Perinatal Adverse Effects in Newborns with Estimated Loss of Weight Percentile between the Third Trimester Ultrasound and Delivery. The GROWIN Study
Abstract
:1. Introduction
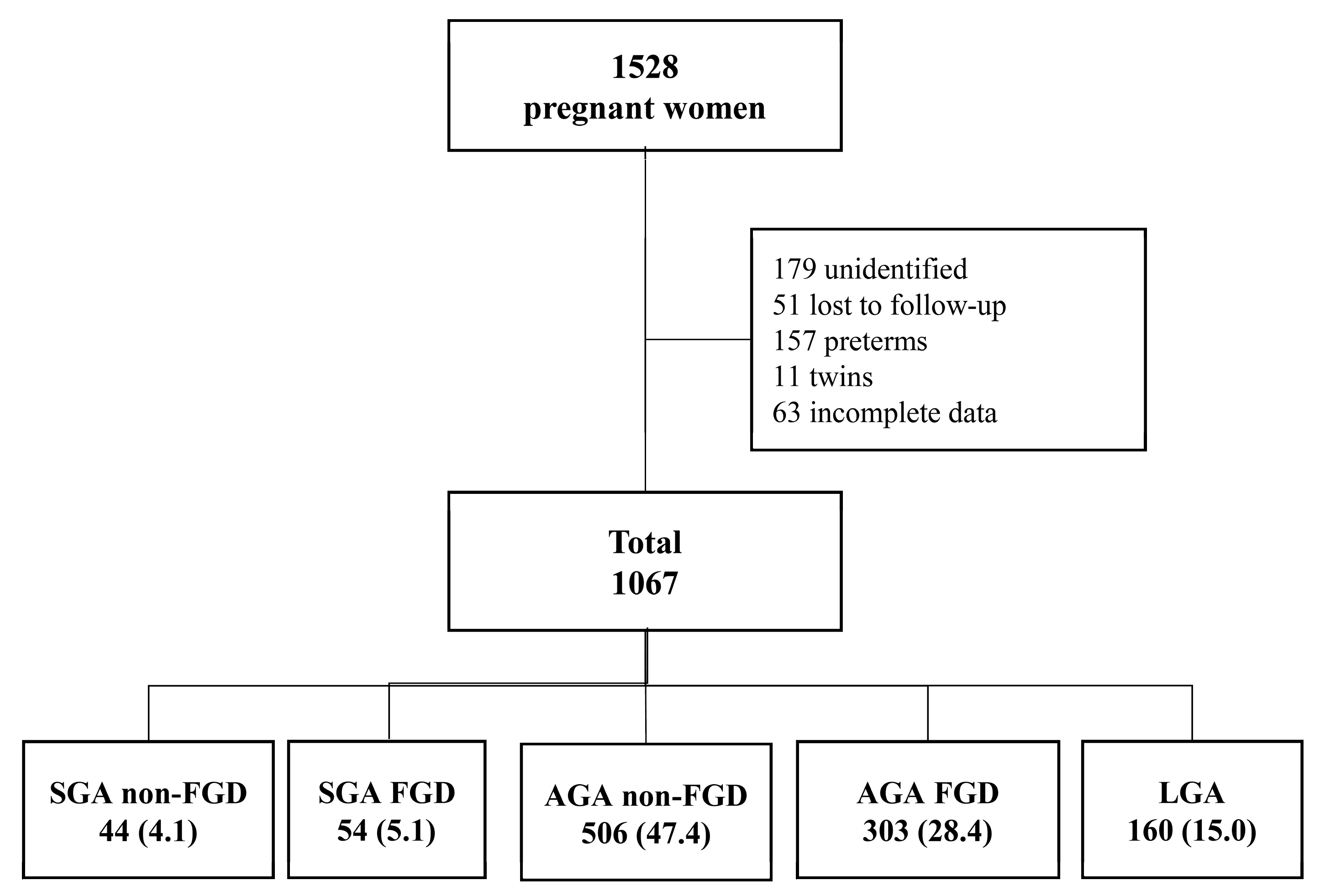
2. Materials and Methods
2.1. Study Design
2.2. Study Groups
2.3. Statistical Analyses
3. Results
3.1. Descriptive Results
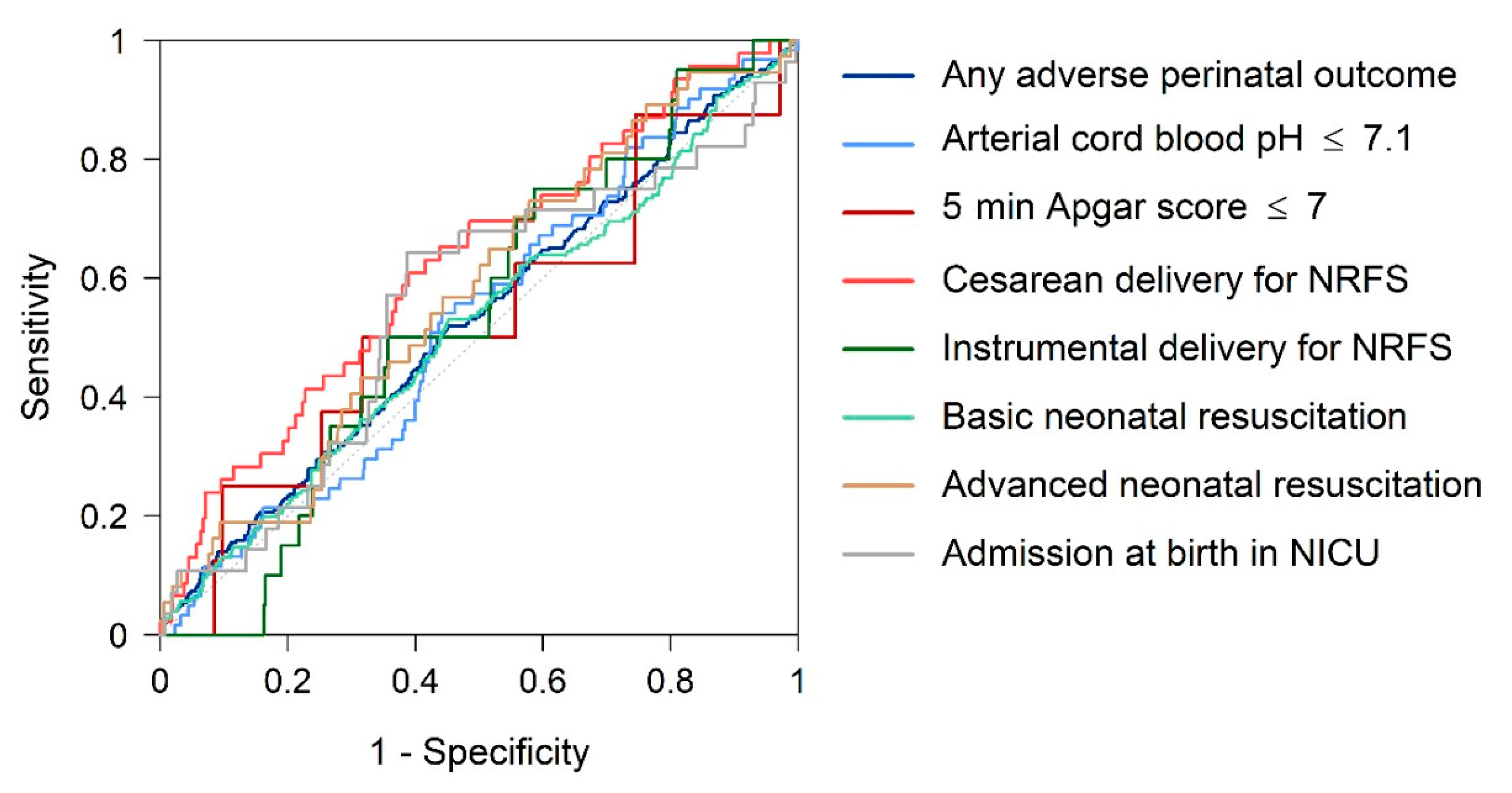
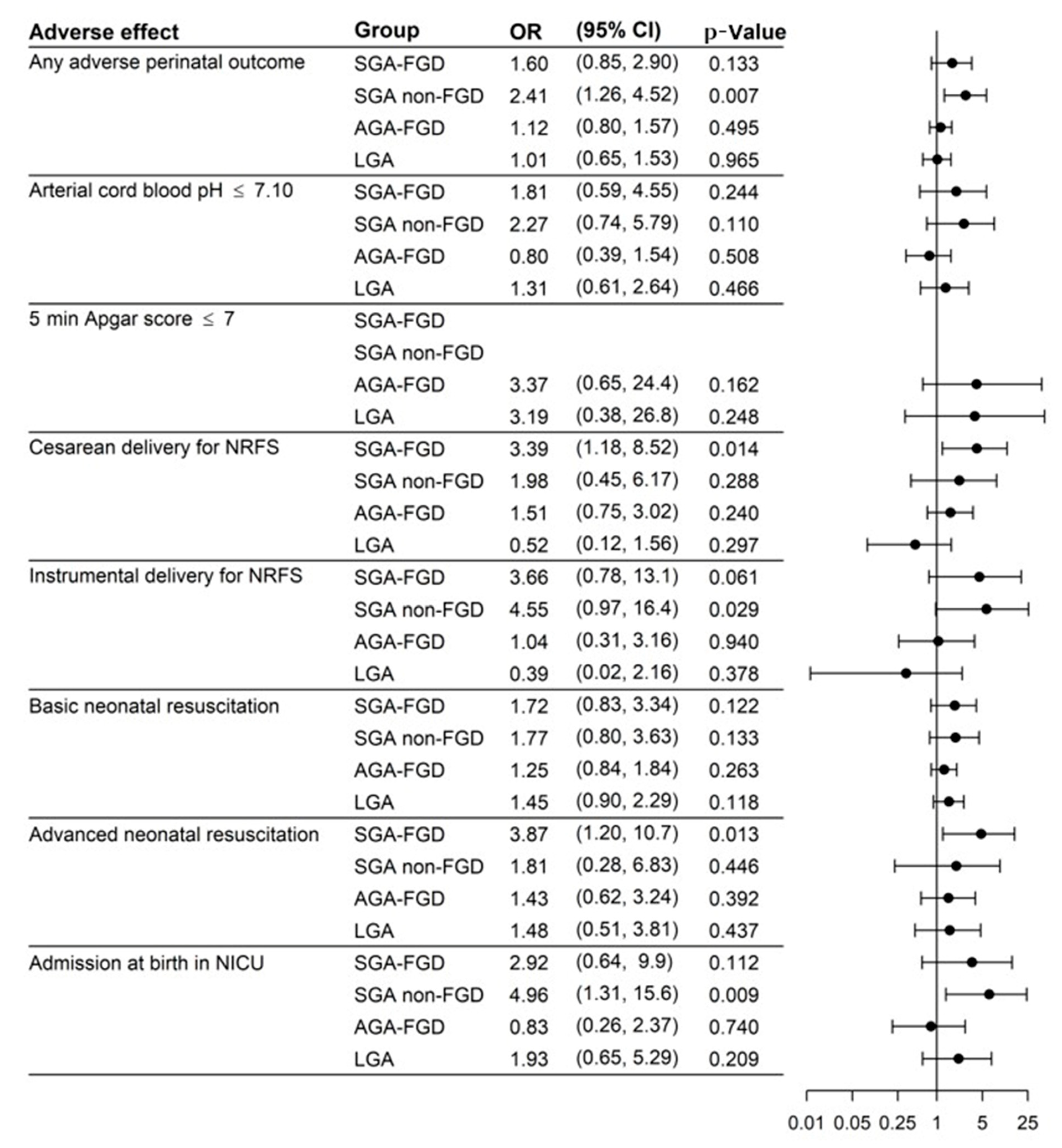
3.2. Adverse Perinatal Outcomes
4. Discussion
4.1. Principal Findings
4.2. Birthweight Percentile and APOs
4.3. Fetal Growth Percentile Deceleration and APOs
4.4. Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Salomon, L.J.; Alfirevic, Z.; Da Silva Costa, F.; Deter, R.L.; Figueras, F.; Ghi, T.; Glanc, P.; Khalil, A.; Lee, W.; Napolitano, R.; et al. ISUOG Practice Guidelines: Ultrasound assessment of fetal biometry and growth. Ultrasound Obstet. Gynecol. 2019, 53, 715–723. [Google Scholar] [CrossRef]
- Gordijn, S.J.; Beune, I.M.; Thilaganathan, B.; Papageorghiou, A.; Baschat, A.A.; Baker, P.N.; Silver, R.M.; Wynia, K.; Ganzevoort, W. Consensus definition of fetal growth restriction: A Delphi procedure. Ultrasound Obstet. Gynecol. 2016, 48, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Audette, M.C.; Kingdom, J.C. Screening for fetal growth restriction and placental insufficiency. Semin. Fetal Neonatal Med. 2018, 23, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Flenady, V.; Koopmans, L.; Middleton, P.; Frøen, J.F.; Smith, G.C.; Gibbons, K.; Coory, M.; Gordon, A.; Ellwood, D.; McIntyre, H.D.; et al. Major risk factors for stillbirth in high-income countries: A systematic review and meta-analysis. Lancet 2011, 377, 1331–1340. [Google Scholar] [CrossRef]
- Beune, I.M.; Bloomfield, F.H.; Ganzevoort, W.; Embleton, N.D.; Rozance, P.J.; van Wassenaer-Leemhuis, A.G.; Wynia, K.; Gordijn, S.J. Consensus Based Definition of Growth Restriction in the Newborn. J. Pediatr. 2018, 196, 71–76. [Google Scholar] [CrossRef]
- McCowan, L.M.; Figueras, F.; Anderson, N.H. Evidence-based national guidelines for the management of suspected fetal growth restriction: Comparison, consensus, and controversy. Am. J. Obstet. Gynecol. 2018, 218, S855–S868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, A.C.C.; Kozuki, N.; Cousens, S.; Stevens, G.A.; Blencowe, H.; Silveira, M.F.; Sania, A.; Rosen, H.E.; Schmiegelow, C.; Adair, L.S.; et al. Estimates of burden and consequences of infants born small for gestational age in low and middle income countries with INTERGROWTH-21st standard: Analysis of CHERG datasets. BMJ 2017, 358, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kesavan, K.; Devaskar, S.U. Intrauterine Growth Restriction: Postnatal Monitoring and Outcomes. Pediatr. Clin. North Am. 2019, 66, 403–423. [Google Scholar] [CrossRef]
- Lees, C.; Marlow, N.; Arabin, B.; Bilardo, C.M.; Brezinka, C.; Derks, J.B.; Duvekot, J.; Frusca, T.; Diemert, A.; Ferrazzi, E.; et al. Perinatal morbidity and mortality in early-onset fetal growth restriction: Cohort outcomes of the trial of randomized umbilical and fetal flow in Europe (TRUFFLE). Ultrasound Obstet. Gynecol. 2013, 42, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Cruz, M.; Cruz-Lemini, M.; Fernández, M.T.; Parra, J.A.; Bartrons, J.; Gõmez-Roig, M.D.; Crispi, F.; Gratacõs, E. Fetal cardiac function in late-onset intrauterine growth restriction vs. small-for-gestational age, as defined by estimated fetal weight, cerebroplacental ratio and uterine artery Doppler. Ultrasound Obstet. Gynecol. 2015, 46, 465–471. [Google Scholar] [CrossRef] [Green Version]
- Kady, S.M.; Gardosi, J. Perinatal mortality and fetal growth restriction. Best Pract. Res. Clin. Obstet. Gynaecol. 2004, 18, 397–410. [Google Scholar] [CrossRef] [PubMed]
- Gardosi, J.; Madurasinghe, V.; Williams, M.; Malik, A.; Francis, A. Maternal and fetal risk factors for stillbirth: Population based study. BMJ 2013, 346, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claris, O.; Beltrand, J.; Levy-Marchal, C. Consequences of intrauterine growth and early neonatal catch-up growth. Semin. Perinatol. 2010, 34, 207–210. [Google Scholar] [CrossRef] [PubMed]
- Barker, D.J.; Osmond, C.; Golding, J.; Kuh, D.; Wadsworth, M.E. Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ 1989, 298, 564–567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Boo, H.A.; Harding, J.E. The Developmental origins of adult disease (Barker) hypothesis. Aust. N. Zeal. J. Obstet. Gynaecol. 2006, 46, 4–14. [Google Scholar] [CrossRef]
- Jarvis, S.; Glinianaia, S.V.; Torrioli, M.G.; Platt, M.J.; Miceli, M.; Jouk, P.S.; Johnson, A.; Hutton, J.; Hemming, K.; Hagberg, G.; et al. Cerebral palsy and intrauterine growth in single births: European collaborative study. Lancet 2003, 362, 1106–1111. [Google Scholar] [CrossRef]
- Lindqvist, P.G.; Molin, J. Does antenatal identification of small-for-gestational age fetuses significantly improve their outcome? Ultrasound Obstet. Gynecol. 2005, 25, 258–264. [Google Scholar] [CrossRef]
- Melamed, N.; Baschat, A.; Yinon, Y.; Athanasiadis, A.; Mecacci, F.; Figueras, F.; Berghella, V.; Nazareth, A.; Tahlak, M.; McIntyre, H.D.; et al. FIGO (International Federation of Gynecology and Obstetrics) initiative on fetal growth: Best practice advice for screening, diagnosis, and management of fetal growth restriction. Int. J. Gynecol. Obstet. 2021, 152, 3–57. [Google Scholar] [CrossRef]
- Gardosi, J.; Clausson, B.; Francis, A. The value of customised centiles in assessing perinatal mortality risk associated with parity and maternal size. BJOG Int. J. Obstet. Gynaecol. 2009, 116, 1356–1363. [Google Scholar] [CrossRef]
- McCowan, L. Customised birthweight centiles predict SGA pregnancies with perinatal morbidity. BJOG Int. J. Obstet. Gynaecol. 2005, 112, 1026–1033. [Google Scholar] [CrossRef]
- Resnik, R. Intrauterine growth restriction. Obstet. Gynecol. 2002, 99, 490–496. [Google Scholar] [PubMed]
- Savirón-Cornudella, R.; Esteban, L.M.; Lerma, D.; Cotaina, L.; Borque, Á.; Sanz, G.; Castán, S. Comparison of fetal weight distribution improved by paternal height by Spanish standard versus Intergrowth 21st standard. J. Perinat. Med. 2018, 46, 750–759. [Google Scholar] [CrossRef] [Green Version]
- Unterscheider, J.; Daly, S.; Geary, M.P.; Kennelly, M.M.; McAuliffe, F.M.; O’Donoghue, K.; Hunter, A.; Morrison, J.J.; Burke, G.; Dicker, P.; et al. Optimizing the definition of intrauterine growth restriction: The multicenter prospective PORTO Study. Am. J. Obstet. Gynecol. 2013, 208, 290.e1–290.e6. [Google Scholar] [CrossRef] [PubMed]
- Vasaks, B.; Koenen, V.; Koster, M.P.H.; Hukkelhoven, C.W.P.M.; Franx, A.; Hanson, M.A.; Visser, G.H.A. Human fetal growth is constrained below optimal for perinatal survival. Ultrasound Obstet. Gynecol. 2015, 45, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Akolekar, R.; Syngelaki, A.; Gallo, D.M.; Poon, L.C.; Nicolaides, K.H. Umbilical and fetal middle cerebral artery Doppler at 35–37 weeks’ gestation in the prediction of adverse perinatal outcome. Ultrasound Obstet. Gynecol. 2015, 46, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Stratton, J.F.; Ni Scanaill, S.; Stuart, B.; Turner, M.J. Are babies of normal birth weight who fail to reach their growth potential as diagnosed by ultrasound at increased risk? Ultrasound Obstet. Gynecol. 1995, 5, 114–118. [Google Scholar] [CrossRef]
- Bardien, N.; Whitehead, C.L.; Tong, S.; Ugoni, A.; McDonald, S.; Walker, S.P. Placental insufficiency in fetuses that slow in growth but are born appropriate for gestational age: A prospective longitudinal study. PLoS ONE 2016, 11, e0142788. [Google Scholar] [CrossRef] [Green Version]
- MacDonald, T.M.; Hui, L.; Tong, S.; Robinson, A.J.; Dane, K.M.; Middleton, A.L.; Walker, S.P. Reduced growth velocity across the third trimester is associated with placental insufficiency in fetuses born at a normal birthweight: A prospective cohort study. BMC Med. 2017, 15, 164. [Google Scholar] [CrossRef]
- Verkauskiene, R.; Beltrand, J.; Claris, O.; Chevenne, D.; Deghmoun, S.; Dorgeret, S.; Alison, M.; Gaucherand, P.; Sibony, O.; Lévy-Marchal, C. Impact of fetal growth restriction on body composition and hormonal status at birth in infants of small and appropriate weight for gestational age. Eur. J. Endocrinol. 2007, 157, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the reporting of observational studies in epidemiology (StroBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [Green Version]
- American College of Obstetricians and Gynecologists. Methods for Estimating the Due Date. Comitee Opinion No. 700. Obstet. Gynecol. 2017, 129, e150–e154. [Google Scholar] [CrossRef]
- Hadlock, F.P.; Harrist, R.B.; Sharman, R.S.; Deter, R.L.; Park, S.K. Estimation of fetal weight with the use of head, body, and femur measurements—A prospective study. Am. J. Obstet. Gynecol. 1985, 151, 333–337. [Google Scholar] [CrossRef]
- Carrascosa, A.; Fernández, J.M.; Ferrández, Á.; López-Siguero, J.P.; López, D.; Sánchez, E.; Colaborador, G. Estudios Españoles de Crecimiento 2010. Revista Española Endocrinología Pediátrica 2011, 2 (Suppl. 1), 59–62. [Google Scholar]
- Madden, J.V.; Flatley, C.J.; Kumar, S. Term small-for-gestational-age infants from low-risk women are at significantly greater risk of adverse neonatal outcomes. Am. J. Obstet. Gynecol. 2018, 218, 525.e1–525.e9. [Google Scholar] [CrossRef] [Green Version]
- Caradeux, J.; Eixarch, E.; Mazarico, E.; Basuki, T.R.; Gratacos, E.; Figueras, F. Longitudinal growth assessment for prediction of adverse perinatal outcome in fetuses suspected to be small-for-gestational age. Ultrasound Obstet. Gynecol. 2018, 52, 325–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Illa, M.; Coloma, J.L.; Eixarch, E.; Meler, E.; Iraola, A.; Gardosi, J.; Gratacós, E.; Figueras, F. Growth deficit in term small-for-gestational fetuses with normal umbilical artery Doppler is associated with adverse outcome. J. Perinat. Med. 2009, 37, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Iraola, A.; González, I.; Eixarch, E.; Meler, E.; Illa, M.; Gardosi, J.; Gratacós, E.; Figueras, F. Prediction of adverse perinatal outcome at term in small-for-gestational age fetuses: Comparison of growth velocity vs. customized assessment. J. Perinat. Med. 2008, 36, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G.; Hytten, F.E. Intrauterine growth retardation: Let’s be clear about it. BJOG Int. J. Obstet. Gynaecol. 1989, 96, 1127–1128. [Google Scholar] [CrossRef]
- Fay, R.A.; Dey, P.L.; Saadie, C.M.J.; Buhl, J.A.; Gebski, V.J. Ponderal Index: A Better Definition of the ‘At Risk’ Group with Intrauterine Growth Problems than Birth-weight for Gestational Age in Term Infants. Aust. N. Zeal. J. Obstet. Gynaecol. 1991, 31, 17–19. [Google Scholar] [CrossRef]
- Unterscheider, J.; Daly, S.; Geary, M.P.; Kennelly, M.M.; McAuliffe, F.M.; O’Donoghue, K.; Hunter, A.; Morrison, J.J.; Burke, G.; Dicker, P.; et al. Definition and management of fetal growth restriction: A survey of contemporary attitudes. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 174, 41–45. [Google Scholar] [CrossRef]
- Owen, P.; Khan, K.S. Fetal growth velocity in the prediction of intrauterine growth retardation in a low risk population. BJOG Int. J. Obstet. Gynaecol. 1998, 105, 536–540. [Google Scholar] [CrossRef] [Green Version]
- Ohuma, E.O.; Villar, J.; Feng, Y.; Xiao, L.; Salomon, L.; Barros, F.C.; Cheikh Ismail, L.; Stones, W.; Jaffer, Y.; Oberto, M.; et al. Fetal growth velocity standards from the Fetal Growth Longitudinal Study of the INTERGROWTH-21st Project. Am. J. Obstet. Gynecol. 2021, 224, 208.e1–208.e18. [Google Scholar] [CrossRef] [PubMed]
- Grantz, K.L.; Kim, S.; Grobman, W.A.; Newman, R.; Owen, J.; Skupski, D.; Grewal, J.; Chien, E.K.; Wing, D.A.; Wapner, R.J.; et al. Fetal growth velocity: The NICHD fetal growth studies. Am. J. Obstet. Gynecol. 2018, 219, 285.e1–285.e36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sovio, U.; White, I.R.; Dacey, A.; Pasupathy, D.; Smith, G.C.S. Screening for fetal growth restriction with universal third trimester ultrasonography in nulliparous women in the Pregnancy Outcome Prediction (POP) study: A prospective cohort study. Lancet 2015, 386, 2089–2097. [Google Scholar] [CrossRef] [Green Version]
- Bligh, L.N.; Flatley, C.J.; Kumar, S. Reduced growth velocity at term is associated with adverse neonatal outcomes in non-small for gestational age infants. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 240, 125–129. [Google Scholar] [CrossRef]
- Caradeux, J.; Eixarch, E.; Mazarico, E.; Basuki, T.R.; Gratacós, E.; Figueras, F. Second- to third-trimester longitudinal growth assessment for prediction of small-for-gestational age and late fetal growth restriction. Ultrasound Obstet. Gynecol. 2018, 51, 219–224. [Google Scholar] [CrossRef] [Green Version]
- Cavallaro, A.; Veglia, M.; Svirko, E.; Vannuccini, S.; Volpe, G.; Impey, L. Using fetal abdominal circumference growth velocity in the prediction of adverse outcome in near-term small-for-gestational-age fetuses. Ultrasound Obstet. Gynecol. 2018, 52, 494–500. [Google Scholar] [CrossRef]
- Barker, E.D.; McAuliffe, F.M.; Alderdice, F.; Unterscheider, J.; Daly, S.; Geary, M.P.; Kennelly, M.M.; O’Donoghue, K.; Hunter, A.; Morrison, J.J.; et al. The role of growth trajectories in classifying fetal growth restriction. Obstet. Gynecol. 2013, 122, 248–254. [Google Scholar] [CrossRef] [Green Version]
- De Jong, C.L.D.; Francis, A.; Van Geijn, H.P.; Gardosi, J. Fetal growth rate and adverse perinatal events. Ultrasound Obstet. Gynecol. 1999, 13, 86–89. [Google Scholar] [CrossRef]
- Marconi, A.M.; Ronzoni, S.; Bozzetti, P.; Vailati, S.; Morabito, A.; Battaglia, F.C. Comparison of fetal and neonatal growth curves in detecting growth restriction. Obstet. Gynecol. 2008, 112, 1227–1234. [Google Scholar] [CrossRef] [Green Version]
- Hendrix, M.L.E.; Van Kuijk, S.M.J.; Gavilanes, A.W.D.; Kramer, D.; Spaanderman, M.E.A.; Al Nasiry, S. Reduced fetal growth velocities and the association with neonatal outcomes in appropriate-for-gestational-age neonates: A retrospective cohort study. BMC Pregnancy Childbirth 2019, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chatzakis, C.; Papaioannou, G.K.; Eleftheriades, M.; Makrydimas, G.; Dinas, K.; Sotiriadis, A. Perinatal outcome of appropriate-weight fetuses with decelerating growth. J. Matern. Fetal Neonatal Med. 2021, 34, 3362–3369. [Google Scholar] [CrossRef] [PubMed]
- Pacora, P.; Romero, R.; Jung, E.; Gudicha, D.W.; Hernandez-Andrade, E.; Musilova, I.; Kacerovsky, M.; Jaiman, S.; Erez, O.; Hsu, C.D.; et al. Reduced fetal growth velocity precedes antepartum fetal death. Ultrasound Obstet. Gynecol. 2021, 57, 942–952. [Google Scholar] [CrossRef] [PubMed]
- Savirón-Cornudella, R.; Esteban, L.M.; Aznar-Gimeno, R.; Dieste Pérez, P.; Pérez-López, F.R.; Castán-Larraz, B.; Sanz, G.; Tajada-Duaso, M. Prediction of Large for Gestational Age by Ultrasound at 35 Weeks and Impact of Ultrasound-Delivery Interval: Comparison of 6 Standards. Fetal Diagn. Ther. 2021, 48, 15–23. [Google Scholar] [CrossRef]
- Dudley, N.J. A systematic review of the ultrasound estimation of fetal weight. Ultrasound Obstet. Gynecol. 2005, 25, 80–89. [Google Scholar] [CrossRef] [PubMed]

| Variable | Total | SGA-FGD | SGA Non-FGD | AGA FGD | AGA Non-FGD | LGA | p-Value |
|---|---|---|---|---|---|---|---|
| Cases | 1067 | 54 (5.1) | 44 (4.1) | 303 (28.4) | 506 (47.4) | 160 (15.0) | |
| Maternal characteristics | |||||||
| Parity | <0.001 | ||||||
| Nulliparous | 626 (58.7) | 41 (75.9) | 29 (65.9) | 181 (59.7) | 307 (60.7) | 68 (42.5) | |
| Multiparous | 441 (41.3) | 13 (24.1) | 15 (34.1) | 122 (40.3) | 199 (39.3) | 92 (57.5) | |
| Maternal weight (kg) | 66.4 (15.0) | 62.6 (13.8) | 60.0 (13.7) | 65.4 (14.1) | 66.2 (15.0) | 68.0 (21.0) | <0.001 |
| Height (cm) | 163 (3.00) | 163 (5.50) | 163 (2.00) | 163 (3.00) | 163 (2.00) | 163 (4.25) | 0.528 |
| Body mass index | 25.0 (5.68) | 24.5 (5.08) | 22.2 (5.61) | 24.5 (5.05) | 25.2 (5.51) | 25.6 (6.75) | <0.001 |
| Age at delivery (years) | 32.5 (8.11) | 34.8 (8.20) | 32.2 (5.38) | 33.5 (8.80) | 32.2 (7.94) | 32.0 (6.10) | 0.075 |
| Pregnancy pathology | |||||||
| Gestational diabetes | 89 (8.3) | 2 (3.7) | 4 (9.1) | 16 (5.3) | 44 (8.7) | 23 (14.4) | 0.014 |
| Hypertensive disorders of pregnancy | 43 (4.0) | 4 (7.4) | 1 (2.3) | 15 (5.0) | 13 (2.6) | 10 (6.2) | 0.082 |
| Type of delivery | 0.346 | ||||||
| Normal vaginal delivery | 702 (65.8) | 28 (51.9) | 27 (61.4) | 199 (65.7) | 342 (67.6) | 106 (66.2) | |
| Instrumental delivery | 224 (21.0) | 13 (24.1) | 11 (25.0) | 63 (20.8) | 106 (20.9) | 31 (19.4) | |
| Cesarean section | 141 (13.2) | 13 (24.1) | 6 (13.6) | 41 (13.5) | 58 (11.5) | 23 (14.4) | |
| Ultrasound parameters at 35 weeks | |||||||
| Gestational age (days) | 246 (5.00) | 246 (3.00) | 247 (6.25) | 246 (4.00) | 246 (5.00) | 246 (5.25) | 0.525 |
| Estimated fetal weight (g) | 2571 (333) | 2421 (138) | 2200 (268) | 2625 (240) | 2513 (321) | 2776 (404) | <0.001 |
| Estimated fetal weight percentile | 65.0 (40.9) | 44.5 (27.7) | 15.5 (12.0) | 72.9 (24.5) | 58.3 (38.6) | 88.5 (20.2) | <0.001 |
| Delivery data | |||||||
| Gestational age at birth (days) | 278 (12.0) | 280 (13.0) | 273 (15.0) | 278 (11.0) | 278 (12.0) | 276 (12.0) | 0.008 |
| Birthweight (g) | 3285 (595) | 2712 (194) | 2518 (251) | 3105 (345) | 3362 (465) | 3935 (355) | <0.001 |
| Birthweight percentile | 53.2 (54.4) | 6.04 (3.57) | 4.55 (5.56) | 33.8 (27.1) | 60.4 (37.5) | 95.4 (5.84) | <0.001 |
| Arterial cord blood pH | 7.27 (0.11) | 7.26 (0.12) | 7.25 (0.10) | 7.27 (0.10) | 7.27 (0.11) | 7.26 (0.12) | 0.133 |
| 5 min Apgar score ≤ 7 | 10.0 (0.00) | 10.0 (0.00) | 10.0 (0.25) | 10.0 (0.00) | 10.0 (0.00) | 10.0 (0.00) | 0.069 |
| Newborn Sex | 0.001 | ||||||
| Male | 577 (54.1) | 26 (48.1) | 22 (50.0) | 141 (46.5) | 307 (60.7) | 81 (50.6) | |
| Female | 490 (45.9) | 28 (51.9) | 22 (50.0) | 162 (53.5) | 199 (39.3) | 79 (49.4) | |
| Newborn length (cm) | 49.0 (2.00) | 47.0 (2.00) | 47.0 (1.62) | 49.0 (2.50) | 49.0 (2.00) | 50.5 (2.12) | <0.001 |
| Newborn head circumference (cm) | 34.0 (1.50) | 33.5 (1.38) | 33.0 (1.78) | 34.0 (2.00) | 34.0 (1.38) | 35.0 (2.00) | <0.001 |
| Adverse Effects | Total | SGA FGD | SGA Non-FGD | AGA FGD | AGA Non-FGD | LGA | p-Value |
|---|---|---|---|---|---|---|---|
| Any adverse perinatal outcome | 258 (24.2) | 17 (31.5) | 18 (40.9) | 74 (24.4) | 113 (22.3) | 36 (22.5) | 0.050 |
| Arterial cord blood pH ≤ 7.10 | 61 (5.7) | 5 (9.3) | 5 (11.4) | 13 (4.3) | 27 (5.3) | 11 (6.9) | 0.236 |
| 5 min Apgar score ≤ 7 | 8 (0.7) | 0 (0.0) | 0 (0.0) | 4 (1.3) | 2 (0.4) | 2 (1.2) | 0.475 |
| Cesarean delivery for NRFS | 46 (4.3) | 6 (11.1) | 3 (6.8) | 16 (5.3) | 18 (3.6) | 3 (1.9) | 0.034 |
| Instrumental delivery for NRFS | 20 (1.9) | 3 (5.6) | 3 (6.8) | 5 (1.7) | 8 (1.6) | 1 (0.6) | 0.030 |
| Basic neonatal resuscitation | 177 (16.6) | 12 (22.2) | 10 (22.7) | 52 (17.2) | 72 (14.2) | 31 (19.4) | 0.245 |
| Advanced neonatal resuscitation | 37 (3.5) | 5 (9.3) | 2 (4.5) | 11 (3.6) | 13 (2.6) | 6 (3.) | 0.144 |
| Admission at birth in NICU | 28 (2.6) | 3 (5.6) | 4 (9.1) | 5 (1.7) | 10 (2.0) | 6 (3.8) | 0.023 |
| Adverse Effect | AUC (95% CI) | Sensitivity a FPR 10% (Specificity 90%) | Birthweight Percentile Threshold |
|---|---|---|---|
| Any adverse perinatal outcome | 0.53 (0.49, 0.57) | 14% | 41.3 |
| Arterial cord blood pH ≤ 7.10 | 0.53 (0.46, 0.60) | 13% | 42.0 |
| 5 min Apgar score ≤ 7 | 0.53 (0.30, 0.76) | 25% | 42.0 |
| Cesarean delivery for NRFS | 0.63 (0.54, 0.71) | 26% | 41.4 |
| Instrumental delivery for NRFS | 0.54 (0.43, 0.65) | 0% | 42.4 |
| Basic neonatal resuscitation | 0.52 (0.47, 0.57) | 13% | 41.8 |
| Advanced neonatal resuscitation | 0.57 (0.48, 0.66) | 19% | 41.8 |
| Admission at birth in NICU | 0.55 (0.44, 0.67) | 7% | 47.1 |
| Percentile Decrease Cutoff | |||
|---|---|---|---|
| Adverse Effect | 30 | 40 | 50 |
| Any adverse perinatal outcome | 1.18 (0.88, 1.58) | 1.36 (0.98, 1.90) | 1.40 (0.89, 2.19) |
| Arterial cord blood pH≤7.10 | 1.24 (0.64, 2.39) | 1.25 (0.56, 2.79) | 1.17 (0.37, 3.72) |
| 5 min Apgar score ≤ 7 | 2.78 (0.39, 19.59) | 4.82 (0.69, 33.8) | |
| Cesarean delivery for NRFS | 1.70 (0.82, 3.53) | 2.41 (1.11, 5.21) | 2.93 (1.14, 7.54) |
| Instrumental delivery for NRFS | 0.70 (0.15, 3.24) | ||
| Basic neonatal resuscitation | 1.24 (0.84, 1.81) | 1.41 (0.91, 2.18) | 1.32 (0.70, 2.47) |
| Advanced neonatal resuscitation | 1.07 (0.39, 2.96) | 1.85 (0.68, 5.09) | 1.62 (0.38, 6.98) |
| Admission at birth in NICU | 0.83 (0.23, 3.00) | 0.96 (0.21, 4.33) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galán Arévalo, M.S.; Mahillo-Fernández, I.; Esteban, L.M.; Andeyro-García, M.; Piñeiro Pérez, R.; Saénz de Pipaón, M.; Savirón-Cornudella, R. Perinatal Adverse Effects in Newborns with Estimated Loss of Weight Percentile between the Third Trimester Ultrasound and Delivery. The GROWIN Study. J. Clin. Med. 2021, 10, 4643. https://doi.org/10.3390/jcm10204643
Galán Arévalo MS, Mahillo-Fernández I, Esteban LM, Andeyro-García M, Piñeiro Pérez R, Saénz de Pipaón M, Savirón-Cornudella R. Perinatal Adverse Effects in Newborns with Estimated Loss of Weight Percentile between the Third Trimester Ultrasound and Delivery. The GROWIN Study. Journal of Clinical Medicine. 2021; 10(20):4643. https://doi.org/10.3390/jcm10204643
Chicago/Turabian StyleGalán Arévalo, María Sonsoles, Ignacio Mahillo-Fernández, Luis Mariano Esteban, Mercedes Andeyro-García, Roi Piñeiro Pérez, Miguel Saénz de Pipaón, and Ricardo Savirón-Cornudella. 2021. "Perinatal Adverse Effects in Newborns with Estimated Loss of Weight Percentile between the Third Trimester Ultrasound and Delivery. The GROWIN Study" Journal of Clinical Medicine 10, no. 20: 4643. https://doi.org/10.3390/jcm10204643
APA StyleGalán Arévalo, M. S., Mahillo-Fernández, I., Esteban, L. M., Andeyro-García, M., Piñeiro Pérez, R., Saénz de Pipaón, M., & Savirón-Cornudella, R. (2021). Perinatal Adverse Effects in Newborns with Estimated Loss of Weight Percentile between the Third Trimester Ultrasound and Delivery. The GROWIN Study. Journal of Clinical Medicine, 10(20), 4643. https://doi.org/10.3390/jcm10204643








