Autologous Fat Injection Laryngoplasty for Unilateral Vocal Fold Paralysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Data Sources
2.2. Study Selection Criteria
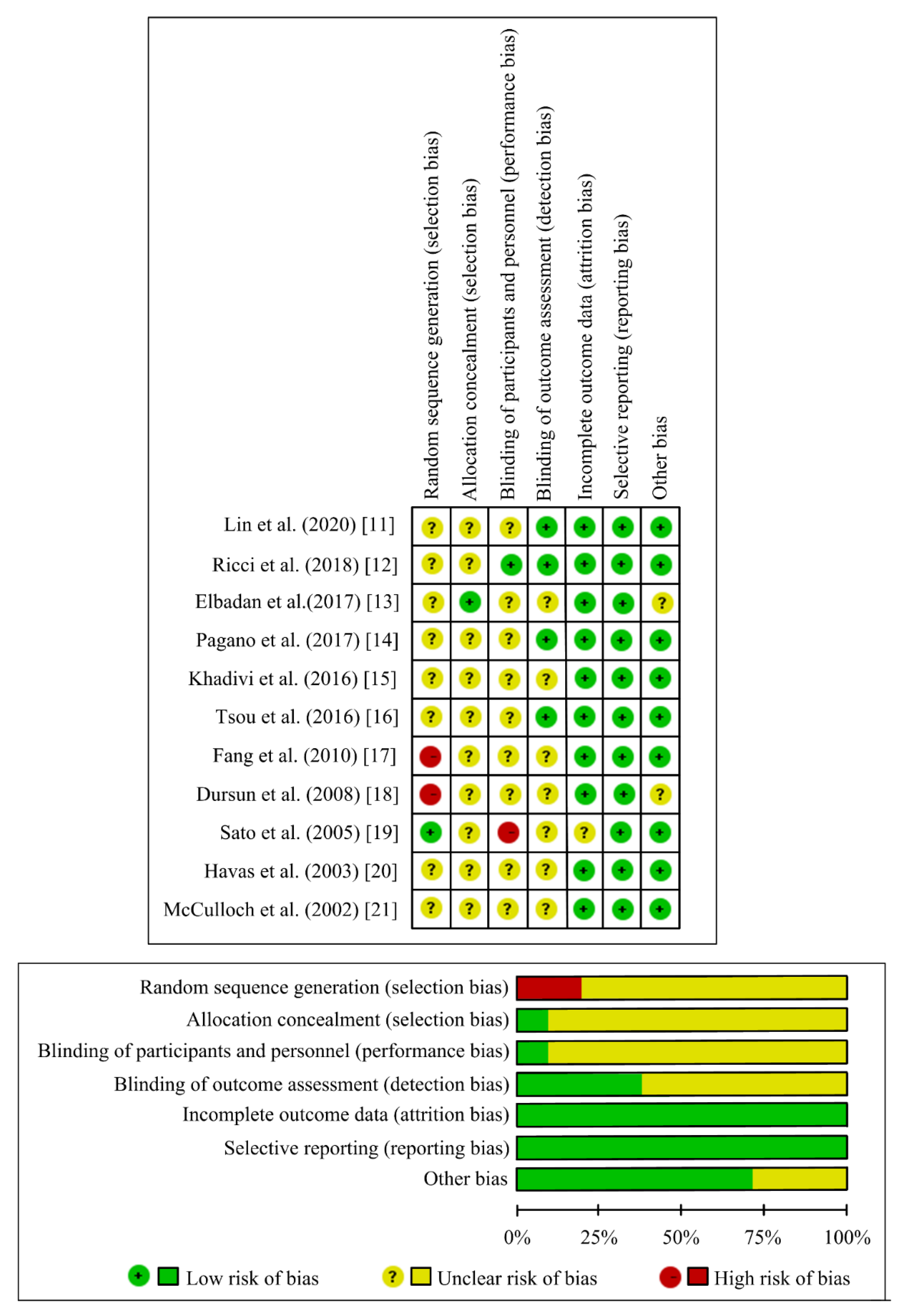
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Data Search Results
3.2. Study Characteristics
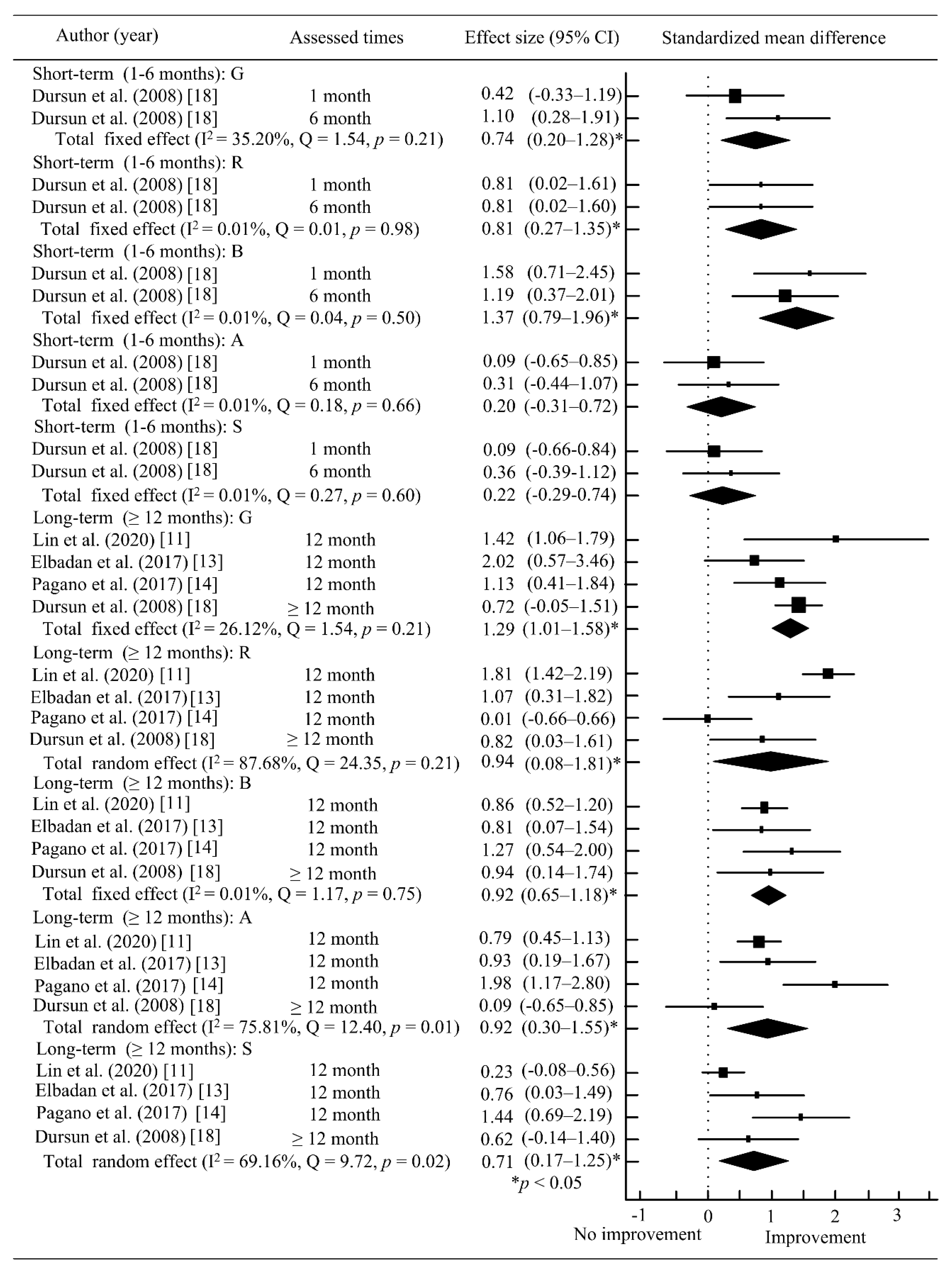
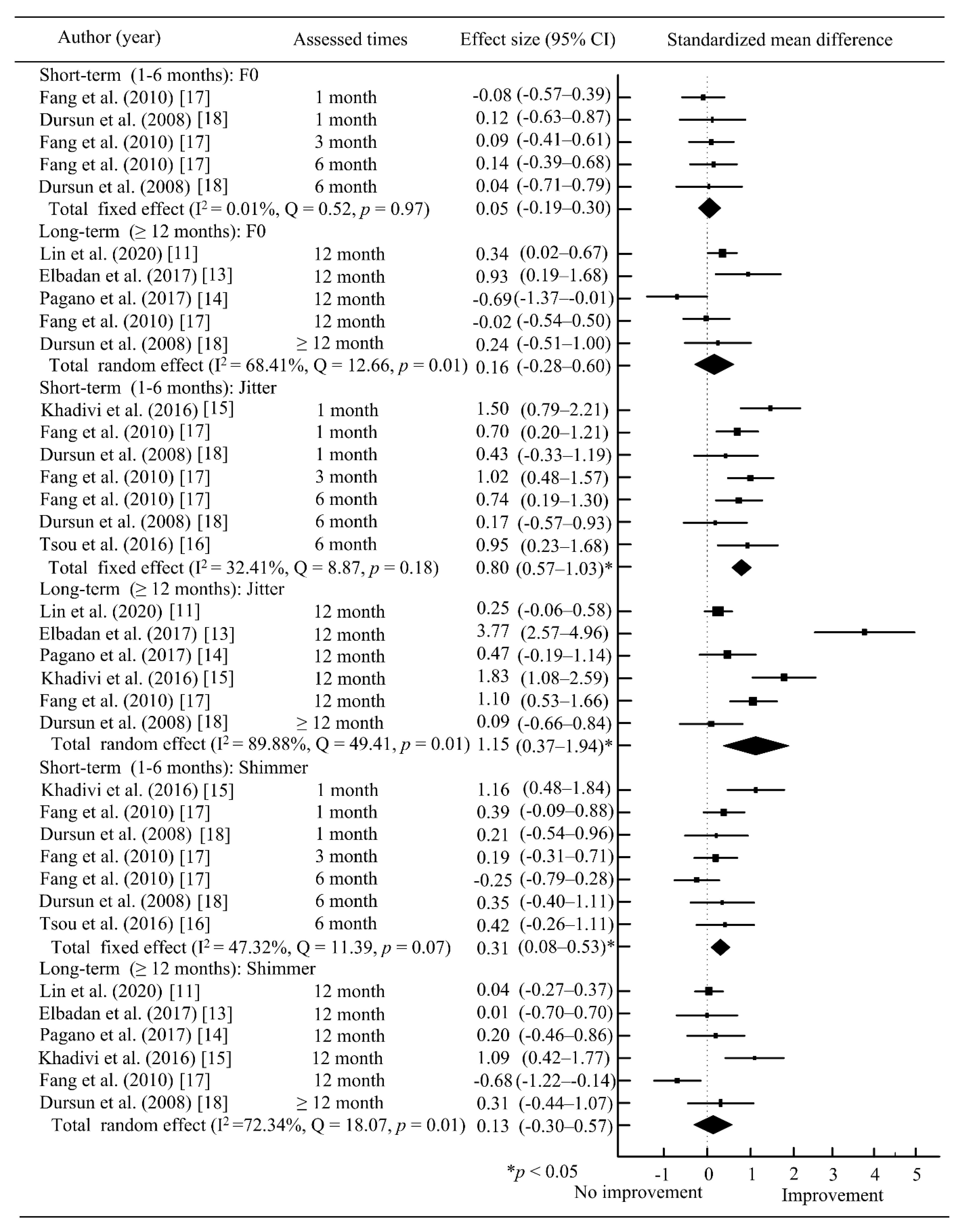
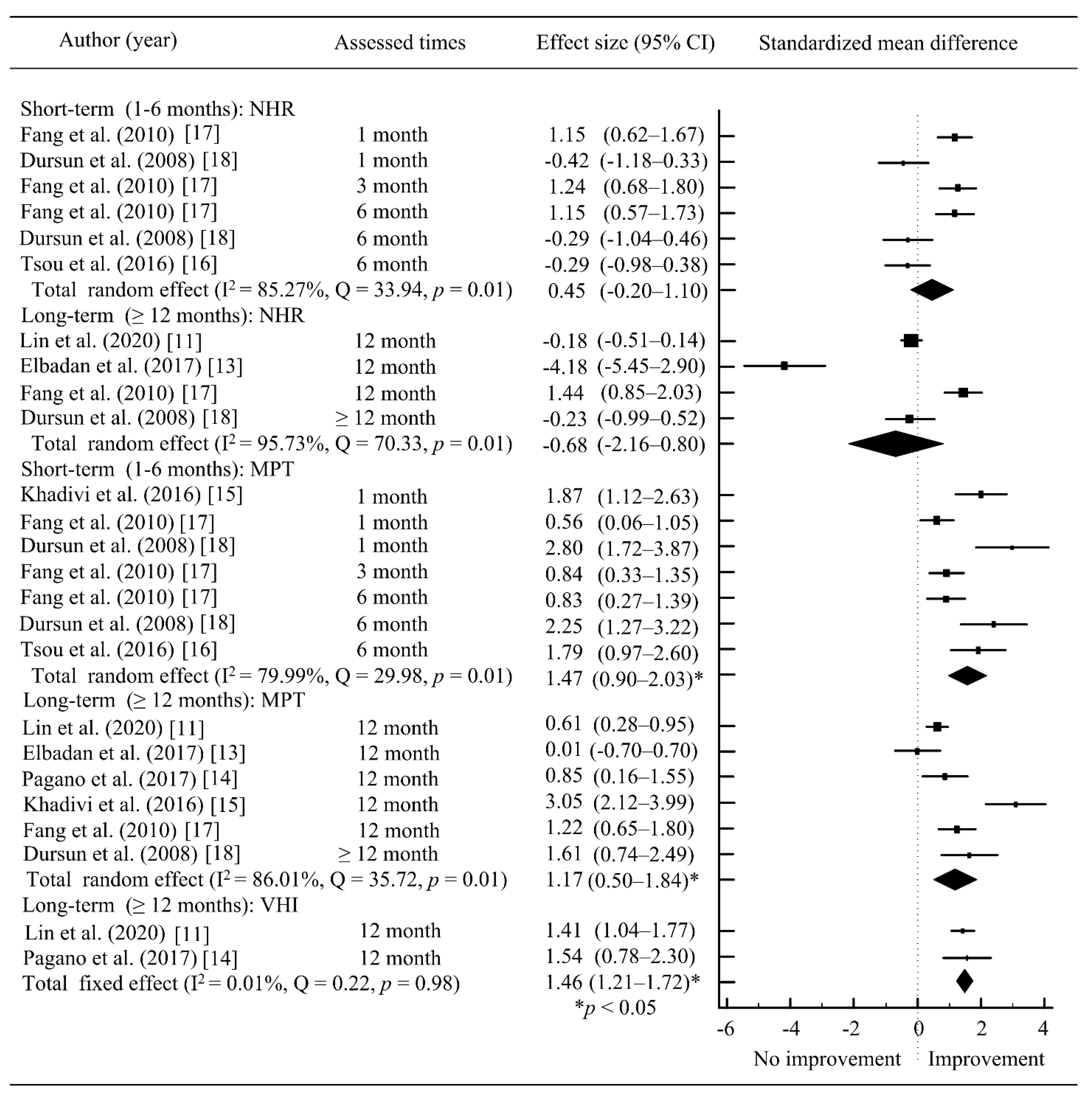
3.3. Study Outcomes
3.4. Outcomes of Meta-Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Schiedermayer, B.; Kendall, K.A.; Stevens, M.; Ou, Z.; Presson, A.P.; Barkmeier-Kraemer, J.M. Prevalence, incidence, and characteristics of dysphagia in those with unilateral vocal fold paralysis. Laryngoscope 2020, 130, 2397–2404. [Google Scholar] [CrossRef] [PubMed]
- Hartl, D.M.; Travagli, J.P.; Leboulleux, S.; Baudin, E.; Brasnu, D.F.; Schlumberger, M. Clinical review: Current concepts in the management of unilateral recurrent laryngeal nerve paralysis after thyroid surgery. J. Clin. Endocrinol. Metab. 2005, 90, 3084–3088. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Siu, J.; Tam, S.; Fung, K. A comparison of outcomes in interventions for unilateral vocal fold paralysis: A systematic review. Laryngoscope 2016, 126, 1616–1624. [Google Scholar] [CrossRef] [PubMed]
- Niemczyk, K. Injection laryngoplasty as mini-invasive office-based surgery in patients with unilateral vocal fold paralysis—Voice quality outcomes. Wideochir. Inne Tech. Maloinwazyjne. 2017, 12, 277–284. [Google Scholar]
- Daniero, J.; Garrett, C.G.; Francis, D.O. Framework Surgery for Treatment of Unilateral Vocal Fold Paralysis. Curr. Otorhinolaryngol. Rep. 2014, 2, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Marie, J.; Hansen, K.; Brami, P.; Marronnier, A.; Bon-Mardion, N. Nonselective Reinnervation as a Primary or Salvage Treatment of Unilateral Vocal Fold Palsy. Laryngoscope 2020, 130, 1756–1763. [Google Scholar] [CrossRef]
- Brunings, W. Uber eine neue behandlungsmethode der rekurrenslahmung. Verh. Ver. Laryngol. 1911, 18, 93–151. [Google Scholar]
- Kwon, T.-K.; Buckmire, R. Injection laryngoplasty for management of unilateral vocal fold paralysis. Curr. Opin. Otolaryngol. Head Neck Surg. 2004, 12, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Laccourreye, O.; Bély, N.; Crevier-Buchman, L.; Brasnu, D.; Halimi, P. Computerized tomography of the glottis after intracordal autologous fat injection. J. Laryngol. Otol. 1998, 112, 971–972. [Google Scholar] [CrossRef]
- Truzzi, G.M.; Pauna, H.F.; Bette, P.; Gusmão, R.J.; Crespo, A.N.; Semenzati, G.O. Methods of Fat Tissue Processing for Human Vocal Fold Injection: A Systematic Review. J. Voice 2017, 31, 244.e17–244.e21. [Google Scholar] [CrossRef]
- Lin, W.-Y.; Chang, W.-D.; Ko, L.-W.; Tsou, Y.-A.; Chen, S.-H. Impact of patient-related factors on successful autologous fat injection laryngoplasty in thyroid surgical treated related unilateral vocal fold paralysis-observational study. Medicine 2020, 99, e18579. [Google Scholar] [CrossRef]
- Ricci Maccarini, A.; Stacchini, M.; Mozzanica, F.; Schindler, A.; Basile, E.; De Rossi, G.; Woo, P.; Remacle, M.; Magnani, M. Efficacy of trans-nasal fiberendoscopic injection laryngoplasty with centrifuged autologous fat in the treatment of glottic insufficiency due to unilateral vocal fold paralysis. Acta. Otorhinolaryngol. Ital. 2018, 38, 204–213. [Google Scholar] [PubMed]
- Elbadan, H.E.M.; Hussein, W.K.A.; Elmaghraby, R.M. Transcervical fat injection laryngoplasty for unilateral vocal fold paralysis: An easy way to do the job. Eur. Arch. Oto-Rhino-Laryngol. 2017, 274, 4161–4167. [Google Scholar] [CrossRef]
- Pagano, R.; Morsomme, D.; Camby, S.; Lejeune, L.; Finck, C. Long-term Results of 18 Fat Injections in Unilateral Vocal Fold Paralysis. J. Voice 2017, 31, 505.e1–505.e9. [Google Scholar] [CrossRef]
- Khadivi, E.; Akbarian, M.; Khazaeni, K.; Salehi, M. Outcomes of Autologous Fat Injection Laryngoplasty in Unilateral Vocal Cord Paralysis. Iran. J. Otorhinolaryngol. 2016, 28, 215–219. [Google Scholar] [PubMed]
- Tsou, Y.-A.; Liu, Y.-W.; Chang, W.-D.; Chen, W.-C.; Ke, H.-C.; Lin, W.-Y.; Yang, H.-R.; Shie, D.-Y.; Tsai, M.-H. Using Innovative Acoustic Analysis to Predict the Postoperative Outcomes of Unilateral Vocal Fold Paralysis. BioMed Res. Int. 2016, 2016, 1–9. [Google Scholar] [CrossRef]
- Fang, T.-J.; Li, H.-Y.; Gliklich, R.E.; Chen, Y.-H.; Wang, P.-C.; Chuang, H.-F. Outcomes of Fat Injection Laryngoplasty in Unilateral Vocal Cord Paralysis. Arch. Otolaryngol.-Head Neck Surg. 2010, 136, 457–462. [Google Scholar] [CrossRef]
- Dursun, G.; Boynukalin, S.; Ozgursoy, O.B.; Coruh, I. Long-term results of different treatment modalities for glottic insufficiency. Am. J. Otolaryngol. 2008, 29, 7–12. [Google Scholar] [CrossRef]
- Sato, K.; Umeno, H.; Nakashima, T. Histological investigation of liposuctioned fat for injection laryngoplasty. Am. J. Otolaryngol. 2005, 26, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Havas, T.E.; Priestley, K.J. Autologous Fat Injection Laryngoplasty for Unilateral Vocal Fold Paralysis. ANZ J. Surg. 2003, 73, 938–943. [Google Scholar] [CrossRef]
- McCulloch, T.M.; Andrews, B.T.; Hoffman, H.T.; Graham, S.M.; Karnell, M.P.; Minnick, C. Long-Term Follow-up of Fat Injection Laryngoplasty for Unilateral Vocal Cord Paralysis. Laryngoscope 2002, 112, 1235–1238. [Google Scholar] [CrossRef] [PubMed]
- Fancello, V.; Nouraei, S.A.R.; Heathcote, K.J. Role of reinnervation in the management of recurrent laryngeal nerve injury: Current state and advances. Curr. Opin. Otolaryngol. Head Neck Surg. 2017, 25, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Cantarella, G.; Dejonckere, P.; Galli, A.; Ciabatta, A.; Gaffuri, M.; Pignataro, L.; Torretta, S. A retrospective evaluation of the etiology of unilateral vocal fold paralysis over the last 25 years. Eur. Arch. Oto-Rhino-Laryngol. 2017, 274, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Ha, J.F. Unilateral vocal fold palsy & dysphagia: A review. Auris Nasus Larynx 2020, 47, 315–334. [Google Scholar] [CrossRef] [PubMed]
- Vila, P.M.; Bhatt, N.K.; Paniello, R.C. Early-injection laryngoplasty may lower risk of thyroplasty: A systematic review and meta-analysis. Laryngoscope 2018, 128, 935–940. [Google Scholar] [CrossRef] [PubMed]
- Courey, M.S. Injection laryngoplasty. Otolaryngol. Clin. N. Am. 2004, 37, 121–138. [Google Scholar] [CrossRef]
- Lewy, R.B. Experience with Vocal Cord Injection. Ann. Otol. Rhinol. Laryngol. 1976, 85, 440–450. [Google Scholar] [CrossRef]
- Shen, T.; Damrose, E.; Morzaria, S. A Meta-analysis of Voice Outcome Comparing Calcium Hydroxylapatite Injection Laryngoplasty to Silicone Thyroplasty. Otolaryngol. Neck Surg. 2012, 148, 197–208. [Google Scholar] [CrossRef] [PubMed]
- Remacle, M.J.M.; Marbaix, E.; Bertrand, B.M.G. The value of injectable collagen in vocal and glottic rehabilitation. Eur. Arch. Oto-Rhino-Laryngol. 1986, 243, 233–237. [Google Scholar] [CrossRef]
- Mallur, P.S.; Rosen, C.A. Vocal Fold Injection: Review of Indications, Techniques, and Materials for Augmentation. Clin. Exp. Otorhinolaryngol. 2010, 3, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Trinh, L.N.; Gupta, A. Non-Hyaluronic Acid Fillers for Midface Augmentation: A Systematic Review. Facial Plast. Surg. 2021. [Google Scholar] [CrossRef]
- Chiu, F.-S.; Lin, Y.-S.; Chang, Y.-N.; Lee, J.-C. Umbilical Hernia—A Potential Donor-Site Complication of Fat Injection Laryngoplasty. J. Voice 2012, 26, 818.e15–818.e17. [Google Scholar] [CrossRef]
- Anderson, T.D.; Sataloff, R.T. Complications of collagen injection of the vocal fold: Report of several unusual cases and review of the literature. J. Voice 2004, 18, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Enver, N.; Asya, O.; Abuzaid, G.; Gürol, E. A Very Rare Complication of Hyaluronic Acid Injection for Medialization Laryngoplasty: A Case with Laryngeal Abscess. J. Voice 2020, 34, 812.e5–812.e8. [Google Scholar] [CrossRef] [PubMed]
- Madgar, O.; Primov-Fever, A. A Very Rare Complication of Vocal Fold Augmentation with Calcium Hydroxylapatite: Neck Abscess. J. Voice 2020, S0892-1997, 30404–30409. [Google Scholar] [CrossRef]
- Zapanta, P.E.; Bielamowicz, S.A. Laryngeal Abscess after Injection Laryngoplasty with Micronized AlloDerm. Laryngoscope 2004, 114, 1522–1524. [Google Scholar] [CrossRef] [PubMed]
- Óvári, A.; Witt, G.; Schuldt, T.; Hingst, V.; Pau, H.-W.; Jäckel, M.; Dommerich, S. Polydimethylsiloxane for injection laryngoplasty: Two cases necessitating tracheotomy. Eur. Arch. Oto-Rhino-Laryngol. 2014, 271, 839–844. [Google Scholar] [CrossRef]
- Rosen, C.A.; Amin, M.R.; Sulica, L.; Simpson, C.B.; Merati, A.L.; Courey, M.S.; Johns, M.M., 3rd; Postma, G.N. Advances in office-based diagnosis and treatment in laryngology. Laryngoscope 2009, 119, 185–212. [Google Scholar] [CrossRef] [PubMed]
- Granato, F.; Martelli, F.; Comini, L.V.; Luparello, P.; Coscarelli, S.; Le Seac, O.; Carucci, S.; Graziani, P.; Santoro, R.; Alderotti, G.; et al. The surgical treatment of unilateral vocal cord paralysis (UVCP): Qualitative review analysis and meta-analysis study. Eur. Arch. Oto-Rhino-Laryngol. 2019, 276, 2649–2659. [Google Scholar] [CrossRef]
- Lasso, J.M.; Poletti, D.; Scola, B.; Gómez-Vilda, P.; García-Martín, A.I.; Fernández-Santos, M.E. Injection Laryngoplasty Using Autologous Fat Enriched with Adipose-Derived Regenerative Stem Cells: A Safe Therapeutic Option for the Functional Reconstruction of the Glottal Gap after Unilateral Vocal Fold Paralysis. Stem Cells Int. 2018, 2018, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ladosky, W.; Wandscheer, D. Interaction between estrogen and biogenic amines in the control of LH secretion. J. Steroid Biochem. 1975, 6, 1013–1020. [Google Scholar] [CrossRef]

| Author (Years) | Study Designs | Patients (n) | Anesthesia | Fat Harvesting Site | Injection Preparation | Preparation Volume | Injection Approach | Injection Guidance |
|---|---|---|---|---|---|---|---|---|
| Lin et al. (2020) [11] | Prospective study | 73 | General | Abdomen | Saline washing | 2 mL | Trans-oral | Rigid suspension laryngoscope |
| Ricci et al. (2018) [12] | Prospective study | 22 | Local | Abdomen | Concentration (3000 rpm for 3 min) | 3 mL | Trans-cutaneous | Flexible endoscope |
| Elbadan et al. (2017) [13] | Retrospective study | 16 | General | Abdomen | Saline washing and survive use of insulin (100 units) | 5 mL | Trans-cutaneous | Laryngoscope |
| Pagano et al. (2017) [14] | Retrospective study | 18 | General | Abdomen or thigh | Concentration (3 min) | 1 mL | Trans-cutaneous | Surgical microscope |
| Khadivi et al. (2016) [15] | Prospective study | 20 | General | Abdomen | Concentration (2000 rpm for 4 min) | 2 mL | Trans-cutaneous | Rigid suspension laryngoscope |
| Tsou et al. (2016) [16] | Prospective study | 17 | General | Abdomen | Saline washing and survive use of insulin (10 mL) | 1.5–2 mL | Trans-oral | Rigid suspension laryngoscope |
| Fang et al. (2010) [17] | Prospective study | 33 | Local | Abdomen | Saline washing | 0.5–2 mL | Trans-cutaneous | Rigid suspension laryngoscope |
| Dursun et al. (2008) [18] | Prospective study | 30 | NA | NA | NA | NA | NA | NA |
| Sato et al. (2005) [19] | Prospective study | 13 | NA | Abdomen | Saline washing and antibiotics | 2 mL | NA | NA |
| Havas et al. (2003) [20] | Prospective study | 45 | Local | Abdomen | NA | 0.3–0.9 mL | NA | NA |
| McCulloch et al. (2002) [21] | Retrospective study | 50 | NA | Abdomen | NA | NA | NA | NA |
| Author (Years) | Assessments | Assessment Times | Outcomes | ||
|---|---|---|---|---|---|
| Perceptual | Acoustic Analysis | Quality of Life | |||
| Lin et al. (2020) [11] | GRBAS | F0, Jitter, Shimmer, NHR, VTI, SPI | VHI-10 | Pre- and post-operation 12 month | Significant improved in GRBAS * and some voice parameters * at 12 month |
| Ricci et al. (2018) [12] | GRBAS | MPT | VHI-10 | Pre- and post-operation 1 week and 6 month | Significant improved in GRBAS * MPT and VHI-10 * at 1 week and 12 month |
| Elbadan et al. (2017) [13] | GRBAS | F0, Jitter, Shimmer, NHR, MPT, MFR, Psub | nil | Pre- and post-operation 12 month | Significant improved in GRBAS * and voice parameters * at 12 month |
| Pagano et al. (2017) [14] | GRBAS | F0, MPT, Jitter, Shimmer, MFR, lowest and highest intensity, ADSI | VHI | Pre-, post-operation immediately and 12 month | Significant improved in GRBAS *, some voice parameters * and VHI after operation |
| Khadivi et al. (2016) [15] | nil | MPT, Jitter, Shimmer | nil | Pre-, post-operation 1, and ≥12 months | Significant improved in voice parameters * post-operation ≥ 12 month |
| Tsou et al. (2016) [16] | GRBAS | F0, Jitter, Shimmer, NHR, MPT | nil | Pre- and post-operation 6 month | Significant improved in some voice parameters * at 6 month |
| Fang et al. (2010) [17] | nil | F0, Jitter, Shimmer, NHR, MPT, SZ ratio | nil | Pre-, post-operation 1, 3, 6, and 12 months | Significant improved in voice parameters * at 12 month |
| Dursun et al. (2008) [18] | GRBAS | F0, Jitter, Shimmer, NHR, MPT | nil | Pre-, post-operation 1, 6, and ≥12 months | Significant improved in GRBAS * and voice parameters * after 1, 6, and ≥12 months |
| Sato et al. (2005) [19] | nil | MPT, MFR | nil | Post-operation ≥ 6 month | nil |
| Havas et al. (2003) [20] | nil | MPT, Sydney Voice Clinic voice dysfunction rating scale | nil | 2 month–8 years | nil |
| McCulloch et al. (2002) [21] | GRBAS | nil | nil | Pre-, post-operation ≥ 6 month | nil |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, W.-D.; Chen, S.-H.; Tsai, M.-H.; Tsou, Y.-A. Autologous Fat Injection Laryngoplasty for Unilateral Vocal Fold Paralysis. J. Clin. Med. 2021, 10, 5034. https://doi.org/10.3390/jcm10215034
Chang W-D, Chen S-H, Tsai M-H, Tsou Y-A. Autologous Fat Injection Laryngoplasty for Unilateral Vocal Fold Paralysis. Journal of Clinical Medicine. 2021; 10(21):5034. https://doi.org/10.3390/jcm10215034
Chicago/Turabian StyleChang, Wen-Dien, Sheng-Hwa Chen, Ming-Hsui Tsai, and Yung-An Tsou. 2021. "Autologous Fat Injection Laryngoplasty for Unilateral Vocal Fold Paralysis" Journal of Clinical Medicine 10, no. 21: 5034. https://doi.org/10.3390/jcm10215034
APA StyleChang, W.-D., Chen, S.-H., Tsai, M.-H., & Tsou, Y.-A. (2021). Autologous Fat Injection Laryngoplasty for Unilateral Vocal Fold Paralysis. Journal of Clinical Medicine, 10(21), 5034. https://doi.org/10.3390/jcm10215034






