Effectiveness of Global Postural Re-Education in Chronic Non-Specific Low Back Pain: Systematic Review and Meta-Analysis
Abstract
1. Introduction
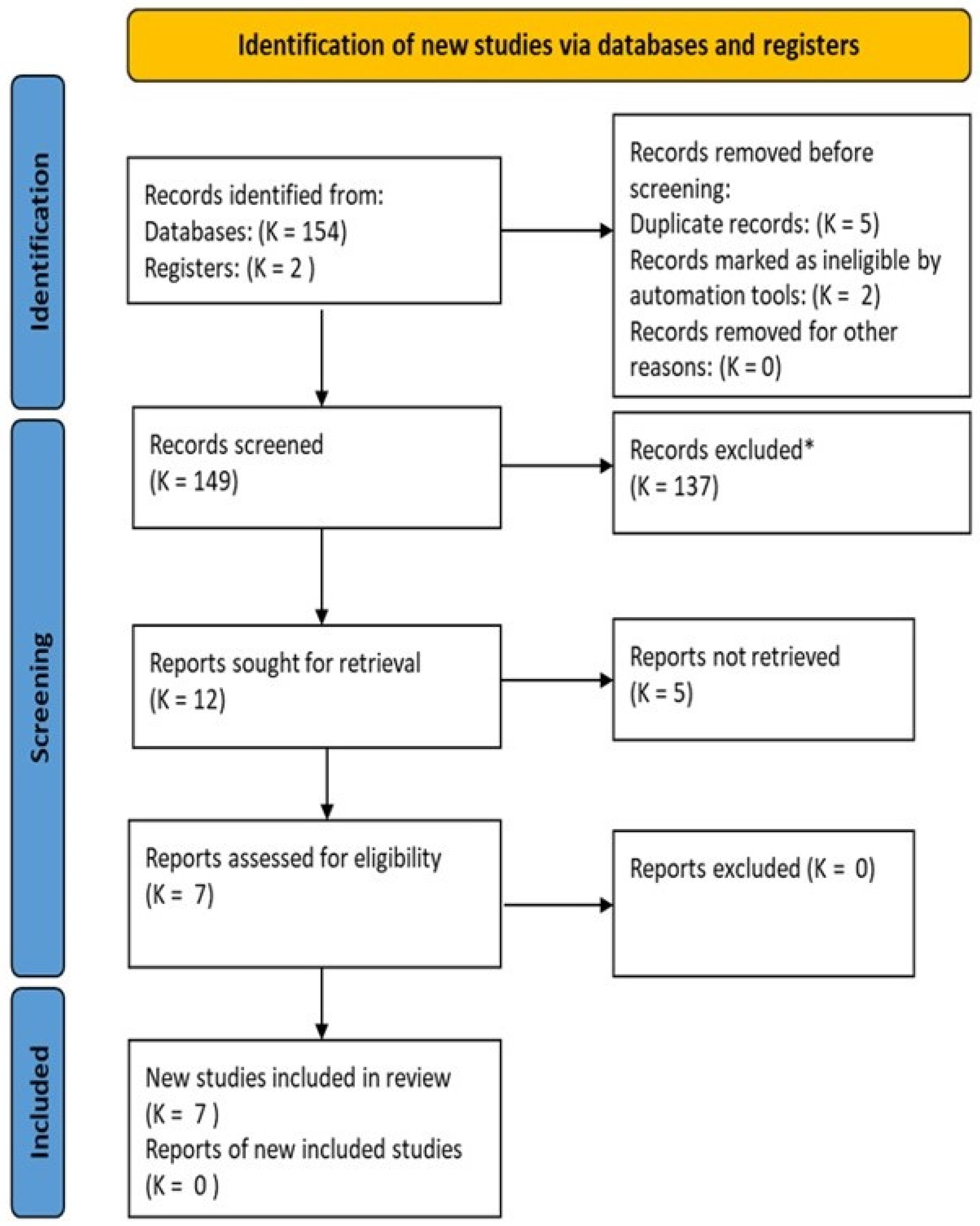
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Criteria for Considering Studies for This Review
2.4. Data Extraction
2.5. Data Analysis and Outcomes
2.6. Evaluation of the Quality and Clinical Relevance
3. Results
3.1. Data Extraction
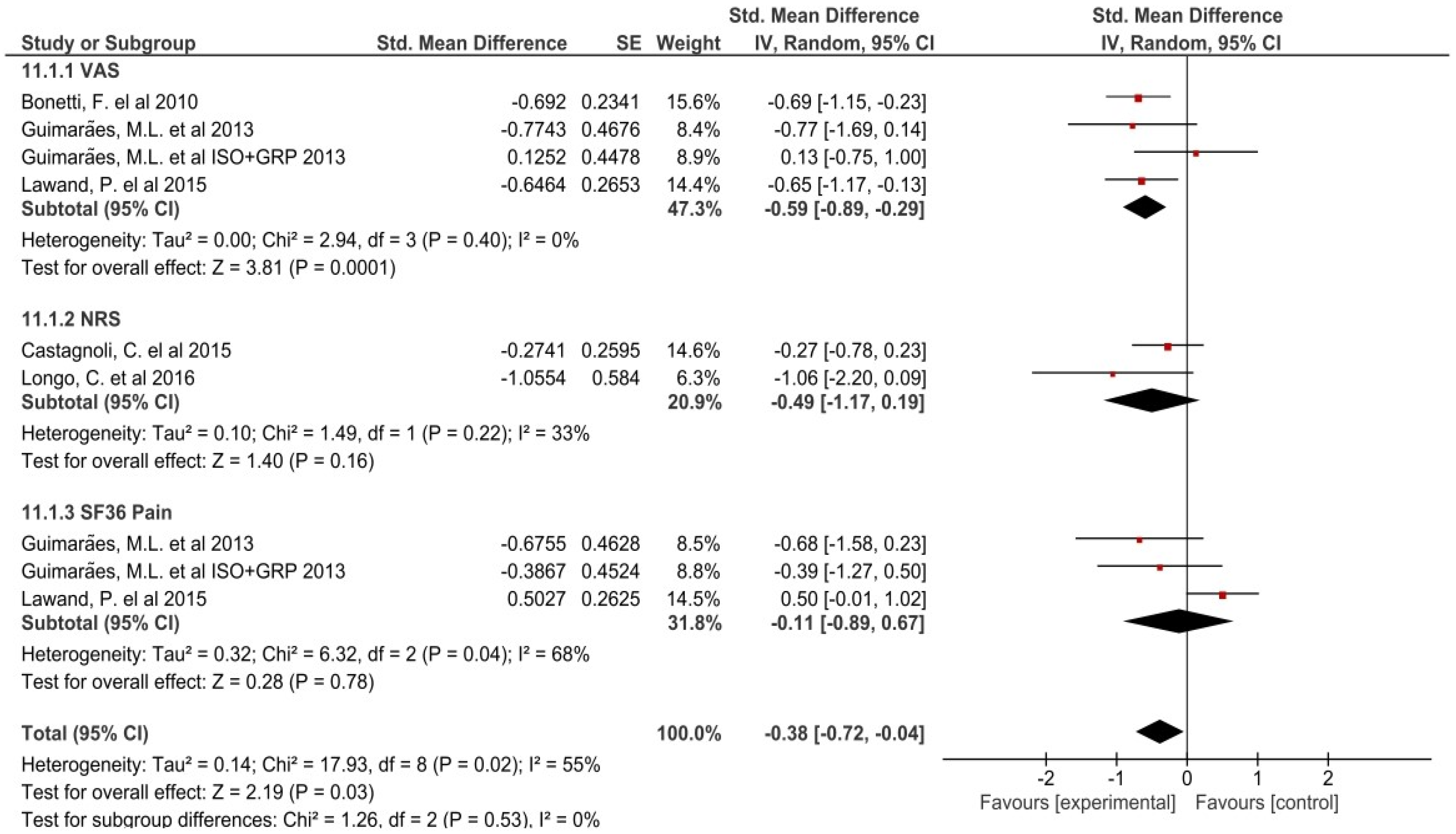
3.2. Data Analysis and Meta-Analyses
3.3. Risk of Bias, Sensitivity and Heterogeneity
3.4. Evaluation of Clinical Relevance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Souchard, P.E. GPR Principles of Global Postural Re-Education; Editorial Paidotribo: Barcelona, Spain, 2005; ISBN 978-84-8019-830-1. [Google Scholar]
- Lawand, P.A.; Jones, A.; Sardim, C.C.; Ribeiro, L.H.; Lombardi, I.; Natour, J. Global postural reeducation to treat chronic low back pain: Randomized, controlled trial. Ann. Rheum. Dis. 2013, 72, A991. [Google Scholar] [CrossRef]
- Todri, J.; Lena, O.; Martínez Gil, J.L. An experimental pilot study of Global Postural Reeducation concerning the cognitive approach of patients with Alzheimer’s disease. Am. J. Alzheimers Dis. Other Demen. 2019, 35, 1533317519867824. [Google Scholar] [CrossRef] [PubMed]
- O’Keeffe, M. Non-pharmacological treatment of low back pain in primary care. Drug Ther. Bull. 2019, 57, 104–108. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Rocha, L.S.; Mineshita, L.N.H.; Sobral, L.L.; Dias Magno, L.; De Souza Santos, M.C.; Barbosa Rocha, R.S. Influence of global postural reeducation method on respiratory muscle strength and parkinsonian quality of life. Man. Ther. Posturol. Rehabil. J. 2018, 15, 1–6. [Google Scholar] [CrossRef][Green Version]
- Agosti, V.; Vitale, C.; Avella, D.; Rucco, R.; Santangelo, G.; Sorrentino, P.; Varriale, P.; Sorrentino, G. Effects of Global Postural Reeducation on gait kinematics in parkinsonian patients: A pilot randomized three-dimensional motion analysis study. Neurol. Sci. 2015, 37, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Cuenca-Martínez, F.; Cortés-Amador, S.; Espí-López, G.V. Effectiveness of classic physical therapy proposals for chronic non-specific low back pain: A literature review. Phys. Ther. Res. 2018, 21, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Bonetti, F.; Curti, S.; Mattioli, S.; Mugnai, R.; Vanti, C.; Violante, F.S.; Pillastrini, P. Effectiveness of a “Global Postural Reeducation” program for persistent Low Back Pain: A non-randomized controlled trial. BMC Musculoskelet. Disord. 2010, 11, 285. [Google Scholar] [CrossRef]
- Guastala, F.A.M.; Guerini, M.H.; Klein, P.F.; Leite, V.C.; Cappellazzo, R.; Facci, L.M. Effect of global postural re-education and isostretching in patients with nonspecific chronic low back pain: A randomized clinical trial. Fisioter. Mov. 2016, 29, 515–525. [Google Scholar] [CrossRef]
- Ehrlich, G.E. Low back pain. Bull. World Health Organ. 2003, 81, 671–676. [Google Scholar] [CrossRef]
- Popescu, A.; Lee, H. Neck Pain and Lower Back Pain. Med. Clin. N. Am. 2020, 104, 279–292. [Google Scholar] [CrossRef]
- Corwell, B.N.; Davis, N.L. The Emergent Evaluation and Treatment of Neck and Back Pain. Emerg. Med. Clin. N. Am. 2020, 38, 167–191. [Google Scholar] [CrossRef]
- Beynon, A.M.; Hebert, J.J.; Lebouef-Yde, C.; Walker, B.F. Potential risk factors and triggers for back pain in children and young adults. A scoping review, part I: Incident and episodic back pain. Chiropr. Man. Ther. 2019, 27, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ma, K.; Zhuang, Z.G.; Wang, L.; Liu, X.G.; Lu, L.J.; Yang, X.Q.; Lu, Y.; Fu, Z.J.; Song, T.; Huang, D.; et al. The Chinese Association for the Study of Pain (CASP): Consensus on the Assessment and Management of Chronic Nonspecific Low Back Pain. Pain Res. Manag. 2019, 2019, 8957847. [Google Scholar] [CrossRef]
- Grotle, M.; Brox, J.I.; Vøllestad, N.K. Functional status and disability questionnaires: What do they assess? A systematic review of back-specific outcome questionnaires. Spine 2005, 30, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, G.E.; Barreto, R.G.P.; Robinson, C.C.; Plentz, R.D.M.; Silva, M.F. Global Postural Reeducation for patients with musculoskeletal conditions: A systematic review of randomized controlled trials. Braz. J. Phys. Ther. 2016, 20, 194–205. [Google Scholar] [CrossRef] [PubMed]
- Page, M.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffman, T.; Mulrow, C.; Shamseer, L.; Tetzlaff, J.; Akl, E.; Brennan, S.; et al. The PRISMA 2020statement: An updated guidelinefor reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P. It’s time for change with the management of non-specific chronic low back pain. Br. J. Sports Med. 2012, 46, 224–227. [Google Scholar] [CrossRef] [PubMed]
- Guimarães Resende Adorno, M.L.; Pereira Brasil-Neto, J. Assessment of the quality of life through the SF-36 questionnaire in patients with chronic nonspecific low back pain. Acta Ortop. Bras. 2013, 21, 202–207. [Google Scholar] [CrossRef]
- Castagnoli, C.; Cecchi, F.; Del Canto, A.; Paperini, A.; Boni, R.; Pasquini, G.; Vannetti, F.; Macchi, C. Effects in short and long term of Global Postural Reeducation (GPR) on Chronic Low Back Pain: A controlled study with one-year follow-up. Sci. World J. 2015, 2015, 271436. [Google Scholar] [CrossRef] [PubMed]
- Longo, C.A.; Ferrari, S.; Lanza, A.; Vanti, C.; Stradiotti, P.A. Effects of the “standing posture with flexion of the trunk” on the lumbar multifidus tropism in patients with chronic low back pain. A randomized, controlled pilot study. Sci. Riabil. 2016, 18, 5–12. [Google Scholar]
- Soares, P.; Cabral, V.; Mendes, M.; Vieira, R.; Aviolo, G.; de Souza Vale, R.G. Efeitos do Programa Escola de Postura e Reeducacão Postural Global sobre a amplitude de movimento e níveis de dor em pacientes com lombalgia crônica. Rev. Andaluza Med. Deport. 2016, 9, 23–28. [Google Scholar] [CrossRef]
- Lawand, P.; Lombardi, I., Jr.; Jones, A.; Sardim, C.; Ribeiro, L.H.; Natour, J. Effect of a muscle stretching program using the global postural reeducation method for patients with chronic low back pain: A randomized controlled trial. Jt. Bone Spine 2015, 82, 272–277. [Google Scholar] [CrossRef]
- Cochrane. Cochrane Training. Available online: https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman (accessed on 3 February 2019).
- Epidemiología General y Demografía Sanitaria, 2010–2011. Open Course Ware (16633). In Epidat: Pruebas Diagnósticas [Internet]; Universidad, Campus de Excelencia: Salamanca, Spain, 2005; [Citado 1 de Mayo de 2014]; Available online: http://ocw.usal.es/ciencias-biosanitarias/epidemiologia-general-y-demografia-sanitaria/contenidos/01PROGRAMATE0RICO/01EPIDEMIOLOGIAenPDF/Tema08enPDF/08Tema8EstudiosEpidemiologicosDescriptivos.pdf (accessed on 3 February 2019).
- Neura. University of Sydney Physiotherapy Evidence Database. Available online: https://www.pedro.org.au/english/downloads/pedro-scale/ (accessed on 1 March 2019).
- McMaster University and Evidence Prime Inc. GRADEPro. GTD. Available online: https://gradepro.org/ (accessed on 4 May 2019).
- Dönmez, U.; Ozturk, C.; Kocanaogullari, H.; Gucenmez, S.; Hepguler, S. Do physical therapy modalities have additional benefit over exercise therapy in the management of ankylosing spondylitis? A randomized controlled trial. Ann. Rheum. Dis. 2014, 73, 727. [Google Scholar] [CrossRef]
- de Melo Gomes, A.V.; Lopes, D.C.; Veloso, E.M.C.; da Costa, R.C.T.S. A influência do método de reeducação postural global sobre a flexibilidade dos músculos da cadeia posterior. Fisioter. Bras. 2014, 15, 203–209. [Google Scholar]
- Lozano-Quijada, C.; Poveda-Pagán, E.J.; Segura-Heras, J.V.; Hernández-Sánchez, S.; Prieto-Castelló, M.J. Changes in postural sway after a single global postural reeducation session in university students: A randomized controlled trial. J. Manip. Physiol. Ther. 2017, 40, 467–476. [Google Scholar] [CrossRef]
- De Amorim, C.S.M.; Gracitelli, M.E.C.; Marques, A.P.; Dos Santos Alves, V.L. Effectiveness of global postural reeducation compared to segmental exercises on function, pain, and quality of life of patients with scapular dyskinesis associated with neck pain: A preliminary clinical trial. J. Manip. Physiol. Ther. 2014, 37, 441–447. [Google Scholar] [CrossRef]
- Fatoye, F.; Gebrye, T.; Odeyemi, I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol. Int. 2019, 39, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-las-Peñas, C.; Alonso-Blanco, C.; Morales-Cabezas, M.; Miangolarra-Page, J.C. Two exercise interventions for the management of patients with ankylosing spondylitis: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2005, 84, 407–419. [Google Scholar] [CrossRef] [PubMed]
- Mota, Y.L.; Barreto, S.L.; Bin, P.R.; Simões, H.G.; Campbell, C.S.G. Cardiovascular responses in the seated posture of the Global Postural Reeducation (GPR) method. Rev. Bras. Fisioter. 2008, 12, 161–168. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Abraira, V.; Royuela, A.; Corcoll, J.; Alegre, L.; Cano, A.; Muriel, A.; Zamora, J.; Gil Del Real, M.T.; Gestoso, M.; et al. Minimal clinically important change for pain intensity and disability in patients with nonspecific low back pain. Spine 2007, 32, 2915–2920. [Google Scholar] [CrossRef]
- Smeets, R.; Köke, A.; Lin, C.W.; Ferreira, M.; Demoulin, C. Measures of function in low back pain/disorders: Low Back Pain Rating Scale (LBPRS), Oswestry Disability Index (ODI), Progressive Isoinertial Lifting Evaluation (PILE), Quebec Back Pain Disability Scale (QBPDS), and Roland-Morris Disability Questionnaire. Arthritis Care Res. 2011, 63, 158–173. [Google Scholar] [CrossRef]
- Ostelo, R.W.J.G.; Deyo, R.A.; Stratford, P.; Waddell, G.; Croft, P.; Von Korff, M.; Bouter, L.M.; De Vet, H.C. Interpreting change scores for pain and functional status in low back pain: Towards international consensus regarding minimal important change. Spine 2008, 33, 90–94. [Google Scholar] [CrossRef]
- Searle, A.; Spink, M.; Ho, A.; Chuter, V. Exercise interventions for the treatment of chronic low back pain: A systematic review and meta-analysis of randomised controlled trials. Clin. Rehabil. 2015, 29, 1155–1167. [Google Scholar] [CrossRef] [PubMed]
- Matarán-Peñarrocha, G.; Lara Palomo, I.; Soler, E.A.; Gil-Martínez, E.; Fernández-Sánchez, M.; Aguilar-Ferrándiz, M.; Castro-Sánchez, A. Comparison of efficacy of a supervised versus non-supervised physical therapy exercise program on the pain, functionality and quality of life of patients with non-specific chronic low-back pain: A randomized controlled trial. Clin. Rehabil. 2020, 34, 948–959. [Google Scholar] [CrossRef]
- Yates, M.; Shastri-Hurst, N. The oswestry disability index. Occup. Med. 2017, 67, 241–242. [Google Scholar] [CrossRef]
- Revicki, D.; Hays, R.D.; Cella, D.; Sloan, J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J. Clin. Epidemiol. 2008, 61, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Stratford, P.W.; Binkley, J.; Solomon, P.; Finch, E.; Gill, C.; Moreland, J. Defining the minimum level of detectable change for the roland morris questionnaire. Phys. Ther. 1996, 76, 359–365. [Google Scholar] [CrossRef]
- Zhu, F.; Zhang, M.; Wang, D.; Hong, Q.; Zeng, C.; Chen, W. Yoga compared to non-exercise or physical therapy exercise on pain, disability, and quality of life for patients with chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2020, 15, e0238544. [Google Scholar] [CrossRef] [PubMed]
- Lomas-Vega, R.; Garrido-Jaut, M.V.; Rus, A.; Del-Pino-Casado, R. Effectiveness of Global Postural Re-education for Treatment of Spinal Disorders. Am. J. Phys. Med. Rehabil. 2017, 96, 124–130. [Google Scholar] [CrossRef]
- Gonzalez-Medina, G.; Perez-Cabezas, V.; Marin-Paz, A.-J.; Galán-Mercant, A.; Ruiz-Molinero, C.; Jimenez-Rejano, J.J. Effectiveness of Global Postural Reeducation in Ankylosing Spondylitis: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2696. [Google Scholar] [CrossRef]
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.B.; Goode, A.P.; George, S.Z.; Cook, C.E. Incidence and risk factors for first-time incident low back pain: A systematic review and meta-analysis. Spine J. 2014, 14, 2299–2319. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Martin, P.; Buist, L. An active finite viscoelastic model for gastric smooth muscle contraction. bioRxiv 2021. [Google Scholar] [CrossRef]



| The Authors Year/Objective | Sample | Intervention | Timeline and Follow-Up | Outcome Measure | Study Results |
|---|---|---|---|---|---|
| Bonetti, F. et al., 2010 [8] To evaluate the GPR effectiveness as compared to a Stabilization Exercise (SE) program in subjects with persistent low back pain (LBP) at short- and mid-term follow-up. | n = 100 Gender G1: M:22; F: 28 G2: M:18; F:32 Age (years): G1: 45.5 (12.2) G2:48.2 (13.2) | G1: GRP (n = 42) G2: stabilization exercise (n = 36) Drop out n = 22 |
| RMDQ VAS ODI FFT | G1 vs. G2 RMDQ, p < 0.001 VAS, p < 0.001 ODI, p = 0.003 FFT, p = 0.008 |
| Guimarães, ML. et al., 2013 [19] To evaluate the quality of life (QL) with the use of the SF-36 questionnaire in patients with chronic nonspecific low back pain (CNLBP). | n = 30 Gender G1: M:4; F: 6 G2: M:3; F:7 G3: M:3; F:7 | G1: isostretching (n = 10)G2: GRP (n = 10) G3: isostretching + GPR (n = 10) |
| VASSF-36 | VAS G1: N/A; G2: p < 0.001; G: N/A SF36 G1: N/A; G2: p < 0.001; G: N/A |
| Castagnoli, C. et al., 2015 [20] Comparing global postural re-education (GPR) to a standard physiotherapy treatment (PT) based on active exercises, stretching and massaging to improve pain and function in chronic low back pain (CLBP) patients. | n = 79 Gender G1: M:4; F: 26 G2: M:7; F:23 Age (years): G1: 58.97 (0.44) G2: 62.54 (13.19) | G1: GRP (n = 30) G2: protocol treatment (n = 30) Drop out n = 19 |
| RMDQNRS | RMDQ G1(T0 vs. T1) p < 0.00; G1 (T0 vs. T2) p = 0.24 G2(T0 vs. T1) p < 0.00; G2 (T0 vs. T2) p = 0.12 NRSG1(T0 vs. T1) p < 0.00; G1 (T0 vs. T2) p = 0.02 G2(T0 vs. T1) p < 0.00; G2 (T0 vs. T2) p = 0.12 |
| Lawand, P. et al., 2015 [23] To assess to assess the effect of a muscle stretching program using the GPR method in pain, function, quality of life and depressive symptoms in patients with chronic low back pain. | n = 61 Gender G1: M:6; F: 25 G2: M:8; F:22 Age (years): G1: 49.4 (12.0) G2: 47.5 (11.9) | G1: GRP (n = 31) G2: drug treatment (n = 30) |
| RMQ VAS SF-36 Beck Inventory | RMQ G1 p < 0.001; G2 p = 0.264; G1 vs. G2 p < 0.001 VASG1 p < 0.001; G2 p = 0.340; G1 vs. G2 p < 0.001 SF36 G1 vs. G2
|
| Soares, P. et al., 2015 [22] To compare the effects of the school of posture program (PEP) and global postural re-education (RPG) on pain levels and range of motion in patients with chronic low back pain. | n = 30 Gender N/A Age (years): G1: 46.3 (8.5) G2: 43.6 (10.93) G3: 44.30 (10.68) | G1: GRP (n = 10) G2: back school exercises and muscle strengthening (n = 10) G3: control (n = 10) |
| Borg scale CR10 Goniometry | Borg Scale G1 vs. G3, p < 0.0001 G2 vs. G3, p < 0.0001 G1 vs. G2, p > 0.05 Hip extension G1 vs. G3, p = 0.019 G2 vs. G3, p = 0.006 G1 vs. G2, p > 0.05 Lumbar spine flexion G1 vs. G3, p = 0.020 G2 vs. G3, p = 0.018 G1 vs. G2, p > 0.05 Reduction of pain scores in back |
| Moreschi, F. et al., 2016 [9] To analyze changes in muscle strength, flexibility, function and pain in patients with chronic low back pain who underwent isostretching and global posture re-education (GPR). | n = 43 Gender G1: M:5; F:16 G2: M:3; F: 15 Age (years): G1: 50.50 G2: 52 | G1: GRP (n = 21) G2: isostretching (n = 18) Drop out n = 4 |
| RMQ VAS Sit and reach test Dynamometry postural analysis | RMQ G1 p = 0.000; G2 p = 0.000; G1 vs. G2 p = 0.192 VAS G1 p = 0.001; G2 p = 0.000; G1 vs. G2 p = 0.494 Sit and reach test G1 p = 0.006; G2 p = 0.039; G1 vs. G2 p > 0.15 Dynamometry G1 p = 0.002; G2 p = 0.000; G1 vs. G2 p > 0.15 Postural analysis G1 p = 0.001; G2 p = 0.007; p > 0.15 |
| Longo, C. et al., 2016 [21] To investigate whether the standing posture with flexion of the trunk added to a standard group physical therapy may increase the LM thickness (primary aim) and reduce pain and disability (secondary aim) in patients with chronic non-specific LBP. | n = 14 Gender G1: M:2; F:5 G2: M:2; F: 5 Age (years): G1: 54.57 (8.16) G2: 49.14 (9.92) | G1: GRP (n = 7) G2: standard protocol (n = 7) |
| RMQ NRS Ultrasound examination | RMQ (T1-T0) G1 vs. G2 p = 0.018 (T2-T0) G1 vs. G2 p = 0.042 NRS (T1-T0) G1 vs. G2 p = 0.071 (T2-T0) G1 vs, G2 p = 0.891 Ultrasound examination (T1-T0) G1 vs. G2 p > 0.05 |
| Variable | Begg (p) | Egger (p) |
|---|---|---|
| RMDQ | p = 0.3082 | p = 0.3670 |
| ODI | p = 1.0000 | |
| VAS | p = 0.2963 | p = 0.3247 |
| NRS | p = 1.000 | |
| VAS + NRS | p = 0.8065 | p = 0.5766 |
| Evaluation Criteria (Items) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author, Year | ||||||||||||
| Bonetti, F. et al., 2010 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Guimarães, M.L. et al., 2013 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 |
| Castagnoli, C. et al., 2015 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| Lawand, P. et al., 2015 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Soares, P. et al., 2015 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 4 |
| Moreschi, F.A. et al., 2016 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Longo, C. et al., 2016 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Pecorone, F. et al., 2020 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Certainty Assessment | No. of Patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | RPG | Placebo | Relative (95% CI) | Absolute (95% CI) | ||
| RMDQ (follow-up: range 2 months to 7 months; scale: from 0 to 24) | ||||||||||||
| 4 | randomized trials | not serious | not serious | not serious | not serious | none | 109 | 103 | - | SMD 0.55 lower (0.83 lower to 0.27 lower) | ⨁⨁⨁⨁ HIGH | IMPORTANT |
| ODI | ||||||||||||
| 2 | randomized trials | not serious | not serious | not serious | not serious | none | 72 | 66 | - | SMD 0.48 lower (0.82 lower to 0.14 lower) | ⨁⨁⨁⨁ HIGH | IMPORTANT |
| VAS | ||||||||||||
| 3 | randomized trials | not serious | not serious | not serious | serious | strong association | 82 | 76 | - | SMD 0.69 lower (1.01 lower to 0.37 lower) | ⨁⨁⨁⨁ HIGH | IMPORTANT |
| NSR | ||||||||||||
| 3 | randomized trials | not serious | not serious | not serious | not serious | none | 58 | 55 | - | SMD 0.49 lower (0.87 lower to 0.12 lower) | ⨁⨁⨁⨁ HIGH | NO IMPORTANT |
| VAS + NRS | ||||||||||||
| 5 | randomized trials | not serious | not serious | not serious | not serious | none | 119 | 113 | - | MD 1.32 lower (1.87 lower to 0.77 lower) | ⨁⨁⨁⨁ HIGH | IMPORTANT |
| SF36 | ||||||||||||
| 3 | randomized trials | not serious | not serious | not serious | not serious | none | 50/50 (100.0%) | 50/50 (100.0%) | not estimable | ⨁⨁⨁⨁ HIGH | NO IMPORTANT | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonzalez-Medina, G.; Perez-Cabezas, V.; Ruiz-Molinero, C.; Chamorro-Moriana, G.; Jimenez-Rejano, J.J.; Galán-Mercant, A. Effectiveness of Global Postural Re-Education in Chronic Non-Specific Low Back Pain: Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5327. https://doi.org/10.3390/jcm10225327
Gonzalez-Medina G, Perez-Cabezas V, Ruiz-Molinero C, Chamorro-Moriana G, Jimenez-Rejano JJ, Galán-Mercant A. Effectiveness of Global Postural Re-Education in Chronic Non-Specific Low Back Pain: Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(22):5327. https://doi.org/10.3390/jcm10225327
Chicago/Turabian StyleGonzalez-Medina, Gloria, Veronica Perez-Cabezas, Carmen Ruiz-Molinero, Gema Chamorro-Moriana, Jose Jesus Jimenez-Rejano, and Alejandro Galán-Mercant. 2021. "Effectiveness of Global Postural Re-Education in Chronic Non-Specific Low Back Pain: Systematic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 22: 5327. https://doi.org/10.3390/jcm10225327
APA StyleGonzalez-Medina, G., Perez-Cabezas, V., Ruiz-Molinero, C., Chamorro-Moriana, G., Jimenez-Rejano, J. J., & Galán-Mercant, A. (2021). Effectiveness of Global Postural Re-Education in Chronic Non-Specific Low Back Pain: Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 10(22), 5327. https://doi.org/10.3390/jcm10225327







