Colonic Lipoma Causing Bowel Intussusception: An Up-to-Date Systematic Review
Abstract
:1. Introduction
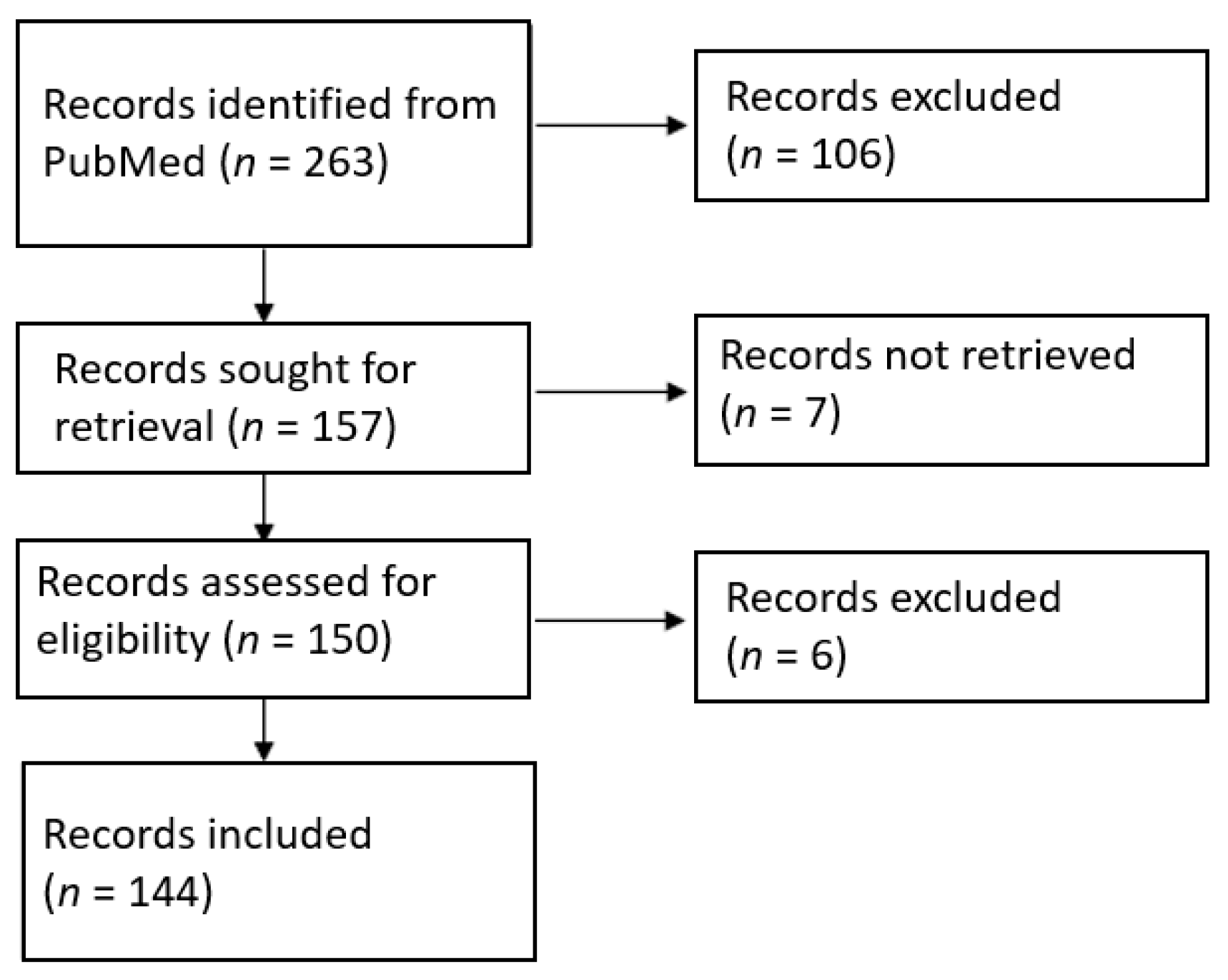
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction and Quality Assessment
2.4. Data Analysis
3. Results
3.1. Demographic Data
3.2. Clinical Presentation and Laboratory
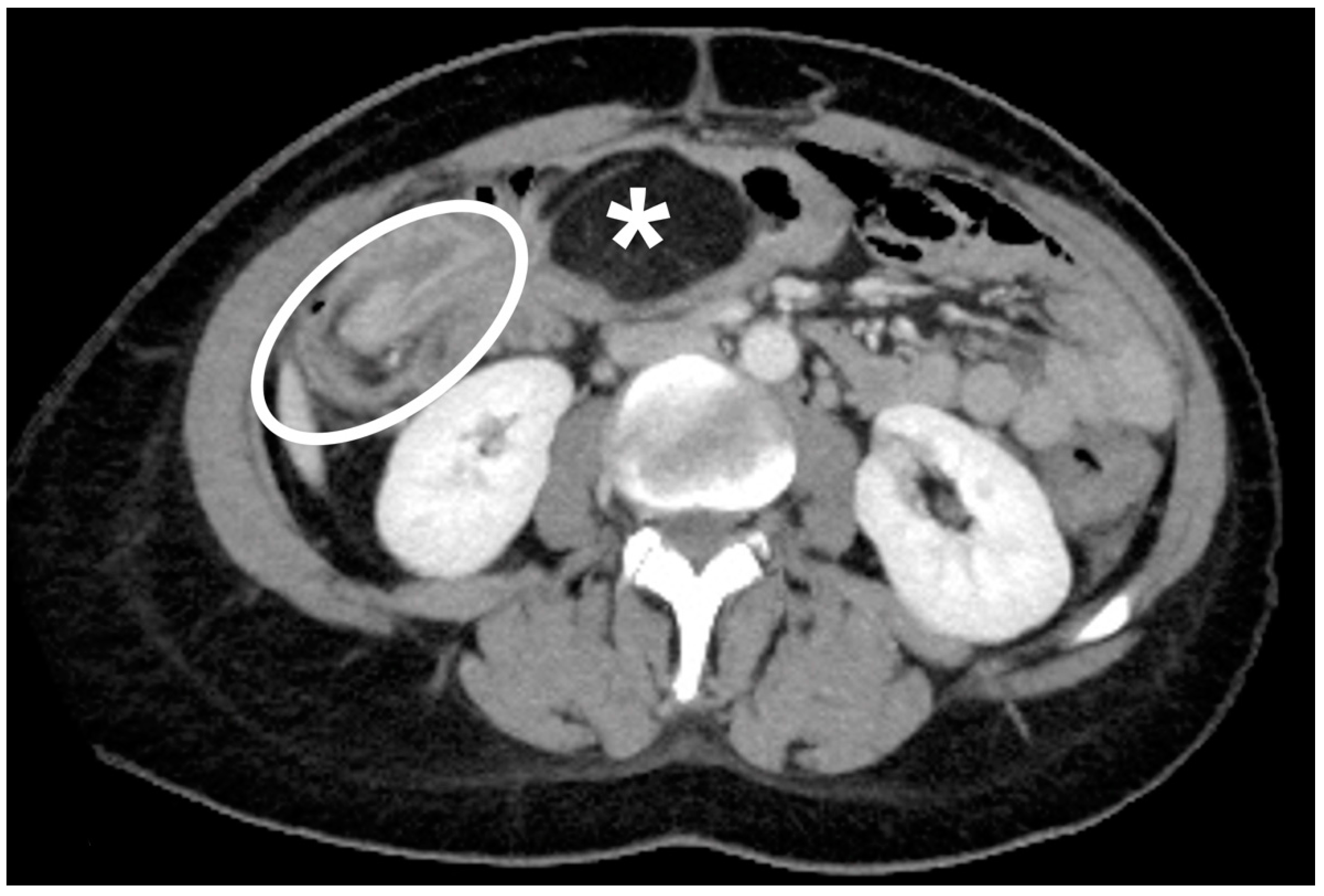
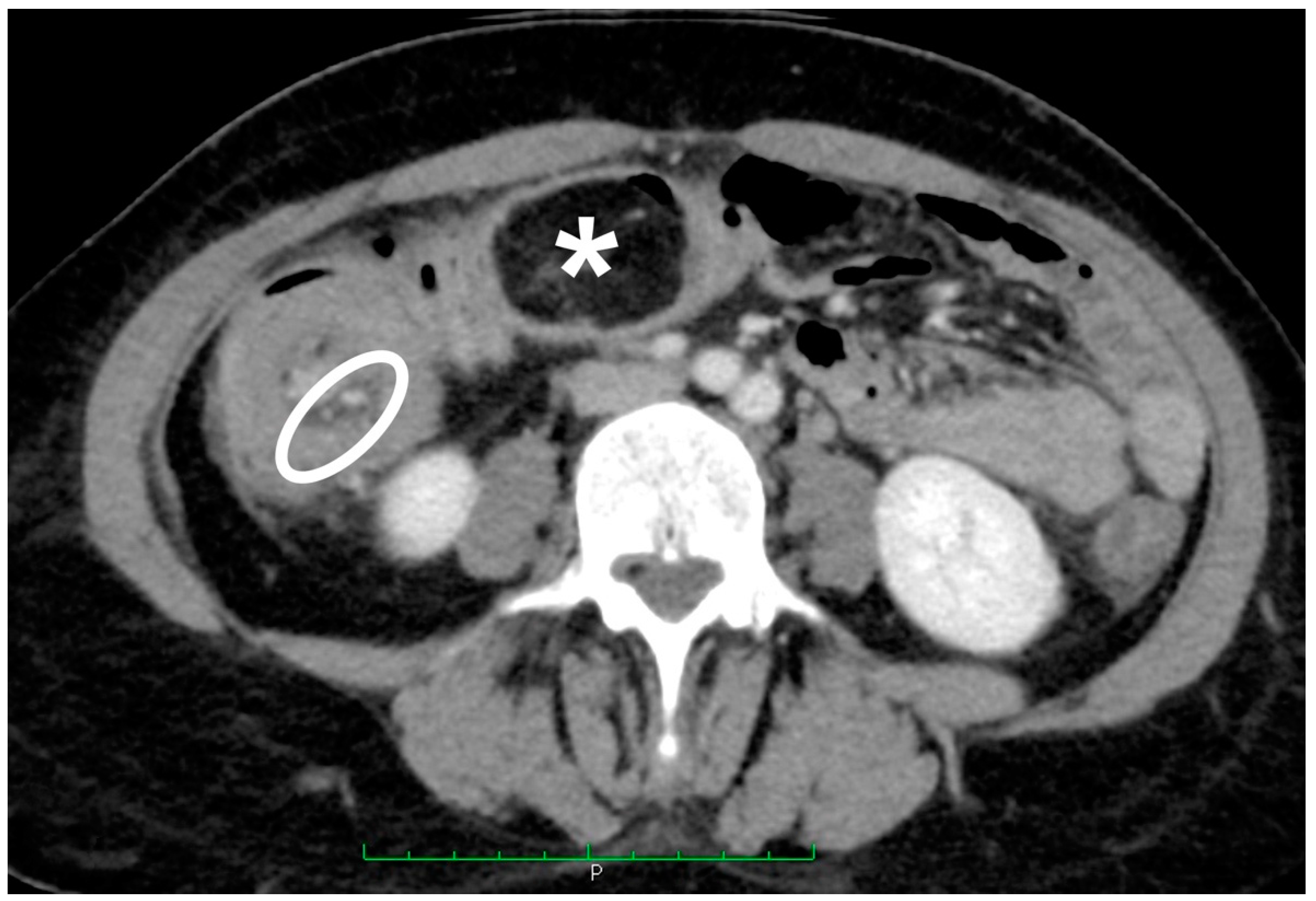
3.3. Instrumental Examinations
3.4. Location and Size of The Lipoma
3.5. Treatment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Panagiotakis, G.I.; Andreou, A.G.; Petrakis, I.E.; Tzardi, M.; Daskalogiannaki, M.; Chalkiadakis, G.E. Laparoscopic resection of a sigmoid colon lipoma in a young female patient: A case report and review of the literature. Oncol. Lett. 2017, 13, 1303–1306. [Google Scholar] [CrossRef] [Green Version]
- Kim, C.Y.; Bandres, D.; Tio, T.L.; Benjamin, S.B.; Al-Kawas, F.H. Endoscopic removal of large colonic lipomas. Gastrointest. Endosc. 2002, 55, 929–931. [Google Scholar] [CrossRef]
- Crocetti, D.; Sapienza, P.; Sterpetti, A.V.; Paliotta, A.; de Gori, A.; Pedullà, G.; de Toma, G. Surgery for symptomatic colon lipoma: A systematic review of the literature. Anticancer Res. 2014, 34, 6271–6276. [Google Scholar] [PubMed]
- Kim, Y.H.; Blake, M.A.; Harisinghani, M.G.; Archer-Arroyo, K.; Hahn, P.F.; Pitman, M.B.; Mueller, P.R. Adult intestinal intussusception: CT appearances and identification of a causative lead point. Radiographics 2006, 26, 733–744. [Google Scholar] [CrossRef]
- Tan, K.Y.; Tan, S.M.; Tan, A.G.; Chen, C.Y.; Chng, H.C.; Hoe, M.N. Adult intussusception: Experience in Singapore. ANZ J. Surg. 2003, 73, 1044–1047. [Google Scholar] [CrossRef]
- Toso, C.; Erne, M.; Lenzlinger, P.M.; Schmid, J.F.; Büchel, H.; Melcher, G.; Morel, P. Intussusception as a cause of bowel obstruction in adults. Swiss. Med. Wkly. 2005, 135, 87–90. [Google Scholar]
- Cochran, A.A.; Higgins, G.L., 3rd; Strout, T.D. Intussusception in traditional pediatric, nontraditional pediatric, and adult patients. Am. J. Emerg. Med. 2011, 29, 523–527. [Google Scholar] [CrossRef]
- Reginelli, A.; Russo, A.; Pinto, A.; Stanzione, F.; Martiniello, C.; Cappabianca, S.; Brunese, L.; Squillaci, E. The role of computed tomography in the preoperative assessment of gastrointestinal causes of acute abdomen in elderly patients. Int. J. Surg. 2014, 12 (Suppl. 2), S181–S186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozogul, B.; Kisaoglu, A.; Ozturk, G.; Atamanalp, S.S.; Yıldırgan, M.İ.; Aköz, A.; Aydinli, B. Adult Intussusception: Clinical Experience from a Single Center. Indian J. Surg. 2015, 77 (Suppl. 2), 490–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomes, A.; Sousa, M.; Pignatelli, N.; Nunes, V. Adult intussusception: A single-center 10-year experience. Eur. Surg. 2013, 45, 239–244. [Google Scholar] [CrossRef]
- Ávila, F.; Pereira, J.R.; Duarte, M.A. Colonic Intussusception Caused by Colonic Lipoma. GE Port. J. Gastroenterol. 2016, 23, 264–266. [Google Scholar] [CrossRef] [Green Version]
- Paškauskas, S.; Latkauskas, T.; Valeikaitė, G.; Paršeliūnas, A.; Svagždys, S.; Saladžinskas, Z.; Tamelis, A.; Pavalkis, D. Colonic intussusception caused by colonic lipoma: A case report. Medicina 2010, 46, 477–481. [Google Scholar] [CrossRef] [Green Version]
- Mnif, L.; Amouri, A.; Masmoudi, M.A.; Mezghanni, A.; Gouiaa, N.; Boudawara, T.; Tahri, N. Giant lipoma of the transverse colon: A case report and review of the literature. Tunis. Med. 2009, 87, 398–402. [Google Scholar] [PubMed]
- Vecchio, R.; Ferrara, M.; Mosca, F.; Ignoto, A.; Latteri, F. Lipomas of the large bowel. Eur. J. Surg. 1996, 162, 915–919. [Google Scholar]
- Bardají, M.; Roset, F.; Camps, R.; Sant, F.; Fernández-Layos, M.J. Symptomatic colonic lipoma: Differential diagnosis of large bowel tumors. Int. J. Colorectal Dis. 1998, 13, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Chiba, T.; Suzuki, S.; Sato, M.; Tsukahara, M.; Saito, S.; Inomata, M.; Orii, S.; Suzuki, K. A case of a lipoma in the colon complicated by intussusception. Eur. J. Gastroenterol. Hepatol. 2002, 14, 701–702. [Google Scholar] [CrossRef]
- Bahadursingh, A.M.; Robbins, P.L.; Longo, W.E. Giant submucosal sigmoid colon lipoma. Am. J. Surg. 2003, 186, 81–82. [Google Scholar] [CrossRef]
- Krasniqi, A.S.; Hamza, A.R.; Salihu, L.M.; Spahija, G.S.; Bicaj, B.X.; Krasniqi, S.A.; Kurshumliu, F.I.; Gashi-Luci, L.H. Compound double ileoileal and ileocecocolic intussusception caused by lipoma of the ileum in an adult patient: A case report. J. Med. Case Rep. 2011, 5, 452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howard, N.; Pranesh, N.; Carter, P. Colo-colonic intusussception secondary to a lipoma. Int. J. Surg. Case Rep. 2012, 3, 52–54. [Google Scholar] [CrossRef] [Green Version]
- Wulff, C.; Jespersen, N. Colo-colonic intussusception caused by lipoma. Case reports. Acta Radiol. 1995, 36, 478–480. [Google Scholar] [CrossRef]
- Karaosmanoglu, D.; Temizoz, O.; Karcaaltincaba, M.; Akata, D. Sonographic findings of colonic lipoma causing intussusception. J. Ultrasound Med. 2007, 26, 1621–1623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, M.M.; Win, T.; Rasheed, S. A Cecal Lipoma Causing Intussusception, Detected on Routine Outpatient Abdominal Ultrasound. J. Med. Ultrasound 2019, 28, 44–47. [Google Scholar] [CrossRef]
- Kuzmich, S.; Harvey, C.J.; Kuzmich, T.; Tan, K.L. Ultrasound detection of colonic polyps: Perspective. Br. J. Radiol. 2012, 85, e1155–e1164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Somma, F.; Faggian, A.; Serra, N.; Gatta, G.; Iacobellis, F.; Berritto, D.; Reginelli, A.; Di Mizio, V.; Cappabianca, S.; Di Mizio, R.; et al. Bowel intussusceptions in adults: The role of imaging. Radiol. Med. 2015, 120, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, C.A.; Seibert, J.J.; Strain, J.D.; Glasier, C.M.; Leithiser, R.E., Jr.; Iqbal, V. Intussusception: Clinical and radiographic factors influencing reducibility. Pediatr. Radiol. 1989, 20, 57–60. [Google Scholar] [CrossRef]
- Byrne, A.T.; Geoghegan, T.; Govender, P.; Lyburn, I.D.; Colhoun, E.; Torreggiani, W.C. The imaging of intussusception. Clin. Radiol. 2005, 60, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Castro, E.B.; Stearns, M.W. Lipoma of the large intestine: A review of 45 cases. Dis. Colon. Rectum. 1972, 15, 441–444. [Google Scholar] [CrossRef]
- Bueto Buetow, P.C.; Buck, J.L.; Carr, N.J.; Pantongrag-Brown, L.; Ros, P.R.; Cruess, D.F. Intussuscepted colonic lipomas: Loss of fat attenuation on CT with pathologic correlation in 10 cases. Abdom. Imaging 1996, 21, 153–156. [Google Scholar] [CrossRef]
- Mouaqit, O.; Hasnai, H.; Chbani, L.; Oussaden, A.; Maazaz, K.; Amarti, A.; Taleb, K.A. Pedunculated lipoma causing colo-colonic intussusception: A rare case report. BMC Surg. 2013, 13, 51. [Google Scholar] [CrossRef]
- Marinis, A.; Yiallourou, A.; Samanides, L.; Dafnios, N.; Anastasopoulos, G.; Vassiliou, I.; Theodosopoulos, T. Intussusception of the bowel in adults: A review. World J. Gastroenterol. 2009, 15, 407–411. [Google Scholar] [CrossRef]
- Nallamothu, G.; Adler, D.G. Large colonic lipomas. Gastroenterol. Hepatol. 2011, 7, 490–492. [Google Scholar]
- Ongom, P.A.; Kijjambu, S.C. Adult intussusception: A continuously unveiling clinical complex illustrating both acute (emergency) and chronic disease management. OA Emerg. Med. 2013, 1, 3. [Google Scholar] [CrossRef]
- Zimmer, V. Naked Fat Sign Is a Characteristic of Colonic Lipoma. Clin. Gastroenterol. Hepatol. 2019, 17, A29. [Google Scholar] [CrossRef]
- Triantopoulou, C.; Vassilaki, A.; Filippou, D.; Velonakis, S.; Dervenis, C.; Koulentianos, E. Adult ileocolic intussusception secondary to a submucosal cecal lipoma. Abdom. Imaging 2004, 29, 426–428. [Google Scholar] [CrossRef]
- Bronswijk, M.; Vandenbroucke, A.M.; Bossuyt, P. Endoscopic treatment of large symptomatic colon lipomas: A systematic review of efficacy and safety. United Eur. Gastroenterol. J. 2020, 8, 1147–1154. [Google Scholar] [CrossRef]
- Ivekovic, H.; Rustemovic, N.; Brkic, T.; Ostojic, R.; Monkemuller, K. Endoscopic ligation (“Loop-And-Let-Go”) is effective treatment for large colonic lipomas: A prospective validation study. BMC Gastroenterol. 2014, 14, 122. [Google Scholar] [CrossRef] [Green Version]
- Meunier, M.; Limgba, A.; Schumacker, I.; Mehdi, A. Intussusception related to transverse colonic lipoma: A case report and review of the literature. Acta Chir. Belg. 2020, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.C.; Chen, Y.Y.; Chen, Y.F.; Lin, C.N.; Yen, H.H.; Lou, H.Y. Adult intussusception in Asians: Clinical presentations, diagnosis, and treatment. J. Gastroenterol. Hepatol. 2007, 22, 1767–1771. [Google Scholar] [CrossRef] [PubMed]



| Symptoms | n. | % |
|---|---|---|
| Abdominal pain - Abdominal pain (intermittent) - Abdominal pain (crampy) | 134/161 39/134 23/134 | 83% 29% 17% |
| Constipation | 29/161 | 18% |
| Rectal blood loss | 26/161 | 16% |
| Vomiting | 23/161 | 14% |
| Diarrhea - Watery diarrhea - Bloody diarrhea | 20/161 3/20 2/20 | 12% 15% 10% |
| Hematochezia | 17/161 | 11% |
| Weight loss | 18/161 | 11% |
| Altered bowel movements | 13/161 | 8% |
| Nausea | 14/161 | 9% |
| Obstruction | 12/161 | 7% |
| Rectal mucus and blood loss | 7/161 | 4% |
| Partial obstruction | 7/161 | 4% |
| Tenesmus | 5/161 | 3% |
| Bloating | 5/161 | 3% |
| Fever | 4/161 | 2% |
| Dyspepsia | 1/161 | 1% |
| Signs | n. | % |
|---|---|---|
| Tenderness | 46/123 | 37% |
| Normal exploration | 29/123 | 24% |
| Distension | 20/123 | 16% |
| Palpable mass | 20/123 | 16% |
| Prolapsing mass through the rectum | 13/123 | 11% |
| Voluntary guarding | 5/123 | 4% |
| Pain | 4/123 | 3% |
| Rectal mass | 3/123 | 2% |
| Rebound tenderness | 3/123 | 2% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menegon Tasselli, F.; Urraro, F.; Sciaudone, G.; Bagaglini, G.; Pagliuca, F.; Reginelli, A.; Ferraraccio, F.; Cappabianca, S.; Selvaggi, F.; Pellino, G. Colonic Lipoma Causing Bowel Intussusception: An Up-to-Date Systematic Review. J. Clin. Med. 2021, 10, 5149. https://doi.org/10.3390/jcm10215149
Menegon Tasselli F, Urraro F, Sciaudone G, Bagaglini G, Pagliuca F, Reginelli A, Ferraraccio F, Cappabianca S, Selvaggi F, Pellino G. Colonic Lipoma Causing Bowel Intussusception: An Up-to-Date Systematic Review. Journal of Clinical Medicine. 2021; 10(21):5149. https://doi.org/10.3390/jcm10215149
Chicago/Turabian StyleMenegon Tasselli, Francesco, Fabrizio Urraro, Guido Sciaudone, Giulia Bagaglini, Francesca Pagliuca, Alfonso Reginelli, Franca Ferraraccio, Salvatore Cappabianca, Francesco Selvaggi, and Gianluca Pellino. 2021. "Colonic Lipoma Causing Bowel Intussusception: An Up-to-Date Systematic Review" Journal of Clinical Medicine 10, no. 21: 5149. https://doi.org/10.3390/jcm10215149
APA StyleMenegon Tasselli, F., Urraro, F., Sciaudone, G., Bagaglini, G., Pagliuca, F., Reginelli, A., Ferraraccio, F., Cappabianca, S., Selvaggi, F., & Pellino, G. (2021). Colonic Lipoma Causing Bowel Intussusception: An Up-to-Date Systematic Review. Journal of Clinical Medicine, 10(21), 5149. https://doi.org/10.3390/jcm10215149







