Long-Term Influence of Paraspinal Muscle Quantity in Adolescent Idiopathic Scoliosis Following Deformity Correction by Posterior Approach
Abstract
:1. Introduction
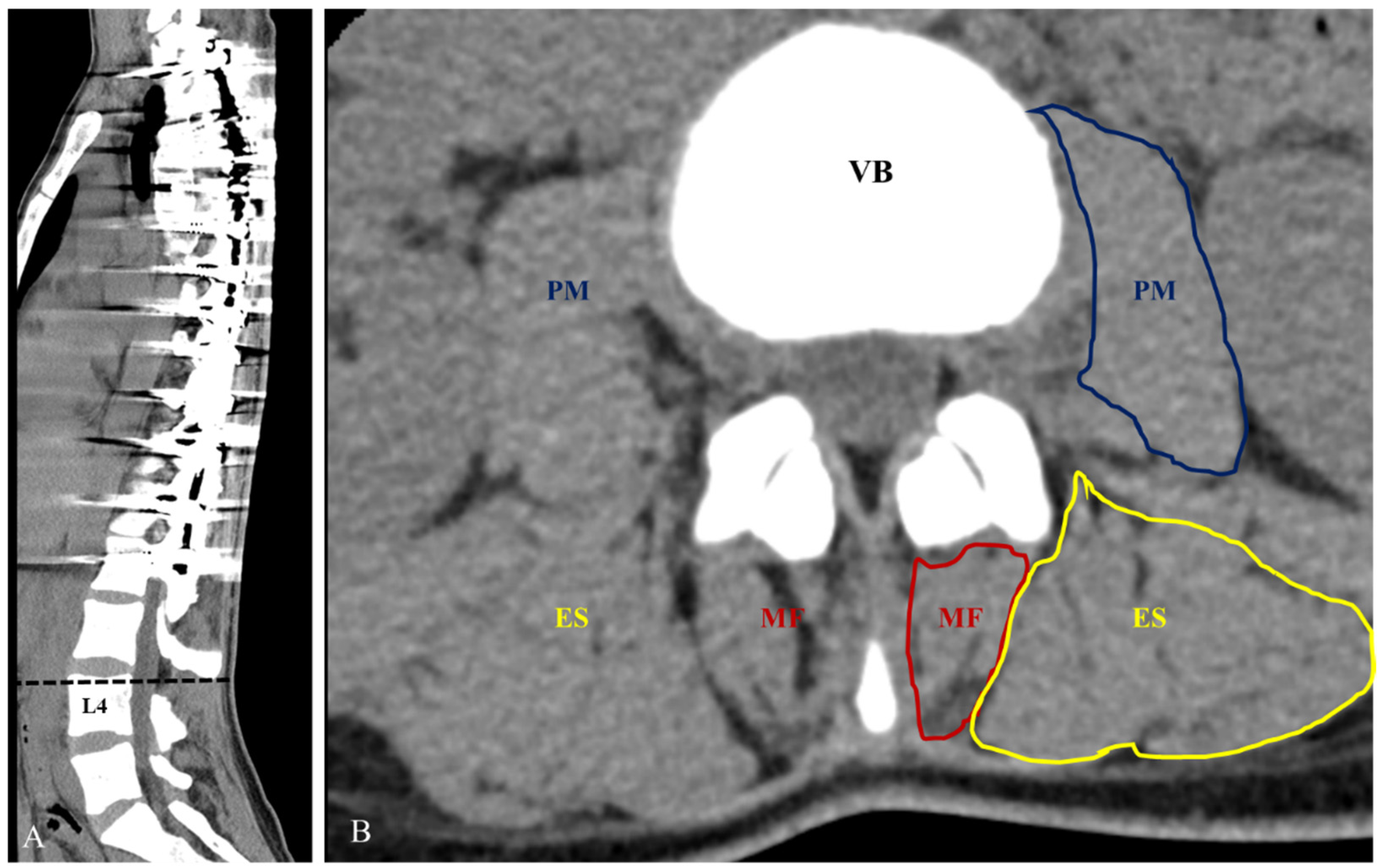
2. Materials and Methods
3. Results
3.1. Comparison of Patient Demographic Data
3.2. Comparison of Radiological Parameters
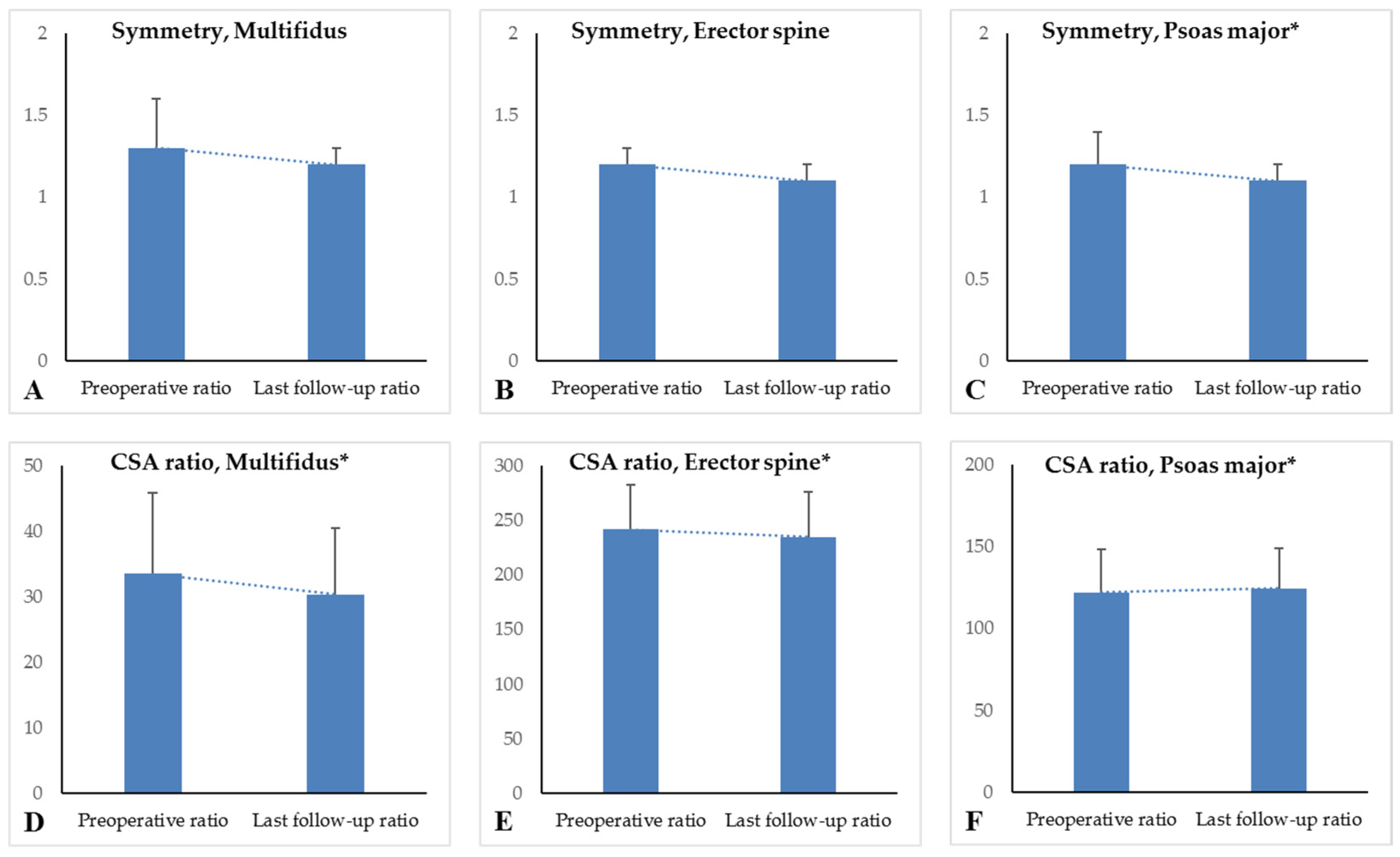
3.3. Comparison of CSAs of the Paraspinal Muscles
3.4. Correlation Analysis for CSA Ratios of Paraspinal Muscles
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weinstein, S.L.; Dolan, L.A.; Cheng, J.C.Y.; Danielsson, A.; Morcuende, J.A. Adolescent idiopathic scoliosis. Lancet 2008, 371, 1527–1537. [Google Scholar] [CrossRef] [Green Version]
- Jada, A.; Mackel, C.E.; Hwang, S.W.; Samdani, A.F.; Stephen, J.H.; Bennett, J.T.; Baaj, A.A. Evaluation and management of adolescent idiopathic scoliosis: A review. Neurosurg. Focus 2017, 43, E2. [Google Scholar] [CrossRef] [Green Version]
- Suk, S.I.; Kim, J.H.; Kim, S.S.; Lim, D.J. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur. Spine J. 2012, 21, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Maki, T.; Oura, P.; Paananen, M.; Niinimaki, J.; Karppinen, J.; Junno, J.A. Longitudinal Analysis of Paraspinal Muscle Cross-Sectional Area During Early Adulthood—A 10-Year Follow-Up MRI Study. Sci. Rep. 2019, 9, 19497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, A.B.; Weiss, E.H.; Khan, A.W.; Omeis, I.; Verla, T. Back Muscle Morphometry: Effects on Outcomes of Spine Surgery. World Neurosurg. 2017, 103, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Jun, H.S.; Kim, J.H.; Ahn, J.H.; Chang, I.B.; Song, J.H.; Kim, T.H.; Park, M.S.; Chan Kim, Y.; Kim, S.W.; Oh, J.K.; et al. The Effect of Lumbar Spinal Muscle on Spinal Sagittal Alignment: Evaluating Muscle Quantity and Quality. Neurosurgery 2016, 79, 847–855. [Google Scholar] [CrossRef] [PubMed]
- Ohashi, M.; Watanabe, K.; Hirano, T.; Hasegawa, K.; Katsumi, K.; Shoji, H.; Mizouchi, T.; Endo, N. Long-term Impacts of Brace Treatment for Adolescent Idiopathic Scoliosis on Body Composition, Paraspinal Muscle Morphology, and Bone Mineral Density. Spine 2019, 44, E1075–E1082. [Google Scholar] [CrossRef]
- Zapata, K.A.; Wang-Price, S.S.; Sucato, D.J.; Dempsey-Robertson, M. Ultrasonographic measurements of paraspinal muscle thickness in adolescent idiopathic scoliosis: A comparison and reliability study. Pediatr. Phys. 2015, 27, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Ohashi, M.; Hirano, T.; Katsumi, K.; Shoji, H.; Mizouchi, T.; Endo, N.; Hasegawa, K. The Influence of Lumbar Muscle Volume on Curve Progression after Skeletal Maturity in Patients with Adolescent Idiopathic Scoliosis: A Long-Term Follow-up Study. Spine Deform. 2018, 6, 691–698. [Google Scholar] [CrossRef]
- Yeung, K.H.; Man, G.C.W.; Shi, L.; Hui, S.C.N.; Chiyanika, C.; Lam, T.P.; Ng, B.K.W.; Cheng, J.C.Y.; Chu, W.C.W. Magnetic Resonance Imaging-Based Morphological Change of Paraspinal Muscles in Girls with Adolescent Idiopathic Scoliosis. Spine 2019, 44, 1356–1363. [Google Scholar] [CrossRef] [PubMed]
- Hyun, S.J.; Bae, C.W.; Lee, S.H.; Rhim, S.C. Fatty Degeneration of the Paraspinal Muscle in Patients With Degenerative Lumbar Kyphosis: A New Evaluation Method of Quantitative Digital Analysis Using MRI and CT Scan. Clin. Spine Surg. 2016, 29, 441–447. [Google Scholar] [CrossRef]
- Dang, N.R.; Moreau, M.J.; Hill, D.L.; Mahood, J.K.; Raso, J. Intra-observer reproducibility and interobserver reliability of the radiographic parameters in the Spinal Deformity Study Group’s AIS Radiographic Measurement Manual. Spine 2005, 30, 1064–1069. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, A.; Katoh, H.; Sakai, D.; Tanaka, M.; Sato, M.; Watanabe, M. The correlation analysis between sagittal alignment and cross-sectional area of paraspinal muscle in patients with lumbar spinal stenosis and degenerative spondylolisthesis. BMC Musculoskelet Disord 2019, 20, 352. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Yang, J.H.; Chang, D.G.; Suk, S.I.; Suh, S.W.; Kim, S.I.; Song, K.S.; Park, J.B.; Cho, W. Proximal Junctional Kyphosis in Adult Spinal Deformity: Definition, Classification, Risk Factors, and Prevention Strategies. Asian Spine J. 2021, in press. [Google Scholar] [CrossRef]
- Kim, H.J.; Yang, J.H.; Chang, D.G.; Suk, S.I.; Suh, S.W.; Song, K.S.; Park, J.B.; Cho, W. Adult Spinal Deformity: Current Concepts and Decision-Making Strategies for Management. Asian Spine J. 2020, 14, 886–897. [Google Scholar] [CrossRef]
- Danneels, L.A.; Vanderstraeten, G.G.; Cambier, D.C.; Witvrouw, E.E.; De Cuyper, H.J. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur. Spine J. 2000, 9, 266–272. [Google Scholar] [CrossRef] [Green Version]
- Tamai, K.; Chen, J.; Stone, M.; Arakelyan, A.; Paholpak, P.; Nakamura, H.; Buser, Z.; Wang, J.C. The evaluation of lumbar paraspinal muscle quantity and quality using the Goutallier classification and lumbar indentation value. Eur. Spine J. 2018, 27, 1005–1012. [Google Scholar] [CrossRef]
- Penning, L. Psoas muscle and lumbar spine stability: A concept uniting existing controversies. Critical review and hypothesis. Eur. Spine J. 2000, 9, 577–585. [Google Scholar] [CrossRef]
- Verla, T.; Adogwa, O.; Elsamadicy, A.; Moreno, J.R.; Farber, H.; Cheng, J.; Bagley, C.A. Effects of Psoas Muscle Thickness on Outcomes of Lumbar Fusion Surgery. World Neurosurg. 2016, 87, 283–289. [Google Scholar] [CrossRef]
- Yang, J.H.; Kim, H.J.; Chang, D.G.; Suh, S.W. Comparative Analysis of Radiologic and Clinical Outcomes between Conventional Open and Minimally Invasive Scoliosis Surgery for Adolescent Idiopathic Scoliosis. World Neurosurg. 2021, 151, e234–e240. [Google Scholar] [CrossRef]
- Yang, J.H.; Kim, H.J.; Chang, D.G.; Suh, S.W. Minimally invasive scoliosis surgery for adolescent idiopathic scoliosis using posterior mini-open technique. J. Clin. Neurosci. 2021, 89, 199–205. [Google Scholar] [CrossRef]
- Yang, J.H.; Chang, D.G.; Suh, S.W.; Damani, N.; Lee, H.N.; Lim, J.; Mun, F. Safety and effectiveness of minimally invasive scoliosis surgery for adolescent idiopathic scoliosis: A retrospective case series of 84 patients. Eur. Spine J. 2020, 29, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Neradi, D.; Kumar, V.; Kumar, S.; Sodavarapu, P.; Goni, V.; Dhatt, S.S. Minimally Invasive Surgery versus Open Surgery for Adolescent Idiopathic Scoliosis: A Systematic Review and Meta-Analysis. Asian Spin J. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
| Variables | Cases (n = 42) | p-Value |
|---|---|---|
| Gender (n (%)) Male Female | 5 (11.9%) 37 (88.1%) | - - |
| Age (years) At surgery At last follow up | 14.6 ± 2.4 * 27.4 ± 3.6 * | <0.001 |
| Follow-up period (years) | 9.9 ± 2.4 * | - |
| BMI at surgery (kg/m2) | 18.1 ± 3.1 * | - |
| Risser stage at surgery | 3.1 ± 0.9 * | - |
| Fused segments | 11.1 ± 2.4 * | - |
| Thoracoplasty (Yes:No) | 40:2 | - |
| Number of resected ribs | 5.5 ± 1.7 * | - |
| Variables | Cases (n = 42) | p-Value |
|---|---|---|
| Coronal parameters | ||
| Main curve Preoperative (°) Postoperative (°) Last follow up (°) Correction rate (%) Loss of correction (°) | 59.9 ± 15.1 16.4 ± 11.5 15.7 ± 12.0 72.7 ± 12.6 1.3 ± 16.4 | <0.001 * Pre vs. Post: <0.001 * Post vs. Last: 0.973 * Last vs. Pre: <0.001 |
| Coronal balance (mm) Preoperative Postoperative Last follow up | 13.4 ± 8.3 14.4 ± 10.9 8.3 ± 6.0 | <0.001 * Pre vs. Post: 0.849 * Post vs. Last: 0.005 * Last vs. Pre: 0.024 |
| Sagittal parameters | - | |
| Sagittal vertical axis (mm) Preoperative Postoperative Last follow up | 18.2 ± 17.5 22.1 ± 13.8 18.1 ± 12.1 | 0.319 |
| Thoracic kyphosis (°) Preoperative Postoperative Last follow up | 25.3 ± 10.2 27.4 ± 6.7 32.2 ± 8.7 | <0.001 * Pre vs. Post: 0.536 * Post vs. Last: 0.002 * Pre vs. Last: 0.001 |
| Lumbar lordosis (°) Preoperative Postoperative Last follow up | 37.3 ± 11.4 39.5 ± 10.2 44.6 ± 12.6 | <0.001 * Pre vs. Post: 0.660 * Post vs. Last: 0.032 * Last vs. Pre: 0.012 |
| Variables | Preoperative (n = 42) | Last Follow Up (n = 42) | p-Value |
|---|---|---|---|
| CSA (mm2) | |||
| Multifidus (mm2) Right Left Mean | 173.9 ± 54.5 170.9 ± 76.1 172.4 ± 59.3 | 185.5 ± 61.1 170.4 ± 60.6 177.9 ± 57.4 | 0.001 0.015 <0.001 |
| Erector spine (mm2) Right Left Mean | 1291.3 ± 280.6 1229.1 ± 250.2 1260.2 ± 243.1 | 1478.5 ± 343.1 1261.5 ± 272.4 1370.0 ± 291.8 | 0.001 0.002 <0.001 |
| Psoas major (mm2) Right Left Mean | 609.3 ± 168.1 656.4 ± 145.7 632.8 ± 144.9 | 737.4 ± 197.2 728.3 ± 201.2 732.8 ± 193.3 | <0.001 0.001 <0.001 |
| L4 vertebrae body (mm2) | 1046.3 ± 132.9 | 1179.9 ± 183.0 | <0.001 |
| Symmetry of CSA | |||
| Multifidus Erector spine Psoas major | 1.3 ± 0.3 1.2 ± 0.1 1.2 ± 0.2 | 1.2 ± 0.1 1.1 ± 0.1 1.1 ± 0.1 | 0.209 0.095 0.005 |
| CSA ratio (%) | |||
| Multifidus Erector spine Psoas major | 33.5 ± 12.4 242.0 ± 40.6 122.0 ± 26.6 | 30.4 ± 10.1 235.0 ± 41.0 124.5 ± 27.4 | 0.001 <0.001 0.002 |
| Parameters of CSA Ratio | Comparative Parameters | Correlation Coefficient | p-Value |
|---|---|---|---|
| Multifidus | Age Duration BMI Correction rate Loss of correction CB (Last follow up) SVA (Last follow up) TK (Last follow up) LL (Last follow up) | 0.048 0.193 0.146 −0.266 0.177 0.023 0.046 0.239 0.081 | 0.765 0.221 0.355 0.088 0.262 0.886 0.770 0.127 0.611 |
| Erector spine | Age Duration BMI Correction rate Loss of correction CB (Last follow up) SVA (Last follow up) TK (Last follow up) LL (Last follow up) Multifidus CSA ratio | 0.304 0.179 −0.280 0.202 0.041 0.160 −0.197 0.281 0.294 0.039 | 0.051 0.257 0.073 0.200 0.795 0.312 0.211 0.072 0.058 0.808 |
| Psoas major | Age Duration BMI Correction rate Loss of correction CB (Last follow up) SVA (Last follow up) TK (Last follow up) LL (Last follow up) Multifidus CSA ratio Erector spine CSA ratio | 0.095 0.089 −0.187 0.268 0.029 0.314 −0.127 0.027 0.035 −0.116 0.546 | 0.549 0.575 0.235 0.087 0.855 0.043 0.423 0.865 0.827 0.465 <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.J.; Yang, J.H.; Chang, D.-G.; Suk, S.-I.; Suh, S.W.; Nam, Y.; Kim, S.-I.; Song, K.-S. Long-Term Influence of Paraspinal Muscle Quantity in Adolescent Idiopathic Scoliosis Following Deformity Correction by Posterior Approach. J. Clin. Med. 2021, 10, 4790. https://doi.org/10.3390/jcm10204790
Kim HJ, Yang JH, Chang D-G, Suk S-I, Suh SW, Nam Y, Kim S-I, Song K-S. Long-Term Influence of Paraspinal Muscle Quantity in Adolescent Idiopathic Scoliosis Following Deformity Correction by Posterior Approach. Journal of Clinical Medicine. 2021; 10(20):4790. https://doi.org/10.3390/jcm10204790
Chicago/Turabian StyleKim, Hong Jin, Jae Hyuk Yang, Dong-Gune Chang, Se-Il Suk, Seung Woo Suh, Yunjin Nam, Sang-Il Kim, and Kwang-Sup Song. 2021. "Long-Term Influence of Paraspinal Muscle Quantity in Adolescent Idiopathic Scoliosis Following Deformity Correction by Posterior Approach" Journal of Clinical Medicine 10, no. 20: 4790. https://doi.org/10.3390/jcm10204790
APA StyleKim, H. J., Yang, J. H., Chang, D.-G., Suk, S.-I., Suh, S. W., Nam, Y., Kim, S.-I., & Song, K.-S. (2021). Long-Term Influence of Paraspinal Muscle Quantity in Adolescent Idiopathic Scoliosis Following Deformity Correction by Posterior Approach. Journal of Clinical Medicine, 10(20), 4790. https://doi.org/10.3390/jcm10204790








