Risk Factors for Spine Reoperation and Joint Replacement Surgeries after Short-Segment Lumbar Spinal Surgeries for Lumbar Degenerative Disc Disease: A Population-Based Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
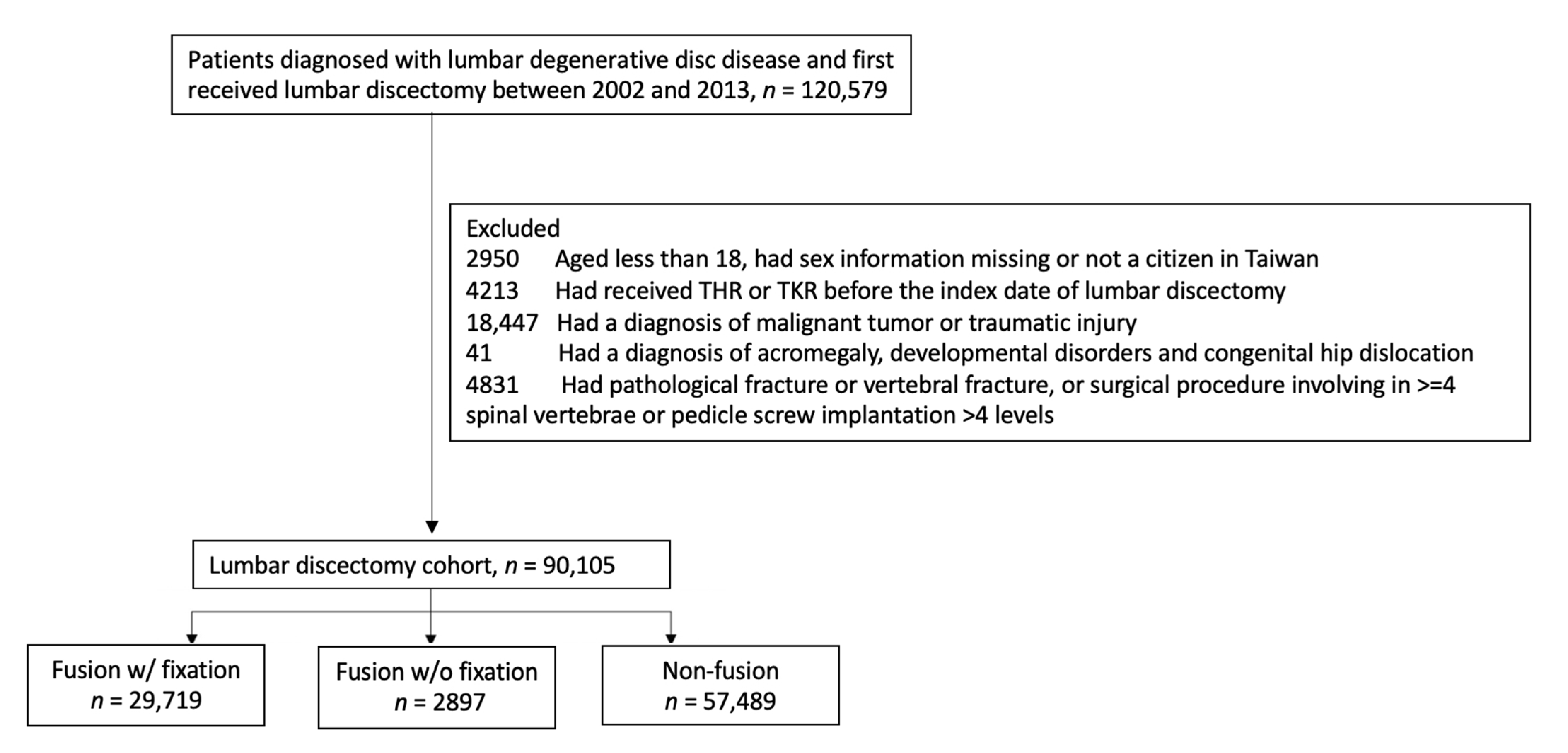
2.2. Study Samples
2.3. Study Outcomes
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Incidence of Spine Reoperation and Joint Replacement
3.3. Risk Factors Associated with 1-Year Spine Reoperation
3.4. Risk Factors Associated with 1-Year THR or TKR
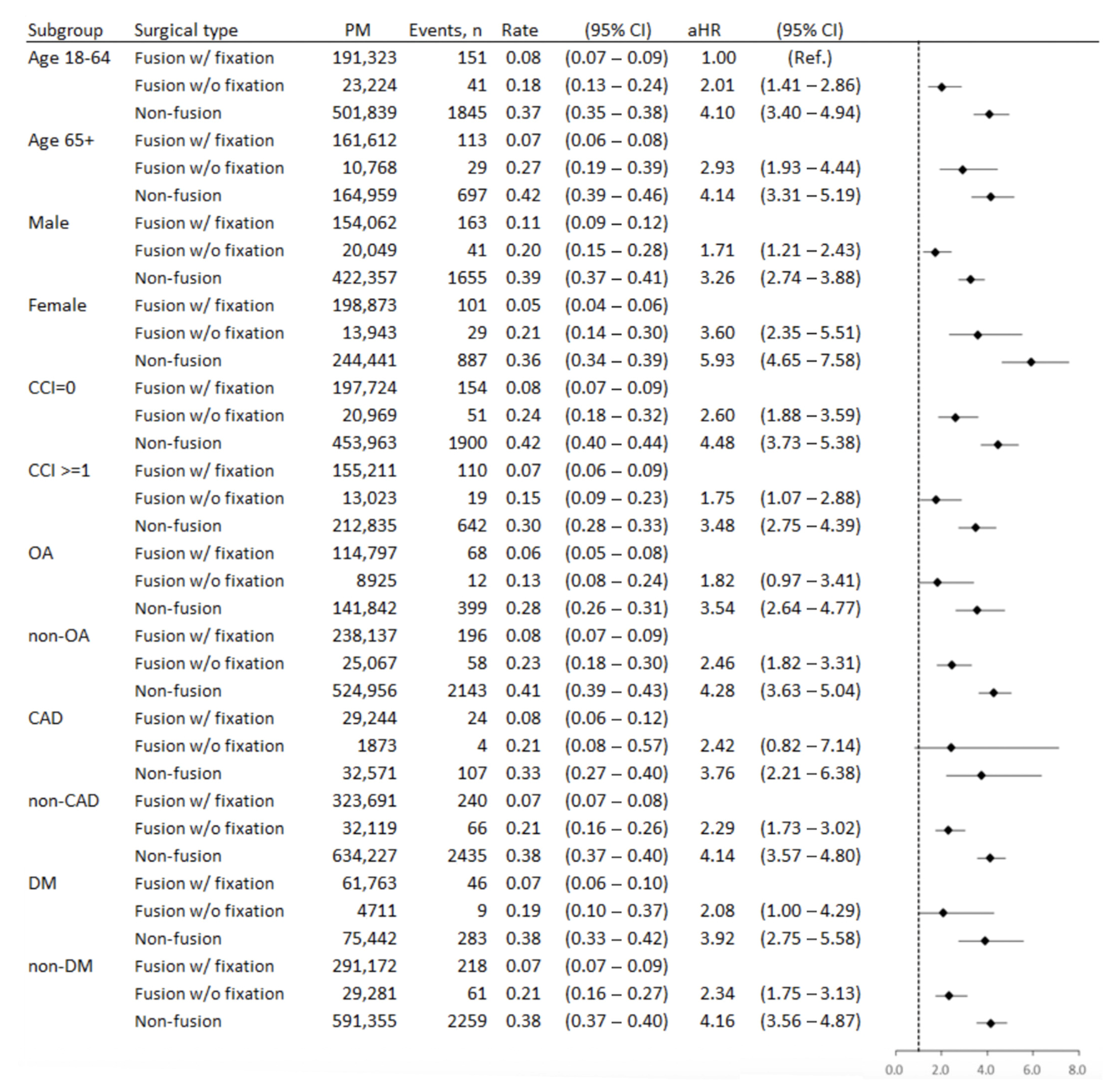
3.5. Subgroup Analysis
4. Discussion
4.1. Surgical Type and the Risk of Spine Reoperation after Lumbar Discectomy Surgery
4.2. Patient’s Factors on the Risk of Spine Reoperation after Lumbar Discectomy Surgery
4.3. Joint Replacement Surgeries after Lumbar Discectomy Surgery
4.4. Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Donnally, I.C.; Varacallo, M. Lumbar Degenerative Disk Disease; StatPearls: Treasure Island, FL, USA, 2018. [Google Scholar]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef]
- Parvizi, J.; Pour, A.E.; Hillibrand, A.; Goldberg, G.; Sharkey, P.F.; Rothman, R.H. Back pain and total hip arthroplasty: A prospective natural history study. Clin. Orthop. Relat. Res. 2010, 468, 1325–1330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsuji, T.; Matsuyama, Y.; Goto, M.; Yimin, Y.; Sato, K.; Hasegawa, Y.; Ishiguro, N. Knee-spine syndrome: Correlation between sacral inclination and patellofemoral joint pain. J. Orthop. Sci. 2002, 7, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.P.; McManus, A.C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine 1994, 19, 1611–1618. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.D.; Smith, T.R.; Lim, S.; Cybulski, G.R.; Kim, J.Y. Predictors of unplanned readmission in patients undergoing lumbar decompression: Multi-institutional analysis of 7016 patients. J. Neurosurg. Spine 2014, 20, 606–616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akins, P.T.; Harris, J.; Alvarez, J.L.; Chen, Y.; Paxton, E.W.; Bernbeck, J.; Guppy, K.H. Risk Factors Associated With 30-day Readmissions After Instrumented Spine Surgery in 14,939 Patients: 30-day readmissions after instrumented spine surgery. Spine 2015, 40, 1022–1032. [Google Scholar] [CrossRef] [PubMed]
- Vorhies, J.S.; Hernandez-Boussard, T.; Alamin, T. Treatment of Degenerative Lumbar Spondylolisthesis With Fusion or Decompression Alone Results in Similar Rates of Reoperation at 5 Years. Clin. Spine Surg. 2018, 31, E74–E79. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.I.; Mirza, S.K.; Flum, D.R.; Wickizer, T.M.; Heagerty, P.J.; Lenkoski, A.F.; Deyo, R.A. Repeat surgery after lumbar decompression for herniated disc: The quality implications of hospital and surgeon variation. Spine J. 2012, 12, 89–97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Irmola, T.M.; Hakkinen, A.; Jarvenpaa, S.; Marttinen, I.; Vihtonen, K.; Neva, M. Reoperation Rates Following Instrumented Lumbar Spine Fusion. Spine 2018, 43, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Gerling, M.C.; Leven, D.; Passias, P.G.; Lafage, V.; Bianco, K.; Lee, A.; Morgan, T.S.; Lurie, J.D.; Tosteson, T.D.; Zhao, W.; et al. Risk Factors for Reoperation in Patients Treated Surgically for Degenerative Spondylolisthesis: A Subanalysis of the 8-year Data From the SPORT Trial. Spine 2017, 42, 1559–1569. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.I.; Mirza, S.K.; Comstock, B.A.; Gray, D.T.; Kreuter, W.; Deyo, R.A. Are lumbar spine reoperation rates falling with greater use of fusion surgery and new surgical technology? Spine 2007, 32, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Malter, A.D.; McNeney, B.; Loeser, J.D.; Deyo, R.A. 5-year reoperation rates after different types of lumbar spine surgery. Spine 1998, 23, 814–820. [Google Scholar] [CrossRef] [PubMed]
- Park, M.S.; Ju, Y.S.; Moon, S.H.; Kim, T.H.; Oh, J.K.; Sung, P.S.; Kim, C.H.; Chung, C.K.; Chang, H.G. Reoperation rates after posterior lumbar spinal fusion surgery according to preoperative diagnoses: A national population-based cohort study. Clin. Neurol. Neurosurg. 2019, 184, 105408. [Google Scholar] [CrossRef] [PubMed]
- Piper, K.; DeAndrea-Lazarus, I.; Algattas, H.; Kimmell, K.T.; Towner, J.; Li, Y.M.; Walter, K.; Vates, G.E. Risk Factors Associated with Readmission and Reoperation in Patients Undergoing Spine Surgery. World Neurosurg. 2018, 110, e627–e635. [Google Scholar] [CrossRef] [PubMed]
- Lesher, J.M.; Dreyfuss, P.; Hager, N.; Kaplan, M.; Furman, M. Hip joint pain referral patterns: A descriptive study. Pain Med. 2008, 9, 22–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Redmond, J.M.; Gupta, A.; Hammarstedt, J.E.; Stake, C.E.; Domb, B.G. The hip-spine syndrome: How does back pain impact the indications and outcomes of hip arthroscopy? Arthroscopy 2014, 30, 872–881. [Google Scholar] [CrossRef] [PubMed]

| Overall | Fusion with Fixation | Fusion without Fixation | Non-Fusion | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | N | (%) | P | |
| Sample size | 90,105 | 29,719 | 2897 | 57,489 | |||||
| Primary disease diagnosis | <0.001 | ||||||||
| Spondylolisthesis | 13,586 | (15.1) | 12,475 | (42.0) | 197 | (6.8) | 914 | (1.6) | |
| Disc herniation | 57,792 | (64.1) | 9738 | (32.8) | 1800 | (62.1) | 46,254 | (80.5) | |
| Others | 18,727 | (20.8) | 7506 | (25.3) | 900 | (31.1) | 10,321 | (18.0) | |
| Male, yes | 51,205 | (56.8) | 13,028 | (43.8) | 1711 | (59.1) | 36,466 | (63.4) | <0.001 |
| Age group (y) | <0.001 | ||||||||
| 18–44 | 29,640 | (32.9) | 5074 | (17.1) | 986 | (34.0) | 23,580 | (41.0) | |
| 45–64 | 31,487 | (34.9) | 10,986 | (37.0) | 974 | (33.6) | 19,527 | (34.0) | |
| 65+ | 28,978 | (32.2) | 13,659 | (46.0) | 937 | (32.3) | 14,382 | (25.0) | |
| Comorbidities, yes | |||||||||
| Rheumatoid arthritis | 1134 | (1.3) | 495 | (1.7) | 43 | (1.5) | 596 | (1.0) | <0.001 |
| Ankylosing spondylitis | 2351 | (2.6) | 527 | (1.8) | 86 | (3.0) | 1738 | (3.0) | <0.001 |
| Osteoarthritis | 22,484 | (25.0) | 9641 | (32.4) | 754 | (26.0) | 12,089 | (21.0) | <0.001 |
| Osteoporosis | 3683 | (4.1) | 1824 | (6.1) | 120 | (4.1) | 1739 | (3.0) | <0.001 |
| Diabetic mellitus | 12,105 | (13.4) | 5208 | (17.5) | 405 | (14.0) | 6492 | (11.3) | <0.001 |
| COPD | 2983 | (3.3) | 1209 | (4.1) | 88 | (3.0) | 1686 | (2.9) | <0.001 |
| Hypertension | 20,776 | (23.1) | 9166 | (30.8) | 681 | (23.5) | 10,929 | (19.0) | <0.001 |
| Coronary artery disease | 5424 | (6.0) | 2471 | (8.3) | 162 | (5.6) | 2791 | (4.9) | <0.001 |
| Mechanical insults to the joint from acute injury or repeated loading | 18,473 | (20.5) | 5922 | (19.9) | 572 | (19.7) | 11,979 | (20.8) | 0.004 |
| CCI | <0.001 | ||||||||
| 0 | 57,739 | (64.1) | 16,647 | (56.0) | 1790 | (61.8) | 39,302 | (68.4) | |
| 1–2 | 26,428 | (29.3) | 10,479 | (35.3) | 889 | (30.7) | 15,060 | (26.2) | |
| 3+ | 5938 | (6.6) | 2593 | (8.7) | 218 | (7.5) | 3127 | (5.4) | |
| Urbanization | <0.001 | ||||||||
| 1 (highest) | 51,519 | (57.2) | 15,827 | (53.3) | 1700 | (58.7) | 33,992 | (59.1) | |
| 2 | 31,255 | (34.7) | 11,043 | (37.2) | 950 | (32.8) | 19,262 | (33.5) | |
| 3 | 7331 | (8.1) | 2849 | (9.6) | 247 | (8.5) | 4235 | (7.4) | |
| Social economic status | <0.001 | ||||||||
| 1 (highest) | 3648 | (4.0) | 1185 | (4.0) | 111 | (3.8) | 2352 | (4.1) | |
| 2 | 8376 | (9.3) | 2887 | (9.7) | 279 | (9.6) | 5210 | (9.1) | |
| 3 | 38,983 | (43.3) | 12,410 | (41.8) | 1232 | (42.5) | 25,341 | (44.1) | |
| 4 | 31,281 | (34.7) | 10,967 | (36.9) | 990 | (34.2) | 19,324 | (33.6) | |
| 5 | 7139 | (7.9) | 2070 | (7.0) | 261 | (9.0) | 4808 | (8.4) | |
| 6 | 678 | (0.8) | 200 | (0.7) | 24 | (0.8) | 454 | (0.8) | |
| Medication use six months before the index date | |||||||||
| Injection steroid use | 13,653 | (15.2) | 3703 | (12.5) | 533 | (18.4) | 9417 | (16.4) | <0.001 |
| Oral steroid use | 32,142 | (35.7) | 12,075 | (40.6) | 1101 | (38.0) | 18,966 | (33.0) | <0.001 |
| NSAID | 63,025 | (69.9) | 21,024 | (70.7) | 2051 | (70.8) | 39,950 | (69.5) | <0.001 |
| Outcomes | Group | People per Month | Events, n | Rate | (95% CI) | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | (95% CI) | P | aHR | (95% CI) | P | ||||||
| Spine reoperation | Overall | 1,053,724 | 2876 | 0.27 | (0.26–0.28) | ||||||
| Fusion with fixation | 352,934 | 264 | 0.07 | (0.07–0.08) | 1.00 | (Ref.) | 1.00 | (Ref.) | |||
| Fusion without fixation | 33,992 | 70 | 0.21 | (0.16–0.26) | 2.74 | (2.11–3.57) | <0.001 | 2.30 | (1.76–3.02) | <0.001 | |
| Non-fusion | 666,798 | 2542 | 0.38 | (0.37–0.40) | 5.07 | (4.47–5.76) | <0.001 | 4.12 | (3.57–4.76) | <0.001 | |
| THR | Overall | 1,073,150 | 435 | 0.04 | (0.04–0.04) | ||||||
| Fusion with fixation | 353,568 | 186 | 0.05 | (0.05–0.06) | 1.00 | (Ref.) | 1.00 | (Ref.) | |||
| Fusion without fixation | 34,394 | 15 | 0.04 | (0.03–0.07) | 0.83 | (0.49–1.40) | 0.485 | 0.98 | (0.57–1.67) | 0.939 | |
| Non-fusion | 685,188 | 234 | 0.03 | (0.03–0.04) | 0.65 | (0.54–0.79) | <0.001 | 0.90 | (0.71–1.14) | 0.379 | |
| TKR | Overall | 1,073,207 | 463 | 0.04 | (0.04–0.05) | ||||||
| Fusion with fixation | 353,423 | 222 | 0.06 | (0.06–0.07) | 1.00 | (Ref.) | 1.00 | (Ref.) | |||
| Fusion without fixation | 34,401 | 14 | 0.04 | (0.02–0.07) | 0.65 | (0.38–1.11) | 0.115 | 1.01 | (0.58–1.75) | 0.971 | |
| Non-fusion | 685,383 | 227 | 0.03 | (0.03–0.04) | 0.53 | (0.44–0.63) | <0.001 | 1.13 | (0.90–1.41) | 0.300 | |
| Variables | aHR | (95% CI) | P |
|---|---|---|---|
| Surgical type (Ref. = fusion with fixation) | 1.00 | (Ref.) | |
| Fusion without fixation | 2.30 | (1.76–3.02) | <0.001 |
| Non-fusion | 4.12 | (3.57–4.76) | <0.001 |
| Disease dx (Ref. = spondylolisthesis) | 1.00 | (Ref.) | |
| Disc herniation | 1.80 | (1.44–2.24) | <0.001 |
| Others | 1.59 | (1.27–1.99) | <0.001 |
| Age group (Ref. = 18–44) | 1.00 | (Ref.) | |
| 45–64 | 1.68 | (1.54–1.85) | <0.001 |
| 65+ | 1.99 | (1.79–2.22) | <0.001 |
| Sex (Ref. = male) | 1.00 | (Ref.) | |
| Female | 0.88 | (0.81–0.95) | 0.001 |
| Comorbidities, yes | |||
| Rheumatoid arthritis | 0.99 | (0.66–1.49) | 0.961 |
| Ankylosing spondylitis | 0.84 | (0.66–1.08) | 0.172 |
| Osteoarthritis | 0.70 | (0.64–0.78) | <0.001 |
| Osteoporosis | 0.64 | (0.49–0.83) | 0.001 |
| Diabetic mellitus | 1.27 | (1.09–1.48) | 0.003 |
| COPD | 0.78 | (0.60–1.02) | 0.075 |
| Hypertension | 0.70 | (0.63–0.79) | <0.001 |
| Coronary artery disease | 0.98 | (0.82–1.17) | 0.811 |
| Mechanical insults to the joint from acute injury or repeated loading | 0.63 | (0.57–0.70) | <0.001 |
| CCI (Ref. = CCI = 0) | 1.00 | (Ref.) | |
| 1–2 | 0.66 | (0.59–0.73) | <0.001 |
| 3+ | 0.79 | (0.64–0.97) | 0.024 |
| Urbanization (Ref. = 1) | 1.00 | (Ref.) | |
| 2 | 0.95 | (0.88–1.04) | 0.273 |
| 3 | 0.98 | (0.85–1.14) | 0.836 |
| SES (Ref. = 1) | 1.00 | (Ref.) | |
| 2 | 1.09 | (0.881.36) | 0.423 |
| 3 | 1.15 | (0.95–1.40) | 0.142 |
| 4 | 1.04 | (0.85–1.27) | 0.685 |
| 5 | 1.11 | (0.88–1.39) | 0.374 |
| 6 | 2.47 | (1.76–3.47) | <0.001 |
| Medication use six months before the index date, yes | |||
| Systemic steroid use | 1.39 | (1.27–1.52) | <0.001 |
| Oral steroid use | 1.08 | (0.99–1.17) | 0.066 |
| NSAID | 0.99 | (0.91–1.08) | 0.855 |
| THR | TKR | |||||
|---|---|---|---|---|---|---|
| Variables | aHR | (95% CI) | P | aHR | (95% CI) | P |
| Surgical type (Ref. = fusion with fixation) | ||||||
| Fusion without fixation | 0.98 | (0.57–1.67) | 0.939 | 1.01 | (0.58–1.75) | 0.971 |
| Non-fusion | 0.90 | (0.71–1.14) | 0.379 | 1.13 | (0.90–1.41) | 0.300 |
| Disease dx (Ref. = fpondylolisthesis) | ||||||
| Disc herniation | 0.89 | (0.66–1.20) | 0.462 | 0.65 | (0.49–0.86) | 0.002 |
| Others | 1.17 | (0.87–1.56) | 0.305 | 1.09 | (0.85–1.42) | 0.492 |
| Age group (Ref. = 18–44) | ||||||
| 45–64 | 2.88 | (2.06–4.04) | <0.001 | 4.70 | (2.80–7.87) | <0.001 |
| 65+ | 5.21 | (3.69–7.35) | <0.001 | 11.5 | (6.91–19.18) | <0.001 |
| Sex (Ref. = male) | ||||||
| Female | 1.02 | (0.84–1.25) | 0.808 | 2.19 | (1.78–2.70) | <0.001 |
| Comorbidities, yes | ||||||
| Rheumatoid arthritis | 0.78 | (0.35–1.78) | 0.562 | 1.93 | (1.17–3.18) | 0.010 |
| Ankylosing spondylitis | 0.89 | (0.47–1.67) | 0.715 | 0.89 | (0.47–1.67) | 0.711 |
| Osteoarthritis | 1.09 | (0.89–1.35) | 0.411 | 2.36 | (1.94–2.88) | 0.000 |
| Osteoporosis | 1.79 | (1.31–2.46) | <0.001 | 0.91 | (0.66–1.26) | 0.576 |
| Diabetic mellitus | 0.66 | (0.46–0.95) | 0.024 | 1.33 | (1.00–1.78) | 0.051 |
| COPD | 1.24 | (0.79–1.95) | 0.350 | 1.10 | (0.71–1.70) | 0.674 |
| Hypertension | 0.82 | (0.65–1.03) | 0.081 | 0.84 | (0.68–1.03) | 0.093 |
| Coronary artery disease | 0.56 | (0.36–0.87) | 0.010 | 1.13 | (0.84–1.51) | 0.421 |
| Mechanical insults to the joint from acute injury or repeated loading | 1.08 | (0.86–1.36) | 0.490 | 0.98 | (0.78–1.22) | 0.848 |
| CCI (Ref. = CCI = 0) | ||||||
| 1–2 | 0.76 | (0.59–0.97) | 0.026 | 0.62 | (0.49–0.80) | <0.001 |
| 3+ | 0.88 | (0.57–1.38) | 0.592 | 0.64 | (0.43–0.95) | 0.026 |
| Urbanization (Ref. = 1) | ||||||
| 2 | 0.93 | (0.75–1.16) | 0.538 | 1.14 | (0.92–1.41) | 0.233 |
| 3 | 1.48 | (1.09–2.01) | 0.013 | 1.38 | (1.01–1.88) | 0.043 |
| SES (Ref. = 1) | ||||||
| 2 | 1.15 | (0.62–2.13) | 0.666 | 1.38 | (0.72–2.64) | 0.326 |
| 3 | 1.30 | (0.75–2.23) | 0.352 | 1.49 | (0.83–2.68) | 0.181 |
| 4 | 1.36 | (0.78–2.37) | 0.278 | 1.53 | (0.84–2.77) | 0.161 |
| 5 | 1.07 | (0.54–2.10) | 0.856 | 1.46 | (0.73–2.93) | 0.284 |
| 6 | 3.22 | (1.34–7.73) | 0.009 | 2.01 | (0.64–6.26) | 0.230 |
| Medication use six months before the index date | ||||||
| Systemic steroid use | 1.38 | (1.09–1.75) | 0.007 | 1.22 | (0.96–1.55) | 0.106 |
| Oral steroid use | 1.16 | (0.95–1.41) | 0.144 | 1.08 | (0.89–1.30) | 0.451 |
| NSAID | 1.59 | (1.23–2.05) | <0.001 | 1.43 | (1.10–1.86) | 0.008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, M.-H.; Wu, C.; Lin, J.-H.; Chen, L.-Y.; Lee, C.-Y.; Huang, T.-J.; Hsieh, Y.-C.; Chien, L.-N. Risk Factors for Spine Reoperation and Joint Replacement Surgeries after Short-Segment Lumbar Spinal Surgeries for Lumbar Degenerative Disc Disease: A Population-Based Cohort Study. J. Clin. Med. 2021, 10, 5138. https://doi.org/10.3390/jcm10215138
Wu M-H, Wu C, Lin J-H, Chen L-Y, Lee C-Y, Huang T-J, Hsieh Y-C, Chien L-N. Risk Factors for Spine Reoperation and Joint Replacement Surgeries after Short-Segment Lumbar Spinal Surgeries for Lumbar Degenerative Disc Disease: A Population-Based Cohort Study. Journal of Clinical Medicine. 2021; 10(21):5138. https://doi.org/10.3390/jcm10215138
Chicago/Turabian StyleWu, Meng-Huang, Christopher Wu, Jiann-Her Lin, Li-Ying Chen, Ching-Yu Lee, Tsung-Jen Huang, Yi-Chen Hsieh, and Li-Nien Chien. 2021. "Risk Factors for Spine Reoperation and Joint Replacement Surgeries after Short-Segment Lumbar Spinal Surgeries for Lumbar Degenerative Disc Disease: A Population-Based Cohort Study" Journal of Clinical Medicine 10, no. 21: 5138. https://doi.org/10.3390/jcm10215138
APA StyleWu, M.-H., Wu, C., Lin, J.-H., Chen, L.-Y., Lee, C.-Y., Huang, T.-J., Hsieh, Y.-C., & Chien, L.-N. (2021). Risk Factors for Spine Reoperation and Joint Replacement Surgeries after Short-Segment Lumbar Spinal Surgeries for Lumbar Degenerative Disc Disease: A Population-Based Cohort Study. Journal of Clinical Medicine, 10(21), 5138. https://doi.org/10.3390/jcm10215138