Hormonal Characteristics of Women Receiving Ovarian Tissue Transplantation with or without Endogenous Ovarian Activity
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Cryopreservation and Transplantation of Ovarian Tissue
2.3. Follow-Up after Transplantation
2.4. Statistical Methods
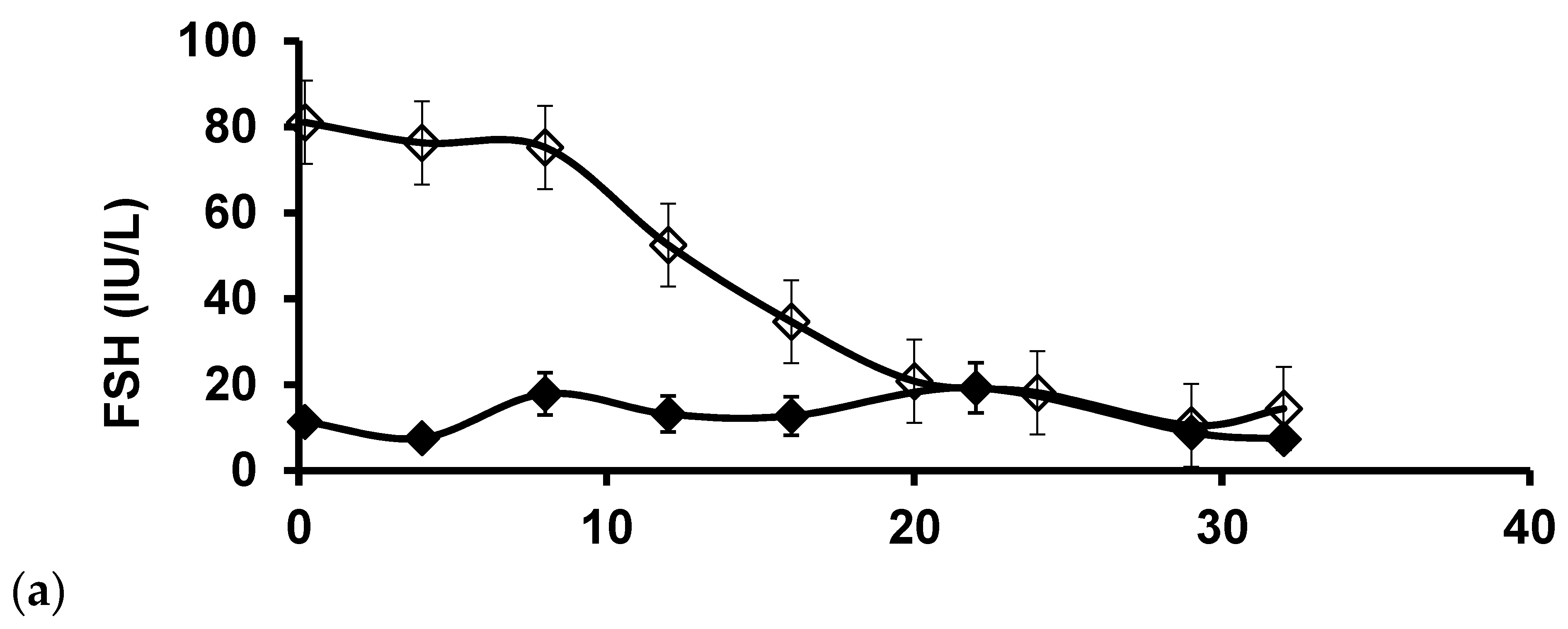
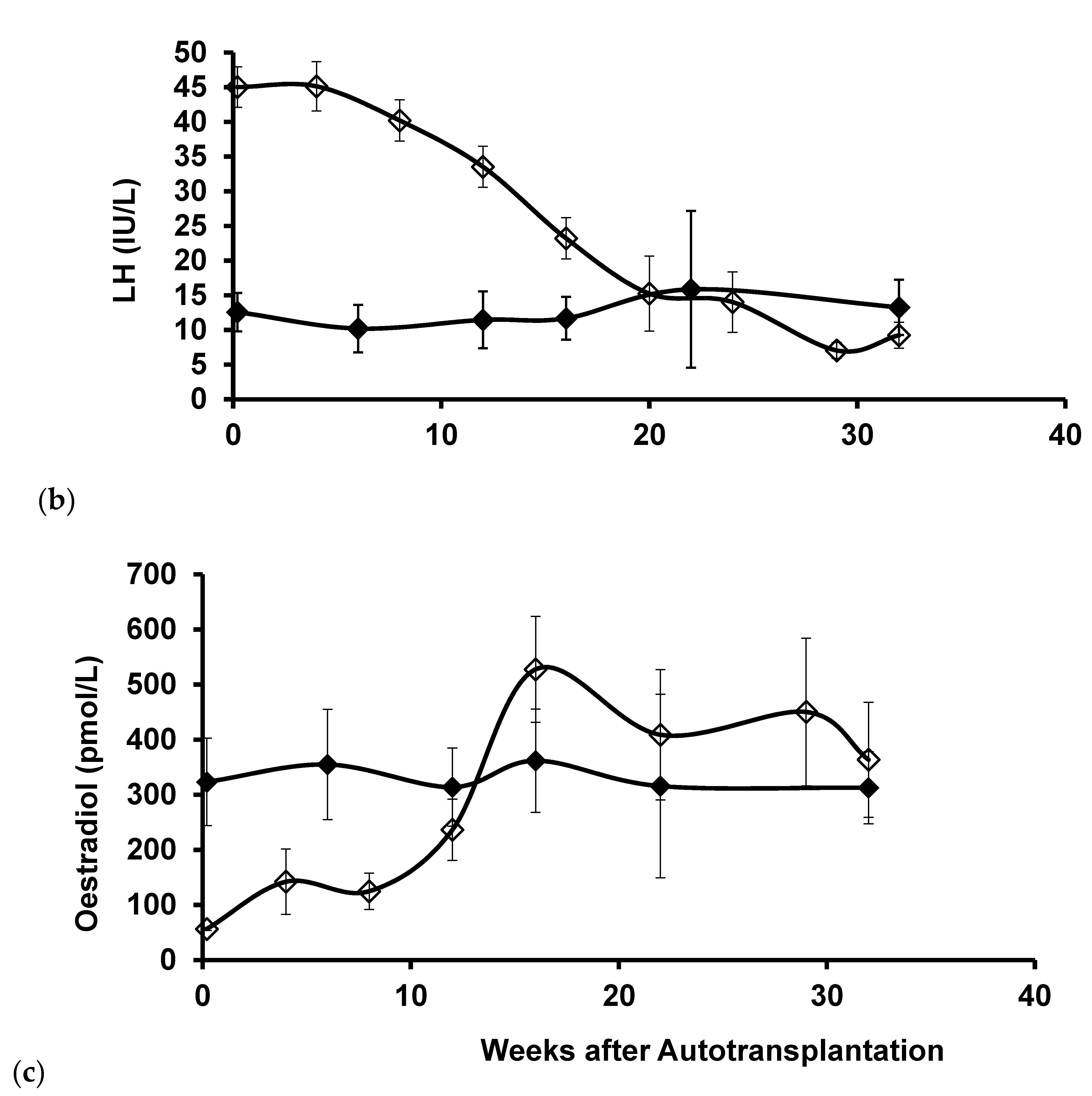
3. Results
Patient Characteristics
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Westergaard, C.G.; Byskov, A.G.; Andersen, C.Y. Morphometric characteristics of the primordial to primary follicle transi-tion in the human ovary in relation to age. Hum. Reprod. 2007, 22, 2225–2231. [Google Scholar] [CrossRef]
- Andersen, C.Y.; Mamsen, L.S.; Kristensen, S.G. FERTILITY PRESERVATION: Freezing of ovarian tissue and clinical opportunities. Reproduction 2019, 158, F27–F34. [Google Scholar] [CrossRef]
- Kristensen, S.G.; Liu, Q.; Mamsen, L.S.; Greve, T.; Pors, S.E.; Bjørn, A.B.; Ernst, E.; Macklon, K.T.; Andersen, C.Y. A simple method to quantify follicle survival in cryopreserved human ovarian tissue. Hum. Reprod. 2018, 33, 2276–2284. [Google Scholar] [CrossRef]
- Dolmans, M.-M.; Donnez, J.; Cacciottola, L. Fertility Preservation: The Challenge of Freezing and Transplanting Ovarian Tissue. Trends Mol. Med. 2021, 27, 777–791. [Google Scholar] [CrossRef]
- Andersen, C.Y.; Kristensen, S.G.; Greve, T.; Schmidt, K.T. Cryopreservation of ovarian tissue for fertility preservation in young female oncological patients. Futur. Oncol. 2012, 8, 595–608. [Google Scholar] [CrossRef]
- Baird, D.T.; Webb, R.; Campbell, B.K.; Harkness, L.M.; Gosden, R.G. Long-term ovarian function in sheep after ovariectomy and transplantation of autografts stored at −196 °C. Endocrinology 1999, 140, 462–471. [Google Scholar] [CrossRef]
- Nugent, D.; Newton, H.; Gallivan, L.; Gosden, R.G. Protective effect of vitamin E on ischaemia-reperfusion injury in ovarian grafts. J. Reprod. Fertil. 1998, 114, 341–346. [Google Scholar] [CrossRef]
- Nisolle, M.; Casanas-Roux, F.; Qu, J.; Motta, P.; Donnez, J. Histologic and ultrastructural evaluation of fresh and frozen-thawed human ovarian xenografts in nude mice. Fertil. Steril. 2000, 74, 122–129. [Google Scholar] [CrossRef]
- Mamsen, L.S.; Olesen, H.Ø.; Pors, S.E.; Hu, X.; Bjerring, P.; Christiansen, K.; Adrados, C.S.; Andersen, C.Y.; Kristensen, S.G. Effects of Er:YAG laser treatment on re-vascularization and follicle survival in frozen/thawed human ovarian cortex transplanted to immunodeficient mice. J. Assist. Reprod. Genet. 2021. [Google Scholar] [CrossRef]
- Dolmans, M.-M.; von Wolff, M.; Poirot, C.; Diaz-Garcia, C.; Cacciottola, L.; Boissel, N.; Liebenthron, J.; Pellicer, A.; Donnez, J.; Andersen, C.Y. Transplantation of cryopreserved ovarian tissue in a series of 285 women: A review of five leading European centers. Fertil. Steril. 2021, 115, 1102–1115, in press. [Google Scholar] [CrossRef]
- Greve, T.; Schmidt, K.T.; Kristensen, S.G.; Ernst, E.; Andersen, C.Y. Evaluation of the ovarian reserve in women transplanted with frozen and thawed ovarian cortical tissue. Fertil. Steril. 2012, 97, 1394–1398.e1. [Google Scholar] [CrossRef]
- Demeestere, I.; Simon, P.; Emiliani, S.; Delbaere, A.; Englert, Y. Orthotopic and heterotopic ovarian tissue transplantation. Hum. Reprod. Updat. 2009, 15, 649–665. [Google Scholar] [CrossRef] [PubMed]
- Shikanov, A.; Zhang, Z.; Xu, M.; Smith, R.M.; Rajan, A.; Woodruff, T.; Shea, L.D. Fibrin Encapsulation and Vascular Endothelial Growth Factor Delivery Promotes Ovarian Graft Survival in Mice. Tissue Eng. Part A 2011, 17, 3095–3104. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A.; Nakamura, H.; Tabata, Y.; Fujimori, Y.; Kumasawa, K.; Kimura, T. Effect of sustained release of basic fibroblast growth factor using biodegradable gelatin hydrogels on frozen-thawed human ovarian tissue in a xenograft model. J. Obstet. Gynaecol. Res. 2018, 44, 1947–1955. [Google Scholar] [CrossRef]
- Suzuki, H.; Ishijima, T.; Maruyama, S.; Ueta, Y.Y.; Abe, Y.; Saitoh, H. Beneficial effect of desialylated erythropoietin administration on the frozen-thawed canine ovarian xenotransplantation. J. Assist. Reprod. Genet. 2008, 25, 571–575. [Google Scholar] [CrossRef][Green Version]
- Kim, E.J.; Lee, H.J.; Lee, J.; Youm, H.W.; Lee, J.R.; Suh, C.S.; Kim, S.H. The beneficial effects of polyethylene glycol-superoxide dis-mutase on ovarian tissue culture and transplantation. J. Assist. Reprod. Genet. 2015, 32, 1561–1569. [Google Scholar] [CrossRef]
- Manavella, D.; Cacciottola, L.; Desmet, C.M.; Jordan, B.F.; Donnez, J.; Amorim, C.A.; Dolmans, M.M. Adipose tissue-derived stem cells in a fibrin implant enhance neovascularization in a peritoneal grafting site: A potential way to improve ovarian tissue transplantation. Hum. Reprod. 2018, 33, 270–279. [Google Scholar] [CrossRef]
- Manavella, D.; Cacciottola, L.; Payen, V.L.; Amorim, C.A.; Donnez, J.; Dolmans, M.M. Adipose tissue-derived stem cells boost vascularization in grafted ovarian tissue by growth factor secretion and differentiation into endothelial cell lineages. Mol. Hum. Reprod. 2019, 25, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Shojafar, E.; Mehranjani, M.S.; Shariatzadeh, S.M.A. Adipose derived mesenchymal stem cells improve the structure and function of autografted mice ovaries through reducing oxidative stress and inflammation: A stereological and bio-chemical analysis. Tissue Cell 2019, 56, 23–30. [Google Scholar] [CrossRef]
- Au, P.; Tam, J.; Fukumura, D.; Jain, R.K. Bone marrow–derived mesenchymal stem cells facilitate engineering of long-lasting functional vasculature. Blood 2008, 111, 4551–4558. [Google Scholar] [CrossRef]
- Huang, B.; Lu, J.; Ding, C.; Zou, Q.; Wang, W.; Li, H. Exosomes derived from human adipose mesenchymal stem cells improve ovary function of premature ovarian insufficiency by targeting SMAD. Stem Cell Res. Ther. 2018, 9, 216. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J.; Silber, S.; Andersen, C.Y.; Demeestere, I.; Piver, P.; Meirow, D.; Pellicer, A.; Dolmans, M.M. Children born after autotrans-plantation of cryopreserved ovarian tissue. A review of 13 live births. Ann. Med. 2011, 43, 437–450. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J.; Dolmans, M.M.; Pellicer, A.; Diaz-Garcia, C.; Serrano, M.S.; Schmidt, K.T.; Ernst, E.; Luyckx, V.; Andersen, C.Y. Restoration of ovarian activity and pregnancy after transplantation of cryopreserved ovarian tissue: A review of 60 cases of reimplantation. Fertil. Steril. 2013, 99, 1503–1513. [Google Scholar] [CrossRef]
- Macklon, K.T.; Jensen, A.K.; Loft, A.; Ernst, E.; Andersen, C.Y. Treatment history and outcome of 24 deliveries worldwide after autotransplantation of cryopreserved ovarian tissue, including two new Danish deliveries years after autotransplantation. J. Assist. Reprod. Genet. 2014, 31, 1557–1564. [Google Scholar] [CrossRef][Green Version]
- Hornshøj, V.G.; Dueholm, M.; Mamsen, L.S.; Ernst, E.; Andersen, C.Y. Hormonal response in patients transplanted with cryo-preserved ovarian tissue is independent of whether freezing was performed in childhood or in adulthood. J. Assist. Reprod. Genet. 2021, 1–7. [Google Scholar] [CrossRef]
- Silber, S.J.; DeRosa, M.; Goldsmith, S.; Fan, Y.; Castleman, L.; Melnick, J. Cryopreservation and transplantation of ovarian tissue: Results from one center in the USA. J. Assist. Reprod. Genet. 2018, 35, 2205–2213. [Google Scholar] [CrossRef] [PubMed]
- Gougeon, A. Regulation of ovarian follicular development in primates: Facts and hypotheses. Endocr. Rev. 1996, 17, 121–155. [Google Scholar] [CrossRef]
- Andersen, C.Y.; Byskov, A.G.; Andersen, A.N. Cryopreservation of human ovarian tissue. Ugeskr. Laeger 2001, 163, 5007–5013. [Google Scholar]
- Dewailly, D.; Andersen, C.Y.; Balen, A.; Broekmans, F.; Dilaver, N.; Fanchin, R.; Griesinger, G.; Kelsey, T.; La Marca, A.; Lambalk, C.; et al. The physiology and clinical utility of anti-Müllerian hormone in women. Hum. Reprod. Updat. 2014, 20, 370–385. [Google Scholar] [CrossRef]
- Jeppesen, J.V.; Anderson, R.A.; Kelsey, T.W.; Christiansen, S.L.; Kristensen, S.G.; Jayaprakasan, K.; Raine-Fenning, N.; Campbell, B.K.; Andersen, C.Y. Which follicles make the most anti-Mullerian hormone in humans? Evidence for an abrupt decline in AMH production at the time of follicle selection. Mol. Hum. Reprod. 2013, 19, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Janse, F.; Donnez, J.; Anckaert, E.; De Jong, F.H.; Fauser, B.C.; Dolmans, M.-M. Limited Value of Ovarian Function Markers following Orthotopic Transplantation of Ovarian Tissue after Gonadotoxic Treatment. J. Clin. Endocrinol. Metab. 2011, 96, 1136–1144. [Google Scholar] [CrossRef]
- Wallace, W.; Kelsey, T. Human ovarian reserve from conception to the menopause. PLoS ONE 2010, 5, e8772. [Google Scholar] [CrossRef] [PubMed]
- Rabinovici, J.; Blankstein, J.; Goldman, B.; Rudak, E.; Dor, Y.; Pariente, C.; Geier, A.; Lunenfeld, B.; Mashiach, S. In vitro fertilization and primary embryonic cleavage are possible in 17 alpha-hydroxylase deficiency despite extremely low intrafollicular 17 beta-estradiol. J. Clin. Endocrinol. Metab. 1989, 68, 693–697. [Google Scholar] [CrossRef]
- Morselli, E.; Santos, R.S.; Criollo, A.; Nelson, M.D.; Palmer, B.F.; Clegg, D.J. The effects of oestrogens and their receptors on cardiometabolic health. Nat. Rev. Endocrinol. 2017, 13, 352–364. [Google Scholar] [CrossRef]
- Felty, Q. Estrogen-induced DNA synthesis in vascular endothelial cells is mediated by ROS signaling. BMC Cardiovasc. Disord. 2006, 6, 16. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, K.; Banerjee, S.; Saxena, N.K.; Banerjee, S.K. Thombospondin-1 disrupts estrogen-induced endothelial cell proliferation and migration and its expression is suppressed by estradiol. Mol. Cancer Res. 2004, 2, 150–158. [Google Scholar] [PubMed]
- Geraldes, P.; Sirois, M.G.; Tanguay, J.F. Specific contribution of estrogen receptors on mitogen-activated protein kinase path-ways and vascular cell activation. Circ. Res. 2003, 93, 399–405. [Google Scholar] [CrossRef]
- Gellert, S.E.; Pors, S.E.; Kristensen, S.G.; Bay-Bjørn, A.M.; Ernst, E.; Andersen, C.Y. Transplantation of frozen-thawed ovarian tissue: An update on worldwide activity published in peer-reviewed papers and on the Danish cohort. J. Assist. Reprod. Genet. 2018, 35, 561–570. [Google Scholar] [CrossRef] [PubMed]
| No. Women | Age at OTC (years) | No. Cortical Pieces Frozen | Ovarian Volume (mL) | Age at OTT (years) | No. Pieces Transplanted | % of One Ovary Grafted * | |
|---|---|---|---|---|---|---|---|
| Postmenopausal (FSH: >40 IU/L) | 51 | 26 ± 1.1 * (9–39) (27.6) | 23 ± 1.1 (9–49) (22) | 6.6 ± 0.5 (1.8–12.2) (6.0) | 31 ± 0.8 * (14–42) (31.2) | 9.5 ± 0.4 * (2–16) (10) | 43 ± 1.7 * (18–77) (42) |
| Not menopausal FSH: ≤40 IU/L) | 23 | 30 ± 1.2 * (15–37) (30.7) | 21 ± 1.2 (8–31) (21) | 7.0 ± 0.8 (2.1–18.3) (6.2) | 35 ± 1.1 * (26–44) (35.9) | 11 ± 0.9 * (5–22) (10) | 59 ± 4.3 * (21–100) (55) |
| No. Women | AMH Measurements below DL Prior to OTT | Pt. with AMH Increase | Age at OTC | Age at OTT | % Tissue Grafted | Age at OTC | Age at OTT | % Tissue Grafted | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| AMH | Postmenopausal | 29 | 81% * | 12 (41%) | 26 ± 1.7 (9–38) | 31 ± 1.2 (20–42) | 44 ± 2.5 (20–77) | AMH increased | 22 ± 2.7 ** (9–22) | 28 ± 1.8 ** (20–37) | 49 ± 2.7 (29–64) |
| No increase | 29 ± 2.0 ** (9–39) | 36 ± 1.6 ** (20–37) | 43 ± 3.9 (20–77) | ||||||||
| Non-menopausal | 19 | 41% * | 13 (68%) | 30 ± 1.4 (15–37) | 35 ± 1.3 (26–44) | 56 ± 4.5 (24–100) | AMH increased | 27 ± 1.9 ** (15–37) | 33 ± 1.6 ** (26-41) | 55 ± 5.4 (24-100) | |
| No increase | 33 ± 1.4 ** (26–37) | 39 ± 1.6 ** (31–44) | 59 ± 8.3 (24–96) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hornshøj Greve, V.; Dueholm, M.; Mamsen, L.S.; Kristensen, S.G.; Ernst, E.; Andersen, C.-Y. Hormonal Characteristics of Women Receiving Ovarian Tissue Transplantation with or without Endogenous Ovarian Activity. J. Clin. Med. 2021, 10, 5217. https://doi.org/10.3390/jcm10225217
Hornshøj Greve V, Dueholm M, Mamsen LS, Kristensen SG, Ernst E, Andersen C-Y. Hormonal Characteristics of Women Receiving Ovarian Tissue Transplantation with or without Endogenous Ovarian Activity. Journal of Clinical Medicine. 2021; 10(22):5217. https://doi.org/10.3390/jcm10225217
Chicago/Turabian StyleHornshøj Greve, Vinnie, Margit Dueholm, Linn Salto Mamsen, Stine Gry Kristensen, Erik Ernst, and Claus-Yding Andersen. 2021. "Hormonal Characteristics of Women Receiving Ovarian Tissue Transplantation with or without Endogenous Ovarian Activity" Journal of Clinical Medicine 10, no. 22: 5217. https://doi.org/10.3390/jcm10225217
APA StyleHornshøj Greve, V., Dueholm, M., Mamsen, L. S., Kristensen, S. G., Ernst, E., & Andersen, C.-Y. (2021). Hormonal Characteristics of Women Receiving Ovarian Tissue Transplantation with or without Endogenous Ovarian Activity. Journal of Clinical Medicine, 10(22), 5217. https://doi.org/10.3390/jcm10225217






