Is Anterior Plating Superior to the Bilateral Use of Retrograde Transpubic Screws for Treatment of Straddle Pelvic Ring Fractures? A Biomechanical Investigation
Abstract
:1. Introduction
2. Materials and Methods
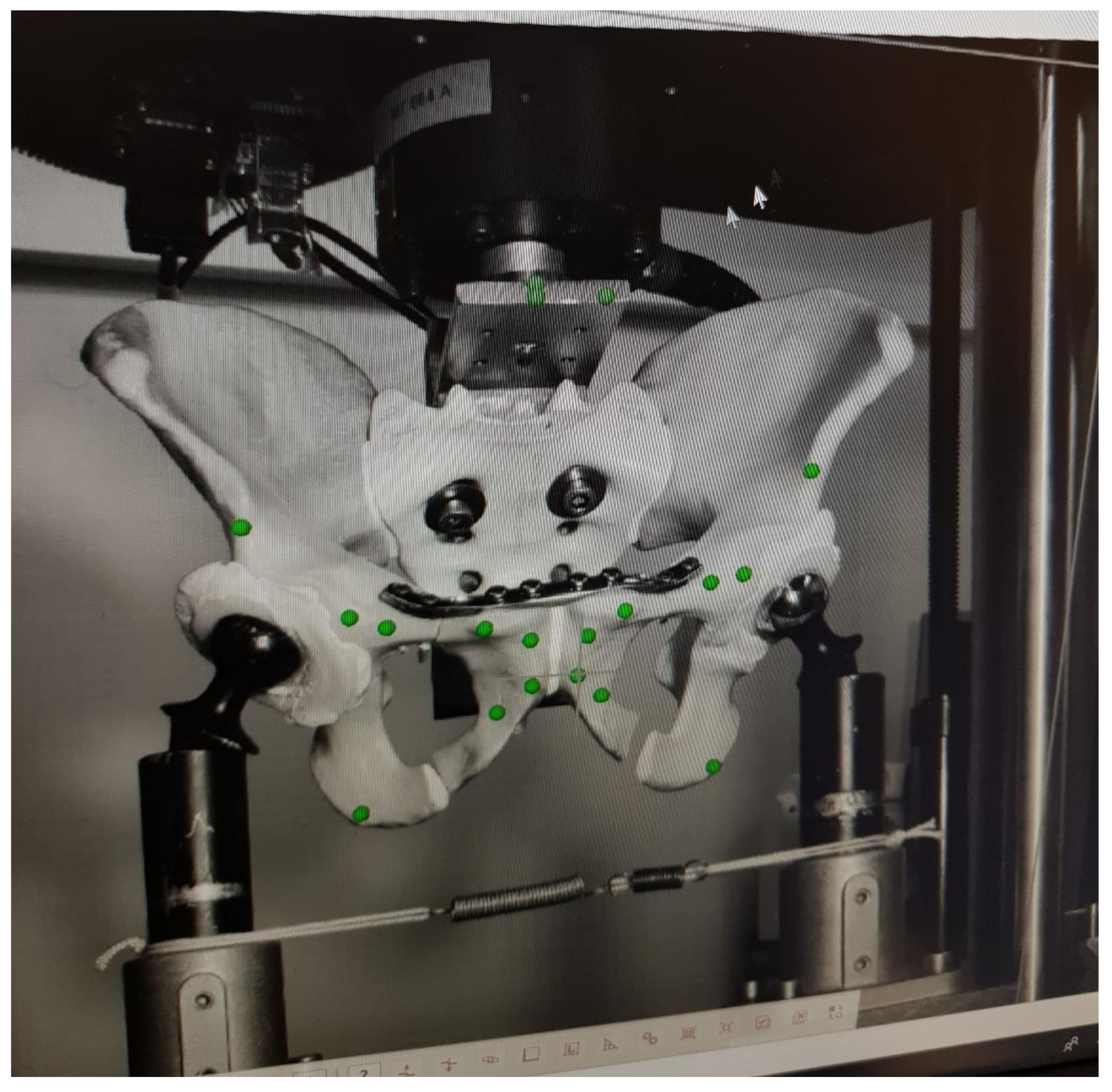
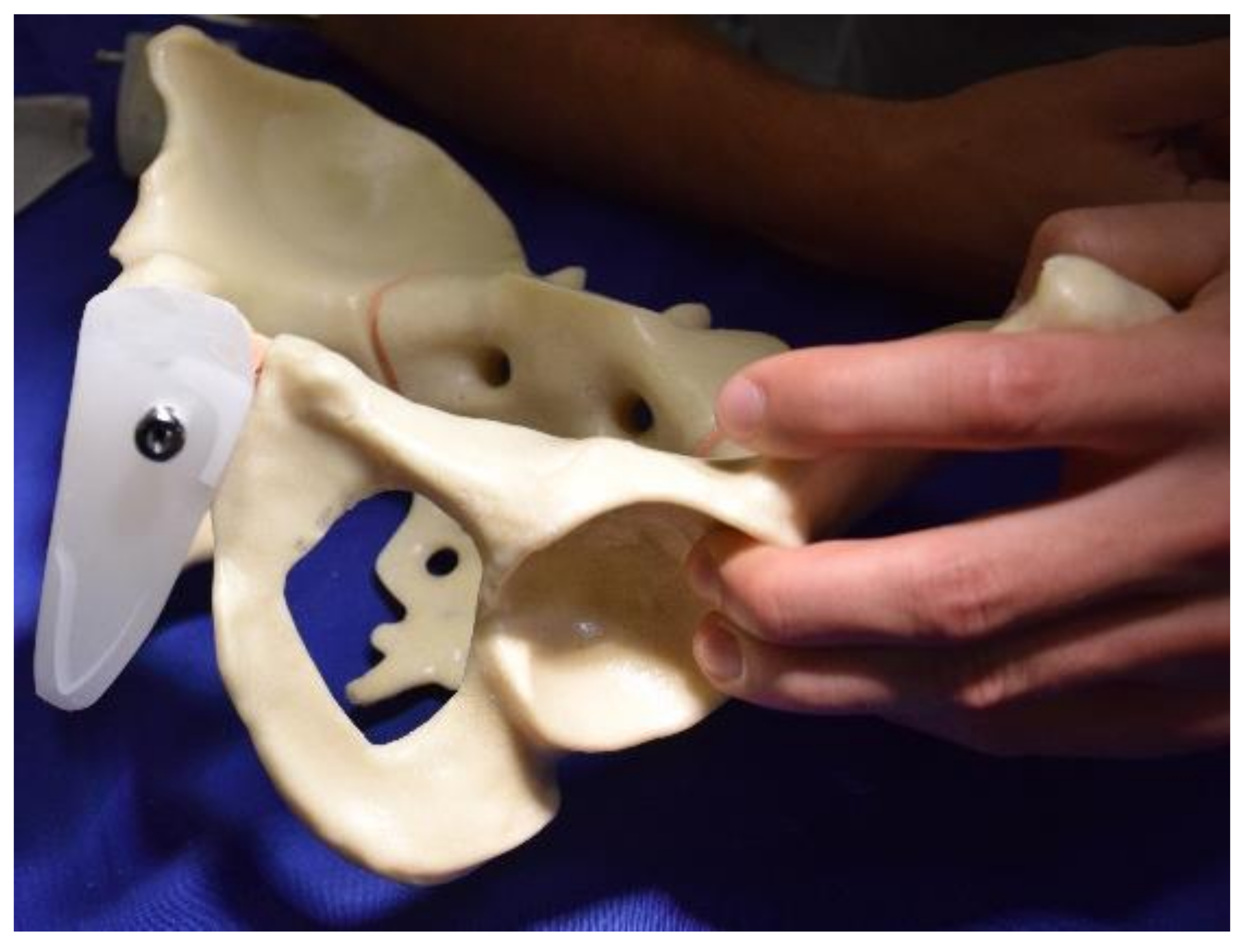
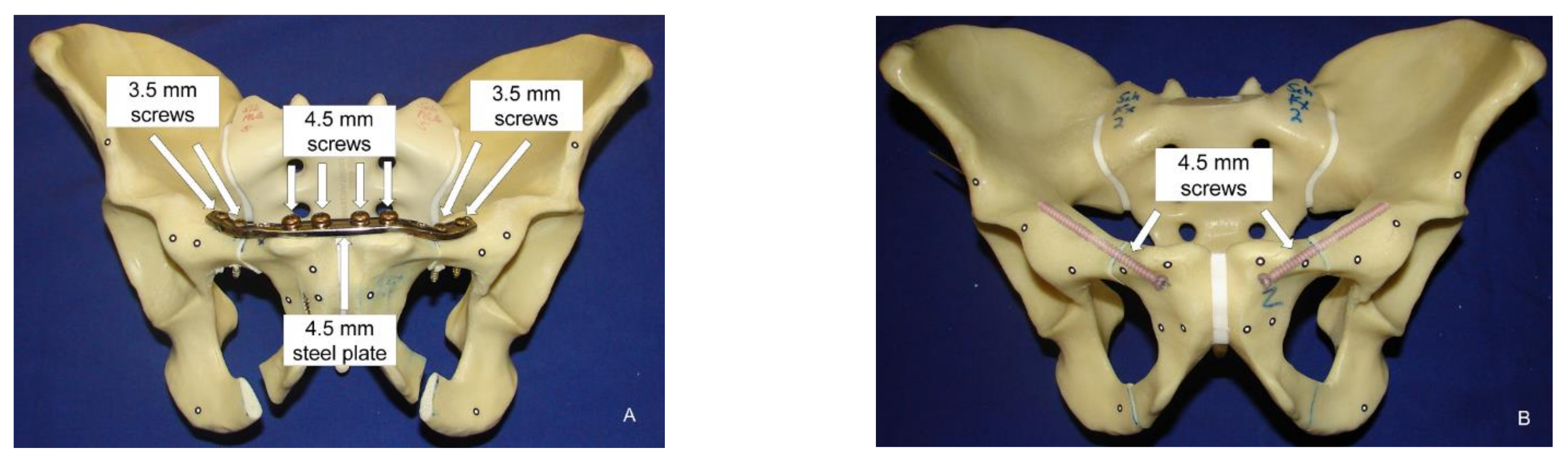
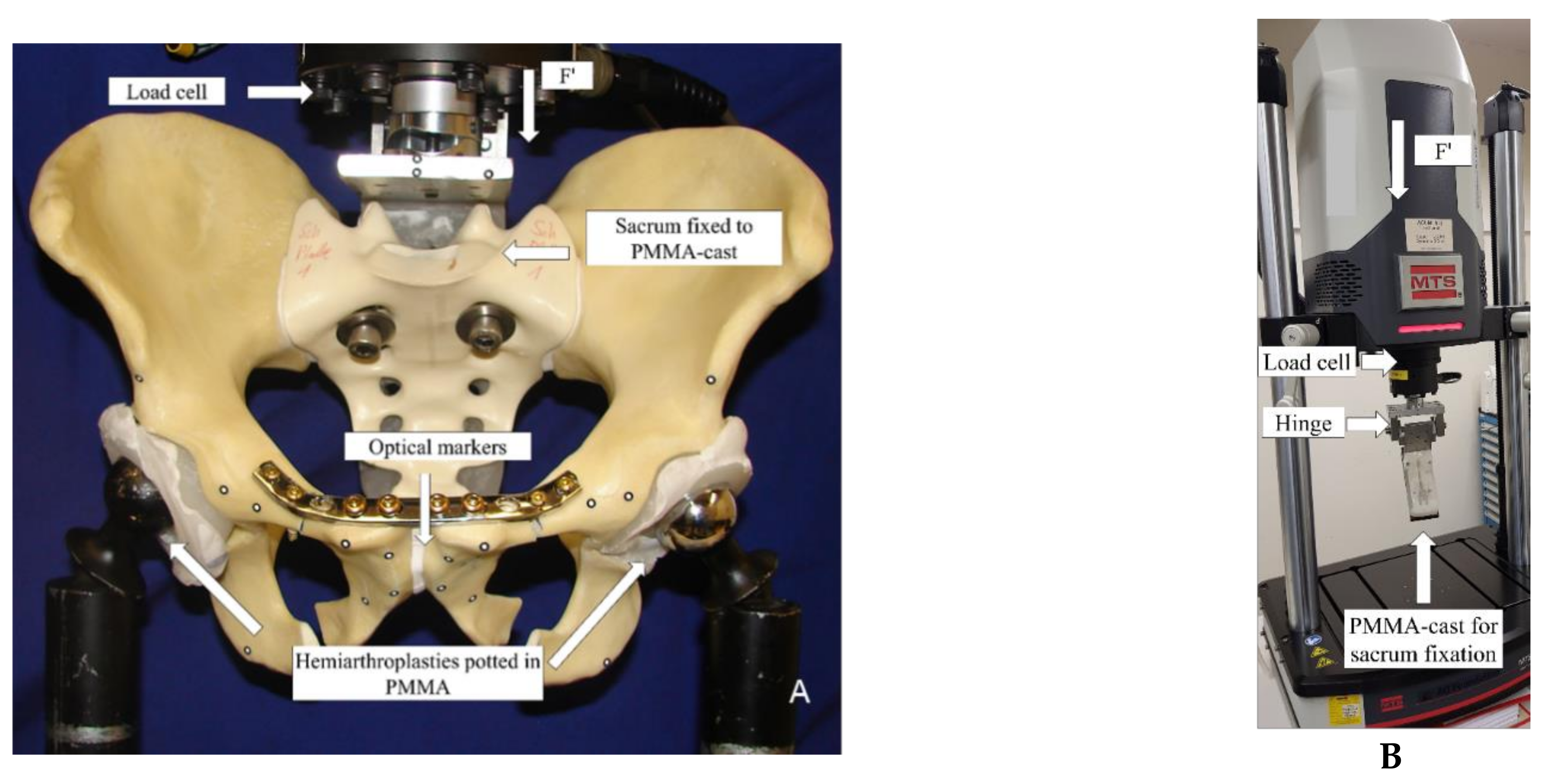
2.1. Biomechanical Testing
2.2. Data Acquisition and Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Dunn, A.W.; Morris, H.D. Fractures and dislocations of the pelvis. J. Bone Jt. Surg. 1968, 50, 1639–1648. [Google Scholar] [CrossRef]
- Young, J.W.; Burgess, A.R.; Brumback, R.J.; Poka, A. Pelvic fractures: Value of plain radiography in early assessment and management. Radiology 1986, 160, 445–451. [Google Scholar] [CrossRef]
- Cosker, T.D.A.; Ghandour, A.; Gupta, S.K.; Tayton, K.J.J. Pelvic ramus fractures in the elderly: 50 patients studied with MRI. Acta Orthop. 2005, 76, 513–516. [Google Scholar] [CrossRef]
- Yoon, Y.-C.; Ma, D.S.; Lee, S.K.; Oh, J.-K.; Song, H.K. Posterior pelvic ring injury of straddle fractures: Incidence, fixation methods, and clinical outcomes. Asian J. Surg. 2020, 44, 59–65. [Google Scholar] [CrossRef]
- Tornetta, P.; Dickson, K.; Matta, J.M. Outcome of Rotationally Unstable Pelvic Ring Injuries Treated Operatively. Clin. Orthop. Relat. Res. 1996, 329, 147–151. [Google Scholar] [CrossRef]
- Gruen, G.S.; Leit, M.E.; Gruen, R.J.; Peitzman, A.B. The acute management of hemodynamically unstable multiple trauma patients with pelvic ring fractures. J. Trauma 1994, 36, 706–711, discussion 711-3. [Google Scholar] [CrossRef] [PubMed]
- Lange, R.H.; Hansen, S.T. Pelvic ring disruptions with symphysis pubis diastasis. Indications, technique, and limitations of anterior internal fixation. Clin. Orthop. Relat. Res. 1985, 201, 130–137. [Google Scholar] [CrossRef]
- Gänsslen, A.; Krettek, C. Retrograde transpubic screw fixation of transpubic instabilities. Oper. Orthop. Traumatol. 2006, 18, 330–340. [Google Scholar] [CrossRef]
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium-2018. J. Orthop. Trauma 2018, 32 (Suppl. S1), S1–S170. [Google Scholar] [CrossRef]
- Tile, M. Pelvic ring fractures: Should they be fixed? J. Bone Jt. Surg. Br. 1988, 70, 1–12. [Google Scholar] [CrossRef]
- Marecek, G.S.; Scolaro, J.A. Anterior Pelvic Ring: Introduction to Evaluation and Management. J. Orthop. Trauma 2018, 32 (Suppl. S6), S1–S3. [Google Scholar] [CrossRef] [PubMed]
- Matta, J.M. Indications for anterior fixation of pelvic fractures. Clin. Orthop. Relat. Res. 1996, 329, 88–96. [Google Scholar] [CrossRef]
- Gamble, J.G.; Simmons, S.C.; Freedman, M. The symphysis pubis. Anatomic and pathologic considerations. Clin. Orthop. Relat. Res. 1986, 203, 261–272. [Google Scholar] [CrossRef]
- Albin, L. L’ Intervention Opératoire dans les Fractures Récentes et Anciennes Envisagées Particuliérement du Point de Vue de L’ostéosynthèse; Lambertin: Brussels, Belgium, 1907. [Google Scholar]
- Albin, L. Chirurgie Opératoire des Fractures; Masson: Paris, France, 1913. [Google Scholar]
- Rommens, P.M.; Tile, M. A short history of pelvic trauma surgery. Part 1; The pelvic ring: From Malgaigne to the present. AO Dialoque 2003, 16, 28–30. [Google Scholar]
- Goldstein, A.; Phillips, T.; Sclafani, S.J.; Scalea, T.; Duncan, A.; Goldstein, J.; Panetta, T.; Shaftan, G. Early open reduction and internal fixation of the disrupted pelvic ring. J. Trauma 1986, 26, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Routt, M.L.; Simonian, P.T.; Grujic, L. The retrograde medullary superior pubic ramus screw for the treatment of anterior pelvic ring disruptions: A new technique. J. Orthop. Trauma 1995, 9, 35–44. [Google Scholar] [CrossRef]
- Keating, J.F.; Werier, J.; Blachut, P.; Broekhuyse, H.; Meek, R.N.; O’Brien, P.J. Early fixation of the vertically unstable pelvis: The role of iliosacral screw fixation of the posterior lesion. J. Orthop. Trauma 1999, 13, 107–113. [Google Scholar] [CrossRef]
- Hiesterman, T.G.; Hill, B.W.; Cole, P.A. Surgical technique: A percutaneous method of subcutaneous fixation for the anterior pelvic ring: The pelvic bridge. Clin. Orthop. Relat. Res. 2012, 470, 2116–2123. [Google Scholar] [CrossRef] [Green Version]
- Cole, P.A.; Dyskin, E.A.; Gilbertson, J.A. Minimally-invasive fixation for anterior pelvic ring disruptions. Injury 2015, 46, S27–S34. [Google Scholar] [CrossRef]
- Winkelhagen, J.; van den Bekerom, M.P.J.; Bolhuis, H.W.; Hogervorst, M. Preliminary results of cannulated screw fixation for isolated pubic ramus fractures. Strateg. Trauma Limb Reconstr. 2012, 7, 87–91. [Google Scholar] [CrossRef] [Green Version]
- Rommens, P.M.; Graafen, M.; Arand, C.; Mehling, I.; Hofmann, A.; Wagner, D. Minimal-invasive stabilization of anterior pelvic ring fractures with retrograde transpubic screws. Injury 2020, 51, 340–346. [Google Scholar] [CrossRef]
- Simonian, P.T.; Routt, M.L.; Harrington, R.M.; Tencer, A.F. Internal fixation of the unstable anterior pelvic ring: A biomechanical comparison of standard plating techniques and the retrograde medullary superior pubic ramus screw. J. Orthop. Trauma 1994, 8, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Grüneweller, N.; Raschke, M.J.; Zderic, I.; Widmer, D.; Wähnert, D.; Gueorguiev, B.; Richards, R.G.; Fuchs, T.; Windolf, M. Biomechanical comparison of augmented versus non-augmented sacroiliac screws in a novel hemi-pelvis test model. J. Orthop. Res. 2017, 35, 1485–1493. [Google Scholar] [CrossRef] [PubMed]
- VDI/VDE. Optical 3D Measuring Systems, Imaging Systems with Point-by-Point Probing; Beuth Verlag, Verein Deutscher Ingenieure Berlin: Berlin, Germany, 2002; pp. 1–10. [Google Scholar]
- Zderic, I.; Wagner, D.; Schopper, C.; Lodde, M.; Richards, G.; Gueorguiev, B.; Rommens, P.; Acklin, Y.P. Screw-in-screw fixation of fragility sacrum fractures provides high stability without loosening-biomechanical evaluation of a new concept. J. Orthop. Res. 2020, 39, 761–770. [Google Scholar] [CrossRef] [PubMed]
- McLachlin, S.; Lesieur, M.; Stephen, D.; Kreder, H.; Whyne, C. Biomechanical analysis of anterior ring fixation of the ramus in type C pelvis fractures. Eur. J. Trauma Emerg. Surg. 2018, 44, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Acklin, Y.P.; Zderic, I.; Grechenig, S.; Richards, R.G.; Schmitz, P.; Gueorguiev, B. Are two retrograde 3.5 mm screws superior to one 7.3 mm screw for anterior pelvic ring fixation in bones with low bone mineral density? Bone Jt. Res. 2017, 6, 8–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Acklin, Y.P.; Zderic, I.; Buschbaum, J.; Varga, P.; Inzana, J.A.; Grechenig, S.; Richards, R.G.; Gueorguiev, B.; Schmitz, P. Biomechanical comparison of plate and screw fixation in anterior pelvic ring fractures with low bone mineral density. Injury 2016, 47, 1456–1460. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Zhang, Y.; Wu, G.; Wang, Z.; Cai, X. The Influence of Pelvic Ramus Fracture on the Stability of Fixed Pelvic Complex Fracture. Comput. Math. Methods Med. 2015, 2015, 790575. [Google Scholar] [CrossRef] [Green Version]
- Cole, P.A.; Gauger, E.M.; Anavian, J.; Ly, T.V.; Morgan, R.A.; Heddings, A.A. Anterior pelvic external fixator versus subcutaneous internal fixator in the treatment of anterior ring pelvic fractures. J. Orthop. Trauma 2012, 26, 269–277. [Google Scholar] [CrossRef]
- Apivatthakakul, T.; Rujiwattanapong, N. “Anterior subcutaneous pelvic internal fixator (INFIX), Is it safe?” A cadaveric study. Injury 2016, 47, 2077–2080. [Google Scholar] [CrossRef]
- Studer, P.; Suhm, N.; Zappe, B.; Bless, N.; Jakob, M. Pubic rami fractures in the elderly—A neglected injury? Swiss Med. Wkly. 2013, 143, w13859. [Google Scholar] [CrossRef] [PubMed]
- Bastian, J.D.; Ansorge, A.; Tomagra, S.; Siebenrock, K.A.; Benneker, L.M.; Büchler, L.; Keel, M.J.B. Anterior fixation of unstable pelvic ring fractures using the modified Stoppa approach: Mid-term results are independent on patients’ age. Eur. J. Trauma Emerg. Surg. 2016, 42, 645–650. [Google Scholar] [CrossRef] [PubMed]
- Elfar, J.; Menorca, R.M.G.; Reed, J.D.; Stanbury, S. Composite bone models in orthopaedic surgery research and education. J. Am. Acad. Orthop. Surg. 2014, 22, 111–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Neill, F.; Condon, F.; McGloughlin, T.; Lenehan, B.; Coffey, C.; Walsh, M. Validity of synthetic bone as a substitute for osteoporotic cadaveric femoral heads in mechanical testing: A biomechanical study. Bone Jt. Res. 2012, 1, 50–55. [Google Scholar] [CrossRef]
- Wähnert, D.; Hoffmeier, K.L.; Klos, K.; Stolarczyk, Y.; Fröber, R.; Hofmann, G.O.; Mückley, T. Biomechanical characterization of an osteoporotic artificial bone model for the distal femur. J. Biomater. Appl. 2012, 26, 565–579. [Google Scholar] [CrossRef]
- Reed, J.D.; Stanbury, S.J.; Menorca, R.M.; Elfar, J.C. The emerging utility of composite bone models in biomechanical studies of the hand and upper extremity. J. Hand Surg. Am. 2013, 38, 583–587. [Google Scholar] [CrossRef] [Green Version]
- Letourne, E. Surgical management of hip joint-acetabulum fractures. Langenbecks Arch. Chir. 1966, 316, 422–437. [Google Scholar] [CrossRef]
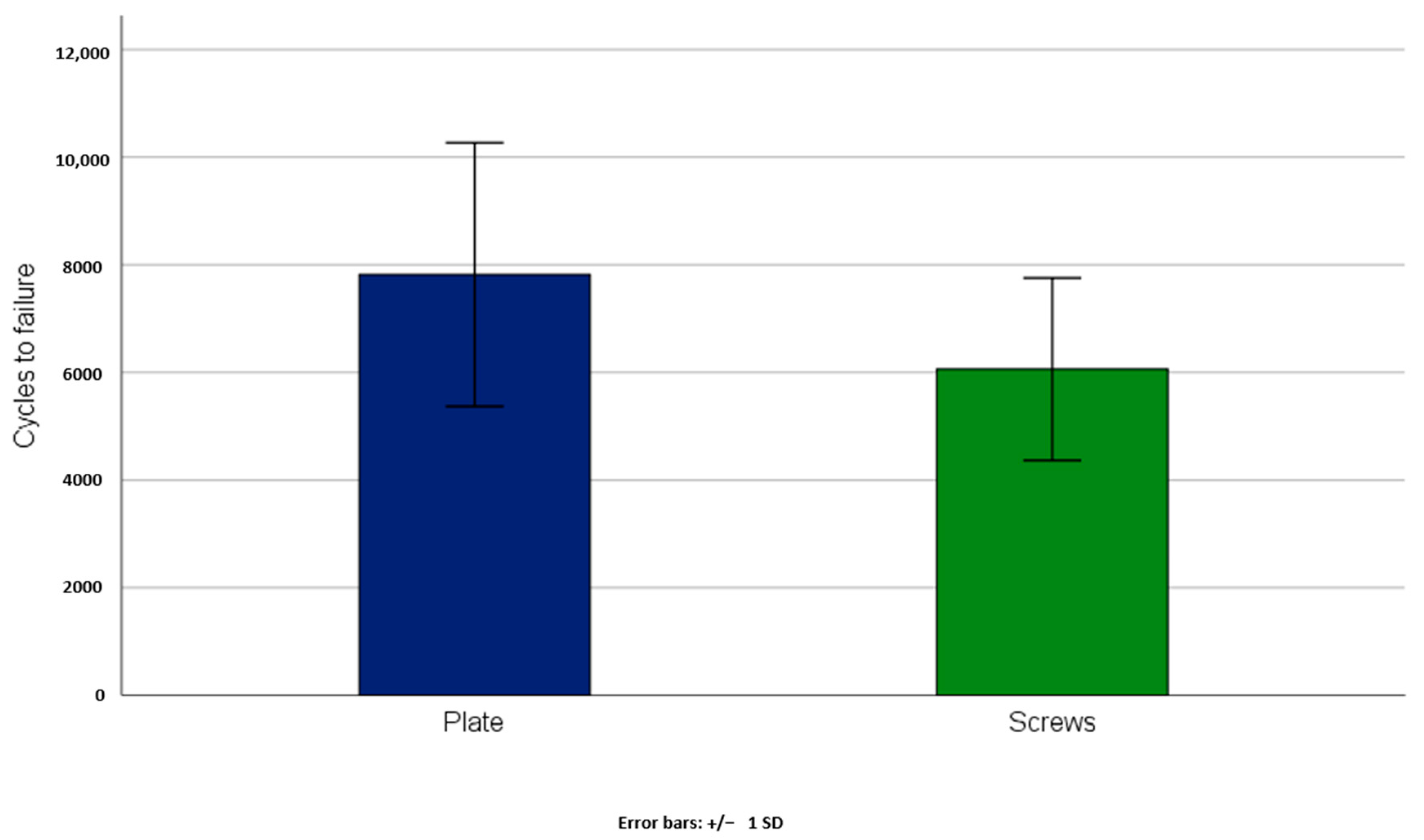
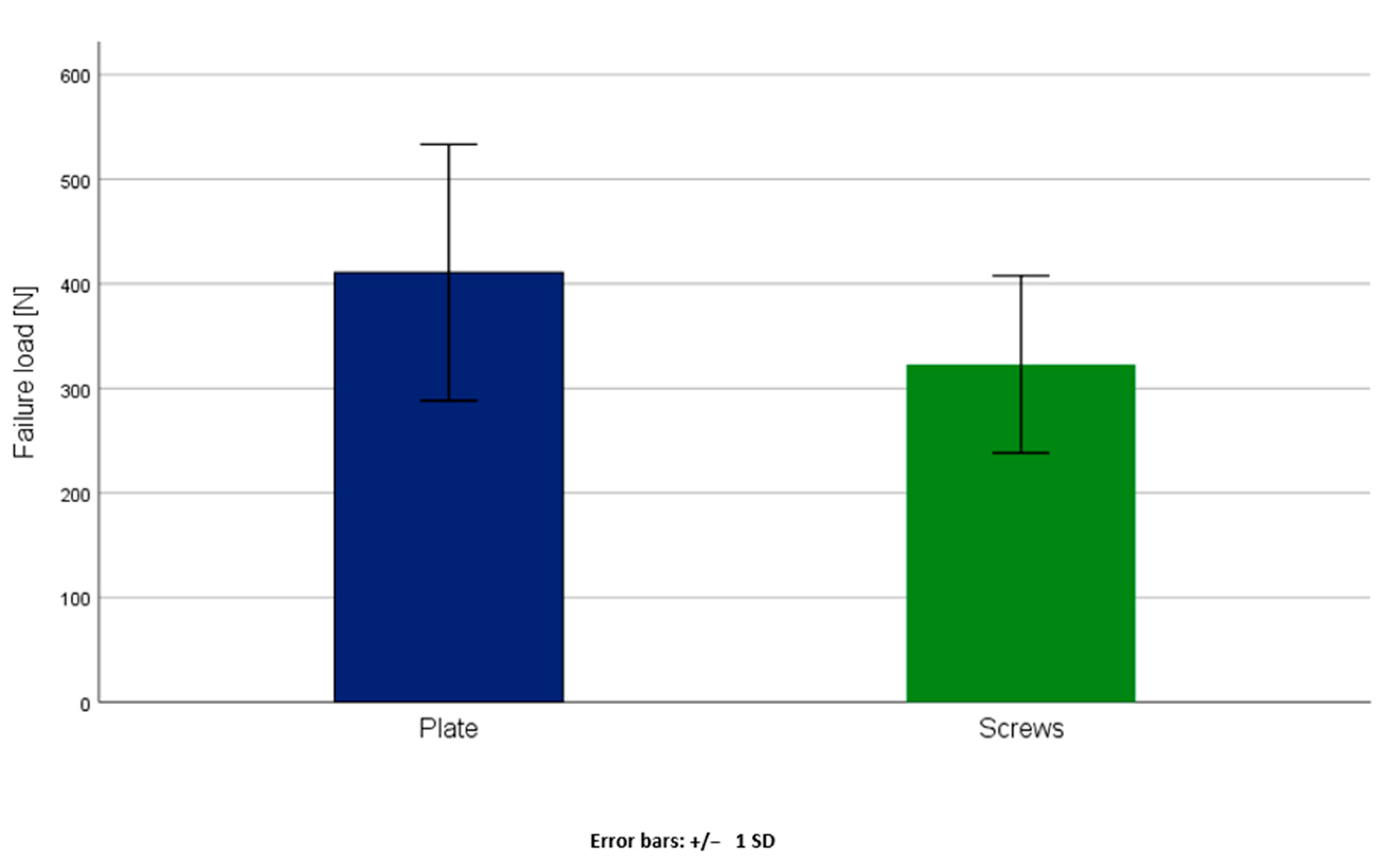
| Groups | Axial Stiffness [N/mm] | Cycles to Failure | Failure Load [N] |
|---|---|---|---|
| Anterior plate fixation | 5.10 ± 4.59 | 7816 ± 2450 | 410.81 ± 122.48 |
| Bilateral retrograde transpubic screws | 4.73 ± 4.23 | 6058 ± 1695 | 322.91 ± 84.74 |
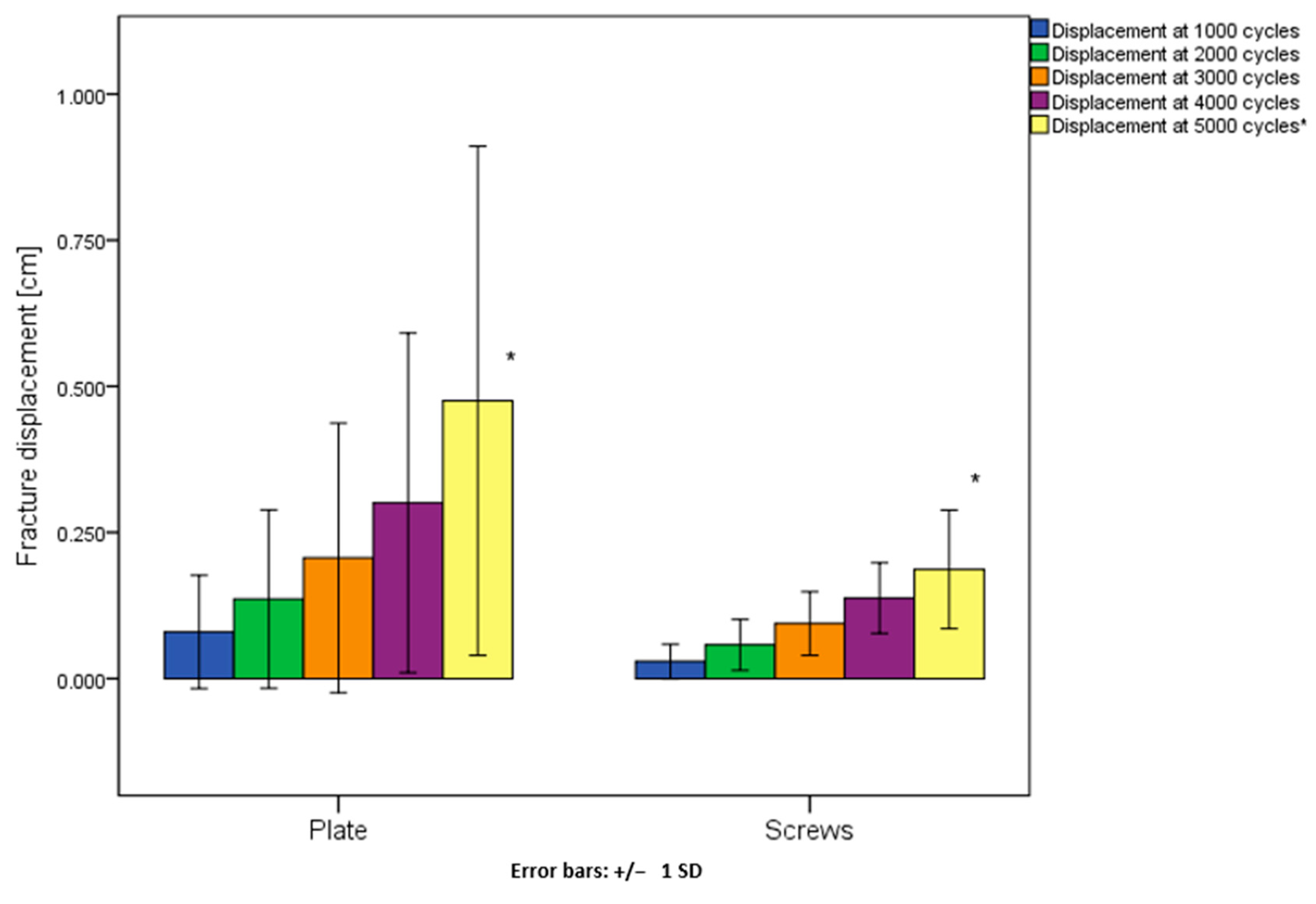
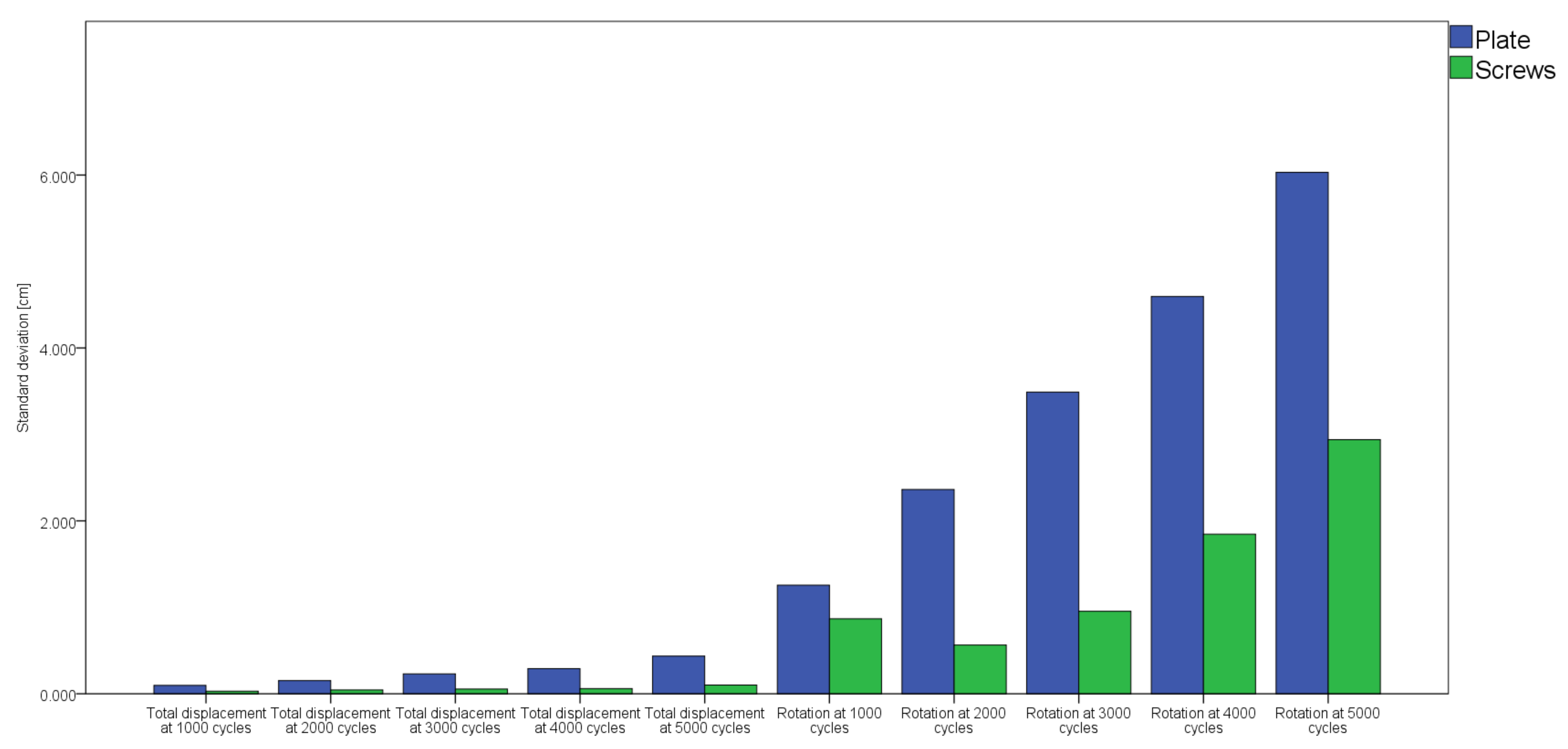
| Groups | Fracture Displacement [cm] | ||||
|---|---|---|---|---|---|
| at 1000 cycles | at 2000 cycles | at 3000 cycles | at 4000 cycles | at 5000 cycles | |
| Anterior plate fixation | 0.03 (0.19) | 0.06 (0.29) | 0.10 (0.44) | 0.21 (0.52) | 0.36 (0.36) |
| Bilateral retrograde transpubic screws | 0.02 (0.02) | 0.05 (0.05) | 0.08 (0.06) | 0.12 (0.10) | 0.19 (0.10) |
| Groups | Relative Flexural Rotations [Degrees] | ||||
|---|---|---|---|---|---|
| at 1000 cycles | at 2000 cycles | at 3000 cycles | at 4000 cycles | at 5000 cycles | |
| Anterior plate fixation | 0.31 (0.35) | 0.42 (1.10) | 1.00 (1.90) | 1.73 (1.50) | 2.47 (2.50) |
| Bilateral retrograde transpubic screws | 0.26 (0.37) | 0.40 (0.72) | 0.77 (1.27) | 1.60 (1.96) | 3.40 (3.45) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, R.G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Is Anterior Plating Superior to the Bilateral Use of Retrograde Transpubic Screws for Treatment of Straddle Pelvic Ring Fractures? A Biomechanical Investigation. J. Clin. Med. 2021, 10, 5049. https://doi.org/10.3390/jcm10215049
Lodde MF, Katthagen JC, Schopper CO, Zderic I, Richards RG, Gueorguiev B, Raschke MJ, Hartensuer R. Is Anterior Plating Superior to the Bilateral Use of Retrograde Transpubic Screws for Treatment of Straddle Pelvic Ring Fractures? A Biomechanical Investigation. Journal of Clinical Medicine. 2021; 10(21):5049. https://doi.org/10.3390/jcm10215049
Chicago/Turabian StyleLodde, Moritz F., J. Christoph Katthagen, Clemens O. Schopper, Ivan Zderic, R. Geoff Richards, Boyko Gueorguiev, Michael J. Raschke, and René Hartensuer. 2021. "Is Anterior Plating Superior to the Bilateral Use of Retrograde Transpubic Screws for Treatment of Straddle Pelvic Ring Fractures? A Biomechanical Investigation" Journal of Clinical Medicine 10, no. 21: 5049. https://doi.org/10.3390/jcm10215049
APA StyleLodde, M. F., Katthagen, J. C., Schopper, C. O., Zderic, I., Richards, R. G., Gueorguiev, B., Raschke, M. J., & Hartensuer, R. (2021). Is Anterior Plating Superior to the Bilateral Use of Retrograde Transpubic Screws for Treatment of Straddle Pelvic Ring Fractures? A Biomechanical Investigation. Journal of Clinical Medicine, 10(21), 5049. https://doi.org/10.3390/jcm10215049









