The Assessment of Fear of COVID-19 among the Elderly Population: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
- is the standard normal variate (at 5% type 1 error p < 0.05), -1.96;
- p is the expected prevalence obtained from a pilot study, -0.4; and
- d is the absolute precision-0.043.
2.2. Explanatory Variables
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Fear of COVID-19 Infection
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johns Hopkins Coronavirus Resource Center. COVID-19 Map. Available online: https://coronavirus.jhu.edu/map.html (accessed on 20 October 2021).
- Berete, F.; Braekman, E.; Bruggeman, H.; Charafeddine, R.; Demarest, S.; Drieskens, S.; Gisle, L.; Hermans, L.; Leclercq, V.; Van der Heyden, J. Zesde COVID-19-Gezondheidsenquête Eerste Resultaten; Levenslang Gezond; Sciensano: Brussels, Belgium, 2021; pp. 1–71. [Google Scholar] [CrossRef]
- Quadros, S.; Garg, S.; Ranjan, R.; Vijayasarathi, G.; Mamun, M.A. Fear of COVID-19 Infection Across Different Cohorts: A Scoping Review. Front. Psychiatry 2021, 12, 1289. [Google Scholar] [CrossRef]
- Schimmenti, A.; Billieux, J.; Starcevic, V. The four horsemen of fear: An integrated model of understanding fear experiences during the COVID-19 pandemic. Clin. Neuropsychiatry 2020, 17, 41–45. [Google Scholar]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Fergus, T.A.; McKay, D.; Asmundson, G.J.G. COVID stress syndrome: Concept, structure, and correlates. Depress. Anxiety 2020, 37, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Mamun, M.A.; Sakib, N.; Gozal, D.; Bhuiyan, A.I.; Hossain, S.; Bodrud-Doza, M.; Al Mamun, F.; Hosen, I.; Safiq, M.B.; Abdullah, A.H.; et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: A population-based nationwide study. J. Affect. Disord. 2021, 279, 462–472. [Google Scholar] [CrossRef]
- Twenge, J.M.; Joiner, T.E. Mental distress among U.S. adults during the COVID-19 pandemic. J. Clin. Psychol. 2020, 76, 2170–2182. [Google Scholar] [CrossRef] [PubMed]
- Roy, D.; Tripathy, S.; Kar, S.K.; Sharma, N.; Verma, S.K.; Kaushal, V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatry 2020, 51, 102083. [Google Scholar] [CrossRef]
- Vahia, I.V.; Jeste, D.V.; Reynolds, C.F. Older Adults and the Mental Health Effects of COVID-19. JAMA 2020, 324, 2253–2254. [Google Scholar] [CrossRef] [PubMed]
- Van Bavel, J.J.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Su, Z.; McDonnell, D.; Wen, J.; Kozak, M.; Abbas, J.; Šegalo, S.; Li, X.; Ahmad, J.; Cheshmehzangi, A.; Cai, Y.; et al. Mental health consequences of COVID-19 media coverage: The need for effective crisis communication practices. Glob. Health 2021, 17, 4. [Google Scholar] [CrossRef]
- Agrawal, S.; Makuch, S.; Dróżdż, M.; Strzelec, B.; Sobieszczańska, M.; Mazur, G. The impact of the COVID-19 emergency on life activities and delivery of healthcare services in the elderly population. J. Clin. Med. 2021, 10, 4089. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 1–9, Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 20 October 2021).
- World Health Organization. COVID-19 Strategy Update. Available online: www.who.int/emergencies/en (accessed on 20 October 2021).
- Arora, A.; Jha, A.K.; Alat, P.; Das, S.S. Understanding coronaphobia. Asian J. Psychiatry 2020, 54, 102384. [Google Scholar] [CrossRef]
- Freckelton, I. COVID-19: Fear, quackery, false representations and the law. Int. J. Law Psychiatry 2020, 72, 101611. [Google Scholar] [CrossRef]
- Mistry, S.K.; Ali, A.R.M.M.; Akther, F.; Yadav, U.N.; Harris, M.F. Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Glob. Health 2021, 17, 47. [Google Scholar] [CrossRef]
- Alsharawy, A.; Spoon, R.; Smith, A.; Ball, S. Gender Differences in Fear and Risk Perception During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 3104. [Google Scholar] [CrossRef]
- Rodríguez-Hidalgo, A.J.; Pantaleón, Y.; Dios, I.; Falla, D. Fear of COVID-19, Stress, and Anxiety in University Undergraduate Students: A Predictive Model for Depression. Front. Psychol. 2020, 11, 3041. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Hosen, I.; Pakpour, A.H.; Sakib, N.; Hussain, N.; Al Mamun, F.; Mamun, M.A. Knowledge and preventive behaviors regarding COVID-19 in Bangladesh: A nationwide distribution. PLoS ONE 2021, 16, e0251151. [Google Scholar] [CrossRef]
- Senst, L.; Baimoukhametova, D.; Sterley, T.-L.; Bains, J.S. Sexually dimorphic neuronal responses to social isolation. eLife 2016, 5, 5904. [Google Scholar] [CrossRef]
- Zhang, J.X.; Wang, Y.N.; Yang, X.D.; Chen, Z.Y.; Gao, W.B. The dynamic analysis of public mental health during SARS epidemic period. Int. J. Psychol. 2004, 39, 455. [Google Scholar]
- Levkovich, I.; Shinan-Altman, S. The impact of gender on emotional reactions, perceived susceptibility and perceived knowledge about COVID-19 among the Israeli public. Int. Health 2021, 1–7. [Google Scholar] [CrossRef]
- Bakioğlu, F.; Korkmaz, O.; Ercan, H. Fear of COVID-19 and Positivity: Mediating Role of Intolerance of Uncertainty, Depression, Anxiety, and Stress. Int. J. Ment. Health Addict. 2020, 1–14. [Google Scholar] [CrossRef]
- Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102076. [Google Scholar] [CrossRef]
- Al-Rahimi, J.S.; Nass, N.M.; Hassoubah, S.A.; Wazqar, D.Y.; Alamoudi, S.A. Levels and predictors of fear and health anxiety during the current outbreak of COVID-19 in immunocompromised and chronic disease patients in Saudi Arabia: A cross-sectional correlational study. PLoS ONE 2021, 16, e0250554. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Chow, N.; Fleming-Dutra, K.; Gierke, R.; Hall, A.; Hughes, M.; Pilishvili, T.; Ritchey, M.; Roguski, K.; Skoff, T.; Ussery, E. Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019—United States, 12 February–28 March 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 382–386. [Google Scholar] [CrossRef]
- Chandra, A.; Chakraborty, U.; Ghosh, S.; Dasgupta, S. Anticoagulation in COVID-19: Current concepts and controversies. Postgrad. Med. J. 2021, 12, 71. [Google Scholar] [CrossRef]
- Nazir, M.; Hussain, I.; Tian, J.; Akram, S.; Tshiaba, S.M.; Mushtaq, S.; Shad, M.A. A multidimensional model of public health approaches against COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3780. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Weaver, M.D.; Robbins, R.; Facer-Childs, E.R.; Barger, L.K.; et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, 24–30 June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1049–1057. [Google Scholar] [CrossRef]
- Garfin, D.R.; Silver, R.C.; Holman, E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychol. 2020, 39, 355–357. [Google Scholar] [CrossRef]
- Asmundson, G.J.G.; Taylor, S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020, 71, 102211. [Google Scholar] [CrossRef]
- Mertens, G.; Gerritsen, L.; Duijndam, S.; Salemink, E.; Engelhard, I.M. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J. Anxiety Disord. 2020, 74, 102258. [Google Scholar] [CrossRef]
- Rahman, M.A.; Islam, S.M.S.; Tungpunkom, P.; Sultana, F.; Alif, S.M.; Banik, B.; Salehin, M.; Joseph, B.; Lam, L.; Watts, M.C.; et al. COVID-19: Factors associated with psychological distress, fear, and coping strategies among community members across 17 countries. Glob. Health 2021, 17, 117. [Google Scholar] [CrossRef]
- Iftimie, S.; López-Azcona, A.F.; Vallverdú, I.; Hernández-Flix, S.; de Febrer, G.; Parra, S.; Hernández-Aguilera, A.; Riu, F.; Joven, J.; Andreychuk, N.; et al. First and second waves of coronavirus disease-19: A comparative study in hospitalized patients in Reus, Spain. PLoS ONE 2021, 16, e0248029. [Google Scholar] [CrossRef]
- Pedro, S.A.; Ndjomatchoua, F.T.; Jentsch, P.; Tchuenche, J.M.; Anand, M.; Bauch, C.T. Conditions for a Second Wave of COVID-19 Due to Interactions Between Disease Dynamics and Social Processes. Front. Phys. 2020, 8, 428. [Google Scholar] [CrossRef]
- Kunno, J.; Supawattanabodee, B.; Sumanasrethakul, C.; Wiriyasivaj, B.; Kuratong, S.; Kaewchandee, C. Comparison of Different Waves during the COVID-19 Pandemic: Retrospective Descriptive Study in Thailand. Adv. Prev. Med. 2021, 2021, 5807056. [Google Scholar] [CrossRef]
- Seong, H.; Hyun, H.J.; Yun, J.G.; Noh, J.Y.; Cheong, H.J.; Kim, W.J.; Song, J.Y. Comparison of the second and third waves of the COVID-19 pandemic in South Korea: Importance of early public health intervention. Int. J. Infect. Dis. 2021, 104, 742–745. [Google Scholar] [CrossRef]
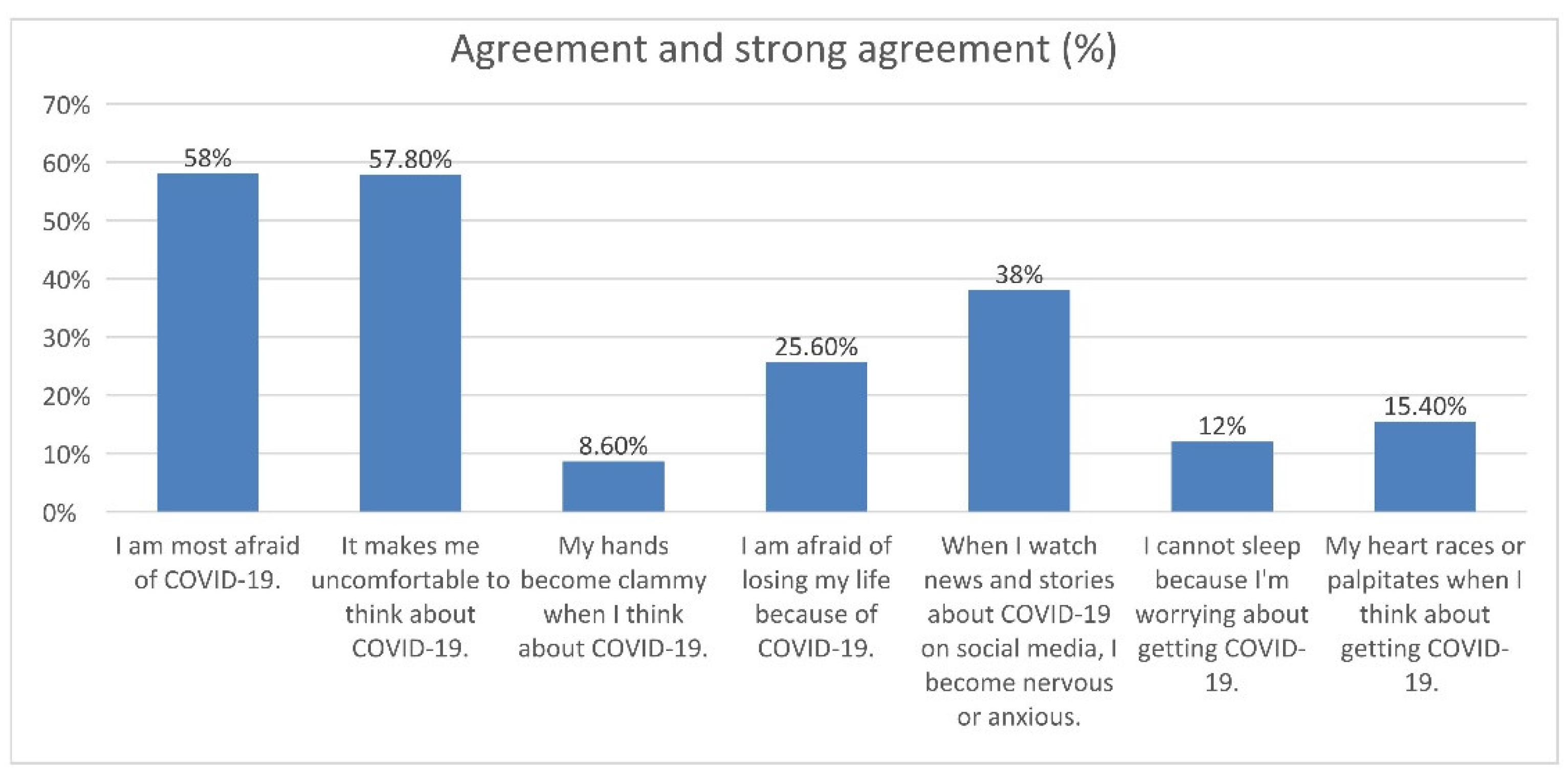
| Questionnaire Item, n (%) | Statistics |
|---|---|
| 1. I am most afraid of COVID-19, Me (IQR) | 4 (3–4) |
| Strongly disagree (1 point) | 18 (3.6%) |
| Disagree (2 points) | 55 (11.0%) |
| Neither agree nor disagree (3 points) | 137 (27.4%) |
| Agree (4 points) | 201 (40.2%) |
| Strongly agree (5 points) | 89 (17.8%) |
| 2. It makes me uncomfortable to think about COVID-19, Me (IQR) | 4 (3–4) |
| Strongly disagree (1 point) | 22 (4.4%) |
| Disagree (2 points) | 77 (15.4%) |
| Neither agree nor disagree (3 points) | 112 (22.4%) |
| Agree (4 points) | 220 (44.0%) |
| Strongly agree (5 points) | 69 (13.8%) |
| 3. My hands become clammy when I think about COVID-19, Me (IQR) | 2 (1–2) |
| Strongly disagree (1 point) | 192 (38.4%) |
| Disagree (2 points) | 193 (38.6%) |
| Neither agree nor disagree (3 points) | 72 (14.4%) |
| Agree (4 points) | 37 (7.4%) |
| Strongly agree (5 points) | 6 (1.2%) |
| 4. I am afraid of losing my life because of COVID-19, Me (IQR) | 3 (2–4) |
| Strongly disagree (1 point) | 73 (14.6%) |
| Disagree (2 points) | 120 (24.0%) |
| Neither agree nor disagree (3 points) | 179 (35.8%) |
| Agree (4 points) | 94 (18.8%) |
| Strongly agree (5 points) | 34 (6.8%) |
| 5. When I watch news and stories about COVID-19 on social media, I become nervous or anxious, Me (IQR) | 3 (2–4) |
| Strongly disagree (1 point) | 44 (8.8%) |
| Disagree (2 points) | 124 (24.8%) |
| Neither agree nor disagree (3 points) | 142 (28.4%) |
| Agree (4 points) | 155 (31.0%) |
| Strongly agree (5 points) | 35 (7.0%) |
| 6. I cannot sleep because I’m worrying about getting COVID-19, Me (IQR) | 2 (1–3) |
| Strongly disagree (1 point) | 135 (27.4%) |
| Disagree (2 points) | 199 (39.8%) |
| Neither agree nor disagree (3 points) | 101 (20.2%) |
| Agree (4 points) | 49 (9.8%) |
| Strongly agree (5 points) | 14 (2.8%) |
| 7. My heart races or palpitates when I think about getting COVID-19, Me (IQR) | 2 (1–3) |
| Strongly disagree (1 point) | 132 (26.4%) |
| Disagree (2 points) | 175 (35.0%) |
| Neither agree nor disagree (3 points) | 116 (23.2%) |
| Agree (4 points) | 63 (12.6%) |
| Strongly agree (5 points) | 14 (2.8%) |
| The total assessment of fear of COVID-19 infection (total points): | |
| M ± SD | 19.3 ± 5.6 |
| Me (IQR) | 19 (15–23) |
| Min–Max | 7–35 |
| Feature (Variable) | Statistics |
|---|---|
| Gender: | |
| Female (n = 290) | 20 (16–23) |
| Male (n = 210) | 19 (14–22) |
| U Mann–Whitney test: | p = 0.025 |
| Age | |
| 60–64 (n = 141) | 19 (15–23) |
| 65–69 (n = 128) | 20 (16–23) |
| 70 and more (n = 231) | 19 (15–23) |
| Kruskal–Wallis test: | p = 0.832 |
| Place of residence | p = 0.644 |
| Housing situation | p = 0.597 |
| Education | p = 0.397 |
| Household income per person per month | p = 0.982 |
| Feature (Variable) | Statistics |
|---|---|
| Coronary heart disease: | |
| Yes (n = 63) | 22 (18–26) |
| No (n = 437) | 19 (15–22) |
| U Mann–Whitney Test: | p < 0.001 |
| Diabetes Mellitus: | |
| Yes (n = 74) | 21 (16–25) |
| No (n = 426) | 19 (15–23) |
| U Mann–Whitney Test: | p = 0.068 |
| Asthma: | |
| Yes (n = 43) | 20 (16–26) |
| No (n = 457) | 19 (15–23) |
| U Mann–Whitney Test: | p = 0.245 |
| COPD: | |
| Yes (n = 33) | 22 (19–26) |
| No (n = 467) | 19 (15–23) |
| U Mann–Whitney Test: | p = 0.007 |
| Heart failure: | |
| Yes (n = 71) | 22 (18–26) |
| No (n = 429) | 19 (15–22) |
| U Mann–Whitney Test: | p < 0.001 |
| Kidney failure: | |
| Tak (n = 20) | 23 (18–27) |
| Nie (n = 480) | 19 (15–23) |
| U Mann–Whitney Test: | p = 0.077 |
| Feature (Variable) | Statistics |
|---|---|
| Number of drugs currently taken | |
| 1 to 3 (n = 301) | 19 (15–22) |
| 4 to 6 (n = 151) | 21 (16–25) |
| 7 to 10 (n = 40) | 20 (16–25) |
| More than 10 (n = 8) | 25 (20–28) |
| U Mann–Whitney Test: | p = 0.002 |
| Cardiac drugs | |
| Yes (n = 132) | 21 (17–25) |
| No (n = 368) | 19 (15–22) |
| U Mann–Whitney Test: | p < 0.001 |
| Antihypertensive drugs | |
| Yes (n = 255) | 20 (16–24) |
| No (n = 368) | 19 (14-22) |
| U Mann–Whitney Test: | p = 0.011 |
| Diuretics | |
| Yes (n = 78) | 20 (17–25) |
| No (n = 422) | 19 (15–23) |
| U Mann–Whitney Test: | p = 0.060 |
| Analgesics | |
| Yes (n = 230) | 20 (16-24) |
| No (n = 270) | 18 (15-22) |
| U Mann–Whitney Test: | p = 0.001 |
| For digestive ailments drugs | |
| Yes (n = 131) | 20 (17–24) |
| No (n = 369) | 19 (15–22) |
| U Mann–Whitney Test: | p = 0.005 |
| Anticoagulants | |
| Yes (n = 87) | 20 (17–25) |
| No (n = 413) | 19 (15–23) |
| U Mann–Whitney Test: | p = 0.004 |
| Antidepresants | |
| Yes (n = 78) | 20 (17–24) |
| No (n = 422) | 19 (15–23) |
| U Mann–Whitney Test: | p = 0.043 |
| To improve memory drugs: | |
| Yes (n = 54) | 19 (16–24) |
| No (n = 446) | 19 (15–23) |
| U Mann–Whitney Test: | p = 0.786 |
| All drugs are prescribed by the same doctor | |
| Yes (n = 352) | 19 (15–23) |
| No (n = 148) | 19 (15–23) |
| U Mann–Whitney Test: | p = 0.684 |
| How many different doctors have prescribed your medications? | |
| 2 (n = 82) | 19 (14–23) |
| 3 (n = 52) | 20 (15–23) |
| 4 and more (n = 14) | 21 (17–25) |
| Kruskal–Wallis Test: | p = 0.455 |
| Feature (Variable) | Statistics |
|---|---|
| Activities of Daily Living (ADL) | |
| Fit people (n = 493) | 19 (15–25) |
| Moderately disabled people (n = 6) | 23 (18–26) |
| Disabled people (n = 1) | 34 |
| Kruskal–Wallis Test: | p = 0.150 |
| The Lawton Instrumental Activities of Daily Living (IADL) | |
| Fit people, ≥24 pts. (n = 361) | 19 (15–22) |
| Less fit people, <24 pts. (n = 139) | 21 (16–24) |
| U Mann–Whitney Test: | p = 0.013 |
| Abbreviated Mental Test Score (AMTS) | |
| Normal condition, 7–10 pts., (n = 491) | 19 (15–23) |
| Moderate disorder, 4–6 pts., (n = 9) | 22 (18–23) |
| U Mann–Whitney Test: | p = 0.013 |
| Geriatric depression scale (GDS-15) | |
| Lack of depression, 0–5 pts., (n = 324) | 18 (15–22) |
| Depression, 6–15 pts., (n = 176) | 22 (17–25) |
| U Mann–Whitney Test: | p < 0.001 |
| Geriatric Anxiety Scale (GAS-10) | |
| Lower anxiety level, 0–5 pts., (n = 210) | 17 (14–21) |
| Higher anxiety level, 6–25 pts., (n = 290) | 21 (17–25) |
| U Mann–Whitney Test: | p < 0.001 |
| Lubben Social Network Scale (LSNS-6) | |
| Lower, 16–30 pts., (n = 209) | 19 (14–22) |
| Higher, 0–15 pts., (n = 291) | 20 (16–24) |
| U Mann–Whitney Test: | p = 0.006 |
| Social loneliness scale (Gierveld Scale) | |
| Lower, 14–18 pts., (n = 209) | 18 (14–22) |
| Higher, 6–13 pts., (n = 291) | 20 (16–23) |
| U Mann–Whitney Test: | p = 0.004 |
| Mini Nutritional Assessment (MNA) | |
| Proper nutritional status, 12–14 pts., (n = 418) | 19 (15–22) |
| The danger of malnutrition, 8–11 pts., (n = 78) | 21 (17–27) |
| Malnutrition, 0–7 pts., (n = 4) | 21 (16–24) |
| Kruskal–Wallis Test: | p = 0.017 |
| Predictors of Fear of COVID-19 Infection | b | p | Beta | p |
|---|---|---|---|---|
| Female gender | 1.24 | 0.015 | 0.124 | 0.007 |
| Coronary heart disease | 2.52 | 0.001 | - | >0.05 |
| COPD | 2.54 | 0.012 | - | >0.05 |
| Heart failure | 2.54 | <0.001 | - | >0.05 |
| The number of currently taken medicines | 1.27 | <0.001 | - | >0.05 |
| Cardiac drugs | 2.08 | <0.001 | - | >0.05 |
| Antihypertensive drugs | 1.33 | 0.008 | - | >0.05 |
| Analgesics | 1.66 | 0.001 | - | >0.05 |
| Digestive ailments’ drugs | 1.64 | 0.004 | - | >0.05 |
| Anticoagulants | 2.02 | 0.002 | 0.095 | 0.041 |
| Antidepressants | 1.23 | 0.078 | - | >0.05 |
| The Lawton Instrumental Activities of Daily Living (IADL) | −0.263 | 0.015 | - | >0.05 |
| Abbreviated Mental Test Score (AMTS) | −0.110 | 0.678 | - | >0.05 |
| Geriatric depression scale (GDS-15) | 0.444 | <0.001 | - | >0.05 |
| Geriatric Anxiety Scale (GAS-10) | 0.473 | <0.001 | 0.359 | <0.001 |
| Lubben Social Network Scale (LSNS-6) | −0.127 | 0.003 | - | >0.05 |
| Social loneliness scale (Gierveld Scale) | −0.481 | <0.001 | - | >0.05 |
| Mini Nutritional Assessment (MNA) | −0.680 | <0.001 | - | >0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agrawal, S.; Dróżdż, M.; Makuch, S.; Pietraszek, A.; Sobieszczańska, M.; Mazur, G. The Assessment of Fear of COVID-19 among the Elderly Population: A Cross-Sectional Study. J. Clin. Med. 2021, 10, 5537. https://doi.org/10.3390/jcm10235537
Agrawal S, Dróżdż M, Makuch S, Pietraszek A, Sobieszczańska M, Mazur G. The Assessment of Fear of COVID-19 among the Elderly Population: A Cross-Sectional Study. Journal of Clinical Medicine. 2021; 10(23):5537. https://doi.org/10.3390/jcm10235537
Chicago/Turabian StyleAgrawal, Siddarth, Mateusz Dróżdż, Sebastian Makuch, Alicja Pietraszek, Małgorzata Sobieszczańska, and Grzegorz Mazur. 2021. "The Assessment of Fear of COVID-19 among the Elderly Population: A Cross-Sectional Study" Journal of Clinical Medicine 10, no. 23: 5537. https://doi.org/10.3390/jcm10235537
APA StyleAgrawal, S., Dróżdż, M., Makuch, S., Pietraszek, A., Sobieszczańska, M., & Mazur, G. (2021). The Assessment of Fear of COVID-19 among the Elderly Population: A Cross-Sectional Study. Journal of Clinical Medicine, 10(23), 5537. https://doi.org/10.3390/jcm10235537






