The Practice of Deep Sedation in Electrophysiology and Cardiac Pacing Laboratories: Results of an Italian Survey Promoted by the AIAC (Italian Association of Arrhythmology and Cardiac Pacing)
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
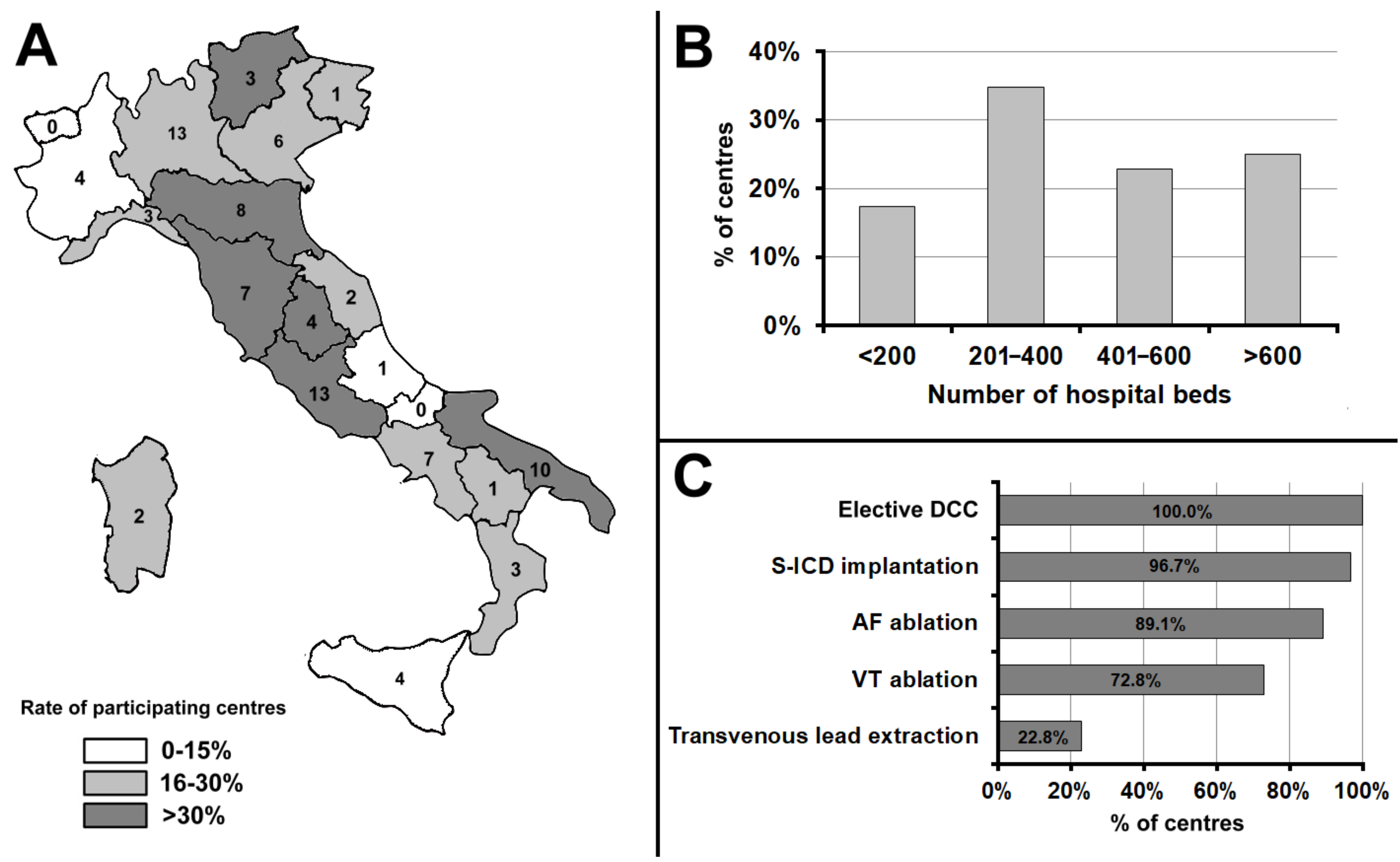
3.1. Participating Centres
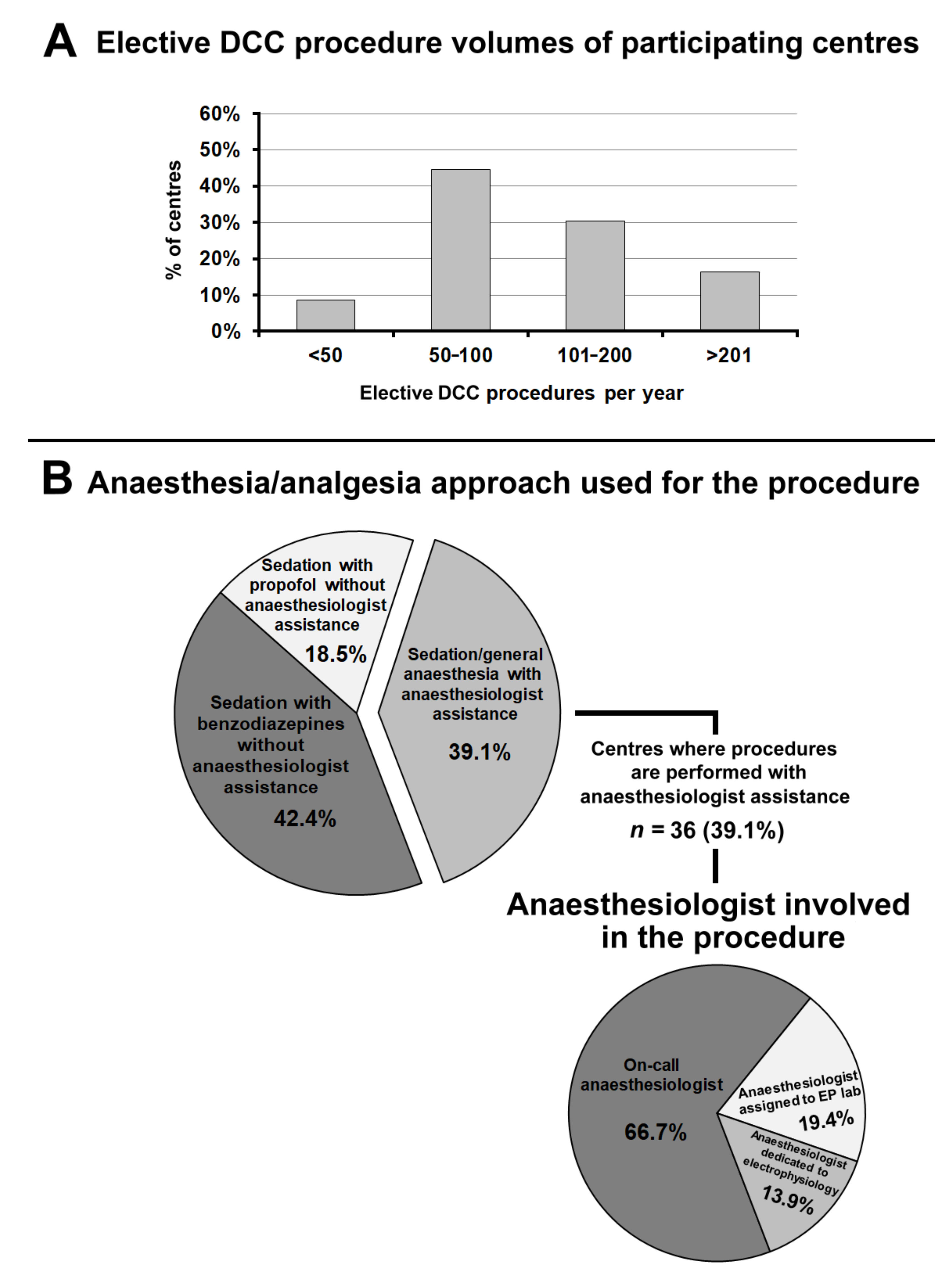
3.2. Elective Direct-Current Cardioversion
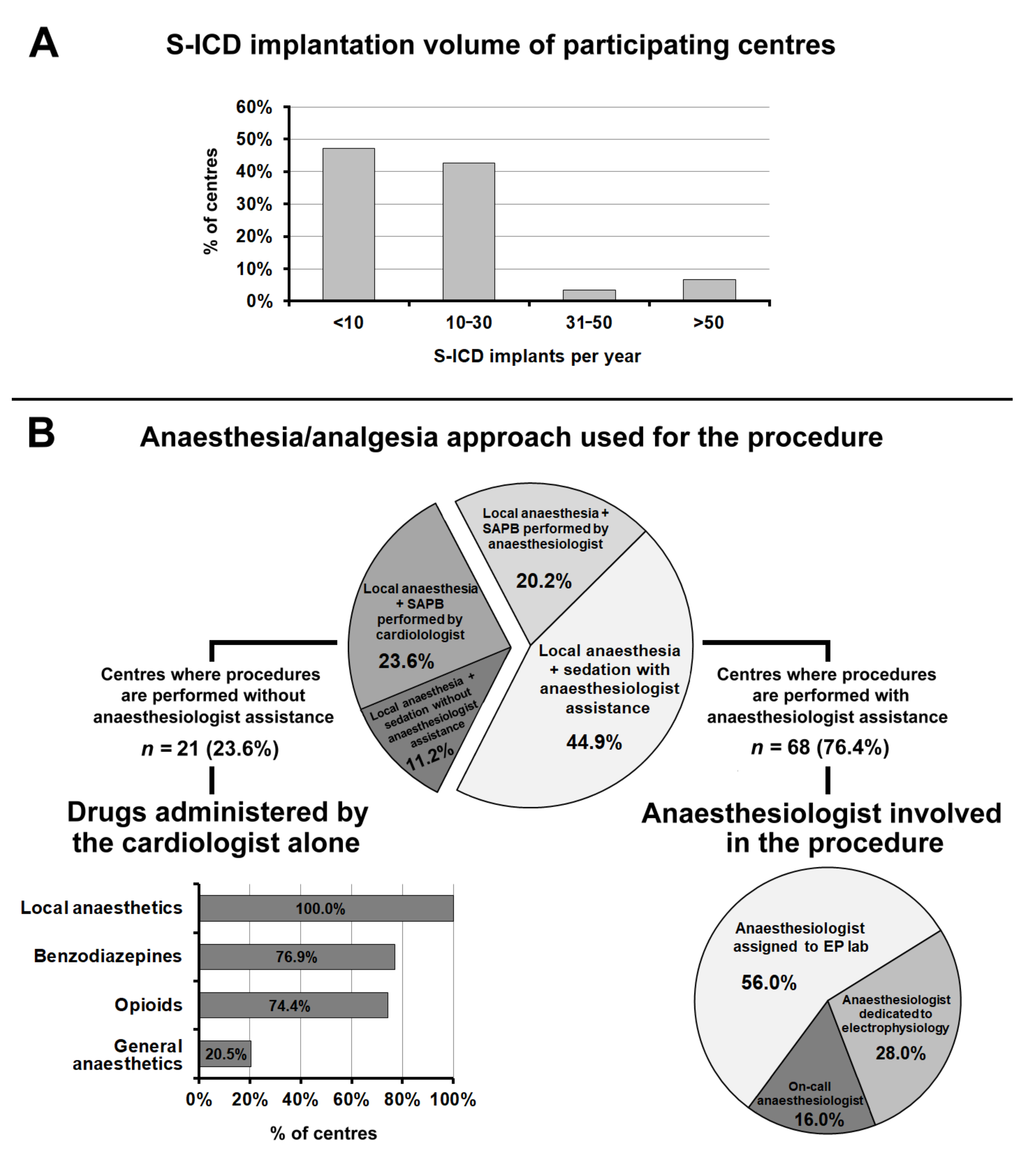
3.3. S-ICD Implantation
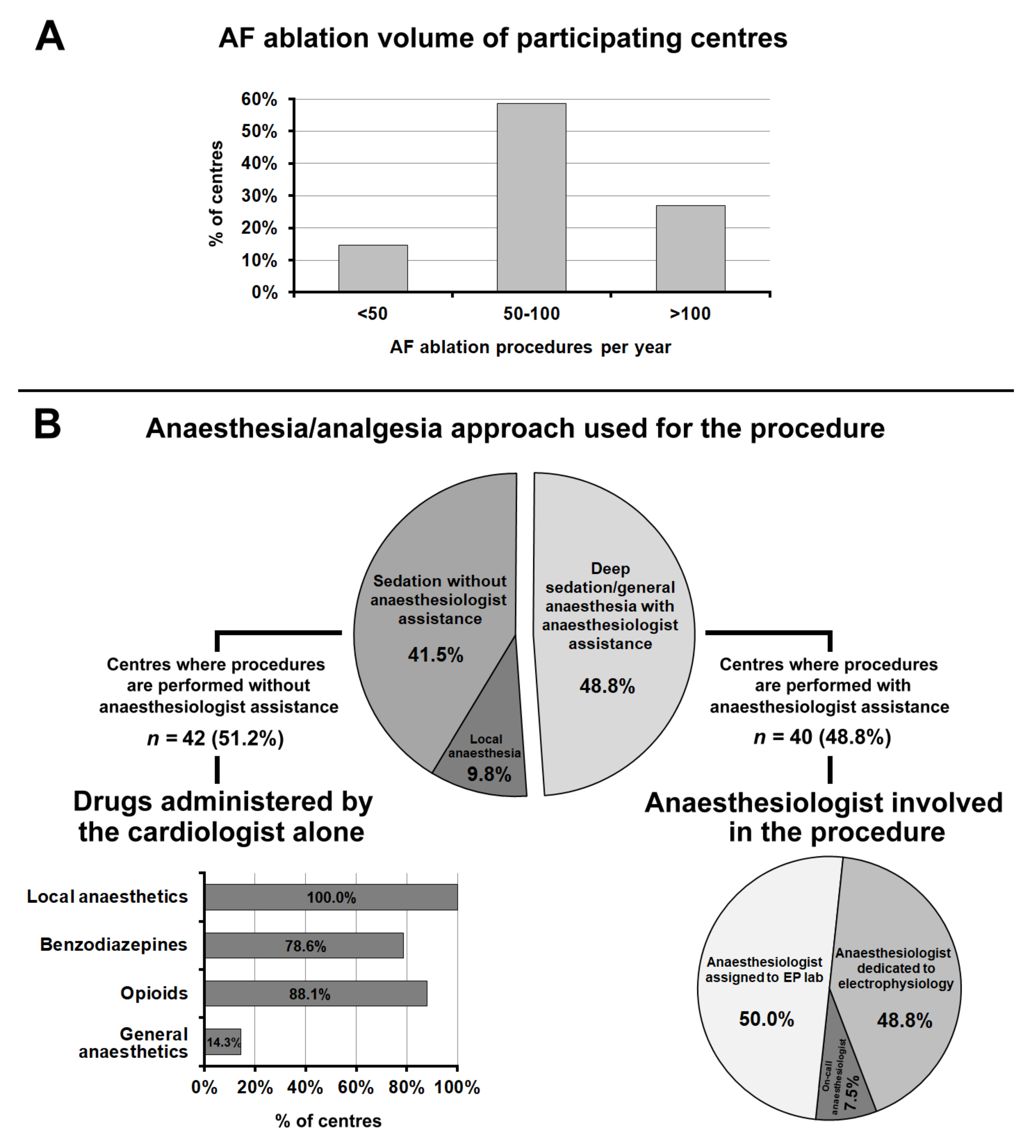
3.4. Atrial Fibrillation Ablation
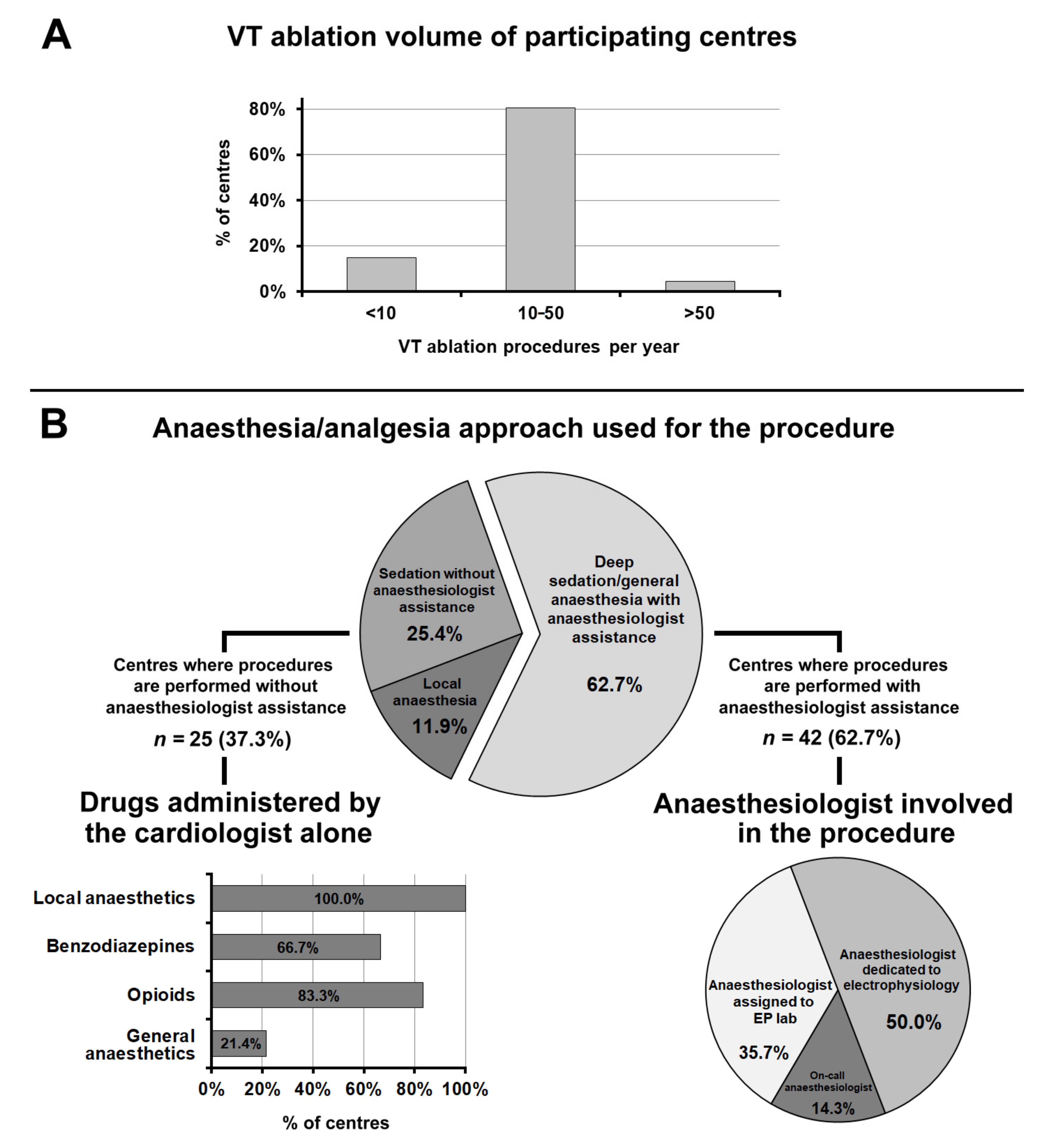
3.5. Ventricular Tachycardia Ablation
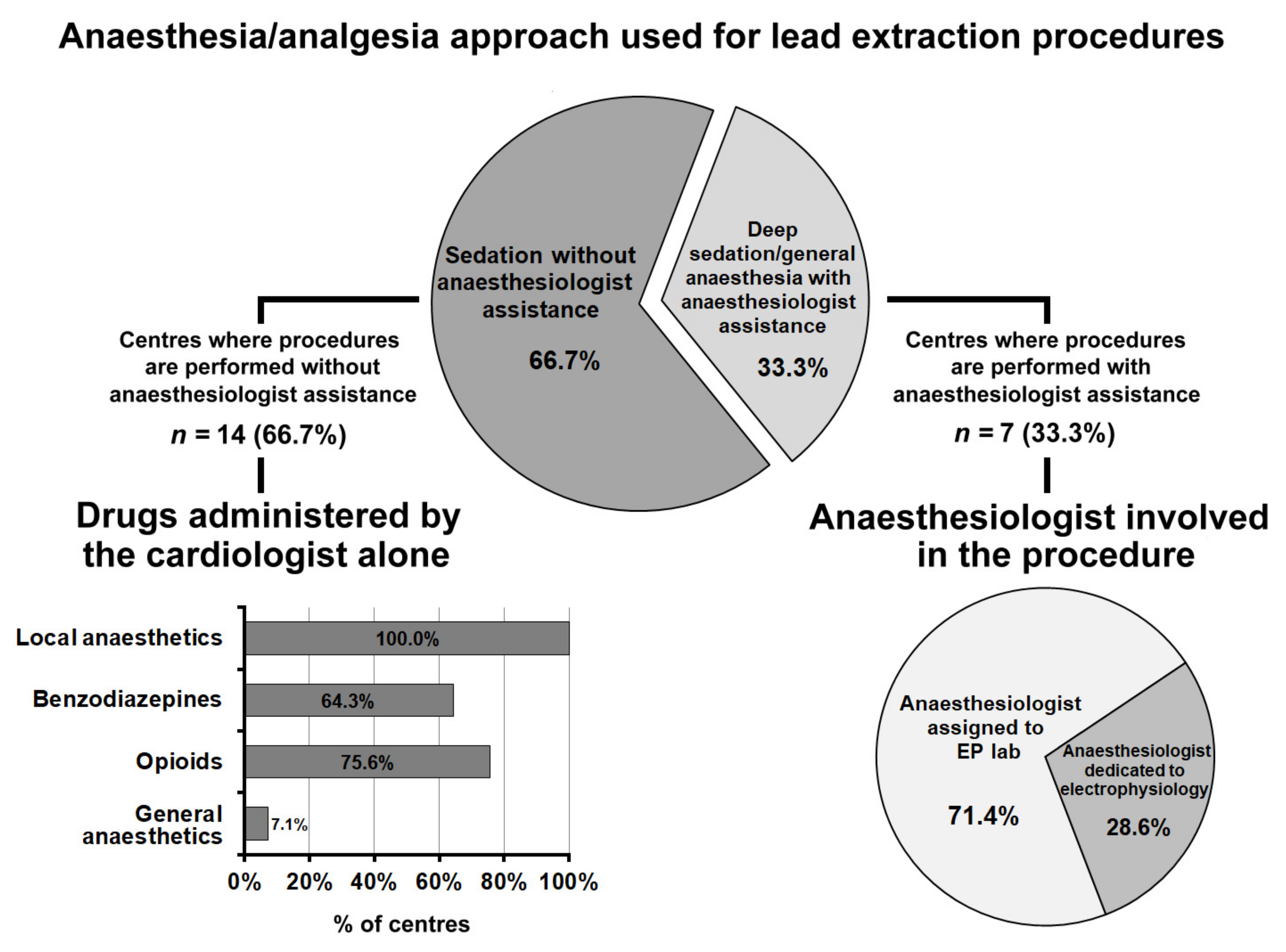
3.6. Transvenous Lead Extraction
3.7. General Aspects of Sedation and Anaesthesia in Electrophysiological Procedures
4. Discussion
5. Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Trentman, T.L.; Fassett, S.L.; Mueller, J.T.; Altemose, G.T. Airway Interventions in the Cardiac Electrophysiology Laboratory: A Retrospective Review. J. Cardiothorac. Vasc. Anesth. 2009, 23, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Gerstein, N.S.; Young, A.; Schulman, P.M.; Stecker, E.C.; Jessel, P.M. Sedation in the Electrophysiology Laboratory: A Multidisciplinary Review. J. Am. Heart Assoc. 2016, 5, e003629. [Google Scholar] [CrossRef] [Green Version]
- Apfelbaum, J.; Gross, J.; Connis, R.; Agarkar, M.; Arnold, D.; Coté, C.; Tung, A. Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018: A Report by the American Society of Anesthesiologists Task Force on Moderate Procedural Sedation and Analgesia, the American Association of Oral and Maxillofacial Surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology. Anesthesiology 2018, 128, 437–479. [Google Scholar]
- Green, S.M.; Roback, M.G.; Krauss, B.S.; Miner, J.R.; Schneider, S.; Kivela, P.D.; Nelson, L.S.; Chumpitazi, C.E.; Fisher, J.D.; Gesek, D.; et al. Unscheduled Procedural Sedation: A Multidisciplinary Consensus Practice Guideline. Ann. Emerg. Med. 2019, 73, e51–e65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ziacchi, M.; Bisignani, G.; Palmisano, P.; Scalone, A.; Martignani, C.; Mocavero, P.E.; Caravati, F.; Della Cioppa, N.; Mazzuero, A.; Pecora, D.; et al. Serratus anterior plane block in subcutaneous implantable cardioverter defibrillator implantation: A case-control analysis. J. Cardiovasc. Electrophysiol. 2019, 31, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Biffi, M.; Ammendola, E.; Menardi, E.; Parisi, Q.; Narducci, M.L.; De Filippo, P.; Manzo, M.; Stabile, G.; Potenza, D.R.; Zanon, F.; et al. Real-life outcome of implantable cardioverter-defibrillator and cardiac resynchronization defibrillator replacement/upgrade in a contemporary population: Observations from the multicentre DECODE registry. Europace 2019, 21, 1527–1536. [Google Scholar] [CrossRef]
- Nair, G.M.; Birnie, D.H.; Sumner, G.L.; Krahn, A.D.; Healey, J.S.; Nery, P.B.; Kalfon, E.; Verma, A.; Ayala-Paredes, F.; Coutu, B.; et al. Post-operative pain following cardiac implantable electronic device implantation: Insights from the BRUISE CONTROL trials. Europace 2021, 23, 748–756. [Google Scholar] [CrossRef]
- Palmisano, P.; Ziacchi, M.; Belotti, G.; Rapacciuolo, A.; Santini, L.; Stabile, G.; Berisso, M.Z.; De Ponti, R.; Landolina, M.; Ricci, R.P.; et al. Clinical and organizational management of cardiac implantable electronic device replacements. J. Cardiovasc. Med. 2019, 20, 531–541. [Google Scholar] [CrossRef]
- Ziacchi, M.; Palmisano, P.; Biffi, M.; Guerra, F.; Stabile, G.; Forleo, G.B.; Zanotto, G.; D’Onofrio, A.; Landolina, M.; De Ponti, R.; et al. Lead choice in cardiac implantable electronic devices: An Italian survey promoted by AIAC (Italian Association of Arrhythmias and Cardiac Pacing). Expert Rev. Med. Devices 2019, 16, 821–828. [Google Scholar] [CrossRef]
- Guerra, F.; Pavoni, I.; Romandini, A.; Baldetti, L.; Matassini, M.V.; Brambatti, M.; Luzi, M.; Pupita, G.; Capucci, A. Feasibility of a cardiologist-only approach to sedation for electrical cardioversion of atrial fibrillation: A randomized, open-blinded, prospective study. Int. J. Cardiol. 2014, 176, 930–935. [Google Scholar] [CrossRef]
- Stronati, G.; Capucci, A.; Russo, A.D.; Adrario, E.; Carsetti, A.; Casella, M.; Donati, A.; Guerra, F. Procedural sedation for direct current cardioversion: A feasibility study between two management strategies in the emergency department. BMC Cardiovasc. Disord. 2020, 20, 388. [Google Scholar] [CrossRef] [PubMed]
- Uran, C.; Giojelli, A.; Borgogna, D.A.; Morello, G.; Marullo, F.; Iodice, P.; Greco, A.; Accogli, M.; Guido, A.; Palmisano, P. Ultrasound-guided serratus anterior plane block combined with parasternal block in subcutaneous implantable cardioverter defibrillator implantation: Results of a pilot study. Pacing Clin. Electrophysiol. 2020, 43, 705–712. [Google Scholar] [CrossRef]
- Vergara, P.; Casella, M.; Barbato, G.; De Ruvo, E.; Grandinetti, G.; Notarstefano, P.; Tola, G.; Calvi, V.; Santini, L.; Nissardi, V.; et al. Nationwide survey on the current practice of ventricular tachycardia ablation. J. Cardiovasc. Med. 2019, 20, 597–605. [Google Scholar] [CrossRef]
- Guarracini, F.; Casella, M.; Muser, D.; Barbato, G.; Notarstefano, P.; Sgarito, G.; Marini, M.; Grandinetti, G.; Mariani, M.V.; Boriani, G.; et al. Clinical management of electrical storm. J. Cardiovasc. Med. 2021, 22, 669–679. [Google Scholar] [CrossRef] [PubMed]
- Guerra, F.; Stronati, G.; Capucci, A. Sedation in cardiac arrhythmias management. Expert Rev. Cardiovasc. Ther. 2018, 16, 163–173. [Google Scholar] [CrossRef]
- Perel, A. Non-anaesthesiologists should not be allowed to administer propofol for procedural sedation: A Consensus Statement of 21 European National Societies of Anaesthesia. Eur. J. Anaesthesiol. 2011, 28, 580–584. [Google Scholar] [CrossRef]
- Dumonceau, J.M.; Riphaus, A.; Aparicio, J.R.; Beilenhoff, U.; Knape, J.T.A.; Ortmann, M. NAAP Task Force Members. European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates, and the European Society of Anaesthesiology Guideline: Non-anaesthesiologist administration of propofol for GI endoscopy. Eur. J. Anaesthesiol. 2010, 27, 1016–1030. [Google Scholar]
- Morani, G.; Bergamini, C.; Angheben, C.; Pozzani, L.; Cicoira, M.; Tomasi, L.; Lanza, D.; Vassanelli, C. General anaesthesia for external electrical cardioversion of atrial fibrillation: Experience of an exclusively cardiological procedural management. Europace 2010, 12, 1558–1563. [Google Scholar] [CrossRef]
- Morani, G.; Borio, G.; Bolzan, B.; Ribichini, F.L. Safety and efficacy of a cardiologist-only approach to deep sedation for electrical cardioversion. J. Cardiovasc. Med. 2019, 20, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Salukhe, T.V.; Willems, S.; Drewitz, I.; Steven, D.; Hoffmann, B.A.; Heitmann, K.; Rostock, T. Propofol sedation administered by cardiologists without assisted ventilation for long cardiac interventions: An assessment of 1000 consecutive patients undergoing atrial fibrillation ablation. Europace 2011, 14, 325–330. [Google Scholar] [CrossRef]
- Servatius, H.S.; Willems, S.; A Hoffmann, B.; Steven, D.; Lüker, J.; Sultan, A.; Höfeler, T.; Schäffer, B. Propofol sedation administered by cardiologists for patients undergoing catheter ablation for ventricular tachycardia. Europace 2016, 18, 1245–1251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slupe, A.M.; Minnier, J.; Raitt, M.H.; Zarraga, I.G.E.; MacMurdy, K.S.; Jessel, P. Dexmedetomidine Sedation for Paroxysmal Supraventricular Tachycardia Ablation Is Not Associated With Alteration of Arrhythmia Inducibility. Anesth. Analg. 2019, 129, 1529–1535. [Google Scholar] [CrossRef]
- Cho, J.S.; Shim, J.-K.; Na, S.; Park, I.; Kwak, Y.L. Improved sedation with dexmedetomidine-remifentanil compared with midazolam-remifentanil during catheter ablation of atrial fibrillation: A randomized, controlled trial. Europace 2014, 16, 1000–1006. [Google Scholar] [CrossRef]
- Sairaku, A.; Yoshida, Y.; Hirayama, H.; Nakano, Y.; Ando, M.; Kihara, Y. Procedural sedation with dexmedetomidine during ablation of atrial fibrillation: A randomized controlled trial. Europace 2014, 16, 994–999. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-T.; Sun, C.-K.; Wu, K.-Y.; Chang, Y.-J.; Chiang, M.-H.; Chen, I.-W.; Liao, S.-W.; Hung, K.-C. The Use of Propofol versus Dexmedetomidine for Patients Receiving Drug-Induced Sleep Endoscopy: A Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2021, 10, 1585. [Google Scholar] [CrossRef] [PubMed]
- Kostroglou, A.; Kapetanakis, E.; Matsota, P.; Tomos, P.; Kostopanagiotou, K.; Tomos, I.; Siristatidis, C.; Papapanou, M.; Sidiropoulou, T. Monitored Anesthesia Care with Dexmedetomidine Supplemented by Midazolam/Fentanyl versus Midazolam/Fentanyl Alone in Patients Undergoing Pleuroscopy: Effect on Oxygenation and Respiratory Function. J. Clin. Med. 2021, 10, 3510. [Google Scholar] [CrossRef]
- Jeong, H.; Kim, D.; Kim, D.; Chung, I.; Bang, Y.; Kim, K.; Kim, M.; Choi, J. Comparison of Respiratory Effects between Dexmedetomidine and Propofol Sedation for Ultrasound-Guided Radiofrequency Ablation of Hepatic Neoplasm: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 3040. [Google Scholar] [CrossRef] [PubMed]
- Wutzler, A.; Rolf, S.; Huemer, M.; Parwani, A.S.; Boldt, L.-H.; Herberger, E.; Hohenbichler, K.; Dietz, R.; Haverkamp, W. Safety Aspects of Deep Sedation during Catheter Ablation of Atrial Fibrillation. Pacing Clin. Electrophysiol. 2012, 35, 38–43. [Google Scholar] [CrossRef]
- Wutzler, A.; Loehr, L.; Huemer, M.; Parwani, A.S.; Steinhagen-Thiessen, E.; Boldt, L.-H.; Haverkamp, W. Deep sedation during catheter ablation for atrial fibrillation in elderly patients. J. Interv. Card. Electrophysiol. 2013, 38, 115–121. [Google Scholar] [CrossRef]
- Kottkamp, H.; Hindricks, G.; Eitel, C.; Müller, K.; Siedziako, A.; Koch, J.; Anastasiou-Nana, M.; Varounis, C.; Arya, A.; Sommer, P.; et al. Deep Sedation for Catheter Ablation of Atrial Fibrillation: A Prospective Study in 650 Consecutive Patients. J. Cardiovasc. Electrophysiol. 2011, 22, 1339–1343. [Google Scholar] [CrossRef]
- Boriani, G.; Palmisano, P.; Guerra, F.; Bertini, M.; Zanotto, G.; Lavalle, C.; Notarstefano, P.; Accogli, M.; Bisignani, G.; Forleo, G.B.; et al. Impact of COVID-19 pandemic on the clinical activities related to arrhythmias and electrophysiology in Italy: Results of a survey promoted by AIAC (Italian Association of Arrhythmology and Cardiac Pacing). Intern. Emerg. Med. 2020, 15, 1445–1456. [Google Scholar] [CrossRef]
- Goudra, B.; Mason, K. Emerging Approaches in Intravenous Moderate and Deep Sedation. J. Clin. Med. 2021, 10, 1735. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palmisano, P.; Ziacchi, M.; Angeletti, A.; Guerra, F.; Forleo, G.B.; Bertini, M.; Notarstefano, P.; Accogli, M.; Lavalle, C.; Bisignani, G.; et al. The Practice of Deep Sedation in Electrophysiology and Cardiac Pacing Laboratories: Results of an Italian Survey Promoted by the AIAC (Italian Association of Arrhythmology and Cardiac Pacing). J. Clin. Med. 2021, 10, 5035. https://doi.org/10.3390/jcm10215035
Palmisano P, Ziacchi M, Angeletti A, Guerra F, Forleo GB, Bertini M, Notarstefano P, Accogli M, Lavalle C, Bisignani G, et al. The Practice of Deep Sedation in Electrophysiology and Cardiac Pacing Laboratories: Results of an Italian Survey Promoted by the AIAC (Italian Association of Arrhythmology and Cardiac Pacing). Journal of Clinical Medicine. 2021; 10(21):5035. https://doi.org/10.3390/jcm10215035
Chicago/Turabian StylePalmisano, Pietro, Matteo Ziacchi, Andrea Angeletti, Federico Guerra, Giovanni Battista Forleo, Matteo Bertini, Pasquale Notarstefano, Michele Accogli, Carlo Lavalle, Giovanni Bisignani, and et al. 2021. "The Practice of Deep Sedation in Electrophysiology and Cardiac Pacing Laboratories: Results of an Italian Survey Promoted by the AIAC (Italian Association of Arrhythmology and Cardiac Pacing)" Journal of Clinical Medicine 10, no. 21: 5035. https://doi.org/10.3390/jcm10215035
APA StylePalmisano, P., Ziacchi, M., Angeletti, A., Guerra, F., Forleo, G. B., Bertini, M., Notarstefano, P., Accogli, M., Lavalle, C., Bisignani, G., Landolina, M., Zanotto, G., D’Onofrio, A., Ricci, R. P., De Ponti, R., & Boriani, G., for AIAC Ricerca Investigators. (2021). The Practice of Deep Sedation in Electrophysiology and Cardiac Pacing Laboratories: Results of an Italian Survey Promoted by the AIAC (Italian Association of Arrhythmology and Cardiac Pacing). Journal of Clinical Medicine, 10(21), 5035. https://doi.org/10.3390/jcm10215035










