [CrossRef]
- Piackova, E.; Jäger, B.; Farhan, S.; Christ, G.; Schreiber, W.; Weidinger, F.; Stefenelli, T.; Delle-Karth, G.; Kaff, A.; Maurer, G.; et al. Gender differences in short- and long-term mortality in the Vienna STEMI registry. Int. J. Cardiol. 2017, 244, 303–308. [Google Scholar] [CrossRef]
- Ben-Yehuda, O.; Chen, S.; Redfors, B.; McAndrew, T.; Crowley, A.; Kosmidou, I.; Kandzari, D.E.; Puskas, J.D.; Morice, M.-C.; Taggart, D.P.; et al. Impact of large periprocedural myocardial infarction on mortality after percutaneous coronary intervention and coronary artery bypass grafting for left main disease: An analysis from the EXCEL trial. Eur. Heart J. 2019, 40, 1930–1941. [Google Scholar] [CrossRef] [PubMed]
- Dziewierz, A.; Brener, S.J.; Siudak, Z.; Plens, K.; Rakowski, T.; Zasada, W.; Tokarek, T.; Bartuś, K.; Dudek, D. Impact of On-Site Surgical Backup on Periprocedural Outcomes of Primary Percutaneous Interventions in Patients Presenting With ST-Segment Elevation Myocardial Infarction (From the ORPKI Polish National Registry). Am. J. Cardiol. 2018, 122, 929–935. [Google Scholar] [CrossRef]
- Bainbridge, D.; Martin, J.; Arango, M.; Cheng, D.; Evidence-Based Peri-operative Clinical Outcomes Research (EPiCOR) Group. Perioperative and anaesthetic-related mortality in developed and developing countries: A systematic review and meta-analysis. Lancet 2012, 380, 1075–1081. [Google Scholar] [CrossRef]
- Dudek, D.; Siudak, Z.; Grygier, M.; Araszkiewicz, A.; Dąbrowski, M.; Kusa, J.; Hawranek, M.; Huczek, Z.; Kralisz, P.; Roleder, T.; et al. Interventional cardiology in Poland in 2019. Summary report of the Association of Cardiovascular Interventions of the Polish Cardiac Society (AISN PTK) and Jagiellonian University Medical College. Adv. Interv. Cardiol. 2020, 16, 123–126. [Google Scholar] [CrossRef]
- Tavakol, M.; Ashraf, S.; Brener, S.J. Risks and Complications of Coronary Angiography: A Comprehensive Review. Glob. J. Health Sci. 2011, 4, 65–93. [Google Scholar] [CrossRef] [PubMed]
- Stehli, J.; Martin, C.; Brennan, A.; Dinh, D.T.; Lefkovits, J.; Zaman, S. Sex Differences Persist in Time to Presentation, Revascularization, and Mortality in Myocardial Infarction Treated with Percutaneous Coronary Intervention. J. Am. Heart Assoc. 2019, 8, e012161. [Google Scholar] [CrossRef] [PubMed]
- Lawesson, S.S.; Isaksson, R.-M.; Thylén, I.; Ericsson, M.; Ängerud, K.; Swahn, E.; SymTime Study Group. Gender differences in symptom presentation of ST-elevation myocardial infarction—An observational multicenter survey study. Int. J. Cardiol. 2018, 264, 7–11. [Google Scholar] [CrossRef]
- Shah, T.; Haimi, I.; Yang, Y.; Gaston, S.; Taoutel, R.; Mehta, S.; Lee, H.J.; Zambahari, R.; Baumbach, A.; Henry, T.D.; et al. Meta-Analysis of Gender Disparities in In-hospital Care and Outcomes in Patients with ST-Segment Elevation Myocardial Infarction. Am. J. Cardiol. 2021, 147, 23–32. [Google Scholar] [CrossRef]
- Eindhoven, D.C.; Hilt, A.D.; Zwaan, T.; Schalij, M.J.; Borleffs, C.J.W. Age and gender differences in medical adherence after myocardial infarction: Women do not receive optimal treatment—The Netherlands claims database. Eur. J. Prev. Cardiol. 2018, 25, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Januszek, R.; Siudak, Z.; Malinowski, K.P.; Wojdyła, R.; Mika, P.; Wańha, W.; Kameczura, T.; Surdacki, A.; Wojakowski, W.; Legutko, J.; et al. Aspiration Thrombectomy in Patients with Acute Myocardial Infarction—5-Year Analysis Based on a Large National Registry (ORPKI). J. Clin. Med. 2020, 9, 3610. [Google Scholar] [CrossRef] [PubMed]
- Tokarek, T.; Siudak, Z.; Dziewierz, A.; Rakowski, T.; Krycińska, R.; Siwiec, A.; Dudek, D. Clinical outcomes in nonagenarians undergoing a percutaneous coronary intervention: Data from the ORPKI Polish National Registry 2014–2016. Coron. Artery Dis. 2018, 29, 573–578. [Google Scholar] [CrossRef] [PubMed]
- MedCalc Statistical Software. Version 19.7. MedCalc Software. 2021. Available online: https://www.medcalc.org (accessed on 15 March 2021).
- Hannan, E.L.; Wu, Y.; Tamis-Holland, J.; Jacobs, A.K.; Berger, P.B.; Ling, F.S.K.; Walford, G.; Venditti, F.J.; King, S.B. Sex differences in the treatment and outcomes of patients hospitalized with ST-elevation myocardial infarction. Catheter. Cardiovasc. Interv. 2020, 95, 196–204. [Google Scholar] [CrossRef]
- Alabas, O.A.; Gale, C.P.; Hall, M.; Rutherford, M.J.; Szummer, K.; Lawesson, S.S.; Alfredsson, J.; Lindahl, B.; Jernberg, T. Sex Differences in Treatments, Relative Survival, and Excess Mortality Following Acute Myocardial Infarction: National Cohort Study Using the SWEDEHEART Registry. J. Am. Heart Assoc. 2017, 6, e007123. [Google Scholar] [CrossRef]
- Rodríguez-Padial, L.; Fernández-Pérez, C.; Bernal, J.L.; Anguita, M.; Sambola, A.; Fernández-Ortiz, A.; Elola, F.J. Differences in in-hospital mortality after STEMI versus NSTEMI by sex. Eleven-year trend in the Spanish National Health Service. Rev. Española Cardiol. 2020, 74, 510–517. [Google Scholar] [CrossRef]
- Heer, T.; Hochadel, M.; Schmidt, K.; Mehilli, J.; Zahn, R.; Kuck, K.; Hamm, C.; Böhm, M.; Ertl, G.; Hoffmeister, H.M.; et al. Sex Differences in Percutaneous Coronary Intervention—Insights from the Coronary Angiography and PCI Registry of the German Society of Cardiology. J. Am. Heart Assoc. 2017, 6, e004972. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.Y.; Liu, K.T.; Lu, H.T.; Ali, R.M.; Fong, A.Y.Y.; Ahmad, W.A.W. Sex and gender differences in presentation, treatment and outcomes in acute coronary syndrome, a 10 year study from a multi-ethnic Asian population: The Malaysian National Cardiovascular Disease Database—Acute Coronary Syndrome (NCVD-ACS) registry. PLoS ONE 2021, 16, e0246474. [Google Scholar] [CrossRef] [PubMed]
- Mallidi, J.; Lata, K. Role of Gender in Dual Antiplatelet Therapy After Acute Coronary Syndrome. Curr. Atheroscler. Rep. 2019, 21, 34. [Google Scholar] [CrossRef] [PubMed]
- Patti, G.; De Caterina, R.; Abbate, R.; Andreotti, F.; Biasucci, L.M.; Calabrò, P.; Cioni, G.; Davì, G.; Di Sciascio, G.; Golia, E.; et al. Platelet function and long-term antiplatelet therapy in women: Is there a gender-specificity? A ‘state-of-the-art’ paper. Eur. Heart J. 2014, 35, 2213–2223. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Lange, S.A.; Wittlinger, T.; Lehnert, G.; Rigopoulos, A.G.; Noutsias, M. In-hospital mortality after acute STEMI in patients undergoing primary PCI. Herz 2017, 43, 741–745. [Google Scholar] [CrossRef] [PubMed]
- Sliman, H.; Jaffe, R.; Rubinshtein, R.; Karkabi, B.; Zissman, K.; Flugelman, M.Y.; Zafrir, B. Clinical features and outcomes of revascularization in very old patients with left main coronary artery disease. Coron. Artery Dis. 2019, 30, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Fordyce, C.B.; Al-Khalidi, H.R.; Jollis, J.G.; Roettig, M.L.; Gu, J.; Bagai, A.; Berger, P.B.; Corbett, C.C.; Dauerman, H.L.; Fox, K.; et al. Association of Rapid Care Process Implementation on Reperfusion Times Across Multiple ST-Segment–Elevation Myocardial Infarction Networks. Circ. Cardiovasc. Interv. 2017, 10, e004061. [Google Scholar] [CrossRef]
- Nallamothu, B.K.; Normand, S.-L.T.; Wang, Y.; Hofer, T.P.; Brush, E., Jr.; Messenger, J.C.; Bradley, E.H.; Rumsfeld, J.S.; Krumholz, H.M. Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: A retrospective study. Lancet 2015, 385, 1114–1122. [Google Scholar] [CrossRef]
- Squire, B.T.; Tamayo-Sarver, J.H.; Rashi, P.; Koenig, W.; Niemann, J.T. Effect of Prehospital Cardiac Catheterization Lab Activation on Door-to-Balloon Time, Mortality, and False-Positive Activation. Prehospital Emerg. Care 2013, 18, 1–8. [Google Scholar] [CrossRef]
- Mehta, S.R.; Wood, D.A.; Cairns, J.A. Complete Revascularization with Multivessel PCI for Myocardial Infarction. N. Engl. J. Med. 2020, 382, 1568–1572. [Google Scholar] [CrossRef]
- Collet, J.-P.; Kerneis, M.; Lattuca, B.; Yan, Y.; Cayla, G.; Silvain, J.; Lapostolle, F.; Ecollan, P.; Diallo, A.; Vicaut, E.; et al. Impact of age on the effect of pre-hospital P2Y12 receptor inhibition in primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: The ATLANTIC-Elderly analysis. EuroIntervention 2018, 14, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-W.; Yoon, C.-H.; Kang, S.-H.; Choi, D.-J.; Kim, H.-S.; Cho, M.C.; Kim, Y.J.; Chae, S.C.; Yoon, J.H.; Gwon, H.-C.; et al. Early- and late-term clinical outcome and their predictors in patients with ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction. Int. J. Cardiol. 2013, 169, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Rakowski, T.; Siudak, Z.; Dziewierz, A.; Plens, K.; Kleczyński, P.; Dudek, D. Contemporary use of P2Y12 inhibitors in patients with ST-segment elevation myocardial infarction referred to primary percutaneous coronary interventions in Poland: Data from ORPKI national registry. J. Thromb. Thrombolysis 2017, 45, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Redfors, B.; Furer, A.; Selker, H.P.; Thiele, H.; Patel, M.R.; Chen, S.; Udelson, J.E.; Ohman, E.M.; Eitel, I.; Granger, C.B.; et al. Effect of Smoking on Outcomes of Primary PCI in Patients With STEMI. J. Am. Coll. Cardiol. 2020, 75, 1743–1754. [Google Scholar] [CrossRef]
- Gennaro, G.; Brener, S.J.; Redfors, B.; Kirtane, A.J.; Généreux, P.; Maehara, A.; Neunteufl, T.; Metzger, D.C.; Mehran, R.; Gibson, C.M.; et al. Effect of Smoking on Infarct Size and Major Adverse Cardiac Events in Patients with Large Anterior ST-Elevation Myocardial Infarction (from the INFUSE-AMI Trial). Am. J. Cardiol. 2016, 118, 1097–1104. [Google Scholar] [CrossRef] [PubMed]
- Michas, G.; Karvelas, G.; Trikas, A. Cardiovascular disease in Greece; the latest evidence on risk factors. Hell. J. Cardiol. 2019, 60, 271–275. [Google Scholar] [CrossRef]
- Gurbel, P.A.; Bliden, K.P.; Logan, D.K.; Kereiakes, D.J.; Lasseter, K.C.; White, A.; Angiolillo, D.J.; Nolin, T.D.; Maa, J.-F.; Bailey, W.L.; et al. The Influence of Smoking Status on the Pharmacokinetics and Pharmacodynamics of Clopidogrel and Prasugrel. J. Am. Coll. Cardiol. 2013, 62, 505–512. [Google Scholar] [CrossRef]
- Katayama, T.; Iwasaki, Y.; Sakoda, N.; Yoshioka, M. The Etiology of ‘Smoker’s Paradox’ in Acute Myocardial Infarction with Special Emphasis on the Association with Inflammation. Int. Heart J. 2008, 49, 13–24. [Google Scholar] [CrossRef][Green Version]
- Crimi, G.; Somaschini, A.; Cattaneo, M.; Angiolillo, D.J.; Piscione, F.; Palmerini, T.; De Servi, S. Cigarette smoking reduces platelet reactivity independently of clopidogrel treatment in patients with non-ST elevation acute coronary syndromes. Platelets 2017, 29, 309–311. [Google Scholar] [CrossRef]
- De Luca, G.; Parodi, G.; Sciagrà, R.; Bellandi, B.; Comito, V.; Vergara, R.; Migliorini, A.; Valenti, R.; Antoniucci, D. Smoking and infarct size among STEMI patients undergoing primary angioplasty. Atherosclerosis 2014, 233, 145–148. [Google Scholar] [CrossRef]
- Ferreiro, J.L.; Bhatt, D.L.; Ueno, M.; Bauer, D.; Angiolillo, D.J. Impact of Smoking on Long-Term Outcomes in Patients With Atherosclerotic Vascular Disease Treated With Aspirin or Clopidogrel: Insights from the CAPRIE trial (Clopidogrel Versus Aspirin in Patients at Risk of Ischemic Events. J. Am. Coll. Cardiol. 2014, 63, 769–777. [Google Scholar] [CrossRef]
- Lundergan, C.F.; Reiner, J.S.; McCarthy, W.F.; Coyne, K.S.; Califf, R.M.; Ross, A.M. Clinical predictors of early infarct-related artery patency following thrombolytic therapy: Importance of body weight, smoking history, infarct-related artery and choice of thrombolytic regimen: The GUSTO-I experience. Global Utilization of Streptokinase and t-PA for Oc-cluded Coronary Arteries. J. Am. Coll. Cardiol. 1998, 32, 641–647. [Google Scholar] [CrossRef]
- Zahger, D.; Cercek, B.; Cannon, C.P.; Jordan, M.; Davis, V.; Braunwald, E.; Shah, P.K. How do smokers differ from nonsmokers in their response to thrombolysis? (The TIMI-4 trial). Am. J. Cardiol. 1995, 75, 232–236. [Google Scholar] [CrossRef]
- Calvo, E.; Teruel, L.; Rosenfeld, L.; Guerrero, C.; Romero, M.; Romaguera, R.; Izquierdo, S.; Asensio, S.; Andreu-Periz, L.; Gómez-Hospital, J.A.; et al. Frailty in elderly patients undergoing primary percutaneous coronary intervention. Eur. J. Cardiovasc. Nurs. 2019, 18, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Goodman, S.G.; Yan, A.T.; Alexander, K.P.; Wong, C.L.; Cheema, A.N.; Udell, J.A.; Kaul, P.; D’Souza, M.; Hyun, K.; et al. Frailty and Outcomes After Myocardial Infarction: Insights from the CONCORDANCE Registry. J. Am. Heart Assoc. 2018, 7, e009859. [Google Scholar] [CrossRef] [PubMed]
- Yoshioka, N.; Takagi, K.; Morita, Y.; Yoshida, R.; Nagai, H.; Kanzaki, Y.; Furui, K.; Yamauchi, R.; Komeyama, S.; Sugiyama, H.; et al. Impact of the clinical frailty scale on mid-term mortality in patients with ST-elevated myocardial infarction. IJC Heart Vasc. 2019, 22, 192–198. [Google Scholar] [CrossRef]
- Siudak, Z.; Wysocka-Dubielecka, K.; Malinowski, K.; Dziewierz, A.; Tokarek, T.; Plens, K.; Dudek, D. Psoriasis is an independent predictor of increased risk of allergic reaction during percutaneous coronary interventions. Big data analysis from the Polish National PCI Registry (ORPKI). Cardiol. J. 2020, 27, 278–284. [Google Scholar] [CrossRef]


| Variable | Total n = 118,601 | Women n = 38,135 (32.2%) | Men n = 80,466 (67.8%) | p Value |
|---|---|---|---|---|
| Clinical factors | ||||
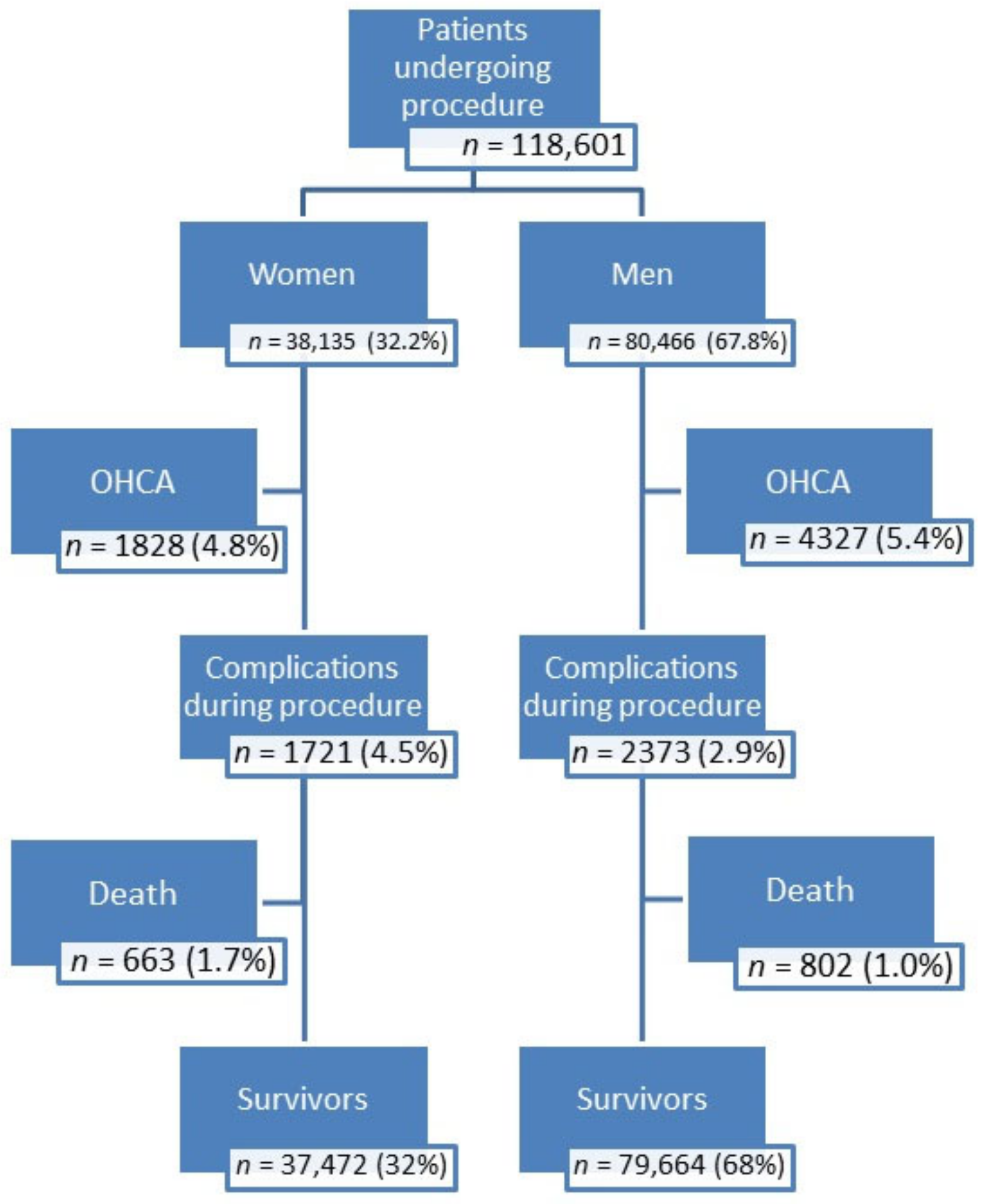
| Sex | 118,601 | 38,135 (32.2) | 80,466 (67.8) | <0.001 |
| Age, median (Q1–Q3) | 65 (57–74) | 70 (62–80) | 63 (56–70) | <0.001 |
| Age (>65 years) | 55,477 (46.8) | 24,141 (63.3) | 31,336 (38.9) | <0.001 |
| Diabetes (n, %) | 21,183 (17.9) | 8956 (23.5) | 12,227 (15.2) | <0.001 |
| Previous stroke (n, %) | 3907 (3.3) | 1550 (4.1) | 2357 (2.9) | <0.001 |
| Previous MI (n, %) | 14,813 (12.5) | 4021 (10.5) | 10,792 (13.4) | <0.001 |
| Previous PCI (n, %) | 13,763 (11.6) | 3593 (9.4) | 10,170 (12.6) | <0.001 |
| Previous CABG (n, %) | 2103 (1.8) | 469 (1.2) | 1634 (2.0) | <0.001 |
| Smoking (n, %) | 35,774 (30.2) | 8240 (21.6) | 27,534 (34.2) | <0.001 |
| Psoriasis (n, %) | 554 (0.5) | 145 (0.4) | 409 (0.5) | 0.003 |
| Hypertension (n, %) | 70,855 (59.7) | 24,688 (64.7) | 46,167 (57.4) | <0.001 |
| Kidney disease (n, %) | 4050 (3.4) | 1809 (4.7) | 2241 (2.8) | <0.001 |
| COPD (n, %) | 1981 (1.7) | 668 (1.8) | 1313 (1.6) | 0.13 |
| Prehospital management | ||||
| Time from pain to first contact (n, %) | <0.001 | |||
| <12 h | 98,711 (83.2) | 31,026 (81.4) | 67,685 (84.1) | |
| 12–48 h | 14,905 (12.6) | 5378 (14.1) | 9527 (11.8) | |
| ≥48 h | 4985 (4.2) | 1731 (4.5) | 3254 (4.0) | |
| Time from pain to inflation or angiogram (n, %) | <0.001 | |||
| <12 h | 114,363 (96.4) | 36,648 (96.1) | 77,715 (96.6) | |
| 12–48 h | 2963 (2.5) | 1045 (2.7) | 1918 (2.4) | |
| ≥48 h | 1275 (1.1) | 442 (1.2) | 833 (1.0) | |
| Time from first contact to inflation or angiogram (n, %) | <0.001 | |||
| <12 h | 105,164 (88.7) | 33,367 (87.5) | 71,797 (89.2) | |
| 12–48 h | 10,032 (8.5) | 3597 (9.4) | 6435 (8.0) | |
| ≥48 h | 3405 (2.9) | 1171 (3.1) | 2234 (2.8) | |
| Direct transfer to cath lab (n, %) | 29,216 (24.6) | 9026 (23.7) | 20,190 (25.1) | <0.001 |
| OHCA (n, %) | 6155 (5.2) | 1828 (4.8) | 4327 (5.4) | <0.001 |
| Variable | Total n = 118,601 | Women n = 38,135 (32.2%) | Men n = 80,466 (67.8%) | p Value |
|---|---|---|---|---|
| Pharmacological factors | ||||
| ASA (n, %) | 95,312 (80.4) | 30,497 (80.0) | 64,815 (80.5) | 0.019 |
| UFH (n, %) | 105,172 (88.7) | 33,778 (88.6) | 71,394 (88.7) | 0.44 |
| LMWH (n, %) | 4374 (3.7) | 1361 (3.6) | 3013 (3.7) | 0.13 |
| P2Y12 (n, %) | 99,447 (83.9) | 31,790 (83.4) | 67,657 (84.1) | 0.002 |
| Thrombolysis (n, %) | 112 (0.09) | 42 (0.1) | 70 (0.09) | 0.23 |
| GPI IIb/IIIa during angiogram (n, %) | 29,737 (25.1) | 8317 (21.8) | 21,420 (26.6) | <0.001 |
| Bivalirudin (n, %) | 60 (0.05) | 23 (0.06) | 37 (0.05) | 0.31 |
| Periprocedural factors | ||||
| IVUS (n, %) | 249 (0.2) | 63 (0.2) | 186 (0.2) | 0.021 |
| OCT (n, %) | 56 (0.05) | 13 (0.03) | 43 (0.05) | 0.15 |
| Vascular access (n, %) | <0.001 | |||
| radial | 86,393 (72.8) | 25,765 (67.6) | 60,628 (75.3) | |
| femoral | 32,208 (27.2) | 12,370 (32.4) | 19,838 (24.7) | |
| FFR (n, %) | 68 (0.06) | 17 (0.04) | 51 (0.06) | 0.21 |
| Aspiration thrombectomy (n, %) | 15,744 (13.3) | 4618 (12.1) | 11,126 (18.8) | <0.001 |
| Rotablation (n, %) | 75 (0.06) | 24 (0.06) | 51 (0.06) | 0.98 |
| GPI IIb/IIIa during PCI (n, %) | 7297 (6.2) | 2090 (5.5) | 5207 (6.5) | <0.001 |
| TIMI before PCI (n, %) | 0.003 | |||
| 0 | 69,383 (58.5) | 22,052 (57.8) | 47,331 (58.8) | |
| 1 | 17,550 (14.8) | 5814 (15.2) | 11,736 (14.6) | |
| 2 | 17,131 (14.4) | 5512 (14.5) | 11,619 (14.4) | |
| 3 | 14,537 (12.3) | 4757 (12.5) | 9780 (12.2) | |
| TIMI after PCI (n, %) | <0.001 | |||
| 0 | 2796 (2.4) | 1119 (2.9) | 1677 (2.1) | |
| 1 | 1810 (1.5) | 728 (1.9) | 1082 (1.3) | |
| 2 | 5708 (4.8) | 2040 (5.4) | 3668 (4.6) | |
| 3 | 107,968 (91.3) | 34,135 (89.9) | 73,833 (92.0) | |
| Total amount of contrast, mL, median (Q1–Q3) | 150 (120–200) | 150 (120–200) | 160 (130–200) | <0.001 |
| Total radiation dose, mGy, median (Q1–Q3) | 766 (437–1300) | 643 (359–1108) | 831 (482–1392) | <0.001 |
| Variable | Total n = 118,601 | Women n = 38,135 (32.2%) | Men n = 80,466 (67.8%) | p Value |
|---|---|---|---|---|
| Coronary anatomy and implanted stents | ||||
| RCA (n, %) | 47,444 (40.0) | 15,740 (41.3) | 31,704 (39.4) | <0.001 |
| LMCA (n, %) | 2638 (2.2) | 797 (2.1) | 1841 (2.3) | 0.031 |
| LAD (n, %) | 48,589 (41.0) | 15,683 (41.3) | 32,906 (40.9) | 0.45 |
| SvG (n, %) | 668 (0.6) | 125 (0.3) | 543 (0.7) | <0.001 |
| LIMA/RIMA (n, %) | 93 (0.08) | 27 (0.07) | 66 (0.08) | 0.52 |
| Bifurcation (n, %) | 8299 (7.0) | 2461 (6.50 | 5838 (7.3) | <0.001 |
| DES (n, %) | 102,460 (86.4) | 32,299 (84.7) | 70,161 (87.2) | <0.001 |
| BVS (n, %) | 587 (0.5) | 137 (0.4) | 450 (0.6) | <0.001 |
| BMS (n, %) | 7098 (6.0) | 2517 (6.6) | 4581 (5.7) | <0.001 |
| Number of implanted stents (n, %) | <0.001 | |||
| 0 | 9054 (7.6) | 3385 (8.9) | 5669 (7.0) | |
| 1 | 90,135 (76.0) | 28,455 (74.6) | 61,680 (76.7) | |
| 2 | 16,434 (13.9) | 5311 (13.9) | 11,123 (13.8) | |
| 3 | 2978 (2.5) | 984 (2.6) | 1994 (2.5) | |
| DEB (n, %) | 706 (0.6) | 234 (0.6) | 472 (0.6) | 0.57 |
| Complications during the procedure | ||||
| Total (n, %) | 4094 (3.5) | 1721 (4.5) | 2373 (2.9) | <0.001 |
| Death (n, %) | 1465 (1.2) | 663 (1.7) | 802 (1.0) | <0.001 |
| Cardiac arrest (n, %) | 927 (0.8) | 366 (1.0) | 561 (0.7) | <0.001 |
| Stroke (n, %) | 18 (0.02) | 11 (0.03) | 7 (0.009) | 0.009 |
| Dissection (n, %) | 146 (0.1) | 73 (0.2) | 73 (0.09) | <0.001 |
| Bleeding at the puncture site (n, %) | 52 (0.04) | 26 (0.07) | 26 (0.03) | 0.006 |
| Allergic reaction (n, %) | 12 (0.01) | 8 (0.02) | 4 (0.005) | 0.01 |
| No reflow (n, %) | 1756 (1.5) | 692 (1.8) | 1064 (1.3) | <0.001 |
| Coronary artery perforation (n, %) | 233 (0.2) | 117 (0.3) | 116 (0.1) | <0.001 |
| Variable | Women | Men | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Age (>65 years) | 1.99 | 1.60–2.47 | <0.001 | 1.95 | 1.66–2.28 | <0.001 |
| Diabetes | 1.52 | 1.26–1.83 | <0.001 | 1.66 | 1.38–1.99 | <0.001 |
| Previous stroke | 1.29 | 0.93–1.80 | 0.13 | 1.68 | 1.25–2.28 | <0.001 |
| Previous MI | 2.02 | 1.53–2.67 | <0.001 | 1.68 | 1.31–2.16 | <0.001 |
| Previous PCI | 0.73 | 0.53–1.01 | 0.06 | 0.85 | 0.65–1.12 | 0.24 |
| Previous CABG | 0.95 | 0.48–1.88 | 0.88 | 0.82 | 0.51–1.33 | 0.43 |
| Smoking | 0.55 | 0.41–0.73 | <0.001 | 0.77 | 0.64–0.92 | 0.003 |
| Psoriasis | 2.01 | 0.73–5.54 | 0.18 | 2.36 | 1.14–4.89 | 0.02 |
| Hypertension | 0.60 | 0.51–0.72 | <0.001 | 0.65 | 0.56–0.76 | <0.001 |
| Kidney disease | 1.58 | 1.20–2.10 | 0.001 | 1.61 | 1.20–2.18 | 0.002 |
| COPD | 1.08 | 0.61–1.90 | 0.8 | 1.51 | 0.98–2.31 | 0.06 |
| Time from pain to first contact | 1.56 | 1.35–1.81 | <0.001 | 1.62 | 1.41–1.86 | <0.001 |
| Time from pain to inflation or angiogram | 0.87 | 0.66–1.16 | 0.34 | 0.89 | 0.64–1.25 | 0.52 |
| Time from first contact to inflation or angiogram | 1.0002 | 0.99–1.0006 | 0.22 | 0.99 | 0.99–1.002 | 0.35 |
| Direct transfer to cath lab | 1.37 | 1.14–1.64 | <0.001 | 1.16 | 0.98–1.36 | 0.09 |
| OHCA | 6.6 | 5.47–8.15 | <0.001 | 9.08 | 7.71–10.69 | <0.001 |
| Variable | Women | Men | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| ASA | 0.96 | 0.75–1.22 | 0.74 | 1.06 | 0.86–1.32 | 0.58 |
| UFH | 1.24 | 0.95–1.63 | 0.11 | 1.09 | 0.87–1.39 | 0.43 |
| LMWH | * | * | ||||
| P2Y12 | 0.47 | 0.38–0.59 | <0.001 | 0.44 | 0.36–0.54 | <0.001 |
| Thrombolysis | 4.09 | 0.92–18.14 | 0.06 | 3.04 | 0.71–13.07 | 0.14 |
| GPI IIb/IIIa during angiogram | 1.14 | 0.92–1.41 | 0.22 | 1.36 | 1.13–1.63 | <0.001 |
| Bivalirudin | * | 3.33 | 0.37–30.33 | 0.29 | ||
| IVUS | * | 0.62 | 0.08–4.71 | 0.64 | ||
| OCT | * | 3.43 | 0.43–27.59 | 0.25 | ||
| Femoral access | 4.06 | 3.38–4.87 | <0.001 | 4.80 | 4.09–5.63 | <0.001 |
| FFR | * | 4.43 | 0.59–33.09 | 0.15 | ||
| Aspiration thrombectomy | 1.08 | 0.83–1.41 | 0.57 | 1.17 | 0.93–1.47 | 0.18 |
| Rotablation | 3.96 | 0.48–32.854 | 0.20 | 2.36 | 0.30–18.49 | 0.41 |
| GPI IIb/IIIa during PCI | 1.28 | 0.89–1.83 | 0.18 | 1.56 | 1.18–2.06 | 0.002 |
| TIMI before PCI | 0.97 | 0.88–1.08 | 0.60 | 1.05 | 0.96–1.15 | 0.29 |
| TIMI after PCI | 0.29 | 0.28–0.32 | <0.001 | 0.27 | 0.26–0.29 | <0.001 |
| Total amount of contrast, ml | 0.999 | 0.998–1.0009 | 0.66 | 0.998 | 0.997–0.999 | 0.002 |
| Total radiation dose, mGy. | 1.0001 | 1.0000–1.0002 | 0.06 | 1.0001 | 1.0001–1.0002 | <0.001 |
| Variable | Women | Men | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| RCA | 1.06 | 0.83–1.35 | 0.66 | 0.83 | 0.66–1.05 | 0.12 |
| LMCA | 7.81 | 5.79–10.54 | <0.001 | 11.99 | 9.56–15.02 | <0.001 |
| LAD | 2.29 | 1.84–2.85 | <0.001 | 1.93 | 1.59–2.34 | <0.001 |
| SvG | 1.42 | 0.29–6.72 | 0.66 | 2.17 | 0.96–4.91 | 0.06 |
| LIMA/RIMA | * | 5.89 | 1.34–25.88 | 0.02 | ||
| Bifurcation | 0.57 | 0.39–0.83 | 0.004 | 0.58 | 0.42–0.80 | 0.001 |
| DES | 0.11 | 0.08–0.14 | <0.001 | 0.09 | 0.08–0.13 | <0.001 |
| BVS | 0.09 | 0.01–0.64 | 0.016 | 0.11 | 0.03–0.43 | 0.003 |
| BMS | 0.49 | 0.35–0.69 | <0.001 | 0.40 | 0.29–0.56 | <0.001 |
| Number of implanted stents | 1.23 | 1.02–1.48 | 0.03 | 1.15 | 0.97–1.36 | 0.11 |
| DEB | 1.03 | 0.50–2.11 | 0.94 | 0.32 | 0.12–0.88 | 0.03 |
| Cardiac arrest during angiogram | 24.55 | 18.74–32.16 | <0.001 | 33.3 | 26.36–42.24 | <0.001 |
| Stroke | 2.02 | 0.15–27.07 | 0.6 | |||
| Dissection | 0.89 | 0.29–2.66 | 0.83 | 0.44 | 0.05–3.76 | 0.45 |
| Bleeding at the puncture site | * | * | ||||
| Allergic reaction | * | * | ||||
| No reflow | 3.37 | 2.43–4.67 | <0.001 | 5.04 | 3.78–6.71 | <0.001 |
| Coronary artery perforation | 3.09 | 1.44–6.65 | 0.004 | 2.02 | 0.69–5.88 | 0.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sielski, J.; Kaziród-Wolski, K.; Jurys, K.; Wałek, P.; Siudak, Z. The Effect of Periprocedural Clinical Factors Related to the Course of STEMI in Men and Women Based on the National Registry of Invasive Cardiology Procedures (ORPKI) between 2014 and 2019. J. Clin. Med. 2021, 10, 5716. https://doi.org/10.3390/jcm10235716
Sielski J, Kaziród-Wolski K, Jurys K, Wałek P, Siudak Z. The Effect of Periprocedural Clinical Factors Related to the Course of STEMI in Men and Women Based on the National Registry of Invasive Cardiology Procedures (ORPKI) between 2014 and 2019. Journal of Clinical Medicine. 2021; 10(23):5716. https://doi.org/10.3390/jcm10235716
Chicago/Turabian StyleSielski, Janusz, Karol Kaziród-Wolski, Karolina Jurys, Paweł Wałek, and Zbigniew Siudak. 2021. "The Effect of Periprocedural Clinical Factors Related to the Course of STEMI in Men and Women Based on the National Registry of Invasive Cardiology Procedures (ORPKI) between 2014 and 2019" Journal of Clinical Medicine 10, no. 23: 5716. https://doi.org/10.3390/jcm10235716
APA StyleSielski, J., Kaziród-Wolski, K., Jurys, K., Wałek, P., & Siudak, Z. (2021). The Effect of Periprocedural Clinical Factors Related to the Course of STEMI in Men and Women Based on the National Registry of Invasive Cardiology Procedures (ORPKI) between 2014 and 2019. Journal of Clinical Medicine, 10(23), 5716. https://doi.org/10.3390/jcm10235716







