Proteomic Analysis of Maternal Urine for the Early Detection of Preeclampsia and Fetal Growth Restriction
Abstract
1. Introduction
2. Materials and Methods
2.1. Mass Spectrometry Analyses
2.2. Bioinformatics and Statistical Treatment
3. Results
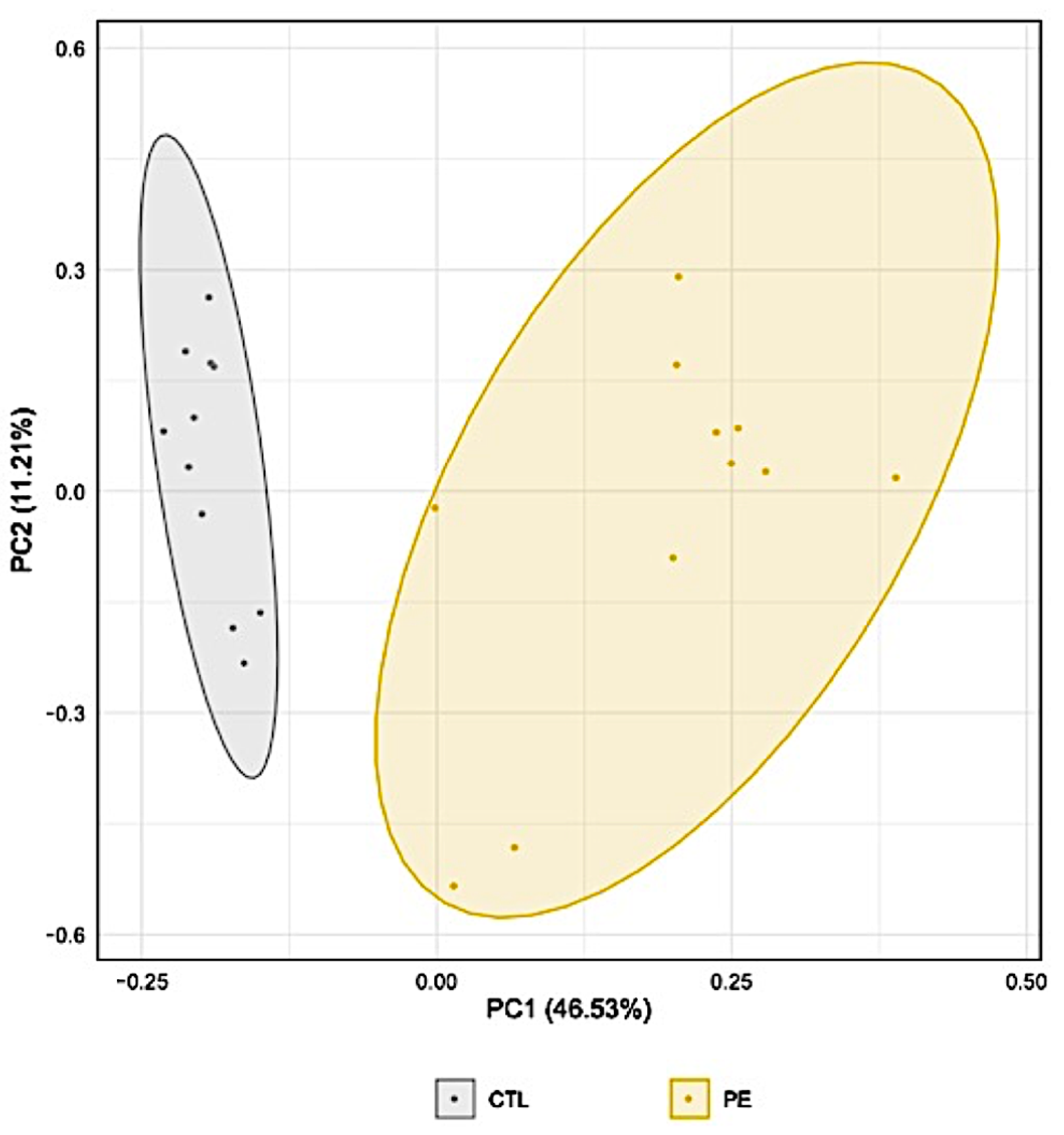
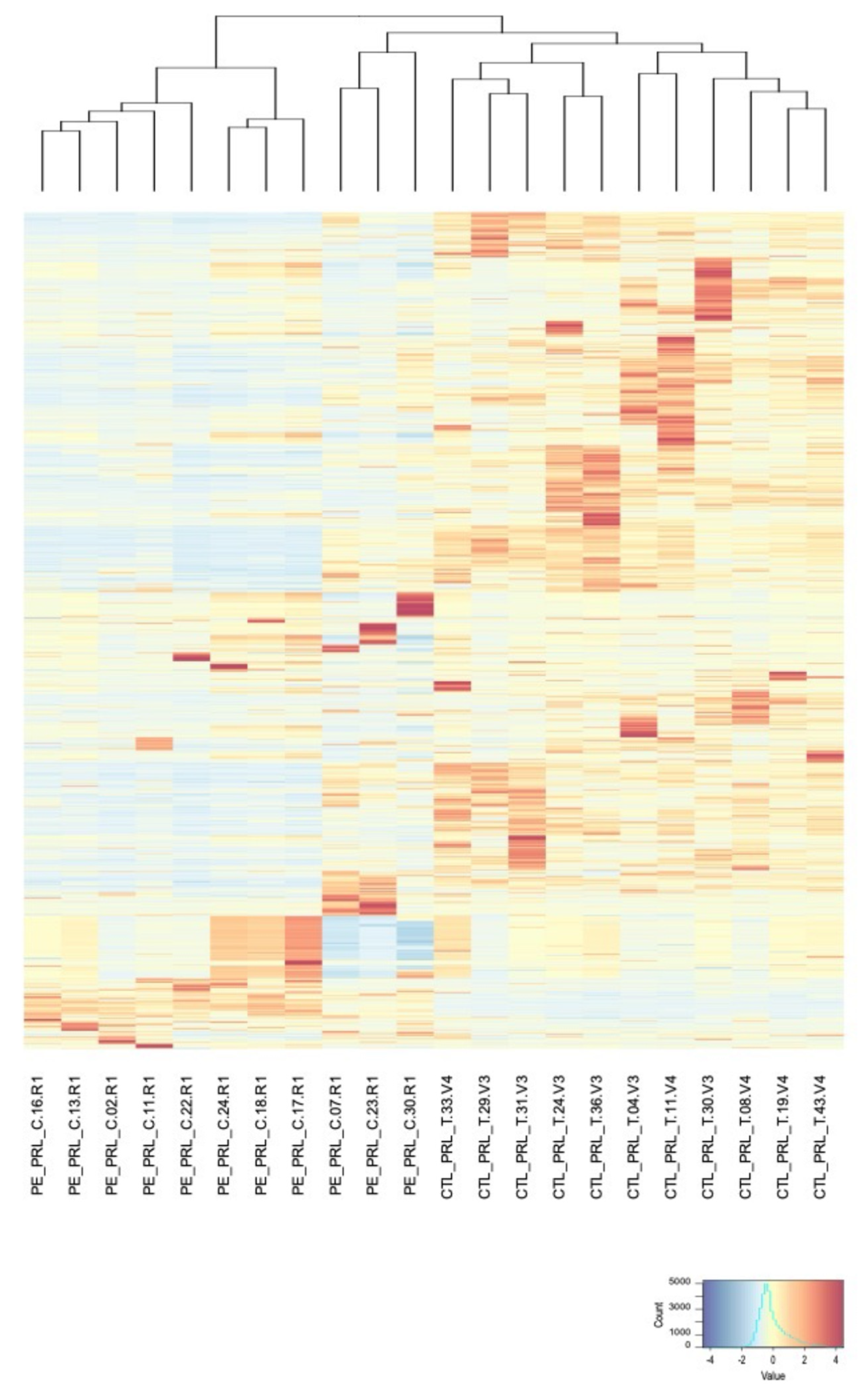
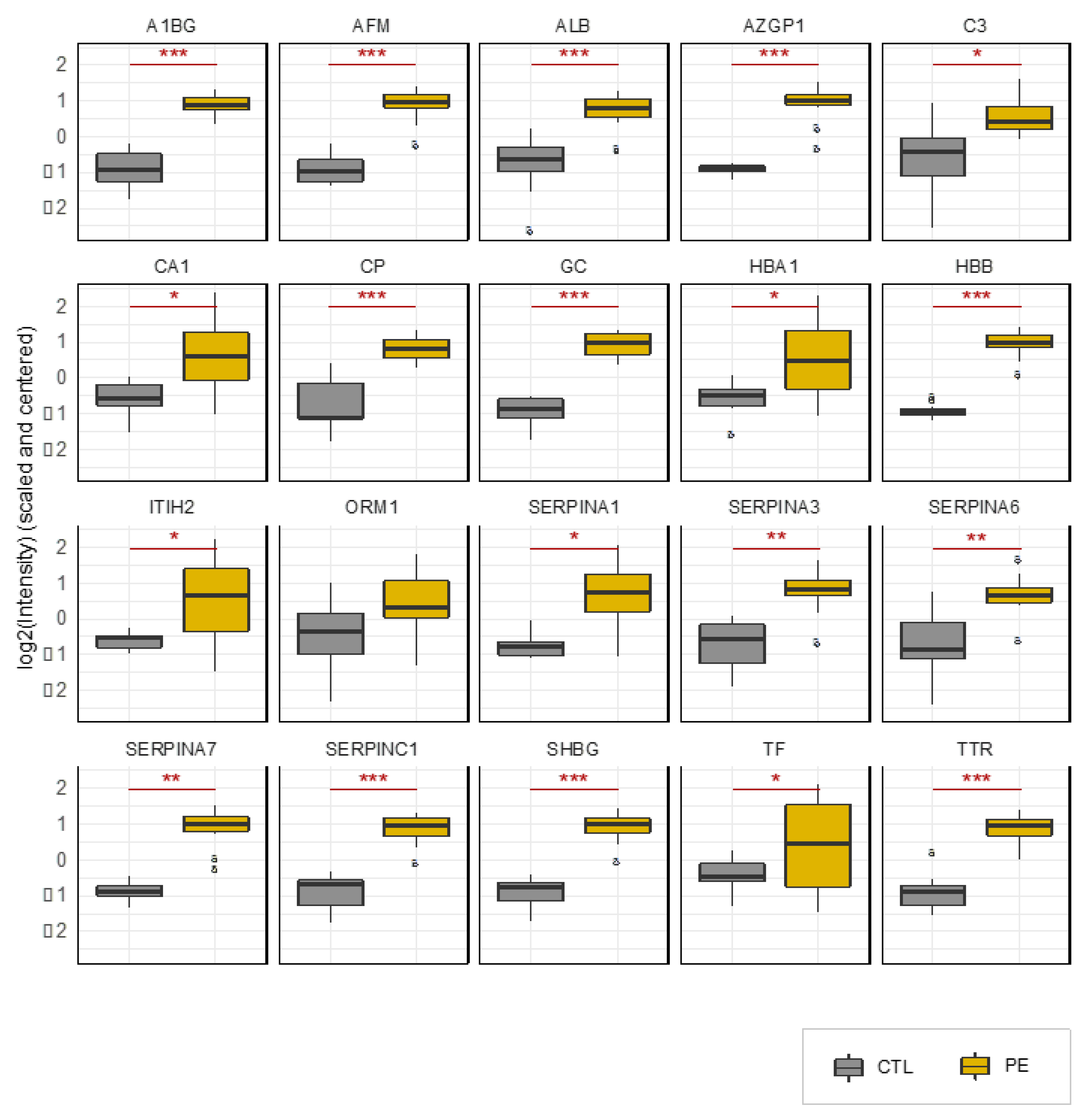
3.1. Discovery Study
3.2. Validation Study
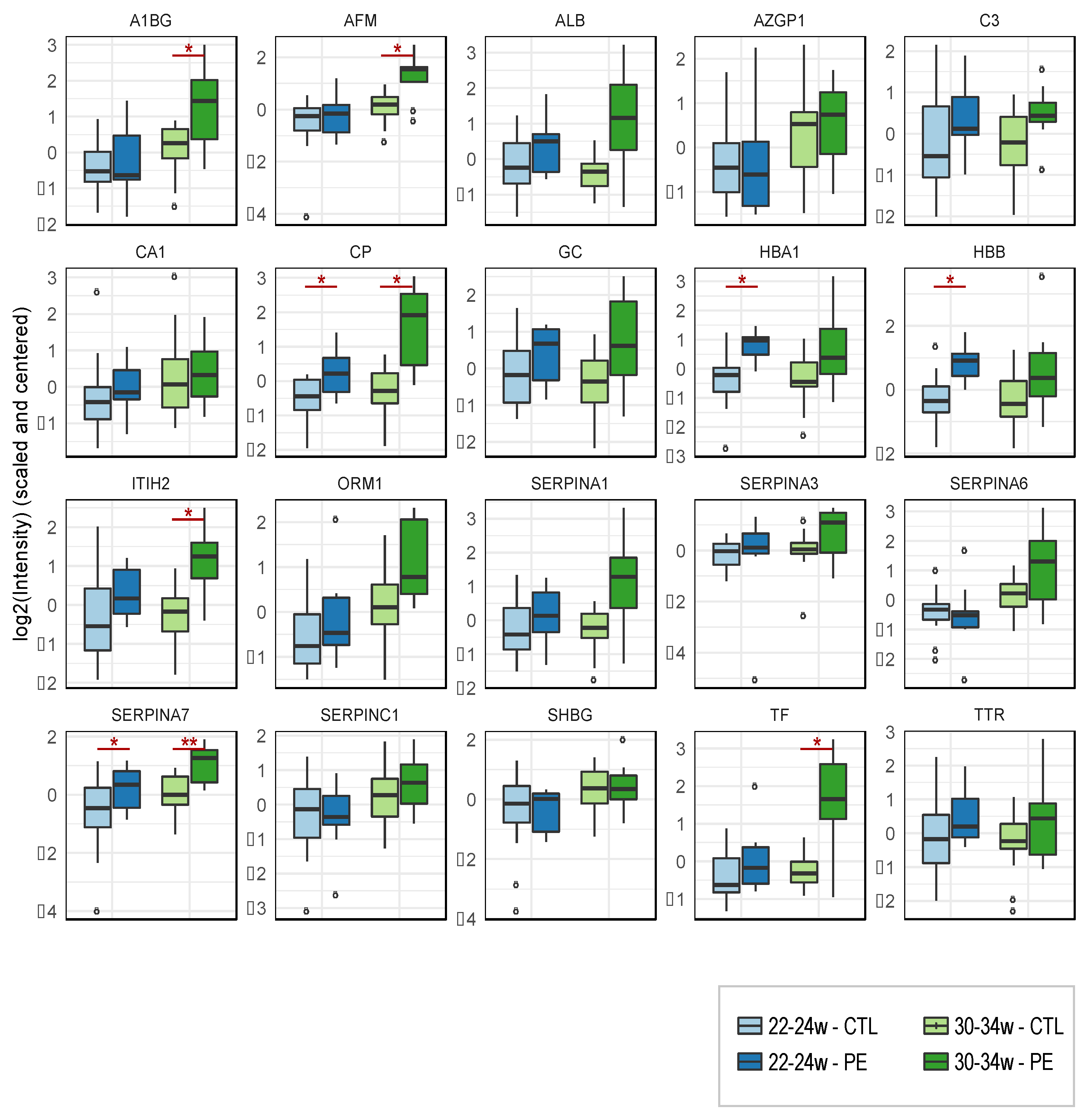
3.3. Longitudinal Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mol, B.W.J.; Roberts, C.T.; Thangaratinam, S.; Magee, L.A.; de Groot, C.J.M.; Hofmeyr, G.J. Pre-eclampsia. Lancet 2016, 387, 999–1011. [Google Scholar] [CrossRef]
- Rana, S.; Lemoine, E.; Granger, J.P.; Karumanchi, S.A. Preeclampsia: Pathophysiology, Challenges, and Perspectives. Circ. Res. 2019, 124, 1094–1112. [Google Scholar] [CrossRef] [PubMed]
- Nakimuli, A.; Chazara, O.; Byamugisha, J.; Elliott, A.M.; Kaleebu, P.; Mirembe, F.; Moffett, A. Pregnancy, parturition and preeclampsia in women of African ancestry. Am. J. Obstet. Gynecol. 2014, 210, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.S.; Smith, G.N. Pre-eclampsia and Cardiovascular Disease Risk Assessment in Women. Am. J. Perinatol. 2016, 33, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Haththotuwa, R.; Kwok, C.S.; Babu, A.; Kotronias, R.A.; Rushton, C.; Zaman, A.; Fryer, A.A.; Kadam, U.; Chew-Graham, C.A.; et al. Preeclampsia and Future Cardiovascular Health: A Systematic Review and Meta-Analysis. Circ. Cardiovasc. Qual. Outcomes 2017, 10, e003497. [Google Scholar] [CrossRef]
- Pinheiro, T.V.; Brunetto, S.; Ramos, J.G.; Bernardi, J.R.; Goldani, M.Z. Hypertensive disorders during pregnancy and health outcomes in the offspring: A systematic review. J. Dev. Orig. Health Dis. 2016, 7, 391–407. [Google Scholar] [CrossRef]
- Davis, E.F.; Lazdam, M.; Lewandowski, A.J.; Worton, S.A.; Kelly, B.; Kenworthy, Y.; Adwani, S.; Wilkinson, A.R.; McCormick, K.; Sargent, I.; et al. Cardiovascular risk factors in children and young adults born to preeclamptic pregnancies: A systematic review. Pediatrics 2012, 129, e1552–e1561. [Google Scholar] [CrossRef]
- Duley, L. The global impact of pre-eclampsia and eclampsia. Semin. Perinatol. 2009, 33, 130–137. [Google Scholar] [CrossRef]
- Steegers, E.A.; von Dadelszen, P.; Duvekot, J.J.; Pijnenborg, R. Pre-eclampsia. Lancet 2010, 376, 631–644. [Google Scholar] [CrossRef]
- Burton, G.J.; Redman, C.W.; Roberts, J.M.; Moffett, A. Pre-eclampsia: Pathophysiology and clinical implications. BMJ 2019, 366, l2381. [Google Scholar] [CrossRef]
- Phipps, E.A.; Thadhani, R.; Benzing, T.; Karumanchi, S.A. Pre-eclampsia: Pathogenesis, novel diagnostics and therapies. Nat. Rev. Nephrol. 2019, 15, 275–289. [Google Scholar] [CrossRef]
- Hod, T.; Cerdeira, A.S.; Karumanchi, S.A. Molecular Mechanisms of Preeclampsia. Cold Spring Harb. Perspect. Med. 2015, 5, a023473. [Google Scholar] [CrossRef]
- Boutin, A.; Gasse, C.; Guerby, P.; Giguere, Y.; Tetu, A.; Bujold, E. First-Trimester Preterm Preeclampsia Screening in Nulliparous Women: The Great Obstetrical Syndrome (GOS) Study. J. Obstet. Gynaecol. Can. 2021, 43, 43–49. [Google Scholar] [CrossRef]
- Rolnik, D.L.; Wright, D.; Poon, L.C.Y.; Syngelaki, A.; O’Gorman, N.; de Paco Matallana, C.; Akolekar, R.; Cicero, S.; Janga, D.; Singh, M.; et al. ASPRE trial: Performance of screening for preterm pre-eclampsia. Ultrasound Obstet. Gynecol. 2017, 50, 492–495. [Google Scholar] [CrossRef]
- Mosimann, B.; Amylidi-Mohr, S.K.; Surbek, D.; Raio, L. First Trimester Screening for Preeclampsia—A Systematic Review. Hypertens. Pregnancy 2020, 39, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Buhimschi, I.A.; Zhao, G.; Funai, E.F.; Harris, N.; Sasson, I.E.; Bernstein, I.M.; Saade, G.R.; Buhimschi, C.S. Proteomic profiling of urine identifies specific fragments of SERPINA1 and albumin as biomarkers of preeclampsia. Am. J. Obstet. Gynecol. 2008, 199, 551.e1–551.e16. [Google Scholar] [CrossRef] [PubMed]
- Lecarpentier, E.; Gris, J.C.; Cochery-Nouvellon, E.; Mercier, E.; Abbas, H.; Thadhani, R.; Karumanchi, S.A.; Haddad, B. Urinary Placental Growth Factor for Prediction of Placental Adverse Outcomes in High-Risk Pregnancies. Obstet. Gynecol. 2019, 134, 1326–1332. [Google Scholar] [CrossRef] [PubMed]
- Parker, C.E.; Pearson, T.W.; Anderson, N.L.; Borchers, C.H. Mass-spectrometry-based clinical proteomics—A review and prospective. Analyst 2010, 135, 1830–1838. [Google Scholar] [CrossRef][Green Version]
- Uzozie, A.C.; Aebersold, R. Advancing translational research and precision medicine with targeted proteomics. J. Proteom. 2018, 189, 1–10. [Google Scholar] [CrossRef]
- Beasley-Green, A. Urine Proteomics in the Era of Mass Spectrometry. Int. Neurourol. J. 2016, 20, S70–S75. [Google Scholar] [CrossRef]
- Marimuthu, A.; O’Meally, R.N.; Chaerkady, R.; Subbannayya, Y.; Nanjappa, V.; Kumar, P.; Kelkar, D.S.; Pinto, S.M.; Sharma, R.; Renuse, S.; et al. A comprehensive map of the human urinary proteome. J. Proteome Res. 2011, 10, 2734–2743. [Google Scholar] [CrossRef] [PubMed]
- Navajas, R.; Corrales, F.; Paradela, A. Quantitative proteomics-based analyses performed on pre-eclampsia samples in the 2004-2020 period: A systematic review. Clin. Proteom. 2021, 18, 6. [Google Scholar] [CrossRef] [PubMed]
- Fillion, A.; Guerby, P.; Lachance, C.; Comeau, M.-P.; Bussières, M.-C.; Doucet-Gingras, F.-A.; Zérounian, S.; Demers, S.; Laforest, G.; Menzies, D.; et al. Placental Growth Factor and soluble Fms-like tyrosine kinase-1 in Preeclampsia: A case-cohort (PEARL) study. J. Obstet. Gynaecol. Can. 2020, 42, 1235–1242. [Google Scholar] [CrossRef] [PubMed]
- Fillion, A.; Guerby, P.; Menzies, D.; Lachance, C.; Comeau, M.P.; Bussieres, M.C.; Doucet-Gingras, F.A.; Zerounian, S.; Bujold, E. Pathological investigation of placentas in preeclampsia (the PEARL study). Hypertens. Pregnancy 2021, 40, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Magee, L.A.; Pels, A.; Helewa, M.; Rey, E.; von Dadelszen, P. Diagnostic, evaluation et prise en charge des troubles hypertensifs de la grossesse: Resume directif. J. Obstet. Gynaecol. Can. 2016, 38, S426–S452. [Google Scholar] [CrossRef]
- Kramer, M.S.; Platt, R.W.; Wen, S.W.; Joseph, K.S.; Allen, A.; Abrahamowicz, M.; Blondel, B.; Breart, G.; Fetal/Infant Health Study Group of the Canadian Perinatal Surveillance, S. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics 2001, 108, E35. [Google Scholar] [CrossRef]
- Rappsilber, J.; Mann, M.; Ishihama, Y. Protocol for micro-purification, enrichment, pre-fractionation and storage of peptides for proteomics using StageTips. Nat. Protoc. 2007, 2, 1896–1906. [Google Scholar] [CrossRef]
- Tyanova, S.; Temu, T.; Cox, J. The MaxQuant computational platform for mass spectrometry-based shotgun proteomics. Nat. Protoc. 2016, 11, 2301–2319. [Google Scholar] [CrossRef]
- RCoreTeam. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Smyth, G. Limma: Linear Models for Microarray Data; Springer: New York, NY, USA, 2005; pp. 397–420. [Google Scholar]
- Pino, L.K.; Searle, B.C.; Bollinger, J.G.; Nunn, B.; MacLean, B.; MacCoss, M.J. The Skyline ecosystem: Informatics for quantitative mass spectrometry proteomics. Mass Spectrom. Rev. 2020, 39, 229–244. [Google Scholar] [CrossRef]
- Szklarczyk, D.; Gable, A.L.; Nastou, K.C.; Lyon, D.; Kirsch, R.; Pyysalo, S.; Doncheva, N.T.; Legeay, M.; Fang, T.; Bork, P.; et al. The STRING database in 2021: Customizable protein-protein networks, and functional characterization of user-uploaded gene/measurement sets. Nucleic Acids Res. 2021, 49, D605–D612. [Google Scholar] [CrossRef]
- Serdar, Z.; Gur, E.; Develioglu, O. Serum iron and copper status and oxidative stress in severe and mild preeclampsia. Cell Biochem. Funct. 2006, 24, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Guller, S.; Buhimschi, C.S.; Ma, Y.Y.; Huang, S.T.; Yang, L.; Kuczynski, E.; Zambrano, E.; Lockwood, C.J.; Buhimschi, I.A. Placental expression of ceruloplasmin in pregnancies complicated by severe preeclampsia. Lab. Investig. 2008, 88, 1057–1067. [Google Scholar] [CrossRef] [PubMed]
- Alemu, A.; Terefe, B.; Abebe, M.; Biadgo, B. Thyroid hormone dysfunction during pregnancy: A review. Int. J. Reprod. Biomed. 2016, 14, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Kaya, E.; Sahin, Y.; Ozkececi, Z.; Pasaoglu, H. Relation between birth weight and thyroid function in preeclampsia-eclampsia. Gynecol. Obstet. Investig. 1994, 37, 30–33. [Google Scholar] [CrossRef]
- Buhimschi, I.A.; Nayeri, U.A.; Zhao, G.; Shook, L.L.; Pensalfini, A.; Funai, E.F.; Bernstein, I.M.; Glabe, C.G.; Buhimschi, C.S. Protein misfolding, congophilia, oligomerization, and defective amyloid processing in preeclampsia. Sci. Transl. Med. 2014, 6, 245ra292. [Google Scholar] [CrossRef]
- Bracken, H.; Buhimschi, I.A.; Rahman, A.; Smith, P.R.S.; Pervin, J.; Rouf, S.; Bousieguez, M.; Lopez, L.G.; Buhimschi, C.S.; Easterling, T.; et al. Congo red test for identification of preeclampsia: Results of a prospective diagnostic case-control study in Bangladesh and Mexico. EClinicalMedicine 2021, 31, 100678. [Google Scholar] [CrossRef]
- Starodubtseva, N.; Nizyaeva, N.; Baev, O.; Bugrova, A.; Gapaeva, M.; Muminova, K.; Kononikhin, A.; Frankevich, V.; Nikolaev, E.; Sukhikh, G. SERPINA1 Peptides in Urine as A Potential Marker of Preeclampsia Severity. Int. J. Mol. Sci. 2020, 21, 914. [Google Scholar] [CrossRef]
- Levine, R.J.; Thadhani, R.; Qian, C.; Lam, C.; Lim, K.H.; Yu, K.F.; Blink, A.L.; Sachs, B.P.; Epstein, F.H.; Sibai, B.M.; et al. Urinary placental growth factor and risk of preeclampsia. JAMA 2005, 293, 77–85. [Google Scholar] [CrossRef]


| Discovery Study | Validation Study | Longitudinal Study | ||||
|---|---|---|---|---|---|---|
| Cases (n = 12) | Controls (n = 12) | Cases (n = 12) | Controls (n = 12) | Cases (n = 10) | Controls (n = 20) | |
| Maternal age (years) | 29 (27–31) | 29 (27–33) | 29 (27–31) | 30 (28–33) | 31 (27–35) | 30 (29–33) |
| BMI (kg/m2) | 33 (28–36) | 28 (26–33) | 30 (28–35) | 30 (25–34) | 31 (29–33) | 24 (22–26) |
| Caucasian | 12 (100%) | 12 (100%) | 11 (92%) | 12 (100%) | 9 (90%) | 20 (100%) |
| Gestational age at birth | 34 (29–36) | 39 (38–40) | 34 (30–35) | 40 (40–41) | 35 (33–36) | 40 (39–41) |
| Preeclampsia | 12 (100%) | 0 (0%) | 12 (100%) | 0 (0%) | 9 (90%) | 0 (0%) |
| Fetal growth restriction | 6 (50%) | 1 (8%) | 2 (17%) | 2 (17%) | 4 (40%) | 0 (0%) |
| Protein Accession | Gene Name | Protein Description | Ratio | p-Value | Significance |
|---|---|---|---|---|---|
| P04217 | A1BG | Alpha-1B-glycoprotein | 4.85 | 0.00000 | *** |
| P43652 | AFM | Afamin | 6.89 | 0.00001 | *** |
| P25311 | AZGP1 | Zinc-alpha-2-glycoprotein | 14.39 | 0.00005 | *** |
| P01024 | C3 | Complement C3 | 1.92 | 0.01029 | * |
| P00915 | CA1 | Carbonic anydrase 1 | 6.20 | 0.03347 | * |
| P00450 | CP | Ceruloplasmin | 6.55 | 0.00005 | *** |
| P02774 | GC | Vitamin D-binding protein | 11.31 | 0.00001 | *** |
| P19823 | ITIH2 | Inter-alpha-trypsin inhibitor heavy chain 2 | 6.35 | 0.01660 | * |
| P02763 | ORM1 | Alpha-1-acid-glycoprotein 1 | 2.96 | 0.06649 | |
| P19652 | ORM2 | Alpha-1-acid-glycoprotein 2 | 1.66 | 0.28634 | |
| P01009 | SERPINA1 | Alpha-1-antitrypsin (serpin A1) | 9.50 | 0.01026 | * |
| P01011 | SERPINA3 | Alpha-1-antichymotrypsin (serpin A3) | 3.83 | 0.00011 | ** |
| P08185 | SERPINA6 | Corticosteroid-binding globulin (serpin A6) | 2.27 | 0.00039 | ** |
| P05543 | SERPINA7 | Thyroxine-binding globulin (serpin A7) | 16.42 | 0.00013 | ** |
| P01008 | SERPINC1 | Antithrombin-III (serpin C1) | 4.38 | 0.00000 | *** |
| I3L145 | SHBG | Sex-hormone-binding globulin | 4.35 | 0.00000 | *** |
| P02766 | TTR | Transthyretin | 4.32 | 0.00000 | *** |
| P02768 | ALB | Albumin | 2.57 | 0.00001 | *** |
| P69905 | HBA1 | Hemoglobin subunit alpha 1 | 3.74 | 0.02510 | * |
| P68871 | HBB | Hemoglobin subunit beta | 24.62 | 0.00004 | *** |
| P02787 | TF | Serotransferrin | 2.82 | 0.02372 | * |
| 20–24 Weeks | 30–34 Weeks | |||||
|---|---|---|---|---|---|---|
| Gene Name | Ratio PE/CTL | p-Value | Significance | Ratio PE/CTL | p-Value | Significance |
| SERPINA7 | 1.42 | 0.04247 | * | 1.62 | 0.00966 | ** |
| CP | 1.81 | 0.04515 | * | 4.87 | 0.01784 | * |
| AFM | 1.29 | 0.33745 | 2.48 | 0.01821 | * | |
| ITIH2 | 1.14 | 0.66046 | 3.67 | 0.02808 | * | |
| TF | 1.86 | 0.27263 | 8.42 | 0.03446 | * | |
| A1BG | 1.19 | 0.50528 | 2.22 | 0.04651 | * | |
| SERPINA3 | 1.39 | 0.22978 | 1.95 | 0.05920 | ||
| GC | 1.20 | 0.28638 | 1.97 | 0.06296 | ||
| ALB | 1.49 | 0.20602 | 5.54 | 0.06954 | ||
| SERPINA1 | 1.36 | 0.24731 | 4.11 | 0.07165 | ||
| C3 | 1.07 | 0.85042 | 1.63 | 0.07776 | ||
| ORM1 | 1.69 | 0.42028 | 2.52 | 0.07781 | ||
| SERPINA6 | 1.05 | 0.84649 | 1.97 | 0.08995 | ||
| ORM2 | 1.35 | 0.49657 | 1.52 | 0.19926 | ||
| TTR | 1.23 | 0.29396 | 1.48 | 0.21370 | ||
| HBA1 | 5.27 | 0.01524 | * | 55.40 | 0.30338 | |
| HBB | 5.43 | 0.02956 | * | 30.91 | 0.33029 | |
| SERPINC1 | 0.99 | 0.97216 | 1.28 | 0.34586 | ||
| AZGP1 | 1.44 | 0.59655 | 1.19 | 0.61454 | ||
| CA1 | 0.62 | 0.55159 | 0.70 | 0.63019 | ||
| SHBG | 0.92 | 0.58530 | 1.07 | 0.72452 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bujold, E.; Fillion, A.; Roux-Dalvai, F.; Scott-Boyer, M.P.; Giguère, Y.; Forest, J.-C.; Gotti, C.; Laforest, G.; Guerby, P.; Droit, A. Proteomic Analysis of Maternal Urine for the Early Detection of Preeclampsia and Fetal Growth Restriction. J. Clin. Med. 2021, 10, 4679. https://doi.org/10.3390/jcm10204679
Bujold E, Fillion A, Roux-Dalvai F, Scott-Boyer MP, Giguère Y, Forest J-C, Gotti C, Laforest G, Guerby P, Droit A. Proteomic Analysis of Maternal Urine for the Early Detection of Preeclampsia and Fetal Growth Restriction. Journal of Clinical Medicine. 2021; 10(20):4679. https://doi.org/10.3390/jcm10204679
Chicago/Turabian StyleBujold, Emmanuel, Alexandre Fillion, Florence Roux-Dalvai, Marie Pier Scott-Boyer, Yves Giguère, Jean-Claude Forest, Clarisse Gotti, Geneviève Laforest, Paul Guerby, and Arnaud Droit. 2021. "Proteomic Analysis of Maternal Urine for the Early Detection of Preeclampsia and Fetal Growth Restriction" Journal of Clinical Medicine 10, no. 20: 4679. https://doi.org/10.3390/jcm10204679
APA StyleBujold, E., Fillion, A., Roux-Dalvai, F., Scott-Boyer, M. P., Giguère, Y., Forest, J.-C., Gotti, C., Laforest, G., Guerby, P., & Droit, A. (2021). Proteomic Analysis of Maternal Urine for the Early Detection of Preeclampsia and Fetal Growth Restriction. Journal of Clinical Medicine, 10(20), 4679. https://doi.org/10.3390/jcm10204679






