Respiratory Monitoring at Bedside in COVID-19 Patients
Abstract
1. Introduction
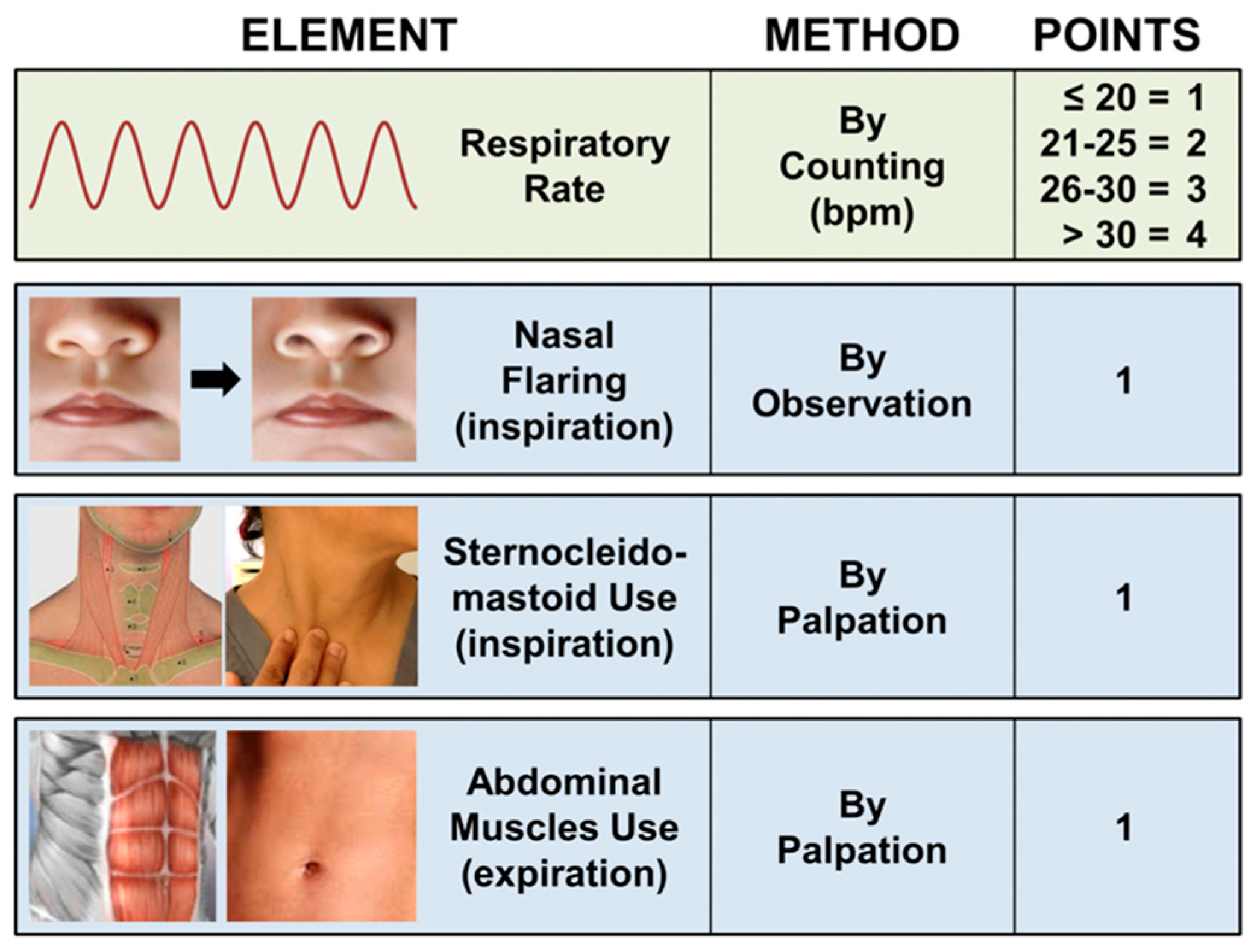
2. Clinical Evaluation
3. Pressure Assessment
4. Volumetric Assessment
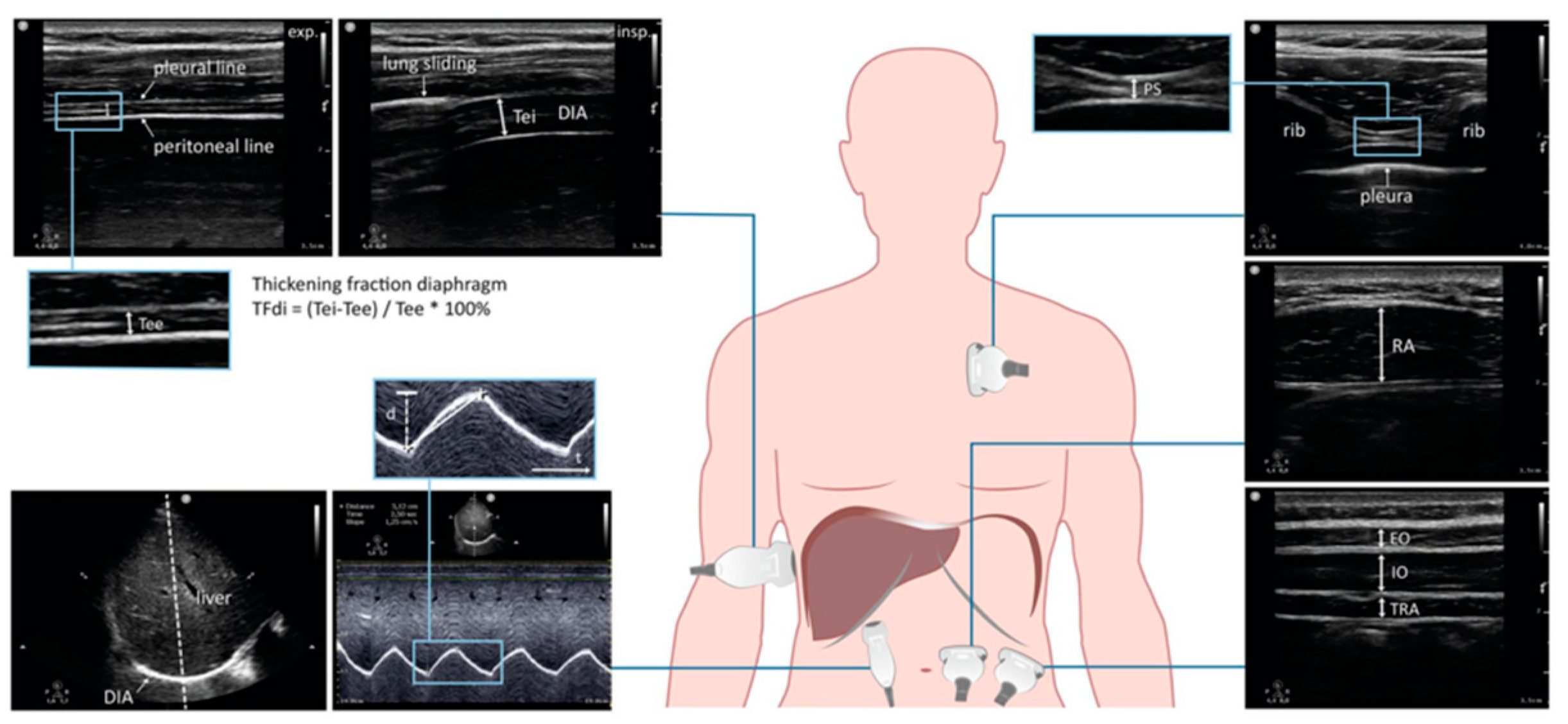
5. Ultrasound Evaluation
6. Discussion
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Disease Outbreak News: Pneumonia of Unknow Case-China. Available online: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ (accessed on 10 July 2020).
- WHO. Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is Suspected: Interim Guidance V.1.2. 2020. Available online: https://apps.who.int/iris/handle/10665/331446 (accessed on 18 March 2020).
- Paglia, S.; Storti, E.; Bisagni, P.; Ferrari, P.; Manelli, A.; Delfanti, F.; Delfanti, F.; Mainardi, C.; Martinenghi, S.; CÒ, F.M.; et al. Lodi’s experience in handling the first COVID-19 hotbed in Europe. Int. J. Emerg. Med. 2020, 9, 93–101. [Google Scholar] [CrossRef]
- Rello, J.; Storti, E.; Belliato, M.; Serrano, R. Clinical phenotypes of SARS-CoV-2: Implications for clinicians and researchers. Eur. Respir. J. 2020, 55, 2001028. [Google Scholar] [CrossRef] [PubMed]
- Marini, J.J.; Gattinoni, L. Management of COVID-19 Respiratory Distress. JAMA 2020, 323, 2329–2330. [Google Scholar] [CrossRef] [PubMed]
- Alhazzani, W.; Evans, L.; Alshamsi, F.; Møller, M.H.; Ostermann, M.; Prescott, H.C.; Arabi, Y.M.; Loeb, M.; Ng Gong, M.; Fan, E.; et al. Surviving Sepsis Campaign Guidelines on the Management of Adults with Coronavirus Disease 2019 (COVID-19) in the ICU: First Update. Crit. Care Med. 2021, 49, e219–e234. [Google Scholar] [CrossRef] [PubMed]
- Brochard, L.; Slutsky, A.; Pesenti, A. Mechanical Ventilation to Minimize Progression of Lung Injury in Acute Respiratory Failure. Am. J. Respir. Crit. Care Med. 2017, 195, 438–442. [Google Scholar] [CrossRef]
- Grieco, D.L.; Menga, L.S.; Eleuteri, D.; Antonelli, M. Patient self-inflicted lung injury: Implications for acute hypoxemic respiratory failure and ARDS patients on non-invasive support. Minerva Anestesiol. 2019, 85, 1014–1023. [Google Scholar] [CrossRef]
- Weaver, L.; Das, A.; Saffaran, S.; Yehya, N.; Scott, T.E.; Chikhani, M.; Laffey, J.G.; Hardman, J.G.; Camporota, L.; Bates, D.G. High risk of patient self-inflicted lung injury in COVID-19 with frequently encountered spontaneous breathing patterns: A computational modelling study. Ann. Intensive Care 2021, 11, 109. [Google Scholar] [CrossRef]
- Apigo, M.; Schechtman, J.; Dhliwayo, N.; Al Tameemi, M.; Gazmuri, R.J. Development of a work of breathing scale and monitoring need of intubation in COVID-19 pneumonia. Crit. Care 2020, 24, 477. [Google Scholar] [CrossRef]
- Cherniack, R.M.; Farhi, L.E.; Armstrong, B.W.; Proctor, D.F. A comparison of esophageal and intrapleural pressure in man. J. Appl. Physiol. 1955, 8, 203–211. [Google Scholar] [CrossRef]
- Tonelli, R.; Fantini, R.; Tabbì, L.; Castaniere, I.; Pisani, L.; Pellegrino, M.R.; Della Casa, G.; D’Amico, R.; Girardis, M.; Nava, S.; et al. Early Inspiratory Effort Assessment by Esophageal Manometry Predicts Noninvasive Ventilation Outcome in De Novo Respiratory Failure. A Pilot Study. Am. J. Respir. Crit. Care Med. 2020, 202, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Giosa, L.; Bonifazi, M.; Pasticci, I.; Busana, M.; Macri, M.; Romitti, F.; Vassalli, F.; Quintel, M. Targeting transpulmonary pressure to prevent ventilator-induced lung injury. Expert Rev. Respir. Med. 2019, 13, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Natalini, G.; Buizza, B.; Granato, A.; Aniballi, E.; Pisani, L.; Ciabatti, G.; Lippolis, V.; Rosano, A.; Latronico, N.; Grasso, S.; et al. Non-invasive assessment of respiratory muscle activity during pressure support ventilation: Accuracy of end-inspiration occlusion and least square fitting methods. J. Clin. Monit. Comput. 2020, 35, 913–921. [Google Scholar] [CrossRef]
- Bertoni, M.; Spadaro, S.; Goligher, E.C. Monitoring Patient Respiratory Effort during Mechanical Ventilation: Lung and Diaphragm-Protective Ventilation. Crit. Care 2020, 24, 106. [Google Scholar] [CrossRef] [PubMed]
- Walling, P.T.; Savege, T.M. A comparison of oesophageal and central venous pressures in the measurement of transpulmonary pressure change. Br. J. Anaesth. 1976, 48, 475–479. [Google Scholar] [CrossRef]
- Kyogoku, M.; Takeuchi, M.; Inata, Y.; Okuda, N.; Shimizu, Y.; Hatachi, T.; Moon, K.; Tachibana, K. A novel method for transpulmonary pressure estimation using fluctuation of central venous pressure. J. Clin. Monit. Comput. 2020, 34, 725–731. [Google Scholar] [CrossRef]
- La Colla, L.; Bronshteyn, Y.S.; Mark, J.B. Respiratory Variation in Central Venous Pressure (CVP) to Guide Ventilatory Support in Coronavirus Disease 2019 (COVID-19)—Related Lung Injury. J. Cardiothorac. Vasc. Anesth. 2021, 35, 345–347. [Google Scholar] [CrossRef] [PubMed]
- Bellani, G.; Grassi, A.; Sosio, S.; Foti, G. Plateau and driving pressure in the presence of spontaneous breathing. Intensive Care Med. 2019, 45, 97–98. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, H.; Yamada, Y.; Fan, E. The future of driving pressure: A primary goal for mechanical ventilation? J. Intensive Care 2018, 6, 64. [Google Scholar] [CrossRef]
- Foti, G.; Cereda, M.; Banfi, G.; Pelosi, P.; Fumagalli, R.; Pesenti, A. End-inspiratory airway occlusion: A method to assess the pressure developed by inspiratory muscles in patients with acute lung injury undergoing pressure support. Am. J. Respir. Crit. Care Med. 1997, 156 Pt 1, 1210–1216. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society; European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am. J. Respir. Crit. Care Med. 2002, 166, 518–624. [Google Scholar] [CrossRef]
- Conti, G.; Cinnella, G.; Barboni, E.; Lemaire, F.; Harf, A.; Brochard, L. Estimation of occlusion pressure during assisted ventilation in patients with intrinsic PEEP. Am. J. Respir. Crit. Care Med. 1996, 154 Pt 1, 907–912. [Google Scholar] [CrossRef]
- Whitelaw, W.A.; Derenne, J.P.; Milic-Emili, J. Occlusion pressure as a measure of respiratory center output cm conscious man. Respir. Physiol. 1975, 23, 181–199. [Google Scholar] [CrossRef]
- Pletsch-Assuncao, R.; Caleffi Pereira, M.; Ferreira, J.G.; Cardenas, L.Z.; de Albuquerque, A.L.P.; de Carvalho, C.R.R.; Caruso, P. Accuracy of Invasive and Noninvasive Parameters for Diagnosing Ventilatory Overassistance During Pressure Support Ventilation. Crit. Care Med. 2018, 46, 411–417. [Google Scholar] [CrossRef]
- Rittayamai, N.; Beloncle, F.; Goligher, E.C.; Chen, L.; Mancebo, J.; Richard, J.M.; Brochard, L. Effect of inspiratory synchronization during pressure-controlled ventilation on lung distension and inspiratory effort. Ann. Intensive Care 2017, 7, 100. [Google Scholar] [CrossRef] [PubMed]
- Bertoni, M.; Telias, I.; Urner, M.; Long, M.; Del Sorbo, L.; Fan, E.; Sinderby, C.; Beck, J.; Liu, L.; Qiu, H.; et al. A novel non-invasive method to detect excessively high respiratory effort and dynamic transpulmonary driving pressure during mechanical ventilation. Crit. Care 2019, 23, 346. [Google Scholar] [CrossRef]
- Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 2000, 342, 1301–1308. [Google Scholar] [CrossRef] [PubMed]
- Slutsky, A.S.; Ranieri, V.M. Ventilator-induced lung injury. N. Engl. J. Med. 2013, 369, 2126–2136, Erratum in 2014, 370, 1668–1669. [Google Scholar] [CrossRef] [PubMed]
- Gregoretti, C.; Cortegiani, A.; Raineri, S.M.; Giarrjatano, A. Noninvasive Ventilation in Hypoxemic Patients: An Ongoing Soccer Game or a Lost One? Turk. J. Anaesthesiol. Reanim. 2017, 45, 329–331. [Google Scholar] [CrossRef]
- De Jong, A.; Hernandez, G.; Chiumello, D. Is there still a place for noninvasive ventilation in acute hypoxemic respiratory failure? Intensive Care Med. 2018, 44, 2248–2250. [Google Scholar] [CrossRef]
- Carteaux, G.; Millán-Guilarte, T.; De Prost, N.; Razazi, K.; Abid, S.; Thille, A.W.; Schortgen, F.; Brochard, L.; Brun-Buisson, C.; Mekontso Dessap, A. Failure of Noninvasive Ventilation for De Novo Acute Hypoxemic Respiratory Failure: Role of Tidal Volume. Crit. Care Med. 2016, 44, 282–290. [Google Scholar] [CrossRef]
- Gattinoni, L.; Pesenti, A.; Avalli, L.; Rossi, F.; Bombino, M. Pressure-volume curve of total respiratory system in acute respiratory failure. Computed tomographic scan study. Am. Rev. Respir. Dis. 1987, 136, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Matamis, D.; Soilemezi, E.; Tsagourias, M.; Akoumianaki, E.; Dimassi, S.; Boroli, F.; Richard, J.C.; Brochard, L. Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications. Intensive Care Med. 2013, 39, 801–810. [Google Scholar] [CrossRef]
- Cohn, D.; Benditt, J.O.; Eveloff, S.; McCool, F.D. Diaphragm thickening during inspiration. J. Appl. Physiol. 1997, 83, 291–296. [Google Scholar] [CrossRef] [PubMed]
- McCool, F.D.; Tzelepis, G.E. Dysfunction of the diaphragm. N. Engl. J. Med. 2012, 366, 932–942, Erratum in 2012, 366, 2138. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, G.; De Filippi, G.; Elia, F.; Panero, F.; Volpicelli, G.; Aprà, F. Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation. Crit. Ultrasound J. 2014, 6, 8. [Google Scholar] [CrossRef] [PubMed]
- Umbrello, M.; Formenti, P.; Longhi, D.; Galimberti, A.; Piva, I.; Pezzi, A.; Mistraletti, G.; Marini, J.J.; Iapichino, G. Diaphragm ultrasound as indicator of respiratory effort in critically ill patients undergoing assisted mechanical ventilation: A pilot clinical study. Crit. Care 2015, 19, 161. [Google Scholar] [CrossRef]
- Vivier, E.; Mekontso Dessap, A.; Dimassi, S.; Vargas, F.; Lyazidi, A.; Thille, A.W.; Brochard, L. Diaphragm ultrasonography to estimate the work of breathing during non-invasive ventilation. Intensive Care Med. 2012, 38, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Schepens, T.; Dres, M.; Heunks, L.; Goligher, E.C. Diaphragm-protective mechanical ventilation. Curr. Opin. Crit. Care 2019, 25, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Boussuges, A.; Gole, Y.; Blanc, P. Diaphragmatic motion studied by m-mode ultrasonography: Methods, reproducibility, and normal values. Chest 2009, 135, 391–400. [Google Scholar] [CrossRef]
- Spadaro, S.; Grasso, S.; Mauri, T.; Dalla Corte, F.; Alvisi, V.; Ragazzi, R.; Cricca, V.; Biondi, G.; Di Mussi, R.; Marangoni, E.; et al. Can diaphragmatic ultrasonography performed during the T-tube trial predict weaning failure? The role of diaphragmatic rapid shallow breathing index. Crit. Care 2016, 20, 305. [Google Scholar] [CrossRef]
- Cohen, E.; Mier, A.; Heywood, P.; Murphy, K.; Boultbee, J.; Guz, A. Diaphragmatic movement in hemiplegic patients measured by ultrasonography. Thorax 1994, 49, 890–895. [Google Scholar] [CrossRef] [PubMed]
- Fayssoil, A.; Behin, A.; Ogna, A.; Mompoint, D.; Amthor, H.; Clair, B.; Laforet, P.; Mansart, A.; Prigent, H.; Orlikowski, D.; et al. Diaphragm: Pathophysiology and Ultrasound Imaging in Neuromuscular Disorders. J. Neuromuscul. Dis. 2018, 5, 1–10. [Google Scholar] [CrossRef]
- Worapratya, P.; Anupat, S.; Suwannanon, R.; Wuthisuthimethawee, P. Correlation of caval index, inferior vena cava diameter, and central venous pressure in shock patients in the emergency room. Open Access Emerg. Med. 2014, 6, 57–62. [Google Scholar] [CrossRef][Green Version]
- Tombini, V.; Di Capua, M.; Capsoni, N.; Lazzati, A.; Bergamaschi, M.; Gheda, S.; Ghezzi, L.; Cassano, G.; Albertini, V.; Porta, L.; et al. Risk Stratification in COVID-19 Pneumonia—Determining the Role of Lung Ultrasound. Ultraschall Med. 2021. [Google Scholar] [CrossRef]
- Yoshida, R.; Tomita, K.; Kawamura, K.; Nozaki, T.; Setaka, Y.; Monma, M.; Ohse, H. Measurement of intercostal muscle thickness with ultrasound imaging during maximal breathing. J. Phys. Ther. Sci. 2019, 31, 340–343. [Google Scholar] [CrossRef]
- Shi, Z.H.; Jonkman, A.; de Vries, H.; Jansen, D.; Ottenheijm, C.; Girbes, A.; Spoelstra-de Man, A.; Zhou, J.X.; Brochard, L.; Heunks, L. Expiratory muscle dysfunction in critically ill patients: Towards improved understanding. Intensive Care Med. 2019, 45, 1061–1071. [Google Scholar] [CrossRef]
- Tuinman, P.R.; Jonkman, A.H.; Dres, M.; Shi, Z.H.; Goligher, E.C.; Goffi, A.; de Korte, C.; Demoule, A.; Heunks, L. Respiratory muscle ultrasonography: Methodology, basic and advanced principles and clinical applications in ICU and ED patients-a narrative review. Intensive Care Med. 2020, 46, 594–605. [Google Scholar] [CrossRef]
- Bandera, A.; Aliberti, S.; Gualtierotti, R.; Baldini, M.; Blasi, F.; Cesari, M.; Costantino, G.; Fracanzani, A.L.; Gori, A.; Montano, N.; et al. COVID-19 Network: The response of an Italian Reference Institute toresearch challenges about a new pandemia. Clin. Microbiol. Infect. 2020, 26, 1576–1578. [Google Scholar] [CrossRef] [PubMed]
- Bandera, A.; Nobili, A.; Tettamanti, M.; Harari, S.; Bosari, S.; Mannucci, P.M. Clinical factors associated with death in 3044 COVID-19 patients managed in internal medicine wards in Italy: Comment. Intern. Emerg. Med. 2021, 1–4. [Google Scholar] [CrossRef]
- Bellani, G.; Grasselli, G.; Cecconi, M.; Antolini, L.; Borelli, M.; De Giacomi, F.; Bosio, G.; Latronico, N.; Filippini, M.; Gemma, M.; et al. Noninvasive Ventilatory Support of Patients with COVID-19 outside the Intensive Care Units (WARd-COVID). Ann. Am. Thorac. Soc. 2021, 18, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Arnal, J.M.; Chatburn, R. Paying attention to patient self-inflicted lung injury. Minerva Anestesiol. 2019, 85, 940–942. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, E.; Mauri, T.; Beitler, J.R.; Pesenti, A.; Brodie, D. Respiratory drive in the acute respiratory distress syndrome: Pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med. 2020, 46, 606–618. [Google Scholar] [CrossRef] [PubMed]
- Di Capua, M.; Tonani, M.; Giustivi, D.; Delfanti, F.; Testa, S.; Paglia, S. Non-Invasive Low PEEP Versus High PEEP Ventilation Strategy in Severe COVID-19 Patients: An Observational Case—Control Study. Am. J. Biomed. Sci. Res. 2021, 11, 288–293. [Google Scholar] [CrossRef]
- Gattinoni, L.; Chiumello, D.; Caironi, P.; Busana, M.; Romitti, F.; Brazzi, L.; Camporota, L. COVID-19 pneumonia: Different respiratory treatments for different phenotypes? Intensive Care Med. 2020, 46, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
| Index/Parameter | Equation | Normal Value |
|---|---|---|
| Esophageal pressure swing (ΔPES) | 3–8 cm H2O | |
| Transpulmonary pressure (PL) | PAW − PES | <20 cm H2O |
| Central Venous Pressure swing (ΔCVP) | uncertain | |
| Plateau pressure (PPLAT) | <30 cm H2O | |
| Driving pressure (ΔP) | PPLAT − PEEP | <15 cm H2O |
| Pressure Muscle Index (PMI) | PPLAT − (PEEP + PS) | <6 cm H2O |
| P.01 | 1.5–3.5 cm H2O | |
| Occlusion pressure (POCC) | Not defined |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giustivi, D.; Bottazzini, F.; Belliato, M. Respiratory Monitoring at Bedside in COVID-19 Patients. J. Clin. Med. 2021, 10, 4943. https://doi.org/10.3390/jcm10214943
Giustivi D, Bottazzini F, Belliato M. Respiratory Monitoring at Bedside in COVID-19 Patients. Journal of Clinical Medicine. 2021; 10(21):4943. https://doi.org/10.3390/jcm10214943
Chicago/Turabian StyleGiustivi, Davide, Francesco Bottazzini, and Mirko Belliato. 2021. "Respiratory Monitoring at Bedside in COVID-19 Patients" Journal of Clinical Medicine 10, no. 21: 4943. https://doi.org/10.3390/jcm10214943
APA StyleGiustivi, D., Bottazzini, F., & Belliato, M. (2021). Respiratory Monitoring at Bedside in COVID-19 Patients. Journal of Clinical Medicine, 10(21), 4943. https://doi.org/10.3390/jcm10214943






