Association between Intraoperative Blood Pressure Drop and Clinically Significant Hypoperfusion in Abdominal Surgery: A Cohort Study
Abstract
:1. Background
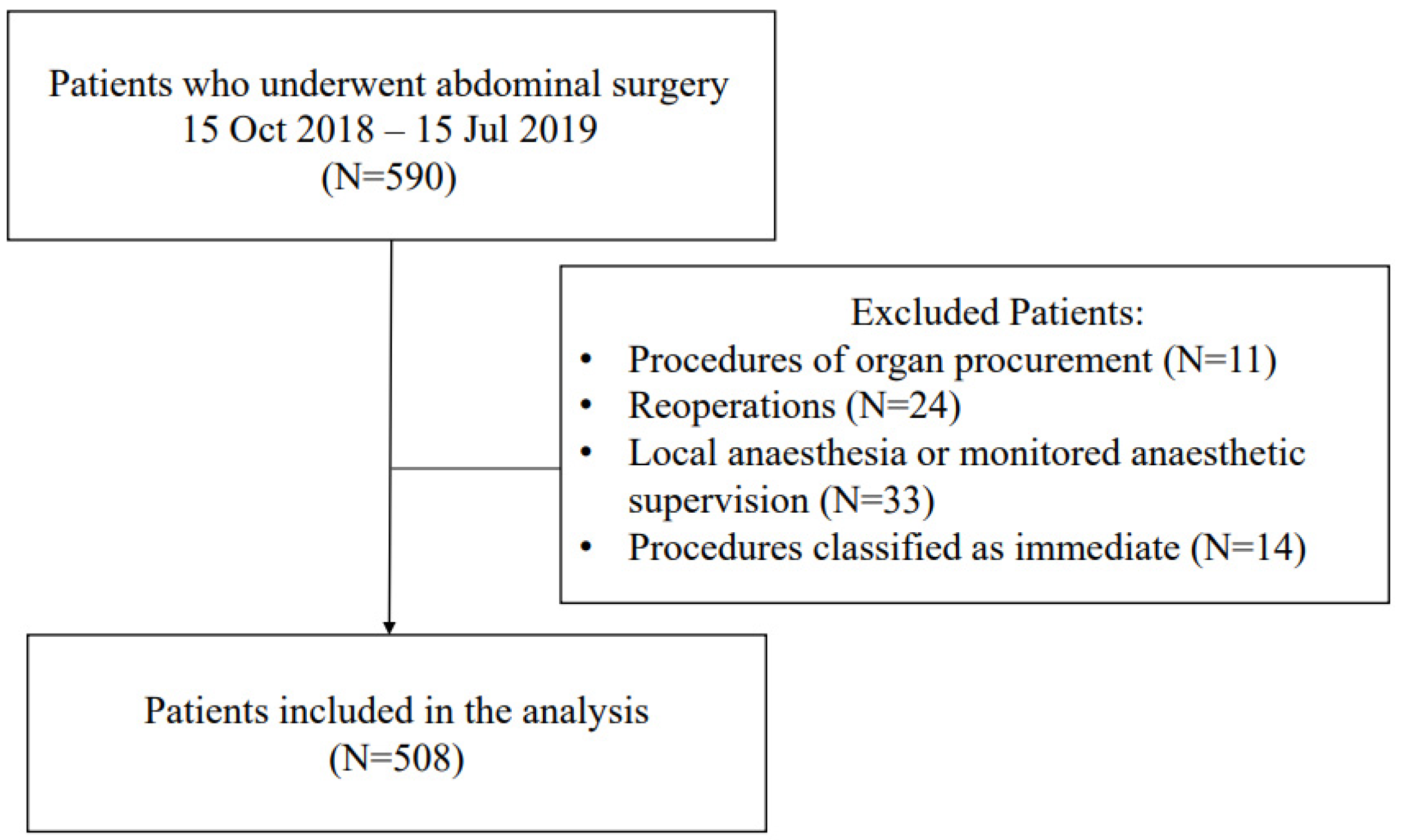
2. Methods
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bijker, J.B.; van Klei, W.A.; Vergouwe, Y.; Eleveld, D.J.; van Wolfswinkel, L.; Moons, K.G.; Kalkman, C.J. Intraoperative hypotension and 1-year mortality after noncardiac surgery. Anesthesiology 2009, 111, 1217–1226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ke, J.X.C.; George, R.B.; Beattie, W.S. Making sense of the impact of intraoperative hypotension: From populations to the individual patient. Br. J. Anaesth. 2018, 121, 689–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Devereaux, P.J.; Yang, H.; Yusuf, S.; Guyatt, G.; Leslie, K.; Villar, J.C.; Xavier, D.; Chrolavicius, S.; Greenspan, L.; Pogue, J.; et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): A randomised controlled trial. Lancet 2008, 371, 1839–1847. [Google Scholar] [PubMed] [Green Version]
- Sessler, D.I.; Bloomstone, J.A.; Aronson, S.; Berry, C.; Gan, T.J.; Kellum, J.A.; Plumb, J.; Mythen, M.G.; Grocott, M.P.; Edwards, M.R.; et al. Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br. J. Anaesth. 2019, 122, 563–574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mascha, E.J.; Yang, D.; Weiss, S.; Sessler, D.I. Intraoperative Mean Arterial Pressure Variability and 30-day Mortality in Patients Having Noncardiac Surgery. Anesthesiology 2015, 123, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Devereaux, P.J.; Garg, A.X.; Kurz, A.; Turan, A.; Rodseth, R.N.; Cywinski, J.; Thabane, L.; Sessler, D.I. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: Toward an empirical definition of hypotension. Anesthesiology 2013, 119, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Monk, T.G.; Bronsert, M.R.; Henderson, W.G.; Mangione, M.P.; Sum-Ping, S.T.J.; Bentt, D.R.; Nguyen, J.D.; Richman, J.S.; Meguid, R.A.; Hammermeister, K.E. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology 2015, 123, 307–319. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.Y.; Wijeysundera, D.N.; Tait, G.A.; Beattie, W.S. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology 2015, 123, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Van Waes, J.A.R.; Van Klei, W.A.; Wijeysundera, D.N.; Van Wolfswinkel, L.; Lindsay, T.F.; Beattie, W.S. Association between intraoperative hypotension and myocardial injury after vascular surgery. Anesthesiology 2016, 124, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Salmasi, V.; Maheshwari, K.; Yang, D.; Mascha, E.J.; Singh, A.; Sessler, D.I.; Kurz, A. Relationship between Intraoperative Hypotension, Defined by Either Reduction from Baseline or Absolute Thresholds, and Acute Kidney and Myocardial Injury after Noncardiac Surgery: A Retrospective Cohort Analysis. Anesthesiology 2017, 126, 47–65. [Google Scholar] [CrossRef] [PubMed]
- National Confidential Enquiry into Patient Outcome and Death. n.d. Available online: www.ncepod.org.uk/classification.html (accessed on 17 October 2020).
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- World Health Organization. International Classification of Diseases: [9th] Ninth Revision, Basic Tabulation List with Alphabetic Index; WHO: Geneva, Switzerland, 1978; 331p. [Google Scholar]
- Doyle, D.J.; Goyal, A.; Bansal, P.; Garmon, E.H. American Society of Anesthesiologists Classification (ASA Class). 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK441940/ (accessed on 17 October 2020).
- Kristensen, S.D.; Knuuti, J.; Saraste, A.; Anker, S.; Bøtker, H.E.; De Hert, S.; Ford, I.; Gonzalez-Juanate, J.R.; Gorene, B.; Heyndrickx, G.R.; et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: Cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: Cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesth. Eur. Heart J. 2014, 35, 2383–2431. [Google Scholar] [PubMed] [Green Version]
- Kellum, J.A.; Lameire, N.; Aspelin, P.; Barsoum, R.S.; Burdmann, E.A.; Goldstein, S.L.; Herzog, C.A.; Joannidis, M.; Kribben, A.; Levey, A.S.; et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. 2012, 2, 1–138. [Google Scholar]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; ESC Scientific Document Group; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef] [Green Version]
- Ringleb, P.; Bousser, M.; Ford, G.; Bath, P.; Brainin, M.; Caso, V.; Cervera, Á.; Chamorro, A.; Cordonnie, C.; Csiba, L.; et al. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008 the European Stroke Organization (ESO) Committee and the ESO Writing Committee Executive. Stroke 2008, 25, 6855–6859. [Google Scholar]
- Wesselink, E.M.; Kappen, T.H.; Torn, H.M.; Slooter, A.J.C.; van Klei, W.A. Intraoperative hypotension and the risk of postoperative adverse outcomes: A systematic review. Br. J. Anaesth. 2018, 121, 706–721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosner, M.H.; Perazella, M.A. Acute Kidney Injury in Patients with Cancer. N. Engl. J. Med. 2017, 376, 1770–1781. [Google Scholar] [CrossRef] [PubMed]
- Jang, W.Y.; Jung, J.K.; Lee, D.K.; Han, S.B. Intraoperative hypotension is a risk factor for postoperative acute kidney injury after femoral neck fracture surgery: A retrospective study. BMC Musculoskelet. Disord. 2019, 20, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schonberger, R.B.; Nwozuzu, A.; Zafar, J.; Chen, E.; Kigwana, S.; Monteiro, M.M.; Charchaflieh, J.; Sophanphattana, S.; Dai, F.; Burg, M.M. Elevated preoperative blood pressures in adult surgical patients are highly predictive of elevated home blood pressures. J. Am. Soc. Hypertens. 2018, 12, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Mathis, M.R.; Naik, B.I.; Freundlich, R.E.; Shanks, A.M.; Heung, M.; Kim, M.; Burns, M.L.; Colquhoun, D.A.; Rangrass, G.; Janda, A.; et al. Preoperative Risk and the Association between Hypotension and Postoperative Acute Kidney Injury. Anesthesiology 2020, 132, 461–475. [Google Scholar] [CrossRef] [PubMed]
| Variable | Outcome (−) n = 470 | Outcome (+) n = 38 | p-Value |
|---|---|---|---|
| Age (years) | 61 (45–68) | 67 (62–75) | 0.0002 |
| Males | 219 (46.6) | 20 (52.6) | 0.4 |
| BMI (kg m−2) | 25.6 (22.5–29.0) | 27.1 (21.9–29.8) | 0.4 |
| Chronic arterial hypertension | 205 (43.6) | 29 (76.3) | <0.0001 |
| Chronic Kidney Disease | 8 (1.7) | 5 (38.5) | <0.0001 |
| Diabetes mellitus | 57 (12.1) | 4 (10.5) | 0.8 |
| Pre-induction SBP (mmHg) | 140 (125–153) | 142.5 (130–155) | 0.2 |
| Pre-induction MAP (mmHg) | 101.7 (92.0-110.0) | 101.5 (95.0–110.0) | 0.6 |
| ACEI/ARB | 97 (20.6) | 13 (34.2) | 0.05 |
| B-blocker | 118 (25.1) | 15 (39.5) | 0.05 |
| Calcium antagonist | 39 (8.3) | 4 (10.5) | 0.6 |
| ASA PS class III/IV/V | 189 (40.2) | 26 (68.4) | 0.0007 |
| CCI (pts) | 3 (1–5) | 5 (3–7) | <0.0001 |
| Premedication | 284 (60.4) | 21 (55.3) | 0.5 |
| Variable | Outcome (−) n = 470 | Outcome (+) n = 38 | p-Value |
|---|---|---|---|
| Adjunction of regional anaesthesia (number of cases) | 31 (6.6) | 9 (23.7) | 0.0002 |
| Invasive blood pressure monitoring (number of cases) | 67 (14.7) | 14 (36.8) | 0.0004 |
| Procedure Risk I * | 44 (9.4) | 1 (2.6) | 0.1 |
| Procedure Risk II * | 314 (66.8) | 21 (55.3) | 0.1 |
| Procedure Risk III * | 112 (23.8) | 16 (42.1) | 0.01 |
| Oncological procedure (number of cases) | 219 (46.6) | 26 (68.4) | 0.009 |
| Catecholamine use (number of cases) | 197 (41.9) | 30 (78.9) | <0.0001 |
| Time of catecholamine administration from the induction of anaesthesia (min) | 40.0 (20.0–80.0) | 37.5 (15.0–60.0) | 0.4 |
| Catecholamine dose (µg kg−1 min−1) | 0.054 (0.042–0.090) | 0.070 (0.048–0.091) | 0.3 |
| Procedure duration (min) | 215.0 (120.0–330.0) | 372.5 (235.0–492.0) | <0.0001 |
| Fluid dose (mL kg−1 h−1) | 6.78 (5.16–8.76) | 6.67 4.74–8.58) | 0.5 |
| Threshold | Outcome (−) n = 470 | Outcome (+) n = 38 | p-Value |
|---|---|---|---|
| <55 mmHg | 44 (9.4) | 10 (26.3) | 0.001 |
| <60 mmHg | 107 (22.9) | 17 (44.7) | 0.002 |
| <65 mmHg | 218 (46.4) | 26 (68.4) | 0.009 |
| <70 mmHg | 345 (73.4) | 29 (76.3) | 0.6 |
| <75 mmHg | 412 (88.0) | 35 (92.1) | 0.4 |
| Drop > 20% from baseline | 432 (91.9) | 35 (92.1) | 0.9 |
| Drop > 25% from baseline | 391 (83.2) | 33 (86.8) | 0.5 |
| Drop > 30% from baseline | 319 (67.9) | 31 (81.6) | 0.07 |
| Drop > 35% from baseline | 243 (51.7) | 25 (65.8) | 0.09 |
| Drop > 40% from baseline | 162 (34.5) | 23 (60.5) | 0.001 |
| Threshold | Outcome (−) n = 470 | Outcome (+) n = 38 | Best Cut-Off Threshold in Predicting Outcome (+) | p-Value |
|---|---|---|---|---|
| <55 mmHg | 0 (0–0) | 0 (0–1) | >0 | 0.001 |
| <60 mmHg | 0 (0–0) | 0 (0–2) | >0 | 0.0009 |
| <65 mmHg | 0 (0–2) | 2 (0–3) | >1 | 0.003 |
| <70 mmHg | 2 (0–6) | 6 (1–16) | >4 | 0.01 |
| <75 mmHg | 7 (2–13) | 13 (3–29) | >17 | 0.005 |
| Drop > 20% from baseline | 15 (5–32) | 29 (9–55) | >27 | 0.006 |
| Drop > 25% from baseline | 9 (1–19) | 16 (3–36) | >20 | 0.04 |
| Drop > 30% from baseline | 3 (0–10) | 5 (1–19) | >2 | 0.03 |
| Drop > 35% from baseline | 1 (0–3) | 2 (0–6) | >4 | 0.04 |
| Drop > 40% from baseline | 0 (0–1) | 1 (0–3) | >0 | 0.001 |
| Model | OR (95% CI) | p-Value |
|---|---|---|
| >0 episodes of MAP < 55 mmHg | 2.56 (1.05–6.26) | 0.039 |
| >0 episodes of MAP < 60 mmHg | 2.61 (1.22–5.59) | 0.01 |
| >1 episodes of MAP < 65 mmHg | 2.50 (1.17–5.30) | 0.017 |
| >4 episodes of MAP < 70 mmHg | 2.67 (1.26–5.67) | 0.01 |
| >17 episodes of MAP < 75 mmHg | * | * |
| >27 episodes of MAP drop > 20% from baseline | * | * |
| >20 episodes of MAP drop > 25% from baseline | * | * |
| >2 episodes of MAP drop > 30% from baseline | * | * |
| >4 episodes of MAP drop > 35% from baseline | * | * |
| >0 episodes of MAP drop > 40% from baseline | * | * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Putowski, Z.; Czajka, S.; Krzych, Ł.J. Association between Intraoperative Blood Pressure Drop and Clinically Significant Hypoperfusion in Abdominal Surgery: A Cohort Study. J. Clin. Med. 2021, 10, 5010. https://doi.org/10.3390/jcm10215010
Putowski Z, Czajka S, Krzych ŁJ. Association between Intraoperative Blood Pressure Drop and Clinically Significant Hypoperfusion in Abdominal Surgery: A Cohort Study. Journal of Clinical Medicine. 2021; 10(21):5010. https://doi.org/10.3390/jcm10215010
Chicago/Turabian StylePutowski, Zbigniew, Szymon Czajka, and Łukasz J. Krzych. 2021. "Association between Intraoperative Blood Pressure Drop and Clinically Significant Hypoperfusion in Abdominal Surgery: A Cohort Study" Journal of Clinical Medicine 10, no. 21: 5010. https://doi.org/10.3390/jcm10215010
APA StylePutowski, Z., Czajka, S., & Krzych, Ł. J. (2021). Association between Intraoperative Blood Pressure Drop and Clinically Significant Hypoperfusion in Abdominal Surgery: A Cohort Study. Journal of Clinical Medicine, 10(21), 5010. https://doi.org/10.3390/jcm10215010







