Updates on the Current Treatments for Diabetic Retinopathy and Possibility of Future Oral Therapy
Abstract
1. Introduction
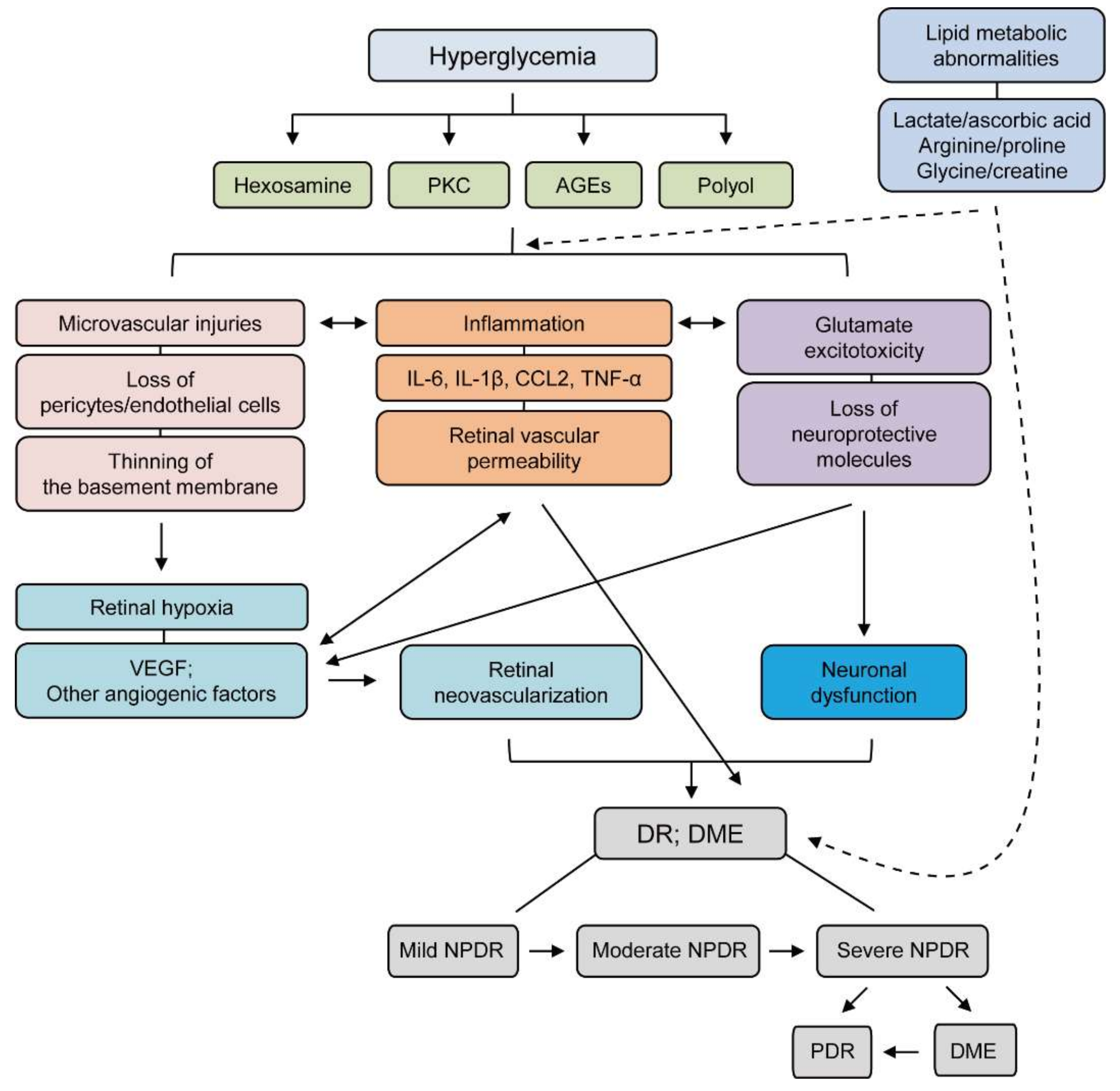
2. Pathophysiology of DR
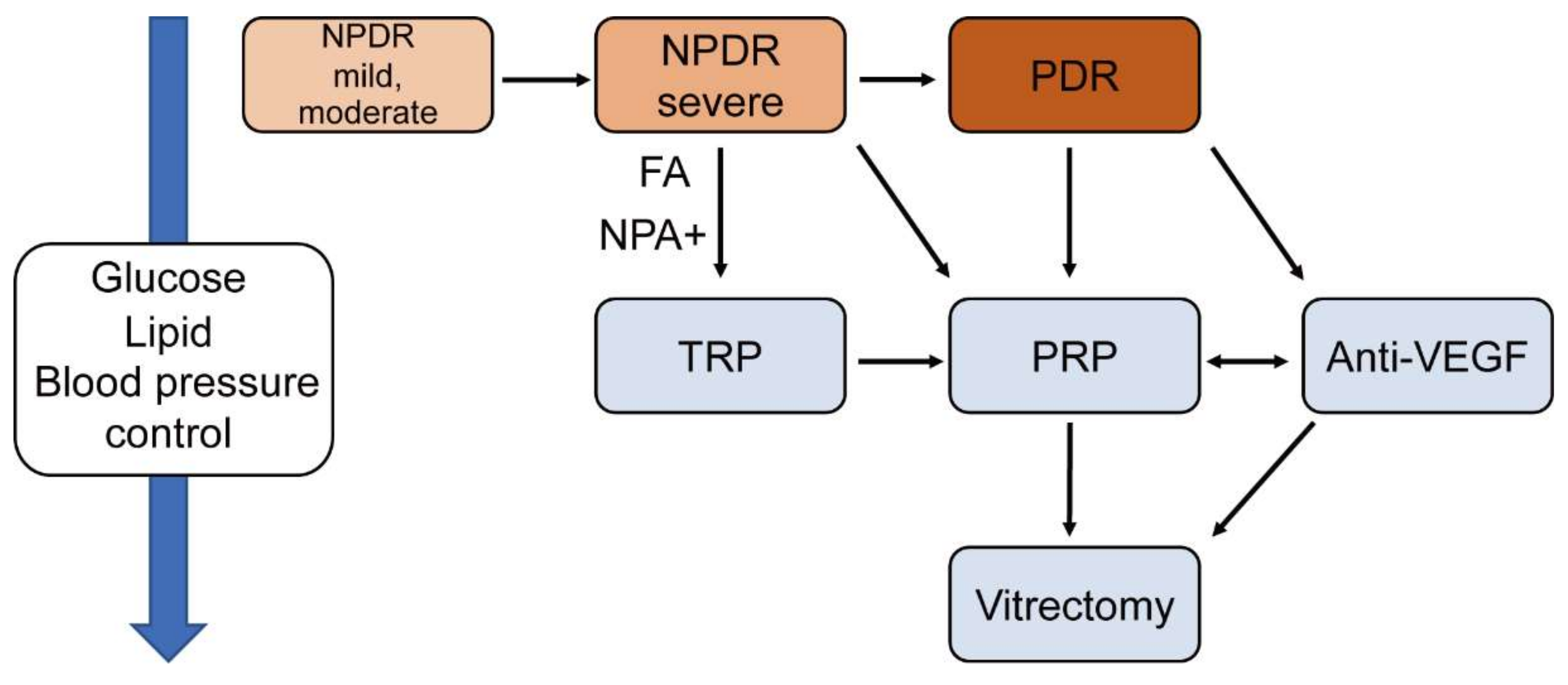
3. Laser Treatment
3.1. Treatment for DR
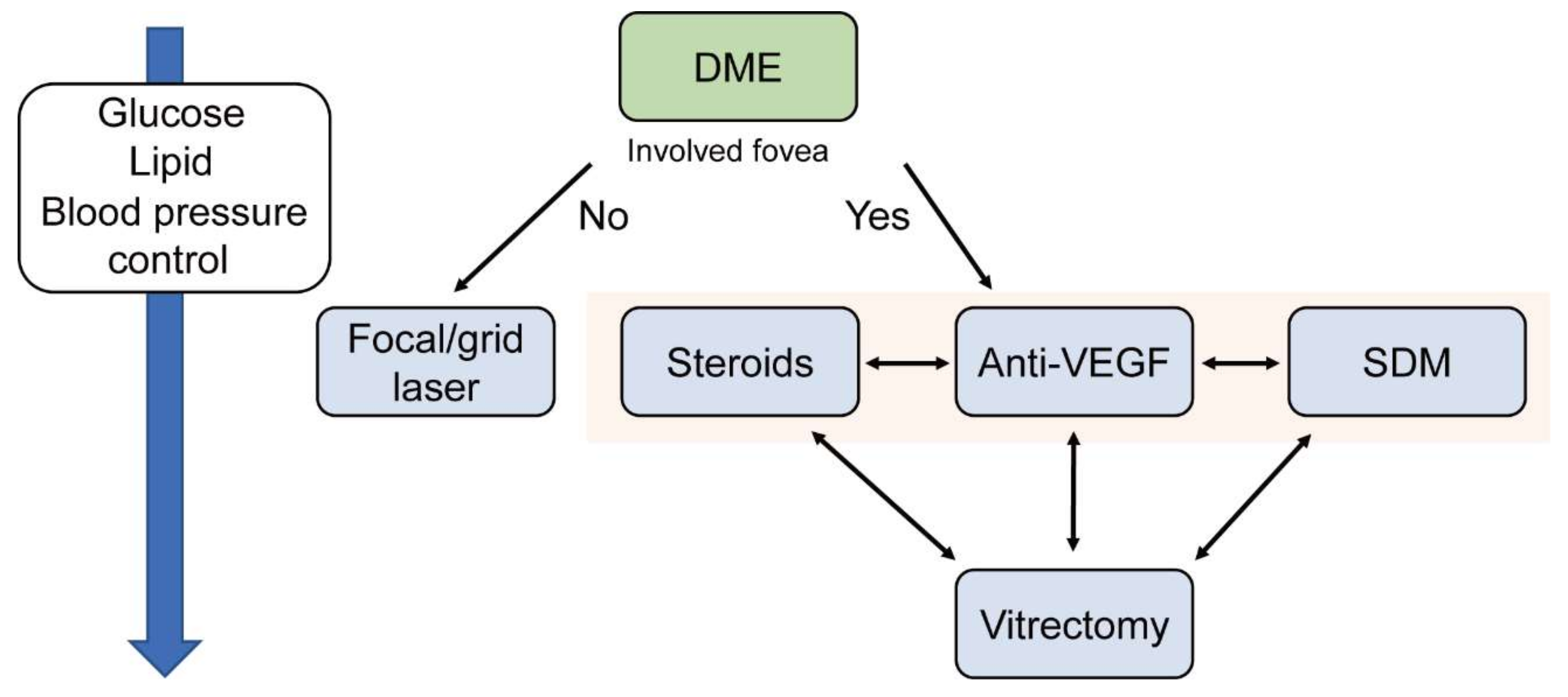
3.2. Treatment for DME
4. Anti-VEGF Treatment
4.1. Treatment for DR
4.2. Treatment for DME
5. Steroid Treatment
Treatment for DME
6. Surgical Treatment
6.1. Treatment for DR
6.2. Treatment for DME
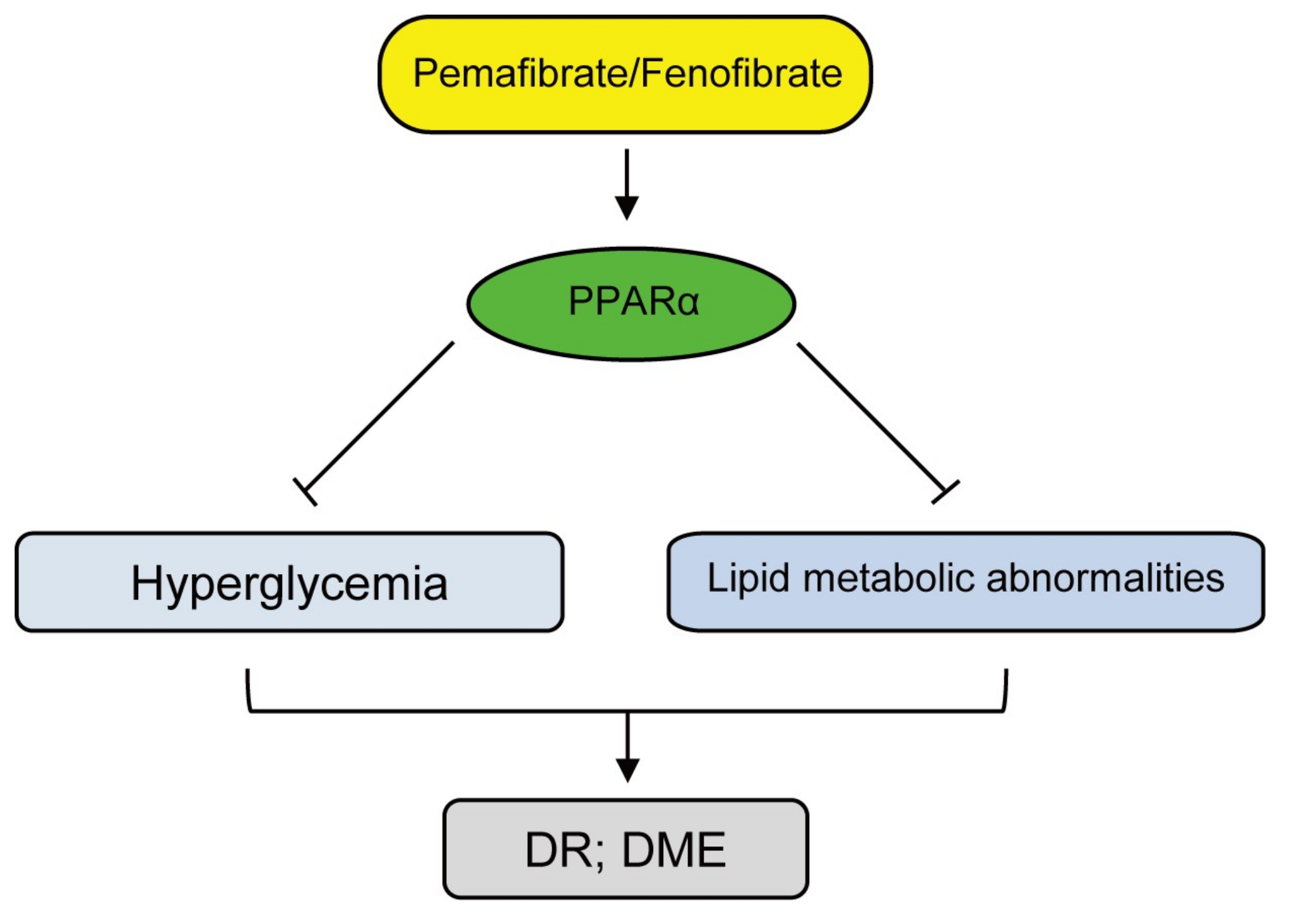
7. Fenofibrate Therapy in DR
8. Pemafibrate Therapy in DR
9. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bourne, R.R.A.; Flaxman, S.R.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; Leasher, J.; Limburg, H.; et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: A systematic review and meta-analysis. Lancet Glob. Health 2017, 5, e888–e897. [Google Scholar] [CrossRef]
- Leasher, J.L.; Bourne, R.R.; Flaxman, S.R.; Jonas, J.B.; Keeffe, J.; Naidoo, K.; Pesudovs, K.; Price, H.; White, R.A.; Wong, T.Y.; et al. Global Estimates on the Number of People Blind or Visually Impaired by Diabetic Retinopathy: A Meta-analysis from 1990 to 2010. Diabetes Care 2016, 39, 1643–1649. [Google Scholar] [CrossRef] [PubMed]
- Zietz, B.; Kasparbauer, A.; Ottmann, S.; Spiegel, D.; Palitzsch, K.D. Diabetic retinopathy and associated risk factors in type-1 and type-2 diabetics in the Upper Palatinate. Dtsch. Med. Wochenschr. 2000, 125, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Matuszewski, W.; Baranowska-Jurkun, A.; Stefanowicz-Rutkowska, M.M.; Modzelewski, R.; Pieczynski, J.; Bandurska-Stankiewicz, E. Prevalence of Diabetic Retinopathy in Type 1 and Type 2 Diabetes Mellitus Patients in North-East Poland. Medicine 2020, 56, 164. [Google Scholar] [CrossRef]
- Stewart, M.W. Socioeconomic Cost of Diabetic Retinopathy and Therapy. In Diabetic Retinopathy: Current Pharmacologic Treatment and Emerging Strategies; Stewart, M.W., Ed.; Springer: Singapore, 2017; pp. 257–268. [Google Scholar] [CrossRef]
- Orji, A.; Rani, P.K.; Narayanan, R.; Sahoo, N.K.; Das, T. The economic burden of diabetic retinopathy care at a tertiary eye care center in South India. Indian J. Ophthalmol. 2021, 69, 666. [Google Scholar]
- Zhang, X.; Low, S.; Kumari, N.; Wang, J.; Ang, K.; Yeo, D.; Yip, C.C.; Tavintharan, S.; Sum, C.F.; Lim, S.C. Direct medical cost associated with diabetic retinopathy severity in type 2 diabetes in Singapore. PLoS ONE 2017, 12, e0180949. [Google Scholar] [CrossRef]
- Avidor, D.; Loewenstein, A.; Waisbourd, M.; Nutman, A. Cost-effectiveness of diabetic retinopathy screening programs using telemedicine: A systematic review. Cost Eff. Resour. Alloc. 2020, 18, 16. [Google Scholar] [CrossRef]
- Simó, R.; Hernández, C. Neurodegeneration in the diabetic eye: New insights and therapeutic perspectives. Trends Endocrinol. Metab. Tem. 2014, 25, 23–33. [Google Scholar] [CrossRef]
- Yamashita, S.; Masuda, D.; Matsuzawa, Y. Pemafibrate, a New Selective PPARα Modulator: Drug Concept and Its Clinical Applications for Dyslipidemia and Metabolic Diseases. Curr. Atheroscler. Rep. 2020, 22, 5. [Google Scholar] [CrossRef]
- Barot, M.; Gokulgandhi, M.R.; Patel, S.; Mitra, A.K. Microvascular complications and diabetic retinopathy: Recent advances and future implications. Future Med. Chem. 2013, 5, 301–314. [Google Scholar] [CrossRef]
- Lutty, G.A. Effects of diabetes on the eye. Investig. Ophthalmol. Vis. Sci. 2013, 54, ORSF81. [Google Scholar] [CrossRef]
- Tomita, Y.; Lee, D.; Tsubota, K.; Kurihara, T. PPARα Agonist Oral Therapy in Diabetic Retinopathy. Biomedicines 2020, 8, 433. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Lo, A.C.Y. Diabetic Retinopathy: Pathophysiology and Treatments. Int. J. Mol. Sci. 2018, 19, 1816. [Google Scholar] [CrossRef]
- Bergers, G.; Song, S. The role of pericytes in blood-vessel formation and maintenance. Neuro-Oncology 2005, 7, 452–464. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Ge, H.M.; Liu, B.H.; Dong, R.; Shan, K.; Chen, X.; Yao, M.D.; Li, X.M.; Yao, J.; Zhou, R.M.; et al. Targeting pericyte-endothelial cell crosstalk by circular RNA-cPWWP2A inhibition aggravates diabetes-induced microvascular dysfunction. Proc. Natl. Acad. Sci. USA 2019, 116, 7455–7464. [Google Scholar] [CrossRef] [PubMed]
- Naruse, K.; Nakamura, J.; Hamada, Y.; Nakayama, M.; Chaya, S.; Komori, T.; Kato, K.; Kasuya, Y.; Miwa, K.; Hotta, N. Aldose reductase inhibition prevents glucose-induced apoptosis in cultured bovine retinal microvascular pericytes. Exp. Eye Res. 2000, 71, 309–315. [Google Scholar] [CrossRef]
- Romeo, G.; Liu, W.H.; Asnaghi, V.; Kern, T.S.; Lorenzi, M. Activation of nuclear factor-kappaB induced by diabetes and high glucose regulates a proapoptotic program in retinal pericytes. Diabetes 2002, 51, 2241–2248. [Google Scholar] [CrossRef]
- Beltramo, E.; Porta, M. Pericyte loss in diabetic retinopathy: Mechanisms and consequences. Curr. Med. Chem. 2013, 20, 3218–3225. [Google Scholar] [CrossRef]
- Bianchi, E.; Ripandelli, G.; Taurone, S.; Feher, J.; Plateroti, R.; Kovacs, I.; Magliulo, G.; Orlando, M.P.; Micera, A.; Battaglione, E.; et al. Age and diabetes related changes of the retinal capillaries: An ultrastructural and immunohistochemical study. Int. J. Immunopathol. Pharm. 2016, 29, 40–53. [Google Scholar] [CrossRef]
- Aiello, L.P.; Wong, J.-S. Role of vascular endothelial growth factor in diabetic vascular complications. Kidney Int. 2000, 58, S113–S119. [Google Scholar] [CrossRef]
- Selim, K.M.; Sahan, D.; Muhittin, T.; Osman, C.; Mustafa, O. Increased levels of vascular endothelial growth factor in the aqueous humor of patients with diabetic retinopathy. Indian J. Ophthalmol. 2010, 58, 375. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Singh, R.P. The role of anti-vascular endothelial growth factor (anti-VEGF) in the management of proliferative diabetic retinopathy. Drugs Context 2018, 7, 212532. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Mansoor, S.; Sharma, A.; Sapkal, A.; Sheth, J.; Falatoonzadeh, P.; Kuppermann, B.; Kenney, M. Diabetic retinopathy and VEGF. Open Ophthalmol. J. 2013, 7, 4–10. [Google Scholar] [CrossRef]
- Roy, S.; Amin, S.; Roy, S. Retinal fibrosis in diabetic retinopathy. Exp. Eye Res. 2016, 142, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Ishibazawa, A.; Nagaoka, T.; Yokota, H.; Takahashi, A.; Omae, T.; Song, Y.S.; Takahashi, T.; Yoshida, A. Characteristics of Retinal Neovascularization in Proliferative Diabetic Retinopathy Imaged by Optical Coherence Tomography Angiography. Investig. Ophthalmol. Vis. Sci. 2016, 57, 6247–6255. [Google Scholar] [CrossRef]
- Cohen, S.R.; Gardner, T.W. Diabetic Retinopathy and Diabetic Macular Edema. Dev. Ophthalmol. 2016, 55, 137–146. [Google Scholar] [CrossRef]
- Huang, H.; He, J.; Johnson, D.; Wei, Y.; Liu, Y.; Wang, S.; Lutty, G.A.; Duh, E.J.; Semba, R.D. Deletion of placental growth factor prevents diabetic retinopathy and is associated with Akt activation and HIF1α-VEGF pathway inhibition. Diabetes 2015, 64, 200–212. [Google Scholar] [CrossRef] [PubMed]
- Campochiaro, P.A. Molecular pathogenesis of retinal and choroidal vascular diseases. Prog. Retin. Eye Res. 2015, 49, 67–81. [Google Scholar] [CrossRef]
- Kelly, B.D.; Hackett, S.F.; Hirota, K.; Oshima, Y.; Cai, Z.; Berg-Dixon, S.; Rowan, A.; Yan, Z.; Campochiaro, P.A.; Semenza, G.L. Cell type-specific regulation of angiogenic growth factor gene expression and induction of angiogenesis in nonischemic tissue by a constitutively active form of hypoxia-inducible factor 1. Circ. Res. 2003, 93, 1074–1081. [Google Scholar] [CrossRef]
- Kim, M.; Kim, Y.; Lee, S.J. Comparison of aqueous concentrations of angiogenic and inflammatory cytokines based on optical coherence tomography patterns of diabetic macular edema. Indian J. Ophthalmol. 2015, 63, 312–317. [Google Scholar] [CrossRef]
- Vujosevic, S.; Micera, A.; Bini, S.; Berton, M.; Esposito, G.; Midena, E. Proteome analysis of retinal glia cells-related inflammatory cytokines in the aqueous humour of diabetic patients. Acta Ophthalmol. 2016, 94, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Boss, J.D.; Singh, P.K.; Pandya, H.K.; Tosi, J.; Kim, C.; Tewari, A.; Juzych, M.S.; Abrams, G.W.; Kumar, A. Assessment of neurotrophins and inflammatory mediators in vitreous of patients with diabetic retinopathy. Investig. Ophthalmol. Vis. Sci. 2017, 58, 5594–5603. [Google Scholar] [CrossRef] [PubMed]
- Adamiec-Mroczek, J.; Oficjalska-Młyńczak, J.; Misiuk-Hojło, M. Proliferative diabetic retinopathy-The influence of diabetes control on the activation of the intraocular molecule system. Diabetes Res. Clin. Pract. 2009, 84, 46–50. [Google Scholar] [CrossRef]
- Bromberg-White, J.L.; Glazer, L.; Downer, R.; Furge, K.; Boguslawski, E.; Duesbery, N.S. Identification of VEGF-independent cytokines in proliferative diabetic retinopathy vitreous. Investig. Ophthalmol. Vis. Sci. 2013, 54, 6472–6480. [Google Scholar] [CrossRef]
- Mao, C.; Yan, H. Roles of elevated intravitreal IL-1β and IL-10 levels in proliferative diabetic retinopathy. Indian J. Ophthalmol. 2014, 62, 699. [Google Scholar]
- Ghodasra, D.H.; Fante, R.; Gardner, T.W.; Langue, M.; Niziol, L.M.; Besirli, C.; Cohen, S.R.; Dedania, V.S.; Demirci, H.; Jain, N.; et al. Safety and Feasibility of Quantitative Multiplexed Cytokine Analysis From Office-Based Vitreous Aspiration. Investig. Ophthalmol. Vis. Sci. 2016, 57, 3017–3023. [Google Scholar] [CrossRef]
- Wu, H.; Hwang, D.K.; Song, X.; Tao, Y. Association between Aqueous Cytokines and Diabetic Retinopathy Stage. J. Ophthalmol. 2017, 2017, 9402198. [Google Scholar] [CrossRef]
- Funatsu, H.; Yamashita, H.; Sakata, K.; Noma, H.; Mimura, T.; Suzuki, M.; Eguchi, S.; Hori, S. Vitreous levels of vascular endothelial growth factor and intercellular adhesion molecule 1 are related to diabetic macular edema. Ophthalmology 2005, 112, 806–816. [Google Scholar] [CrossRef]
- Vujosevic, S.; Micera, A.; Bini, S.; Berton, M.; Esposito, G.; Midena, E. Aqueous Humor Biomarkers of Müller Cell Activation in Diabetic Eyes. Investig. Ophthalmol. Vis. Sci. 2015, 56, 3913–3918. [Google Scholar] [CrossRef] [PubMed]
- Feenstra, D.J.; Yego, E.C.; Mohr, S. Modes of Retinal Cell Death in Diabetic Retinopathy. J. Clin. Exp. Ophthalmol. 2013, 4, 298. [Google Scholar] [CrossRef] [PubMed]
- Rübsam, A.; Parikh, S.; Fort, P.E. Role of Inflammation in Diabetic Retinopathy. Int. J. Mol. Sci. 2018, 19, 942. [Google Scholar] [CrossRef]
- Mohr, S.; Xi, X.; Tang, J.; Kern, T.S. Caspase Activation in Retinas of Diabetic and Galactosemic Mice and Diabetic Patients. Diabetes 2002, 51, 1172. [Google Scholar] [CrossRef] [PubMed]
- Podestà, F.; Romeo, G.; Liu, W.-H.; Krajewski, S.; Reed, J.C.; Gerhardinger, C.; Lorenzi, M. Bax Is Increased in the Retina of Diabetic Subjects and Is Associated with Pericyte Apoptosis in Vivo and in Vitro. Am. J. Pathol. 2000, 156, 1025–1032. [Google Scholar] [CrossRef]
- Kowluru, R.A.; Koppolu, P. Diabetes-induced Activation of Caspase-3 in Retina: Effect of Antioxidant Therapy. Free Radic. Res. 2002, 36, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Dornan, T.L.; Carter, R.D.; Bron, A.J.; Turner, R.C.; Mann, J.I. Low density lipoprotein cholesterol: An association with the severity of diabetic retinopathy. Diabetologia 1982, 22, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Kissebah, A.H.; Kohner, E.M.; Lewis, B.; Siddiq, Y.K.; Lowy, C.; Fraser, T.R. Plasma-lipids and glucose/insulin relationship in non-insulin-requiring diabetics with and without retinopathy. Lancet 1975, 1, 1104–1108. [Google Scholar] [CrossRef]
- Eckel, R.H.; McLean, E.; Albers, J.J.; Cheung, M.C.; Bierman, E.L. Plasma lipids and microangiopathy in insulin-dependent diabetes mellitus. Diabetes Care 1981, 4, 447–453. [Google Scholar] [CrossRef]
- Mohan, R.; Mohan, V.; Susheela, L.; Ramachandran, A.; Viswanathan, M. Increased LDL cholesterol in non-insulin-dependent diabetics with maculopathy. Acta Diabetol. Lat. 1984, 21, 85–89. [Google Scholar]
- Chakraborty, A.; Mondal, P.R.; Kundu, S.C.; Batabyal, S.K. Serum lipids and lipoproteins in diabetic retinopathy. J. Assoc. Physicians India 1986, 34, 631–632. [Google Scholar]
- Chew, E.Y.; Klein, M.L.; Ferris, F.L., III; Remaley, N.A.; Murphy, R.P.; Chantry, K.; Hoogwerf, B.J.; Miller, D. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Arch. Ophthalmol. 1996, 114, 1079–1084. [Google Scholar] [CrossRef]
- Sasongko, M.B.; Wong, T.Y.; Nguyen, T.T.; Kawasaki, R.; Jenkins, A.; Shaw, J.; Wang, J.J. Serum apolipoprotein AI and B are stronger biomarkers of diabetic retinopathy than traditional lipids. Diabetes Care 2011, 34, 474–479. [Google Scholar] [CrossRef]
- Reaven, G.M.; Chen, Y.D. Role of insulin in regulation of lipoprotein metabolism in diabetes. Diabetes/Metab. Rev. 1988, 4, 639–652. [Google Scholar] [CrossRef]
- Goff, D.C., Jr.; D’Agostino, R.B., Jr.; Haffner, S.M.; Otvos, J.D. Insulin resistance and adiposity influence lipoprotein size and subclass concentrations. Results from the Insulin Resistance Atherosclerosis Study. Metab. Clin. Exp. 2005, 54, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Ginsberg, H.N.; Zhang, Y.L.; Hernandez-Ono, A. Regulation of plasma triglycerides in insulin resistance and diabetes. Arch. Med. Res. 2005, 36, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Hermans, M.P.; Fioretto, P.; Valensi, P.; Davis, T.; Horton, E.; Wanner, C.; Al-Rubeaan, K.; Aronson, R.; Barzon, I.; et al. Association between plasma triglycerides and high-density lipoprotein cholesterol and microvascular kidney disease and retinopathy in type 2 diabetes mellitus: A global case-control study in 13 countries. Circulation 2014, 129, 999–1008. [Google Scholar] [CrossRef] [PubMed]
- Cetin, E.N.; Bulgu, Y.; Ozdemir, S.; Topsakal, S.; Akın, F.; Aybek, H.; Yıldırım, C. Association of serum lipid levels with diabetic retinopathy. Int. J. Ophthalmol. 2013, 6, 346–349. [Google Scholar] [CrossRef] [PubMed]
- Hammer, S.S.; Busik, J.V. The role of dyslipidemia in diabetic retinopathy. Vis. Res. 2017, 139, 228–236. [Google Scholar] [CrossRef]
- Chang, Y.-C.; Wu, W.-C. Dyslipidemia and diabetic retinopathy. Rev. Diabet. Stud. 2013, 10, 121–132. [Google Scholar] [CrossRef]
- Barba, I.; Garcia-Ramirez, M.; Hernandez, C.; Alonso, M.A.; Masmiquel, L.; Garcia-Dorado, D.; Simo, R. Metabolic fingerprints of proliferative diabetic retinopathy: An 1H-NMR-based metabonomic approach using vitreous humor. Investig. Ophthalmol. Vis. Sci. 2010, 51, 4416–4421. [Google Scholar] [CrossRef] [PubMed]
- Paris, L.P.; Johnson, C.H.; Aguilar, E.; Usui, Y.; Cho, K.; Hoang, L.T.; Feitelberg, D.; Benton, H.P.; Westenskow, P.D.; Kurihara, T.; et al. Global metabolomics reveals metabolic dysregulation in ischemic retinopathy. Metabolomics 2016, 12, 15. [Google Scholar] [CrossRef]
- Haines, N.R.; Manoharan, N.; Olson, J.L.; D’Alessandro, A.; Reisz, J.A. Metabolomics Analysis of Human Vitreous in Diabetic Retinopathy and Rhegmatogenous Retinal Detachment. J. Proteome Res. 2018, 17, 2421–2427. [Google Scholar] [CrossRef]
- Tomita, Y.; Cagnone, G.; Fu, Z.; Cakir, B.; Kotoda, Y.; Asakage, M.; Wakabayashi, Y.; Hellstrom, A.; Joyal, J.S.; Talukdar, S.; et al. Vitreous metabolomics profiling of proliferative diabetic retinopathy. Diabetologia 2021, 64, 70–82. [Google Scholar] [CrossRef] [PubMed]
- Diabetic Retinopathy Study Research Group. Four risk factors for severe visual loss in diabetic retinopathy. The third report from the Diabetic Retinopathy Study. The Diabetic Retinopathy Study Research Group. Arch. Ophthalmol. 1979, 97, 654–655. [Google Scholar] [CrossRef]
- Diabetic Retinopathy Study Research Group. Indications for photocoagulation treatment of diabetic retinopathy: Diabetic Retinopathy Study Report no. 14. The Diabetic Retinopathy Study Research Group. Int. Ophthalmol. Clin. 1987, 27, 239–253. [Google Scholar] [CrossRef]
- Early Treatment Diabetic Retinopathy Study Research Group. Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report no. 3. The Early Treatment Diabetic Retinopathy Study Research Group. Int. Ophthalmol. Clin. 1987, 27, 254–264. [Google Scholar] [CrossRef]
- Gozawa, M.; Takamura, Y.; Miyake, S.; Matsumura, T.; Morioka, M.; Yamada, Y.; Inatani, M. Photocoagulation of the Retinal Nonperfusion Area Prevents the Expression of the Vascular Endothelial Growth Factor in an Animal Model. Investig. Ophthalmol. Vis. Sci. 2017, 58, 5946–5953. [Google Scholar] [CrossRef] [PubMed]
- Aiello, L.P.; Avery, R.L.; Arrigg, P.G.; Keyt, B.A.; Jampel, H.D.; Shah, S.T.; Pasquale, L.R.; Thieme, H.; Iwamoto, M.A.; Park, J.E.; et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N. Engl. J. Med. 1994, 331, 1480–1487. [Google Scholar] [CrossRef] [PubMed]
- Early Treatment Diabetic Retinopathy Study Research Group. Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics. ETDRS report number 7. Ophthalmology 1991, 98, 741–756. [Google Scholar] [CrossRef]
- Chew, E.Y.; Ferris, F.L., III; Csaky, K.G.; Murphy, R.P.; Agron, E.; Thompson, D.J.; Reed, G.F.; Schachat, A.P. The long-term effects of laser photocoagulation treatment in patients with diabetic retinopathy: The early treatment diabetic retinopathy follow-up study. Ophthalmology 2003, 110, 1683–1689. [Google Scholar] [CrossRef]
- Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology 1981, 88, 583–600. [Google Scholar]
- Striph, G.G.; Hart, W.M., Jr.; Olk, R.J. Modified grid laser photocoagulation for diabetic macular edema. The effect on the central visual field. Ophthalmology 1988, 95, 1673–1679. [Google Scholar] [CrossRef]
- Sims, L.M.; Stoessel, K.; Thompson, J.T.; Hirsch, J. Assessment of visual-field changes before and after focal photocoagulation for clinically significant diabetic macular edema. Ophthalmologica 1990, 200, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Seiberth, V.; Alexandridis, E.; Feng, W. Function of the diabetic retina after panretinal argon laser coagulation. Graefes. Arch. Clin. Exp. Ophthalmol. 1987, 225, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Golden, M.P.; Russell, B.P.; Ingersoll, G.M.; Gray, D.L.; Hummer, K.M. Management of diabetes mellitus in children younger than 5 years of age. Am. J. Dis. Child. 1985, 139, 448–452. [Google Scholar] [CrossRef]
- Blumenkranz, M.S.; Yellachich, D.; Andersen, D.E.; Wiltberger, M.W.; Mordaunt, D.; Marcellino, G.R.; Palanker, D. Semiautomated patterned scanning laser for retinal photocoagulation. Retina 2006, 26, 370–376. [Google Scholar] [CrossRef]
- Takamura, Y.; Arimura, S.; Miyake, S.; Matsumura, T.; Gozawa, M.; Iwasaki, K.; Inatani, M. Panretinal Photocoagulation Using Short-Pulse Laser Induces Less Inflammation and Macular Thickening in Patients with Diabetic Retinopathy. J. Ophthalmol. 2017, 2017, 8530261. [Google Scholar] [CrossRef]
- Iwase, T.; Ueno, Y.; Ra, E.; Ito, Y.; Terasaki, H. Changes in choriocapillaris and retinal morphology after laser photocoagulation by OCT angiography: A case report. Medicine 2018, 97, e13278. [Google Scholar] [CrossRef]
- Sanghvi, C.; McLauchlan, R.; Delgado, C.; Young, L.; Charles, S.J.; Marcellino, G.; Stanga, P.E. Initial experience with the Pascal photocoagulator: A pilot study of 75 procedures. Br. J. Ophthalmol. 2008, 92, 1061–1064. [Google Scholar] [CrossRef]
- Lavinsky, D.; Cardillo, J.A.; Mandel, Y.; Huie, P.; Melo, L.A.; Farah, M.E.; Belfort, R.; Palanker, D. Restoration of retinal morphology and residual scarring after photocoagulation. Acta Ophthalmol. 2013, 91, e315–e323. [Google Scholar] [CrossRef]
- Chappelow, A.V.; Tan, K.; Waheed, N.K.; Kaiser, P.K. Panretinal photocoagulation for proliferative diabetic retinopathy: Pattern scan laser versus argon laser. Am. J. Ophthalmol. 2012, 153, 137–142.e132. [Google Scholar] [CrossRef] [PubMed]
- Japanese Society of Ophthalmic Diabetology, Subcommittee on the Study of Diabetic Retinopathy Treatment; Sato, Y.; Kojimahara, N.; Kitano, S.; Kato, S.; Ando, N.; Yamaguchi, N.; Hori, S. Multicenter randomized clinical trial of retinal photocoagulation for preproliferative diabetic retinopathy. JPN J. Ophthalmol. 2012, 56, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Nikkhah, H.; Ghazi, H.; Razzaghi, M.R.; Karimi, S.; Ramezani, A.; Soheilian, M. Extended targeted retinal photocoagulation versus conventional pan-retinal photocoagulation for proliferative diabetic retinopathy in a randomized clinical trial. Int. Ophthalmol. 2018, 38, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Chhablani, J.; Mathai, A.; Rani, P.; Gupta, V.; Arevalo, J.F.; Kozak, I. Comparison of conventional pattern and novel navigated panretinal photocoagulation in proliferative diabetic retinopathy. Investig. Ophthalmol. Vis. Sci. 2014, 55, 3432–3438. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brown, D.M.; Ou, W.C.; Wong, T.P.; Kim, R.Y.; Croft, D.E.; Wykoff, C.C.; DAVE Study Group. Targeted Retinal Photocoagulation for Diabetic Macular Edema with Peripheral Retinal Nonperfusion: Three-Year Randomized DAVE Trial. Ophthalmology 2018, 125, 683–690. [Google Scholar] [CrossRef]
- Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Arch. Ophthalmol. 1985, 103, 1796–1806. [Google Scholar]
- Early Treatment Diabetic Retinopathy Study Research Group. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 1987, 94, 761–774. [Google Scholar] [CrossRef]
- Fong, D.S.; Segal, P.P.; Myers, F.; Ferris, F.L.; Hubbard, L.D.; Davis, M.D. Subretinal fibrosis in diabetic macular edema. ETDRS report 23. Early Treatment Diabetic Retinopathy Study Research Group. Arch. Ophthalmol. 1997, 115, 873–877. [Google Scholar] [CrossRef]
- Writing Committee for the Diabetic Retinopathy Clinical Research Network; Fong, D.S.; Strauber, S.F.; Aiello, L.P.; Beck, R.W.; Callanan, D.G.; Danis, R.P.; Davis, M.D.; Feman, S.S.; Ferris, F.; et al. Comparison of the modified Early Treatment Diabetic Retinopathy Study and mild macular grid laser photocoagulation strategies for diabetic macular edema. Arch. Ophthalmol. 2007, 125, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Ohkoshi, K.; Yamaguchi, T. Subthreshold micropulse diode laser photocoagulation for diabetic macular edema in Japanese patients. Am. J. Ophthalmol. 2010, 149, 133–139. [Google Scholar] [CrossRef]
- Lavinsky, D.; Cardillo, J.A.; Melo, L.A., Jr.; Dare, A.; Farah, M.E.; Belfort, R., Jr. Randomized clinical trial evaluating mETDRS versus normal or high-density micropulse photocoagulation for diabetic macular edema. Investig. Ophthalmol. Vis. Sci. 2011, 52, 4314–4323. [Google Scholar] [CrossRef] [PubMed]
- Qiao, G.; Guo, H.K.; Dai, Y.; Wang, X.L.; Meng, Q.L.; Li, H.; Chen, X.H.; Chen, Z.L. Sub-threshold micro-pulse diode laser treatment in diabetic macular edema: A Meta-analysis of randomized controlled trials. Int. J. Ophthalmol. 2016, 9, 1020–1027. [Google Scholar] [CrossRef] [PubMed]
- Inagaki, K.; Hamada, M.; Ohkoshi, K. Minimally invasive laser treatment combined with intravitreal injection of anti-vascular endothelial growth factor for diabetic macular oedema. Sci. Rep. 2019, 9, 7585. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.K.; Glassman, A.R.; Beaulieu, W.T.; Stockdale, C.R.; Bressler, N.M.; Flaxel, C.; Gross, J.G.; Shami, M.; Jampol, L.M.; Diabetic Retinopathy Clinical Research Network. Rationale and Application of the Protocol S Anti-Vascular Endothelial Growth Factor Algorithm for Proliferative Diabetic Retinopathy. Ophthalmology 2019, 126, 87–95. [Google Scholar] [CrossRef]
- Gross, J.G.; Glassman, A.R.; Liu, D.; Sun, J.K.; Antoszyk, A.N.; Baker, C.W.; Bressler, N.M.; Elman, M.J.; Ferris, F.L., III; Gardner, T.W.; et al. Five-Year Outcomes of Panretinal Photocoagulation vs Intravitreous Ranibizumab for Proliferative Diabetic Retinopathy: A Randomized Clinical Trial. JAMA Ophthalmol. 2018, 136, 1138–1148. [Google Scholar] [CrossRef]
- Writing Committee for the Diabetic Retinopathy Clinical Research Network; Gross, J.G.; Glassman, A.R.; Jampol, L.M.; Inusah, S.; Aiello, L.P.; Antoszyk, A.N.; Baker, C.W.; Berger, B.B.; Bressler, N.M.; et al. Panretinal Photocoagulation vs Intravitreous Ranibizumab for Proliferative Diabetic Retinopathy: A Randomized Clinical Trial. JAMA 2015, 314, 2137–2146. [Google Scholar] [CrossRef]
- Sivaprasad, S.; Prevost, A.T.; Vasconcelos, J.C.; Riddell, A.; Murphy, C.; Kelly, J.; Bainbridge, J.; Tudor-Edwards, R.; Hopkins, D.; Hykin, P.; et al. Clinical efficacy of intravitreal aflibercept versus panretinal photocoagulation for best corrected visual acuity in patients with proliferative diabetic retinopathy at 52 weeks (CLARITY): A multicentre, single-blinded, randomised, controlled, phase 2b, non-inferiority trial. Lancet 2017, 389, 2193–2203. [Google Scholar] [CrossRef]
- Lang, G.E.; Stahl, A.; Voegeler, J.; Quiering, C.; Lorenz, K.; Spital, G.; Liakopoulos, S. Efficacy and safety of ranibizumab with or without panretinal laser photocoagulation versus laser photocoagulation alone in proliferative diabetic retinopathy—The PRIDE study. Acta Ophthalmol. 2019, 98, e530–e539. [Google Scholar] [CrossRef]
- Lang, G.E.; Stahl, A.; Voegeler, J.; Quiering, C.; Zaremba, L.; Lorenz, K.; Spital, G.; Liakopoulos, S. Observational outcomes in proliferative diabetic retinopathy patients following treatment with ranibizumab, panretinal laser photocoagulation or combination therapy—The non-interventional second year follow-up to the PRIDE study. Acta Ophthalmol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Obeid, A.; Su, D.; Patel, S.N.; Uhr, J.H.; Borkar, D.; Gao, X.; Fineman, M.S.; Regillo, C.D.; Maguire, J.I.; Garg, S.J.; et al. Outcomes of Eyes Lost to Follow-up with Proliferative Diabetic Retinopathy That Received Panretinal Photocoagulation versus Intravitreal Anti-Vascular Endothelial Growth Factor. Ophthalmology 2019, 126, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Diabetic Retinopathy Clinical Research Network; Elman, M.J.; Aiello, L.P.; Beck, R.W.; Bressler, N.M.; Bressler, S.B.; Edwards, A.R.; Ferris, F.L., III; Friedman, S.M.; Glassman, A.R.; et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 2010, 117, 1064–1077.e35. [Google Scholar] [CrossRef]
- Mitchell, P.; Bandello, F.; Schmidt-Erfurth, U.; Lang, G.E.; Massin, P.; Schlingemann, R.O.; Sutter, F.; Simader, C.; Burian, G.; Gerstner, O.; et al. The RESTORE study: Ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 2011, 118, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Q.D.; Brown, D.M.; Marcus, D.M.; Boyer, D.S.; Patel, S.; Feiner, L.; Gibson, A.; Sy, J.; Rundle, A.C.; Hopkins, J.J.; et al. Ranibizumab for diabetic macular edema: Results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012, 119, 789–801. [Google Scholar] [CrossRef] [PubMed]
- Korobelnik, J.F.; Do, D.V.; Schmidt-Erfurth, U.; Boyer, D.S.; Holz, F.G.; Heier, J.S.; Midena, E.; Kaiser, P.K.; Terasaki, H.; Marcus, D.M.; et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology 2014, 121, 2247–2254. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.M.; Schmidt-Erfurth, U.; Do, D.V.; Holz, F.G.; Boyer, D.S.; Midena, E.; Heier, J.S.; Terasaki, H.; Kaiser, P.K.; Marcus, D.M.; et al. Intravitreal Aflibercept for Diabetic Macular Edema: 100-Week Results From the VISTA and VIVID Studies. Ophthalmology 2015, 122, 2044–2052. [Google Scholar] [CrossRef]
- Diabetic Retinopathy Clinical Research Network; Wells, J.A.; Glassman, A.R.; Ayala, A.R.; Jampol, L.M.; Aiello, L.P.; Antoszyk, A.N.; Arnold-Bush, B.; Baker, C.W.; Bressler, N.M.; et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N. Engl. J. Med. 2015, 372, 1193–1203. [Google Scholar] [CrossRef]
- Wells, J.A.; Glassman, A.R.; Ayala, A.R.; Jampol, L.M.; Bressler, N.M.; Bressler, S.B.; Brucker, A.J.; Ferris, F.L.; Hampton, G.R.; Jhaveri, C.; et al. Aflibercept, Bevacizumab, or Ranibizumab for Diabetic Macular Edema: Two-Year Results from a Comparative Effectiveness Randomized Clinical Trial. Ophthalmology 2016, 123, 1351–1359. [Google Scholar] [CrossRef]
- Cai, S.; Bressler, N.M. Aflibercept, bevacizumab or ranibizumab for diabetic macular oedema: Recent clinically relevant findings from DRCR.net Protocol T. Curr. Opin. Ophthalmol. 2017, 28, 636–643. [Google Scholar] [CrossRef]
- Hirano, T.; Toriyama, Y.; Iesato, Y.; Imai, A.; Hirabayashi, K.; Nagaoka, T.; Takamura, Y.; Sugimoto, M.; Murata, T. Effect of leaking perifoveal microaneurysms on resolution of diabetic macular edema treated by combination therapy using anti-vascular endothelial growth factor and short pulse focal/grid laser photocoagulation. JPN J. Ophthalmol. 2017, 61, 51–60. [Google Scholar] [CrossRef]
- Fintak, D.R.; Shah, G.K.; Blinder, K.J.; Regillo, C.D.; Pollack, J.; Heier, J.S.; Hollands, H.; Sharma, S. Incidence of endophthalmitis related to intravitreal injection of bevacizumab and ranibizumab. Retina 2008, 28, 1395–1399. [Google Scholar] [CrossRef]
- Hernandez-Pastor, L.J.; Ortega, A.; Garcia-Layana, A.; Giraldez, J. Ranibizumab for neovascular age-related macular degeneration. Am. J. Health Syst. Pharm. 2008, 65, 1805–1814. [Google Scholar] [CrossRef]
- Pearson, P.A.; Comstock, T.L.; Ip, M.; Callanan, D.; Morse, L.S.; Ashton, P.; Levy, B.; Mann, E.S.; Eliott, D. Fluocinolone acetonide intravitreal implant for diabetic macular edema: A 3-year multicenter, randomized, controlled clinical trial. Ophthalmology 2011, 118, 1580–1587. [Google Scholar] [CrossRef]
- Martidis, A.; Duker, J.S.; Greenberg, P.B.; Rogers, A.H.; Puliafito, C.A.; Reichel, E.; Baumal, C. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology 2002, 109, 920–927. [Google Scholar] [CrossRef]
- Jonas, J.B.; Sofker, A.; Hayler, J.; Degenring, R.F. Intravitreal crystalline triamcinolone acetonide as an additional tool in pars plana vitrectomy for complicated proliferative vitreoretinopathy? Acta Ophthalmol. Scand. 2003, 81, 663–665. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.; Lee, W.K. Effect of intravitreal triamcinolone in diabetic macular edema unresponsive to intravitreal bevacizumab. Retina 2014, 34, 1606–1611. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, T.G.; Lew, Y.J. Short-term efficacy of intravitreal triamcinolone acetonide for bevacizumab-resistant diabetic macular oedema. Acta Ophthalmol. 2015, 93, e178–e179. [Google Scholar] [CrossRef] [PubMed]
- Ahmadieh, H.; Ramezani, A.; Shoeibi, N.; Bijanzadeh, B.; Tabatabaei, A.; Azarmina, M.; Soheilian, M.; Keshavarzi, G.; Mohebbi, M.R. Intravitreal bevacizumab with or without triamcinolone for refractory diabetic macular edema; a placebo-controlled, randomized clinical trial. Graefes. Arch. Clin. Exp. Ophthalmol. 2008, 246, 483–489. [Google Scholar] [CrossRef]
- Entezari, M.; Ahmadieh, H.; Dehghan, M.H.; Ramezani, A.; Bassirnia, N.; Anissian, A. Posterior sub-tenon triamcinolone for refractory diabetic macular edema: A randomized clinical trial. Eur. J. Ophthalmol. 2005, 15, 746–750. [Google Scholar] [CrossRef] [PubMed]
- Bakri, S.J.; Kaiser, P.K. Posterior subtenon triamcinolone acetonide for refractory diabetic macular edema. Am. J. Ophthalmol. 2005, 139, 290–294. [Google Scholar] [CrossRef]
- Choi, Y.J.; Oh, I.K.; Oh, J.R.; Huh, K. Intravitreal versus posterior subtenon injection of triamcinolone acetonide for diabetic macular edema. Korean J. Ophthalmol. 2006, 20, 205–209. [Google Scholar] [CrossRef]
- Qi, H.P.; Bi, S.; Wei, S.Q.; Cui, H.; Zhao, J.B. Intravitreal versus subtenon triamcinolone acetonide injection for diabetic macular edema: A systematic review and meta-analysis. Curr. Eye Res. 2012, 37, 1136–1147. [Google Scholar] [CrossRef]
- Shimura, M.; Yasuda, K.; Minezaki, T.; Noma, H. Reduction in the frequency of intravitreal bevacizumab administrations achieved by posterior subtenon injection of triamcinolone acetonide in patients with diffuse diabetic macular edema. JPN J. Ophthalmol. 2016, 60, 401–407. [Google Scholar] [CrossRef]
- Rishi, P.; Rishi, E.; Attiku, Y.; Dhami, A.; Iyer, V. Real-world experience with pro re nata dosing of intravitreal dexamethasone implant for eyes with refractory diabetic macular edema. GMS Ophthalmol. Cases 2020, 10, Doc21. [Google Scholar] [CrossRef] [PubMed]
- Bansal, P.; Gupta, V.; Gupta, A.; Dogra, M.R.; Ram, J. Efficacy of Ozurdex implant in recalcitrant diabetic macular edema—A single-center experience. Int. Ophthalmol. 2016, 36, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Totan, Y.; Guler, E.; Guragac, F.B. Dexamethasone Intravitreal Implant for Chronic Diabetic Macular Edema Resistant to Intravitreal Bevacizumab Treatment. Curr. Eye Res. 2016, 41, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.R.; Xi, M.; Abbey, A.M.; Yonekawa, Y.; Faia, L.J.; Hassan, T.S.; Ruby, A.J.; Wolfe, J.D. Short-term Efficacy of Intravitreal Dexamethasone Implant in Vitrectomized Eyes with Recalcitrant Diabetic Macular Edema and Prior Anti-VEGF Therapy. J. Ophthalmic. Vis. Res. 2016, 11, 183–187. [Google Scholar] [CrossRef]
- Maturi, R.K.; Glassman, A.R.; Liu, D.; Beck, R.W.; Bhavsar, A.R.; Bressler, N.M.; Jampol, L.M.; Melia, M.; Punjabi, O.S.; Salehi-Had, H.; et al. Effect of Adding Dexamethasone to Continued Ranibizumab Treatment in Patients With Persistent Diabetic Macular Edema: A DRCR Network Phase 2 Randomized Clinical Trial. JAMA Ophthalmol. 2018, 136, 29–38. [Google Scholar] [CrossRef]
- Coney, J.M. Fluocinolone acetonide 0.19 mg intravitreal implant improves foveal thickness and reduces treatment burden for up to 1 year in eyes with persistent diabetic macular edema. Int. Med. Case Rep. J. 2019, 12, 161–169. [Google Scholar] [CrossRef]
- Chronopoulos, A.; Chronopoulos, P.; Ashurov, A.; Korb, C.; Pfeiffer, N.; Hattenbach, L.O. Switching to intravitreal fluocinolone acetonide implant for refractory diabetic macular edema: 12- and 24-month results. Eur. J. Ophthalmol. 2021, 1120672121992982. [Google Scholar] [CrossRef]
- McCluskey, J.D.; Kaufman, P.L.; Wynne, K.; Lewis, G. Early adoption of the fluocinolone acetonide (FAc) intravitreal implant in patients with persistent or recurrent diabetic macular edema (DME). Int. Med. Case Rep. J. 2019, 12, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Pessoa, B.; Coelho, J.; Correia, N.; Ferreira, N.; Beirao, M.; Meireles, A. Fluocinolone Acetonide Intravitreal Implant 190 mug (ILUVIEN(R)) in Vitrectomized versus Nonvitrectomized Eyes for the Treatment of Chronic Diabetic Macular Edema. Ophthalmic Res. 2018, 59, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Massin, P.; Erginay, A.; Dupas, B.; Couturier, A.; Tadayoni, R. Efficacy and safety of sustained-delivery fluocinolone acetonide intravitreal implant in patients with chronic diabetic macular edema insufficiently responsive to available therapies: A real-life study. Clin. Ophthalmol. 2016, 10, 1257–1264. [Google Scholar] [CrossRef]
- Grover, D.; Li, T.J.; Chong, C.C. Intravitreal steroids for macular edema in diabetes. Cochrane Database Syst. Rev. 2008, CD005656. [Google Scholar] [CrossRef]
- Kocabora, M.S.; Yilmazli, C.; Taskapili, M.; Gulkilik, G.; Durmaz, S. Development of ocular hypertension and persistent glaucoma after intravitreal injection of triamcinolone. Clin. Ophthalmol. 2008, 2, 167–171. [Google Scholar] [CrossRef]
- Cekic, O.; Chang, S.; Tseng, J.J.; Akar, Y.; Barile, G.R.; Schiff, W.M. Cataract progression after intravitreal triamcinolone injection. Am. J. Ophthalmol. 2005, 139, 993–998. [Google Scholar] [CrossRef]
- Jonisch, J.; Lai, J.C.; Deramo, V.A.; Flug, A.J.; Fastenberg, D.M. Increased incidence of sterile endophthalmitis following intravitreal preserved triamcinolone acetonide. Br. J. Ophthalmol. 2008, 92, 1051–1054. [Google Scholar] [CrossRef]
- Mason, R.H.; Ballios, B.G.; Yan, P. Noninfectious endophthalmitis following intravitreal triamcinolone acetonide: Clinical case and literature review. Can. J. Ophthalmol. 2020, 55, 471–479. [Google Scholar] [CrossRef]
- Eckardt, C. Transconjunctival sutureless 23-gauge vitrectomy. Retina 2005, 25, 208–211. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Kurihara, T.; Uchida, A.; Nagai, N.; Shinoda, H.; Tsubota, K.; Ozawa, Y. Wide-Angle Viewing System versus Conventional Indirect Ophthalmoscopy for Scleral Buckling. Sci. Rep. 2015, 5, 13256. [Google Scholar] [CrossRef]
- Fujii, G.Y.; De Juan, E., Jr.; Humayun, M.S.; Pieramici, D.J.; Chang, T.S.; Awh, C.; Ng, E.; Barnes, A.; Wu, S.L.; Sommerville, D.N. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology 2002, 109, 1807–1812. [Google Scholar] [CrossRef]
- Inoue, M. Wide-angle viewing system. Dev. Ophthalmol. 2014, 54, 87–91. [Google Scholar] [CrossRef]
- Oellers, P.; Mahmoud, T.H. Surgery for Proliferative Diabetic Retinopathy: New Tips and Tricks. J. Ophthalmic Vis. Res. 2016, 11, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.H.; Liu, H.Y.; Hernandez-Da Mota, S.E.; Romano, M.R.; Falavarjani, K.G.; Ahmadieh, H.; Xu, X.; Liu, K. Vitrectomy with or without preoperative intravitreal bevacizumab for proliferative diabetic retinopathy: A meta-analysis of randomized controlled trials. Am. J. Ophthalmol. 2013, 156, 106–115.e102. [Google Scholar] [CrossRef]
- Zhao, X.Y.; Xia, S.; Chen, Y.X. Antivascular endothelial growth factor agents pretreatment before vitrectomy for complicated proliferative diabetic retinopathy: A meta-analysis of randomised controlled trials. Br. J. Ophthalmol. 2018, 102, 1077–1085. [Google Scholar] [CrossRef] [PubMed]
- Berrocal, M.H.; Acaba, L.A.; Acaba, A. Surgery for Diabetic Eye Complications. Curr. Diab. Rep. 2016, 16, 99. [Google Scholar] [CrossRef] [PubMed]
- Khuthaila, M.K.; Hsu, J.; Chiang, A.; DeCroos, F.C.; Milder, E.A.; Setlur, V.; Garg, S.J.; Spirn, M.J. Postoperative vitreous hemorrhage after diabetic 23-gauge pars plana vitrectomy. Am. J. Ophthalmol. 2013, 155, 757–763.e2. [Google Scholar] [CrossRef]
- Park, D.H.; Shin, J.P.; Kim, S.Y. Comparison of clinical outcomes between 23-gauge and 20-gauge vitrectomy in patients with proliferative diabetic retinopathy. Retina 2010, 30, 1662–1670. [Google Scholar] [CrossRef] [PubMed]
- Tachi, N.; Ogino, N. Vitrectomy for diffuse macular edema in cases of diabetic retinopathy. Am. J. Ophthalmol. 1996, 122, 258–260. [Google Scholar] [CrossRef]
- Yamamoto, T.; Hitani, K.; Tsukahara, I.; Yamamoto, S.; Kawasaki, R.; Yamashita, H.; Takeuchi, S. Early postoperative retinal thickness changes and complications after vitrectomy for diabetic macular edema. Am. J. Ophthalmol. 2003, 135, 14–19. [Google Scholar] [CrossRef]
- Lewis, H.; Abrams, G.W.; Blumenkranz, M.S.; Campo, R.V. Vitrectomy for diabetic macular traction and edema associated with posterior hyaloidal traction. Ophthalmology 1992, 99, 753–759. [Google Scholar] [CrossRef]
- Park, D.W.; Dugel, P.U.; Garda, J.; Sipperley, J.O.; Thach, A.; Sneed, S.R.; Blaisdell, J. Macular pucker removal with and without internal limiting membrane peeling: Pilot study. Ophthalmology 2003, 110, 62–64. [Google Scholar] [CrossRef]
- Kumagai, K.; Furukawa, M.; Ogino, N.; Larson, E.; Iwaki, M.; Tachi, N. Long-term follow-up of vitrectomy for diffuse nontractional diabetic macular edema. Retina 2009, 29, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Doi, N.; Sakamoto, T.; Sonoda, Y.; Yasuda, M.; Yonemoto, K.; Arimura, N.; Uchino, E.; Ishibashi, T. Comparative study of vitrectomy versus intravitreous triamcinolone for diabetic macular edema on randomized paired-eyes. Graefes Arch. Clin. Exp. Ophthalmol. 2012, 250, 71–78. [Google Scholar] [CrossRef]
- Kumagai, K.; Hangai, M.; Ogino, N.; Larson, E. Effect of Internal Limiting Membrane Peeling on Long-Term Visual Outcomes for Diabetic Macular Edema. Retina 2015, 35, 1422–1428. [Google Scholar] [CrossRef]
- Simunovic, M.P.; Hunyor, A.P.; Ho, I.V. Vitrectomy for diabetic macular edema: A systematic review and meta-analysis. Can. J. Ophthalmol. 2014, 49, 188–195. [Google Scholar] [CrossRef]
- Imai, H.; Tetsumoto, A.; Yamada, H.; Hayashida, M.; Otsuka, K.; Miki, A.; Kusuhara, S.; Nakamura, M. Long-Term Effect of Cystotomy with or without the Fibrinogen Clot Removal for Refractory Cystoid Macular Edema Secondary to Diabetic Retinopathy. Retina 2021, 41, 844–851. [Google Scholar] [CrossRef]
- Oosterveer, M.H.; Grefhorst, A.; van Dijk, T.H.; Havinga, R.; Staels, B.; Kuipers, F.; Groen, A.K.; Reijngoud, D.-J. Fenofibrate simultaneously induces hepatic fatty acid oxidation, synthesis, and elongation in mice. J. Biol. Chem. 2009, 284, 34036–34044. [Google Scholar] [CrossRef]
- Arai, T.; Kim, H.-J.; Chiba, H.; Matsumoto, A. Interaction of Fenofibrate and Fish Oil in Relation to Lipid Metabolism in Mice. J. Atheroscler. Thromb. 2009, 16, 283–291. [Google Scholar] [CrossRef]
- Sasaki, J.; Yamamoto, K.; Ageta, M. Effects of fenofibrate on high-density lipoprotein particle size in patients with hyperlipidemia: A randomized, double-blind, placebo-controlled, multicenter, crossover study. Clin. Ther. 2002, 24, 1614–1626. [Google Scholar] [CrossRef]
- Mellies, M.J.; Stein, E.A.; Khoury, P.; Lamkin, G.; Glueck, C.J. Effects of fenofibrate on lipids, lipoproteins, and apolipoproteins in 33 subjects with primary hypercholesterolemia. Atherosclerosis 1987, 63, 57–64. [Google Scholar] [CrossRef]
- Sharma, R.; Mahajan, M.; Singh, B.; Bal, B.S.; Kant, R. Apolipoprotein modifying effects of statins and fibrate in various age groups of coronary artery disease patients. J. Indian Med. Assoc. 2006, 104, 492–494, 496, 498. [Google Scholar]
- Guay, D.R. Micronized fenofibrate: A new fibric acid hypolipidemic agent. Ann. Pharmacother. 1999, 33, 1083–1103. [Google Scholar] [CrossRef] [PubMed]
- Keech, A.; Simes, R.J.; Barter, P.; Best, J.; Scott, R.; Taskinen, M.R.; Forder, P.; Pillai, A.; Davis, T.; Glasziou, P.; et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): Randomised controlled trial. Lancet 2005, 366, 1849–1861. [Google Scholar] [CrossRef]
- ACCORD Study Group; ACCORD Eye Study Group; Chew, E.Y.; Ambrosius, W.T.; Davis, M.D.; Danis, R.P.; Gangaputra, S.; Greven, C.M.; Hubbard, L.; Esser, B.A.; et al. Effects of medical therapies on retinopathy progression in type 2 diabetes. N. Engl. J. Med. 2010, 363, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Bogdanov, P.; Hernández, C.; Corraliza, L.; Carvalho, A.R.; Simó, R. Effect of fenofibrate on retinal neurodegeneration in an experimental model of type 2 diabetes. Acta Diabetol. 2015, 52, 113–122. [Google Scholar] [CrossRef]
- Wang, N.; Zou, C.; Zhao, S.; Wang, Y.; Han, C.; Zheng, Z. Fenofibrate Exerts Protective Effects in Diabetic Retinopathy via Inhibition of the ANGPTL3 Pathway. Investig. Ophthalmol. Vis. Sci. 2018, 59, 4210–4217. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Zhang, F.; Zhang, X.; Cheng, R.; Ma, J.-X.; Yi, J.; Li, J. Fenofibrate ameliorates diabetic retinopathy by modulating Nrf2 signaling and NLRP3 inflammasome activation. Mol. Cell. Biochem. 2018, 445, 105–115. [Google Scholar] [CrossRef]
- Kostapanos, M.S.; Florentin, M.; Elisaf, M.S. Fenofibrate and the kidney: An overview. Eur. J. Clin. Investig. 2013, 43, 522–531. [Google Scholar] [CrossRef]
- Jun, M.; Zhu, B.; Tonelli, M.; Jardine, M.J.; Patel, A.; Neal, B.; Liyanage, T.; Keech, A.; Cass, A.; Perkovic, V. Effects of Fibrates in Kidney Disease: A Systematic Review and Meta-Analysis. J. Am. Coll. Cardiol. 2012, 60, 2061–2071. [Google Scholar] [CrossRef]
- Kim, S.; Ko, K.; Park, S.; Lee, D.R.; Lee, J. Effect of Fenofibrate Medication on Renal Function. Korean J. Fam. Med. 2017, 38, 192–198. [Google Scholar] [CrossRef]
- Ida, S.; Kaneko, R.; Murata, K. Efficacy and safety of pemafibrate administration in patients with dyslipidemia: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2019, 18, 38. [Google Scholar] [CrossRef] [PubMed]
- Fruchart, J.-C. Pemafibrate (K-877), a novel selective peroxisome proliferator-activated receptor alpha modulator for management of atherogenic dyslipidaemia. Cardiovasc. Diabetol. 2017, 16, 124. [Google Scholar] [CrossRef] [PubMed]
- Suto, K.; Fukuda, D.; Shinohara, M.; Ganbaatar, B.; Yagi, S.; Kusunose, K.; Yamada, H.; Soeki, T.; Hirata, K.-I.; Sata, M. Pemafibrate, A Novel Selective Peroxisome Proliferator-Activated Receptor α Modulator, Reduces Plasma Eicosanoid Levels and Ameliorates Endothelial Dysfunction in Diabetic Mice. J. Atheroscler. Thromb. 2021, 61101. [Google Scholar] [CrossRef]
- Horikawa, T.; Kawanami, T.; Hamaguchi, Y.; Tanaka, Y.; Kita, S.; Ryorin, R.; Takashi, Y.; Takahashi, H.; Tanabe, M.; Yanase, T.; et al. Pemafibrate, a PPAR alpha agonist, attenuates neointima formation after vascular injury in mice fed normal chow and a high-fat diet. Heliyon 2020, 6, e05431. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Lee, D.; Miwa, Y.; Jiang, X.; Ohta, M.; Tsubota, K.; Kurihara, T. Pemafibrate Protects Against Retinal Dysfunction in a Murine Model of Diabetic Retinopathy. Int. J. Mol. Sci. 2020, 21, 6243. [Google Scholar] [CrossRef] [PubMed]
- Shiono, A.; Sasaki, H.; Sekine, R.; Abe, Y.; Matsumura, Y.; Inagaki, T.; Tanaka, T.; Kodama, T.; Aburatani, H.; Sakai, J.; et al. PPARα activation directly upregulates thrombomodulin in the diabetic retina. Sci. Rep. 2020, 10, 10837. [Google Scholar] [CrossRef] [PubMed]
- Fujita, N.; Sase, K.; Tsukahara, C.; Arizono, I.; Takagi, H.; Kitaoka, Y. Pemafibrate prevents retinal neuronal cell death in NMDA-induced excitotoxicity via inhibition of p-c-Jun expression. Mol. Biol. Rep. 2021, 48, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Ozawa, N.; Miwa, Y.; Ishida, A.; Ohta, M.; Tsubota, K.; Kurihara, T. Pemafibrate Prevents Retinal Pathological Neovascularization by Increasing FGF21 Level in a Murine Oxygen-Induced Retinopathy Model. Int. J. Mol. Sci. 2019, 20, 5878. [Google Scholar] [CrossRef]
- Klein, R.; Klein, B.E.; Moss, S.E.; Davis, M.D.; DeMets, D.L. The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch. Ophthalmol. 1984, 102, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, N.V. Diabetic retinopathy I. The course of retinopathy in insulin-treated diabetics. A one year epidemiological cohort study of diabetes mellitus. The Island of Falster, Denmark. Acta Ophthalmol. 1984, 62, 256–265. [Google Scholar] [CrossRef]
- Kawasaki, R.; Tanaka, S.; Tanaka, S.; Yamamoto, T.; Sone, H.; Ohashi, Y.; Akanuma, Y.; Yamada, N.; Yamashita, H.; Japan Diabetes Complications Study Group. Incidence and progression of diabetic retinopathy in Japanese adults with type 2 diabetes: 8 year follow-up study of the Japan Diabetes Complications Study (JDCS). Diabetologia 2011, 54, 2288–2294. [Google Scholar] [CrossRef]
- Diep, T.M.; Tsui, I. Risk factors associated with diabetic macular edema. Diabetes Res. Clin. Pract. 2013, 100, 298–305. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomita, Y.; Lee, D.; Tsubota, K.; Negishi, K.; Kurihara, T. Updates on the Current Treatments for Diabetic Retinopathy and Possibility of Future Oral Therapy. J. Clin. Med. 2021, 10, 4666. https://doi.org/10.3390/jcm10204666
Tomita Y, Lee D, Tsubota K, Negishi K, Kurihara T. Updates on the Current Treatments for Diabetic Retinopathy and Possibility of Future Oral Therapy. Journal of Clinical Medicine. 2021; 10(20):4666. https://doi.org/10.3390/jcm10204666
Chicago/Turabian StyleTomita, Yohei, Deokho Lee, Kazuo Tsubota, Kazuno Negishi, and Toshihide Kurihara. 2021. "Updates on the Current Treatments for Diabetic Retinopathy and Possibility of Future Oral Therapy" Journal of Clinical Medicine 10, no. 20: 4666. https://doi.org/10.3390/jcm10204666
APA StyleTomita, Y., Lee, D., Tsubota, K., Negishi, K., & Kurihara, T. (2021). Updates on the Current Treatments for Diabetic Retinopathy and Possibility of Future Oral Therapy. Journal of Clinical Medicine, 10(20), 4666. https://doi.org/10.3390/jcm10204666









