3D-Analysis of the Proximal Humeral Anatomy before and after Stemless Shoulder Arthroplasty—A Prospective Case Series Study
Abstract
1. Introduction
2. Experimental Section
2.1. Study Design
2.2. Patient Selection
2.3. Subjective and Functional Outcome Scoring
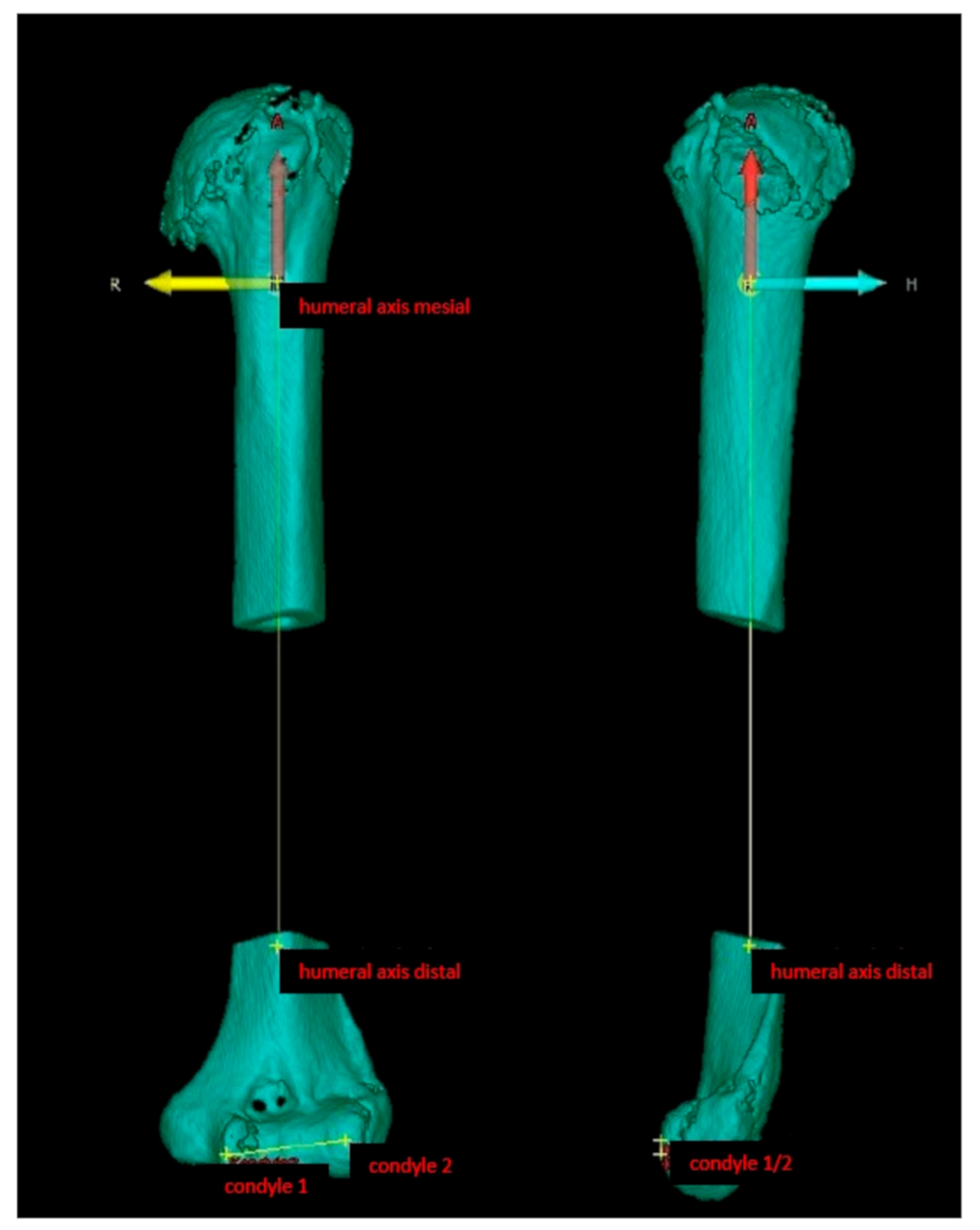
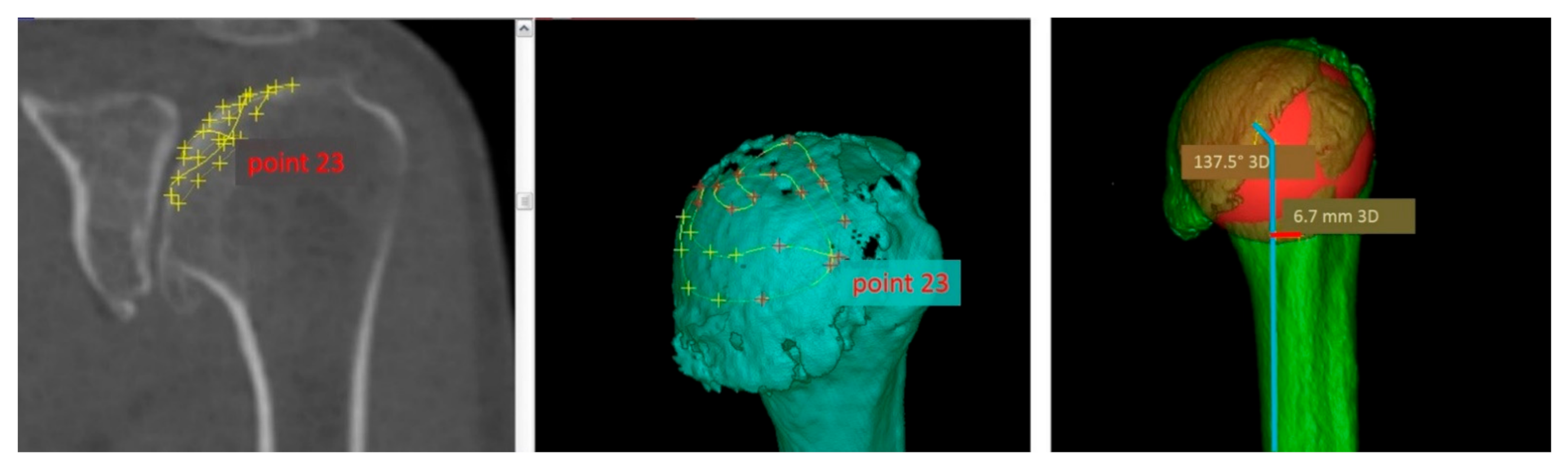
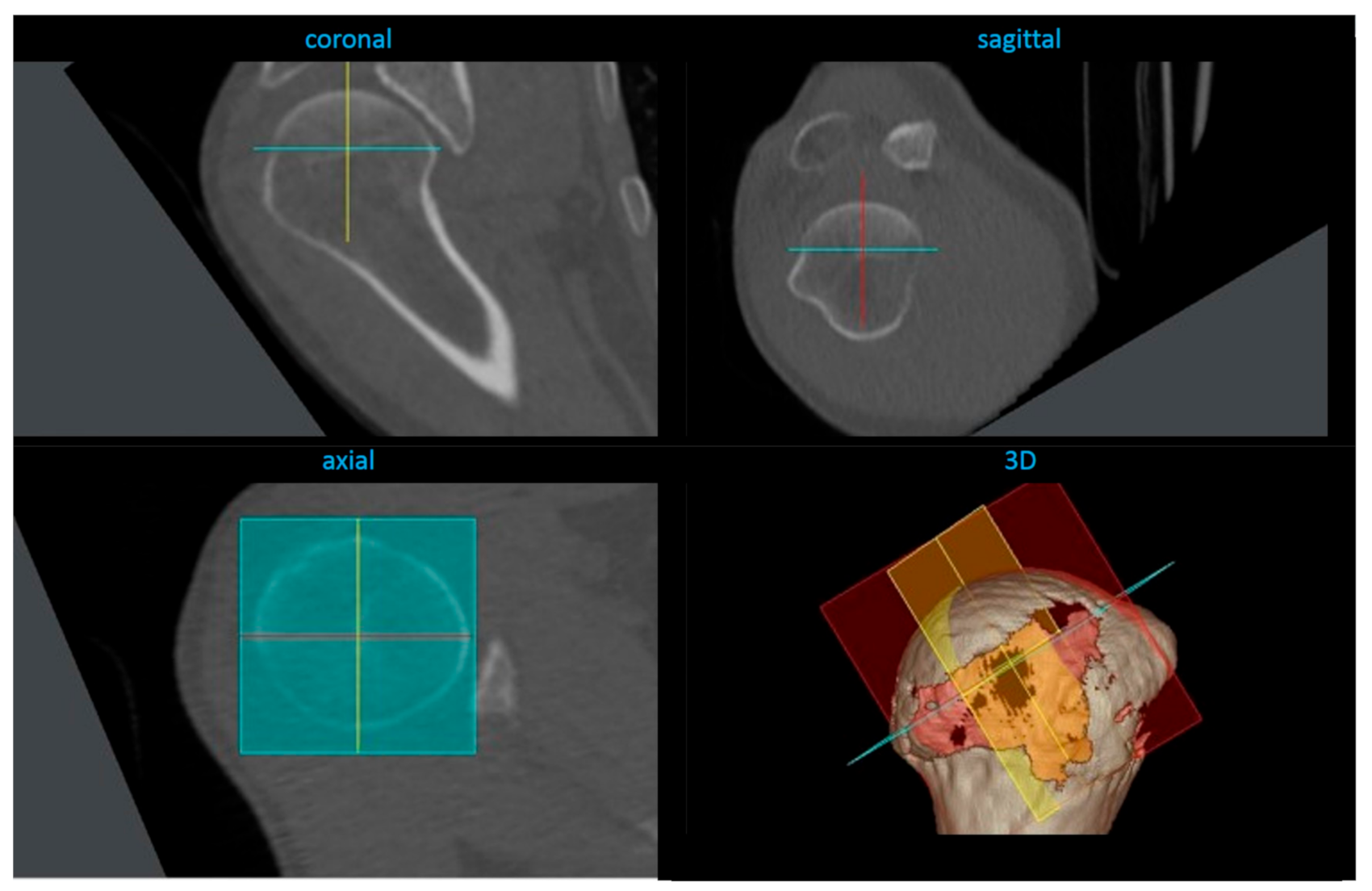
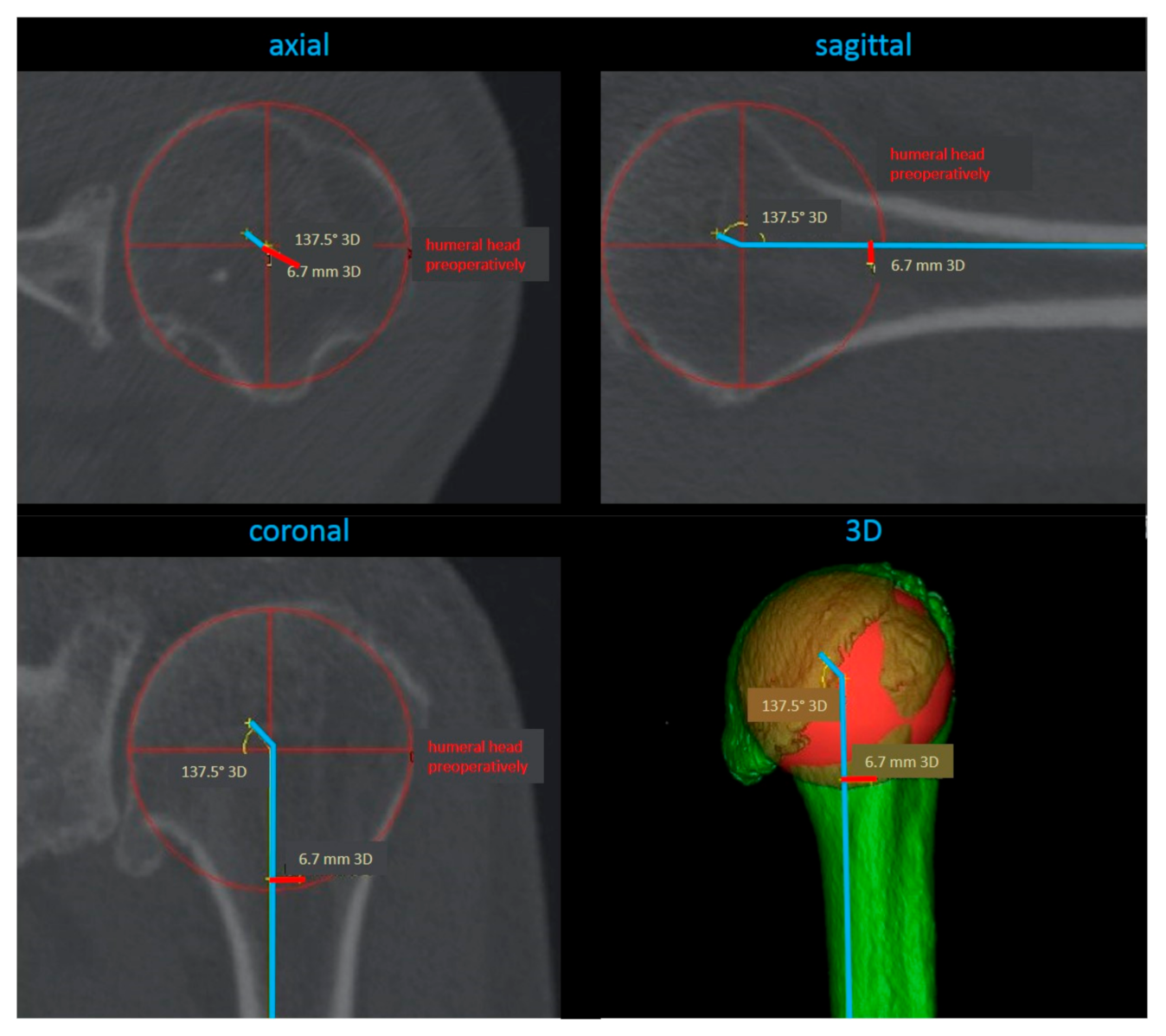
2.4. Radiological Analysis
2.5. Surgical Procedure
2.6. Statistical Analysis
3. Results
3.1. General Data
3.2. Clinical Outcome
3.3. Radiological Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hawi, N.; Tauber, M.; Messina, M.J.; Habermeyer, P.; Martetschläger, F. Anatomic stemless shoulder arthroplasty and related outcomes: A systematic review. BMC Musculoskelet. Disord. 2016, 17, 376. [Google Scholar] [CrossRef] [PubMed]
- Brabston, E.W.; Fehringer, E.V.; Owen, M.T.; Ponce, B.A. Stemless Humeral Implants in Total Shoulder Arthroplasty. J. Am. Acad. Orthop. Surg. 2020, 28, e277–e287. [Google Scholar] [CrossRef]
- Churchill, R.S. Stemless shoulder arthroplasty: Current status. J. Shoulder Elb. Surg. 2014, 23, 1409–1414. [Google Scholar] [CrossRef]
- Lazarus, M.D.; Cox, R.M.; Murthi, A.M.; Levy, O.; Abboud, J.A. Stemless Prosthesis for Total Shoulder Arthroplasty. J. Am. Acad. Orthop. Surg. 2017, 25, e291–e300. [Google Scholar] [CrossRef]
- Churchill, R.S.; Athwal, G.S. Stemless shoulder arthroplasty—Current results and designs. Curr. Rev. Musculoskelet. Med. 2016, 9, 10–16. [Google Scholar] [CrossRef]
- Huguet, D.; Declercq, G.; Rio, B.; Teissier, J.; Zipoli, B. Results of a new stemless shoulder prosthesis: Radiologic proof of maintained fixation and stability after a minimum of three years’ follow-up. J. Shoulder Elb. Surg. 2010, 19, 847–852. [Google Scholar] [CrossRef]
- Beck, S.; Beck, V.; Wegner, A.; Dudda, M.; Patsalis, T.; Jäger, M. Long-term survivorship of stemless anatomical shoulder replacement. Int. Orthop. 2018, 42, 1327–1330. [Google Scholar] [CrossRef]
- Brolin, T.J.; Cox, R.M.; Abboud, J.A.; Namdari, S. Stemless Shoulder Arthroplasty: Review of Early Clinical and Radiographic Results. JBJS Rev. 2017, 5, e3. [Google Scholar] [CrossRef]
- Von Engelhardt, L.V.; Manzke, M.; Breil-Wirth, A.; Filler, T.J.; Jerosch, J. Restoration of the joint geometry and outcome after stemless TESS shoulder arthroplasty. World J. Orthop. 2017, 8, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Kadum, B.; Hassany, H.; Wadsten, M.; Sayed-Noor, A.; Sjoden, G. Geometrical analysis of stemless shoulder arthroplasty: A radiological study of seventy TESS total shoulder prostheses. Int. Orthop. 2015, 40, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Alolabi, B.; Youderian, A.R.; Napolitano, L.; Szerlip, B.W.; Evans, P.J.; Nowinski, R.J.; Ricchetti, E.T.; Iannotti, J.P. Radiographic assessment of prosthetic humeral head size after anatomic shoulder arthroplasty. J. Shoulder Elb. Surg. 2014, 23, 1740–1746. [Google Scholar] [CrossRef]
- Pinto, M.C.; Archie, A.T.; Mosher, Z.A.; Ransom, E.F.; McGwin, G.; Fehringer, E.V.; Brabston, E.W., III; Ponce, B.A. Radiographic restoration of native anatomy: A comparison between stemmed and stemless shoulder arthroplasty. J. Shoulder Elb. Surg. 2019, 28, 1595–1600. [Google Scholar] [CrossRef] [PubMed]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C.; Beaton, D.; Cole, D.; Davis, A.; Hawker, G.; Katz, J.N.; Makela, M.; Marx, R.G.; et al. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Constant, C.R.; Murley, A.H. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Medelnik, J.; Hertrich, K.; Steinhauser-Andresen, S.; Hirschfelder, U.; Hofmann, E. Accuracy of anatomical landmark identification using different CBCT- and MSCT-based 3D images: An in vitro study. J. Orofac. Orthop. 2011, 72, 261–278. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.N.; Foley, A.P.; Swallow, H.M.; Wallace, W.A.; Coughlan, D.P. The geometry of the humeral head and the design of prostheses. J. Bone Jt. Surg. 1991, 73, 647–655. [Google Scholar] [CrossRef] [PubMed]
- Boileau, P.; Walch, G. The three-dimensional geometry of the proximal humerus. Implications for surgical technique and prosthetic design. J. Bone Jt. Surg. 1997, 79, 857–865. [Google Scholar] [CrossRef]
- Iannotti, J.P.; Gabriel, J.P.; Schneck, S.L.; Evans, B.G.; Misra, S. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J. Bone Jt. Surg. 1992, 74, 491–500. [Google Scholar] [CrossRef]
- Pearl, M.L.; Volk, A.G. Coronal plane geometry of the proximal humerus relevant to prosthetic arthroplasty. J. Shoulder Elb. Surg. 1996, 5, 320–326. [Google Scholar] [CrossRef]
- Kummer, F.J.; Perkins, R.; Zuckerman, J.D. The use of the bicipital groove for alignment of the humeral stem in shoulder arthroplasty. J. Shoulder Elb. Surg. 1998, 7, 144–146. [Google Scholar] [CrossRef]
- Hertel, R.; Knothe, U.; Ballmer, F.T. Geometry of the proximal humerus and implications for prosthetic design. J. Shoulder Elb. Surg. 2002, 11, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Hawi, N.; Magosch, P.; Tauber, M.; Lichtenberg, S.; Habermeyer, P. Nine-year outcome after anatomic stemless shoulder prosthesis: Clinical and radiologic results. J. Shoulder Elb. Surg. 2017, 26, 1609–1615. [Google Scholar] [CrossRef] [PubMed]
- Jia, X.; Chen, Y.-X.; Qiang, M.; Zhang, K.; Li, H.; Jiang, Y.; Zhang, Y. Compared to X-ray, three-dimensional computed tomography measurement is a reproducible radiographic method for normal proximal humerus. J. Orthop. Surg. Res. 2016, 11, 82. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Mean | SD | Min | Max | |
|---|---|---|---|---|---|
| retroversion | preop. | 20.9 * | 13.8 | 1.9 | 52.8 |
| postop. | 21.8 * | 16.4 | 1.5 | 51.0 | |
| contralateral | 29.6 * | 12.5 | 8.7 | 52.8 | |
| inclination | preop. | 125.5 | 17.2 | 41.0 | 142.7 |
| postop. | 130.3 | 7.9 | 114.4 | 146.2 | |
| contralateral | 131.3 | 5.9 | 119.3 | 141.6 | |
| medial offset | preop. | 4.0 | 1.5 | 0.6 | 6.4 |
| postop. | 3.6 | 2.2 | 0.3 | 10.2 | |
| contralateral | 4.1 | 1.8 | 0.2 | 6.9 | |
| posterior offset | preop. | 2.3 | 1.5 | 0 | 5.1 |
| postop. | 1.6 | 1.5 | 0 | 5.5 | |
| contralateral | 1.6 | 1.3 | 0.1 | 5.6 | |
| head height | preop. | 17.1 * | 3.1 | 10.6 | 23.8 |
| postop. | 14.5 * | 1.4 | 13.0 | 18.0 | |
| contralateral | 16.9 * | 2.5 | 12.8 | 22.2 | |
| head radius | preop. | 24.4 * | 3.0 | 18.7 | 31.6 |
| postop. | 23.5 | 1.4 | 22.0 | 27.0 | |
| contralateral | 23.4 * | 2.8 | 18.6 | 29.1 | |
| minimal resection diameter | preop. | 46.9 * | 5.8 | 37.2 | 58.4 |
| contralateral | 44.8 * | 4.8 | 37.6 | 57.9 | |
| maximal resection diameter | preop. | 50.4 * | 6.1 | 39.6 | 63.9 |
| contralateral | 47.9 * | 5.1 | 38 | 60.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koch, M.; Frankewycz, B.; Voss, A.; Kaeaeb, M.; Herrmann, S.; Alt, V.; Greiner, S. 3D-Analysis of the Proximal Humeral Anatomy before and after Stemless Shoulder Arthroplasty—A Prospective Case Series Study. J. Clin. Med. 2021, 10, 259. https://doi.org/10.3390/jcm10020259
Koch M, Frankewycz B, Voss A, Kaeaeb M, Herrmann S, Alt V, Greiner S. 3D-Analysis of the Proximal Humeral Anatomy before and after Stemless Shoulder Arthroplasty—A Prospective Case Series Study. Journal of Clinical Medicine. 2021; 10(2):259. https://doi.org/10.3390/jcm10020259
Chicago/Turabian StyleKoch, Matthias, Borys Frankewycz, Andreas Voss, Max Kaeaeb, Sebastian Herrmann, Volker Alt, and Stefan Greiner. 2021. "3D-Analysis of the Proximal Humeral Anatomy before and after Stemless Shoulder Arthroplasty—A Prospective Case Series Study" Journal of Clinical Medicine 10, no. 2: 259. https://doi.org/10.3390/jcm10020259
APA StyleKoch, M., Frankewycz, B., Voss, A., Kaeaeb, M., Herrmann, S., Alt, V., & Greiner, S. (2021). 3D-Analysis of the Proximal Humeral Anatomy before and after Stemless Shoulder Arthroplasty—A Prospective Case Series Study. Journal of Clinical Medicine, 10(2), 259. https://doi.org/10.3390/jcm10020259






