Effect of Neuromuscular Blockade on Intraoperative Respiratory Mechanics and Surgical Space Conditions during Robot-Assisted Radical Prostatectomy: A Prospective Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
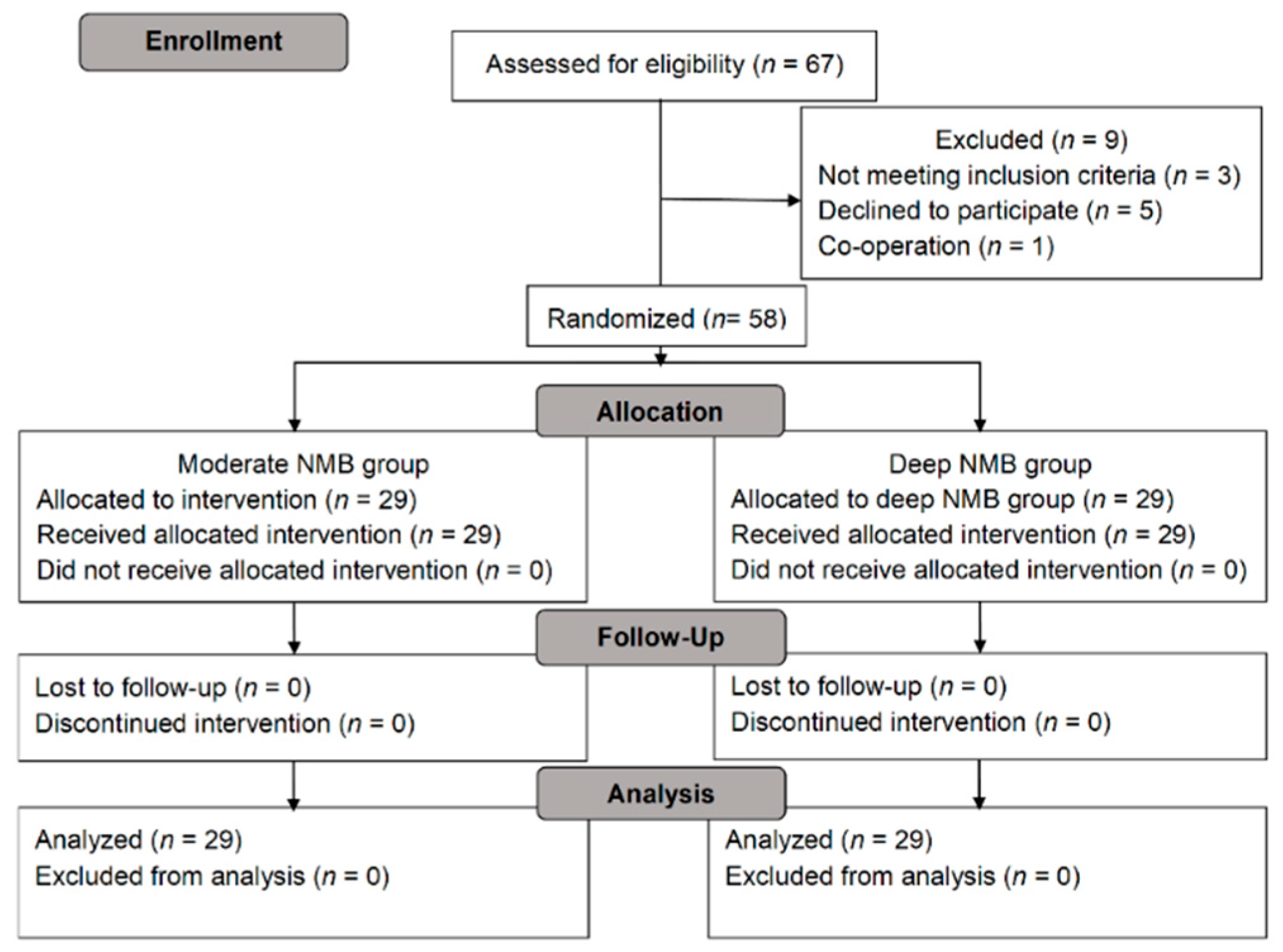
2.1. Study Design
2.2. Participants
2.3. Randomization and Intervention
2.4. Randomization and Intervention
2.5. Surgery
2.6. Measurements
2.7. Sample Size Calculation
2.8. Statistical Analysis
3. Results
3.1. Respiratory Mechanics
3.2. Endoscopic Surgical Conditions and Surgical Difficulty
3.3. Recovery Profiles
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Meininger, D.; Byhahn, C.; Bueck, M.; Binder, J.; Kramer, W.; Kessler, P.; Westphal, K. Effects of prolonged pneumoperitoneum on hemodynamics and acid-base balance during totally endoscopic robot-assisted radical prostatectomies. World J. Surg. 2002, 26, 1423–1427. [Google Scholar] [CrossRef]
- Hirvonen, E.A.; Nuutinen, L.S.; Kauko, M. Ventilatory effects, blood gas changes, and oxygen consumption during laparoscopic hysterectomy. Anesth. Analg. 1995, 80, 961–966. [Google Scholar]
- Safran, D.B.; Orlando, R., 3rd. Physiologic effects of pneumoperitoneum. Am. J. Surg. 1994, 167, 281–286. [Google Scholar] [CrossRef]
- Key Statistics for Prostate Cancer. Available online: https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html (accessed on 5 March 2021).
- Lee, D.K.; Kim, Y.H.; Kim, J.H. Postoperative care of geriatric patients. J. Korean Med. Assoc. 2017, 60, 384–390. [Google Scholar] [CrossRef] [Green Version]
- De Carlo, F.; Celestino, F.; Verri, C.; Masedu, F.; Liberati, E.; Di Stasi, S.M. Retropubic, laparoscopic, and robot-assisted radical prostatectomy: Surgical, oncological, and functional outcomes: A systematic review. Urol. Int. 2014, 93, 373–383. [Google Scholar] [CrossRef] [Green Version]
- Koo, B.W.; Oh, A.Y.; Seo, K.S.; Han, J.W.; Han, H.S.; Yoon, Y.S. Randomized Clinical Trial of Moderate Versus Deep Neuromuscular Block for Low-Pressure Pneumoperitoneum During Laparoscopic Cholecystectomy. World J. Surg. 2016, 40, 2898–2903. [Google Scholar] [CrossRef]
- Martini, C.H.; Boon, M.; Bevers, R.F.; Aarts, L.P.; Dahan, A. Evaluation of surgical conditions during laparoscopic surgery in patients with moderate vs deep neuromuscular block. Br. J. Anaesth. 2014, 112, 498–505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, M.; Sujirattanawimol, N.; Danielson, D.R.; Hall, B.A.; Schroeder, D.R.; Warner, D.O. Requirements for muscle relaxants during radical retropubic prostatectomy. Anesthesiology 2000, 93, 1392–1397. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.J.; Jung, J.W.; Lee, S.; Lee, S.W.; Kim, J.H.; Hong, S.K.; Byun, S.S.; Lee, S.E.; Jeong, S.J. Contemporary trends in radical prostatectomy and predictors of recovery of urinary continence in men aged over 70 years: Comparisons between cohorts aged over 70 and less than 70 years. Asian J. Androl. 2020, 22, 280–286. [Google Scholar] [PubMed]
- Choi, E.S.; Oh, A.Y.; In, C.B.; Ryu, J.H.; Jeon, Y.T.; Kim, H.G. Effects of recruitment manoeuvre on perioperative pulmonary complications in patients undergoing robotic assisted radical prostatectomy: A randomised single-blinded trial. PLoS ONE 2017, 12, e0183311. [Google Scholar] [CrossRef] [PubMed]
- Brandão, J.C.; Lessa, M.A.; Motta-Ribeiro, G.; Hashimoto, S.; Paula, L.F.; Torsani, V.; Le, L.; Bao, X.; Eikermann, M.; Dahl, D.M.; et al. Global and Regional Respiratory Mechanics During Robotic-Assisted Laparoscopic Surgery: A Randomized Study. Anesth. Analg. 2019, 129, 1564–1573. [Google Scholar] [CrossRef] [PubMed]
- Chassard, D.; Berrada, K.; Tournadre, J.; Boulétreau, P. The effects of neuromuscular block on peak airway pressure and abdominal elastance during pneumoperitoneum. Anesth. Analg. 1996, 82, 525–527. [Google Scholar]
- Dubois, P.E.; Putz, L.; Jamart, J.; Marotta, M.L.; Gourdin, M.; Donnez, O. Deep neuromuscular block improves surgical conditions during laparoscopic hysterectomy: A randomised controlled trial. Eur. J. Anesthesiol. 2014, 31, 430–436. [Google Scholar] [CrossRef] [Green Version]
- Bruintjes, M.H.; van Helden, E.V.; Braat, A.E.; Dahan, A.; Scheffer, G.J.; van Laarhoven, C.J.; Warlé, M.C. Deep neuromuscular block to optimize surgical space conditions during laparoscopic surgery: A systematic review and meta-analysis. Br. J. Anaesth. 2017, 118, 834–842. [Google Scholar] [CrossRef] [Green Version]
- Yoo, Y.C.; Kim, N.Y.; Shin, S.; Choi, Y.D.; Hong, J.H.; Kim, C.Y.; Park, H.; Bai, S.J. The Intraocular Pressure under Deep versus Moderate Neuromuscular Blockade during Low-Pressure Robot Assisted Laparoscopic Radical Prostatectomy in a Randomized Trial. PLoS ONE 2015, 10, e0135412. [Google Scholar] [CrossRef]
- Zhu, S.J.; Zhang, X.L.; Xie, Q.; Zhou, Y.F.; Wang, K.R. Comparison of the effects of deep and moderate neuromuscular block on respiratory system compliance and surgical space conditions during robot-assisted laparoscopic radical prostatectomy: A randomized clinical study. J. Zhejiang Univ. Sci. B 2020, 21, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Koo, C.H.; Chung, S.H.; Kim, B.G.; Min, B.H.; Lee, S.C.; Oh, A.Y.; Jeon, Y.T.; Ryu, J.H. Comparison between the effects of deep and moderate neuromuscular blockade during transurethral resection of bladder tumor on endoscopic surgical condition and recovery profile: A prospective, randomized, and controlled trial. World J. Urol. 2019, 37, 359–365. [Google Scholar] [CrossRef]
- Raval, A.D.; Deshpande, S.; Rabar, S.; Koufopoulou, M.; Neupane, B.; Iheanacho, I.; Bash, L.D.; Horrow, J.; Fuchs-Buder, T. Does deep neuromuscular blockade during laparoscopy procedures change patient, surgical, and healthcare resource outcomes? A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2020, 15, e0231452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kyle, E.B.; Maheux-Lacroix, S.; Boutin, A.; Laberge, P.Y.; Lemyre, M. Low vs. Standard Pressures in Gynecologic Laparoscopy: A Systematic Review. Jsls 2016, 20, e2015.00113. [Google Scholar] [CrossRef] [Green Version]
- Gainsburg, D.M. Anesthetic concerns for robotic-assisted laparoscopic radical prostatectomy. Minerva Anestesiol. 2012, 78, 596–604. [Google Scholar] [PubMed]
- Veelo, D.P.; Gisbertz, S.S.; Binnekade, J.M.; Hannivoort, R.A.; Bosman, J.A.; Geerts, B.F.; Blobner, M.; van Berge Henegouwen, M.I.; Hollmann, M.W. On-demand versus continuous rocuronium infusion for deep neuromuscular relaxation in patients undergoing thoraco-laparoscopic esophagectomy: A randomized-controlled clinical trial (DEPTH). Can. J. Anaesth. 2019, 66, 1062–1074. [Google Scholar] [CrossRef] [Green Version]
- Altermatt, F.R.; Munoz, H.R.; Delfino, A.E.; Cortinez, L.I. Pre-oxygenation in the obese patient: Effects of position on tolerance to apnoea. Br. J. Anaesth. 2005, 95, 706–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Jong, A.; Changues, G.; Jaber, S. Mechanical ventilation in obese ICU patients: From intubation to extubation. Crit. Care 2017, 21, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pathak, R.A.; Wilson, R.R.A.; Craven, T.E.; Matz, E.; Hemal, A.K. The role of body mass index on quality indicators following minimally-invasive radical prostatectomy. Investig. Clin. Urol. 2021, 62, 209–297. [Google Scholar] [CrossRef] [PubMed]
- Claudius, C.; Viby-Mogensen, J. Neuromuscular monitoring. In Miller’s Anesthesia, 8th ed.; Miller, R.D., Ed.; Elsevier: Philadelphia, PA, USA, 2015; pp. 1604–1621. [Google Scholar]
- McGrath, C.D.; Hunter, J.M. Monitoring of neuromuscular block. CEACCP 2006, 6, 7–12. [Google Scholar] [CrossRef] [Green Version]

| Moderate NMB (n = 29) | Deep NMB (n = 29) | p-Value | |
|---|---|---|---|
| Age, years | 66.9 (6.7) | 65.9 (5.7) | 0.543 |
| Weight, kg | 71.2 (9.0) | 69.6 (7.3) | 0.458 |
| Height, cm | 167.1 (5.1) | 168.1 (5.4) | 0.474 |
| BMI, kg/m2 | 25.4 (2.5) | 24.4 (2.8) | 0.156 |
| ASA physical status (I/II), n (%) | 6 (20.7)/23 (79.3) | 5 (17.2)/24 (82.8) | 0.738 |
| Pulmonary function test, n (%) | 0.254 | ||
| Normal | 28 (96.6) | 26 (89.7) | |
| Borderline obstructive | 0 | 2 (6.9) | |
| Mild obstructive | 0 | 1 (3.4) | |
| Mild restrictive | 1 (3.4) | 0 | |
| Duration of surgery, min | 147.8 (25.6) | 149.1 (23.0) | 0.830 |
| Duration of anesthesia, min | 175.0 (25.0) | 180.0 (32.5) | 0.658 |
| Duration of CO2 insufflation, min | 118.1 (22.6) | 120.9 (23.8) | 0.652 |
| Crystalloid, mL | 655.5 (150.9) | 701.7 (211.9) | 0.343 |
| Estimated blood loss, mL | 131.0 (98.4) | 123.5 (67.5) | 0.733 |
| Rocuronium, mg | 68.1 (14.1) | 107.5 (21.5) | <0.001 |
| Moderate NMB (n = 29) | Deep NMB (n = 29) | p Value | |
|---|---|---|---|
| Endoscopic surgical conditions, n (%) | 0.014 | ||
| Extremely poor | 0 | 0 | |
| Poor | 1 (3.4) | 0 | |
| Acceptable | 2 (6.9) | 0 | |
| Good | 6 (20.7) | 0 | |
| Optimal | 20 (69.0) | 29 (100) | |
| Surgical difficulty, n (%) | 0.823 | ||
| Extremely poor | 3 (10.3) | 3 (10.3) | |
| Poor | 14 (48.3) | 12 (41.4) | |
| Acceptable | 8 (27.6) | 10 (34.5) | |
| Good | 3 (10.3) | 4 (13.8) | |
| Optimal | 1 (3.4) | 0 | |
| Increase in CO2 insufflation pressure | |||
| Number | 1 (1–2) | 1 (1–2) | 0.906 |
| Duration, min | 10 (5–27.5) | 12.5 (5–20) | 0.809 |
| Moderate NMB (n = 29) | Deep NMB (n = 29) | p Value | |
|---|---|---|---|
| SpO2 < 90% or RR < 8/min, n (%) | 2 (6.9) | 1 (3.4) | 0.553 |
| Lowest SpO2, % | 95.7 (2.7) | 96.1 (1.9) | 0.504 |
| Atelectasis, n (%) | 2 (6.9) | 0 | 0.150 |
| PaO2, mmHg | 89.5 (20.6) | 91.6 (24.7) | 0.735 |
| PaCO2, mmHg | 34.6 (6.9) | 35.5 (6.9) | 0.637 |
| Pain score, n (%) | 0.106 | ||
| NRS 3 | 1 (3.4) | 0 | |
| NRS 6 | 16 (55.2) | 8 (27.6) | |
| NRS 7 | 7 (24.1) | 12 (41.4) | |
| NRS 8 | 5 (17.2) | 9 (31.0) | |
| Analgesic requirement | 2 (1.5–3) | 2 (2–3) | 0.413 |
| PONV, n (%) | 1 (3.4) | 0 | 0.313 |
| a modified Aldrete score ≥ 9, min | 15 (6.0) | 15 (11.5) | 0.826 |
| PACU stay, min | 50 (14) | 50 (13) | 0.950 |
| Length of hospital stay, day | 8 (1) | 8 (2) | 0.616 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koo, C.-H.; Park, I.; Ahn, S.; Lee, S.; Ryu, J.-H. Effect of Neuromuscular Blockade on Intraoperative Respiratory Mechanics and Surgical Space Conditions during Robot-Assisted Radical Prostatectomy: A Prospective Randomized Controlled Trial. J. Clin. Med. 2021, 10, 5090. https://doi.org/10.3390/jcm10215090
Koo C-H, Park I, Ahn S, Lee S, Ryu J-H. Effect of Neuromuscular Blockade on Intraoperative Respiratory Mechanics and Surgical Space Conditions during Robot-Assisted Radical Prostatectomy: A Prospective Randomized Controlled Trial. Journal of Clinical Medicine. 2021; 10(21):5090. https://doi.org/10.3390/jcm10215090
Chicago/Turabian StyleKoo, Chang-Hoon, Insun Park, Sungmin Ahn, Sangchul Lee, and Jung-Hee Ryu. 2021. "Effect of Neuromuscular Blockade on Intraoperative Respiratory Mechanics and Surgical Space Conditions during Robot-Assisted Radical Prostatectomy: A Prospective Randomized Controlled Trial" Journal of Clinical Medicine 10, no. 21: 5090. https://doi.org/10.3390/jcm10215090
APA StyleKoo, C.-H., Park, I., Ahn, S., Lee, S., & Ryu, J.-H. (2021). Effect of Neuromuscular Blockade on Intraoperative Respiratory Mechanics and Surgical Space Conditions during Robot-Assisted Radical Prostatectomy: A Prospective Randomized Controlled Trial. Journal of Clinical Medicine, 10(21), 5090. https://doi.org/10.3390/jcm10215090






