Animal Model Dependent Response to Pentagalloyl Glucose in Murine Abdominal Aortic Injury
Abstract
1. Introduction
2. Materials and Methods
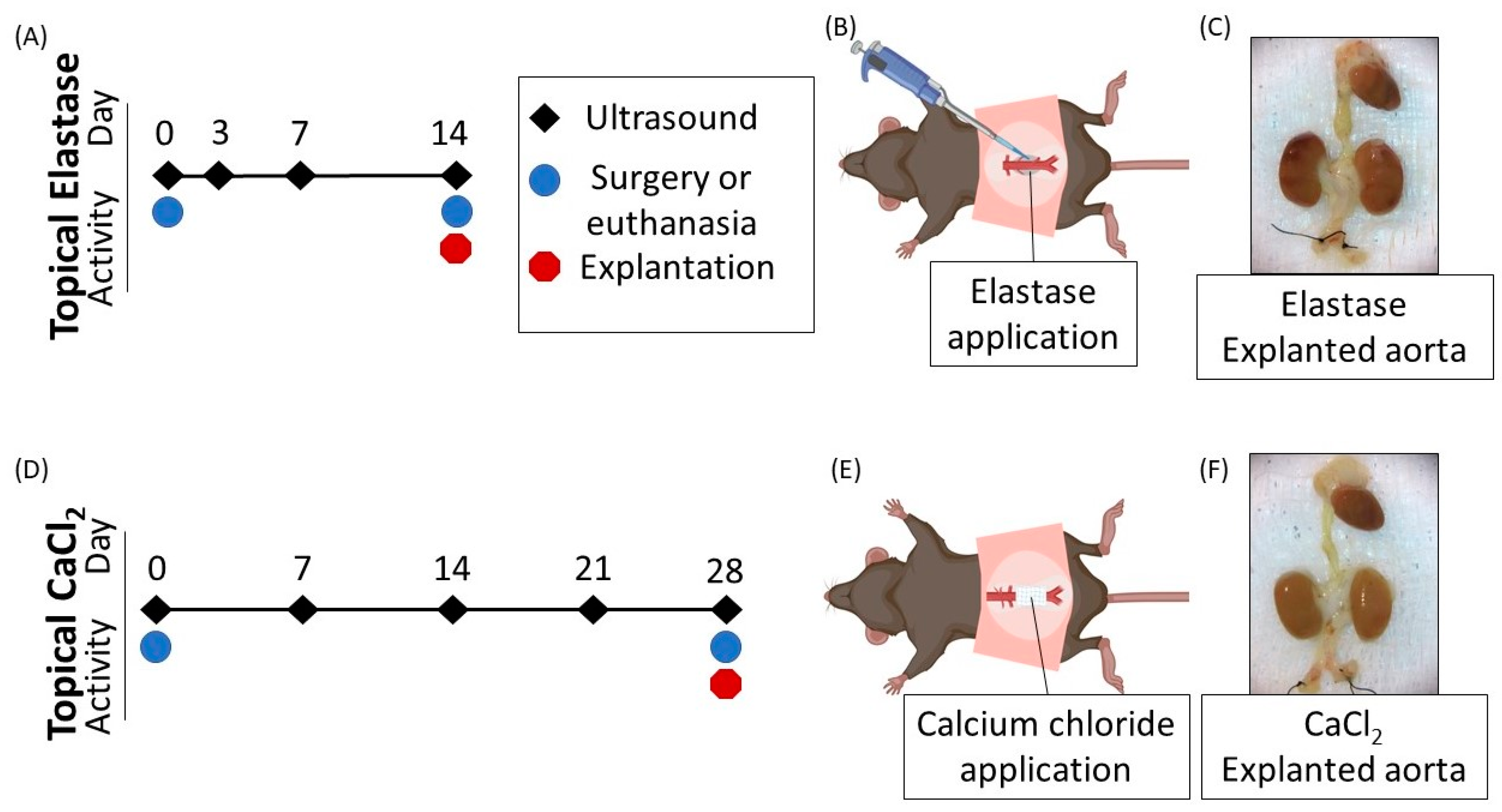
2.1. Surgical Procedure
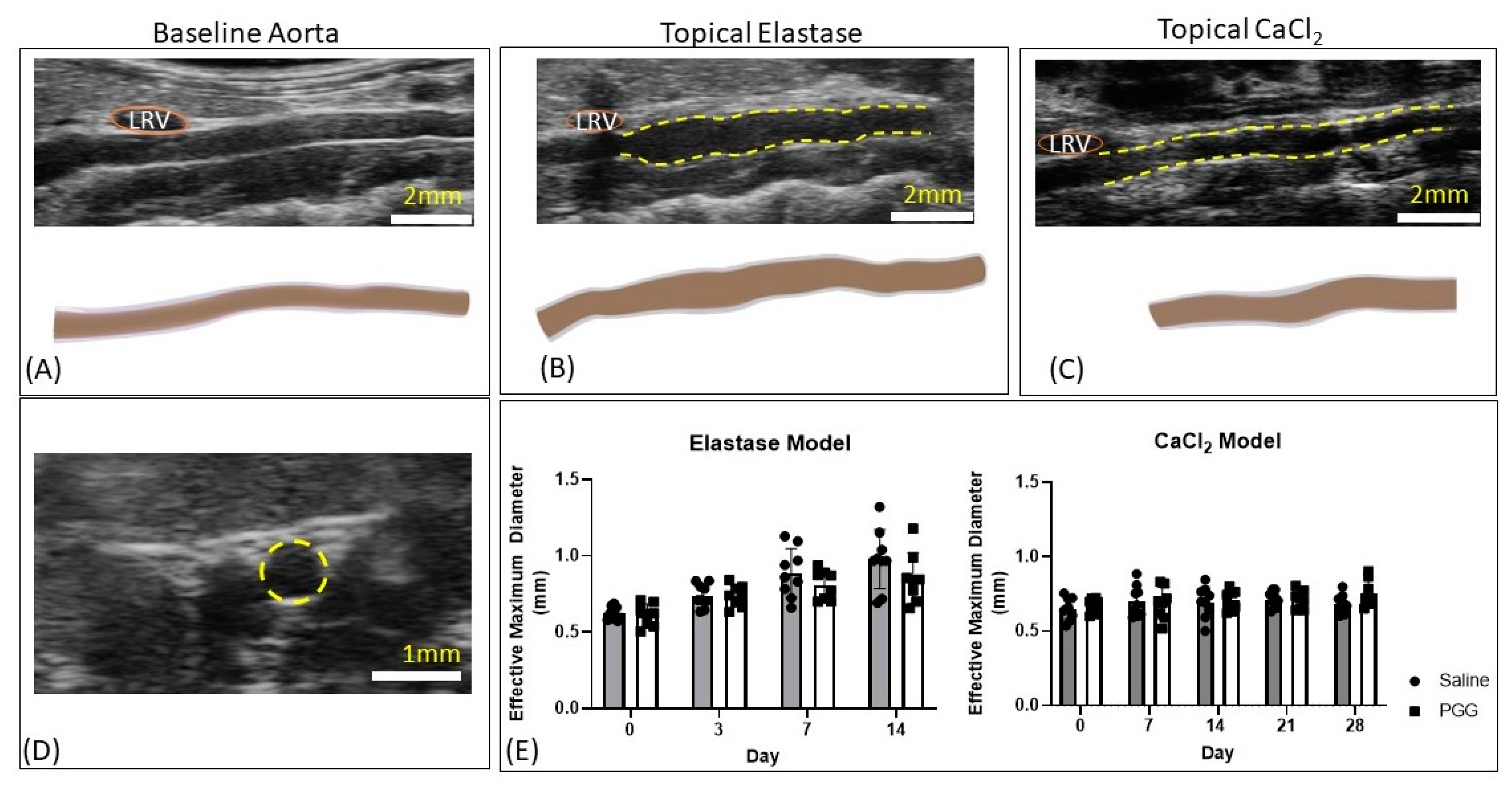
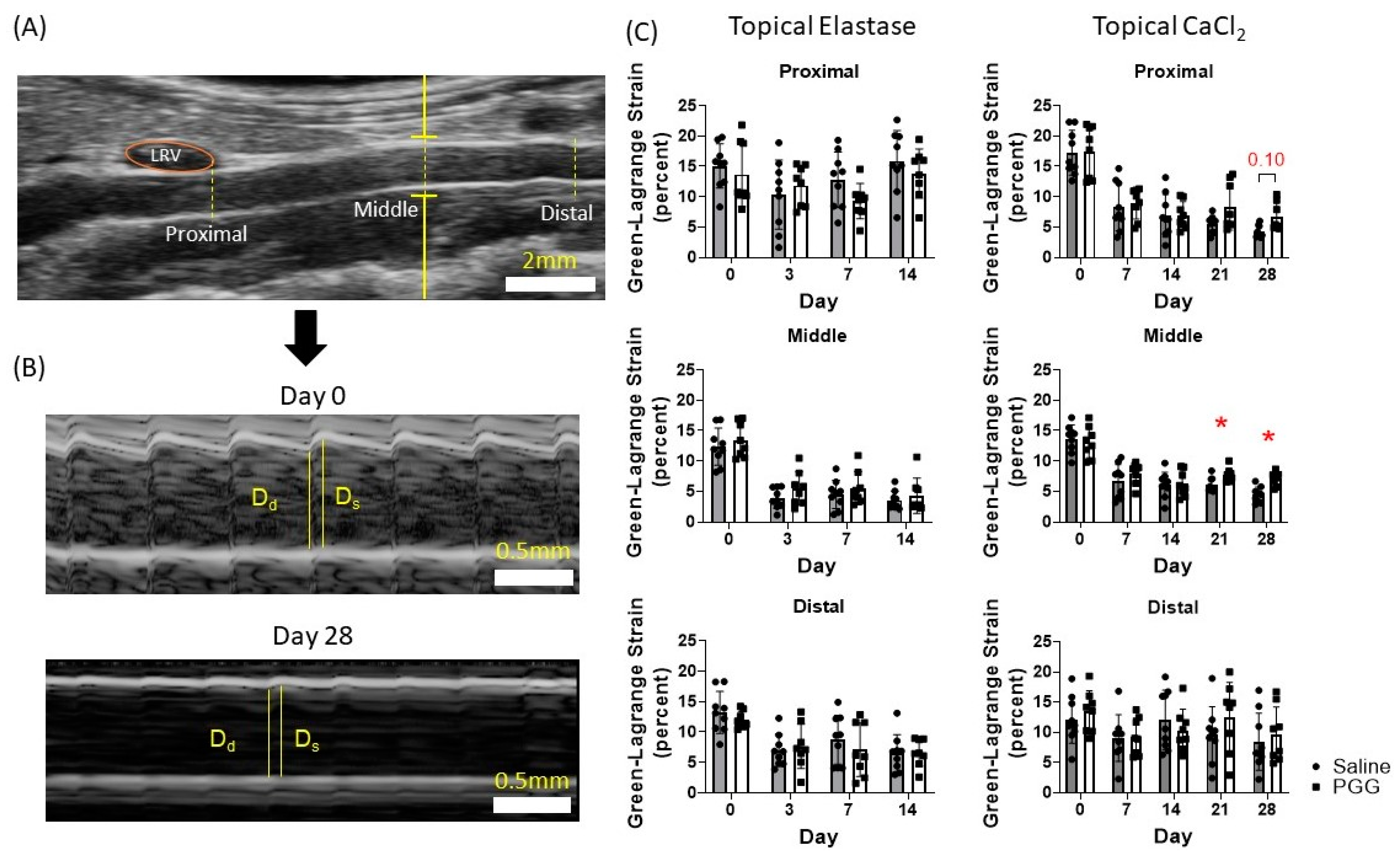
2.2. Imaging Protocol
2.3. Biomechanical Testing
2.4. Histologic Preparation and Analysis
2.4.1. Microstructural Quantification
2.4.2. Intima-Media and Adventitial Thickness
2.5. Statistical Analysis
3. Results
3.1. In Vivo Imaging Revealed Preserved Green-Lagrange Circumferential Cyclic Strain in the PGG-Treated CaCl2 Group
3.2. Biomechanical Testing Demonstrated No Significant Difference in Burst Pressure or Time to Failure
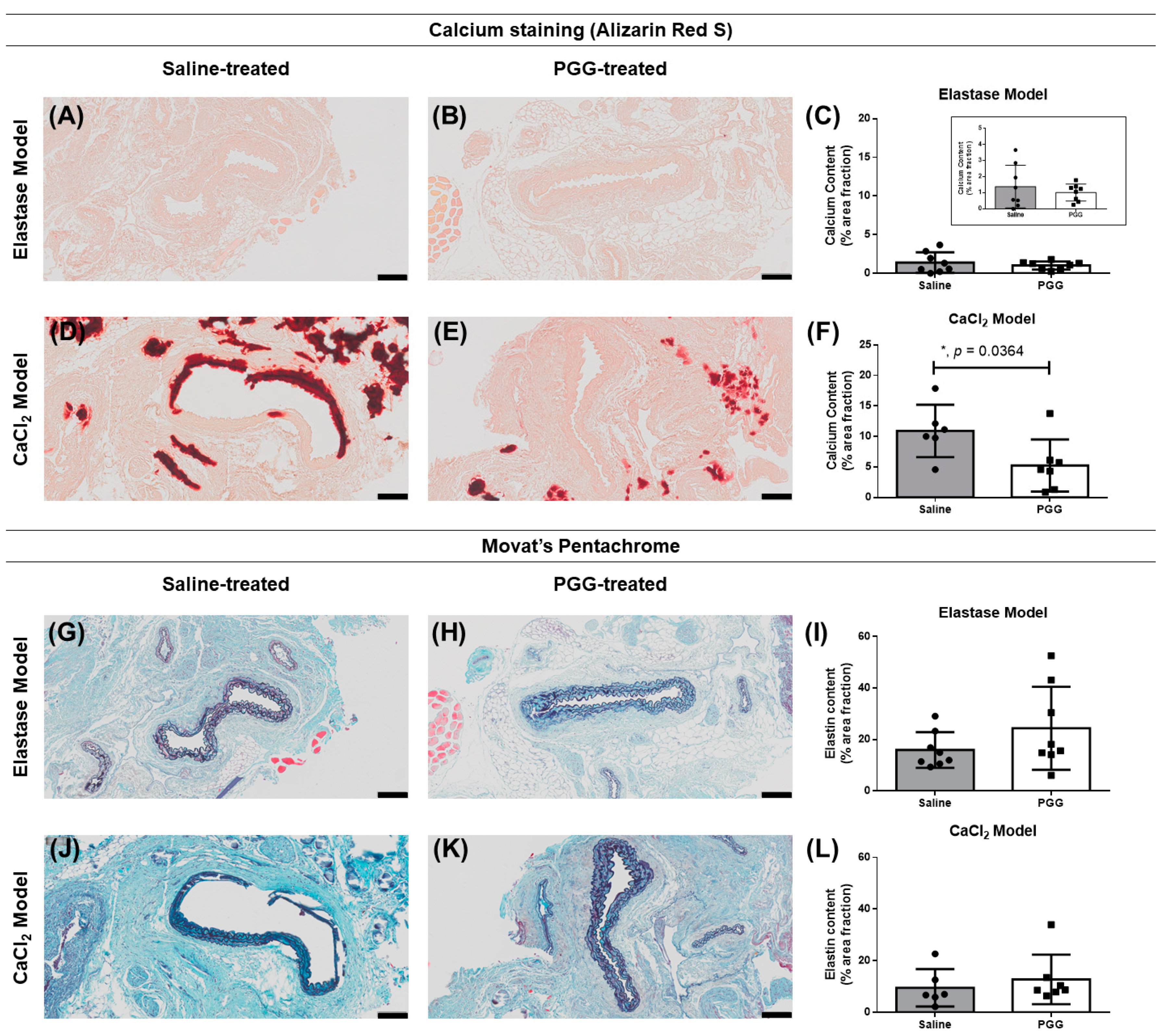
3.3. Histology Showed a Significant Difference in Calcium Deposition in the PGG-Treated CaCl2 Model
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Animal Care and Use Committee Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Underlying Cause of Death, 1999–2015 Results Form. Available online: https://wonder.cdc.gov/controller/datarequest/D76;jsessionid=ED3A4ABA7F918FF39FB54B2B5919F1B9 (accessed on 27 August 2017).
- Benjamin, E.J.M.; Blaha, M.J.M.; Chiuve, S.E.S.; Cushman, M.M.; Das, S.R.M.; Deo, R.M.; de Ferranti, S.D.M.; Floyd, J.M.; Fornage, M.; Gillespie, C.M.; et al. Heart Disease and Stroke Statistics-2017 Update: A Report from the American Heart Association. Circulation 2017, 135. [Google Scholar] [CrossRef]
- Nicholls, S.C.; Gardner, J.B.; Meissner, M.H.; Johansen, K.H. Rupture in small abdominal aortic aneurysms. J. Vasc. Surg. 1998, 28, 884–888. [Google Scholar] [CrossRef]
- Wilmink, T.B.M.; Quick, C.R.G.; Hubbard, C.S.; Day, N.E. The influence of screening on the incidence of ruptured abdominal aortic aneurysms. J. Vasc. Surg. 1999, 30, 203–208. [Google Scholar] [CrossRef]
- Grant, S.W.; Grayson, A.D.; Purkayastha, D.; Wilson, S.D.; McCollum, C. Logistic risk model for mortality following elective abdominal aortic aneurysm repair. BJS Br. J. Surg. 2011, 98, 652–658. [Google Scholar] [CrossRef]
- Lederle, F.A.; Kane, R.L.; MacDonald, R.; Wilt, T.J. Systematic Review: Repair of Unruptured Abdominal Aortic Aneurysm. Ann. Intern. Med. 2007, 146, 735–741. [Google Scholar] [CrossRef]
- Patnaik, S.S.; Simionescu, D.T.; Goergen, C.J.; Hoyt, K.; Sirsi, S.; Finol, E.A. Pentagalloyl Glucose and Its Functional Role in Vascular Health: Biomechanics and Drug-Delivery Characteristics. Ann. Biomed. Eng. 2019, 47, 39–59. [Google Scholar] [CrossRef]
- Isenburg, J.C.; Simionescu, D.T.; Starcher, B.C.; Vyavahare, N.R. Elastin Stabilization for Treatment of Abdominal Aortic Aneurysms. Circulation 2007, 115, 1729–1737. [Google Scholar] [CrossRef]
- Patnaik, S.S.; Piskin, S.; Pillalamarri, N.R.; Romero, G.; Escobar, G.P.; Sprague, E.; Finol, E.A. Biomechanical Restoration Potential of Pentagalloyl Glucose after Arterial Extracellular Matrix Degeneration. Bioengineering 2019, 6, 58. [Google Scholar] [CrossRef]
- Pavey, S.N.; Cocciolone, A.J.; Gutierrez Marty, A.; Ismail, H.N.; Hawes, J.Z.; Wagenseil, J.E. Pentagalloyl Glucose (PGG) Partially Prevents Arterial Mechanical Changes Due to Elastin Degradation. Exp. Mech. 2020. [Google Scholar] [CrossRef]
- Nosoudi, N.; Chowdhury, A.; Siclari, S.; Parasaram, V.; Karamched, S.; Vyavahare, N. Systemic Delivery of Nanoparticles Loaded with Pentagalloyl Glucose Protects Elastic Lamina and Prevents Abdominal Aortic Aneurysm in Rats. J. Cardiovasc. Transl. Res. 2016, 9, 445–455. [Google Scholar] [CrossRef]
- Nosoudi, N.; Chowdhury, A.; Siclari, S.; Karamched, S.; Parasaram, V.; Parrish, J.; Gerard, P.; Vyavahare, N. Reversal of Vascular Calcification and Aneurysms in a Rat Model Using Dual Targeted Therapy with EDTA- and PGG-Loaded Nanoparticles. Theranostics 2016, 6, 1975–1987. [Google Scholar] [CrossRef] [PubMed]
- Thirugnanasambandam, M.; Simionescu, D.T.; Escobar, P.G.; Sprague, E.; Goins, B.; Clarke, G.D.; Han, H.-C.; Amezcua, K.L.; Adeyinka, O.R.; Goergen, C.J.; et al. The Effect of Pentagalloyl Glucose on the Wall Mechanics and Inflammatory Activity of Rat Abdominal Aortic Aneurysms. J. Biomech. Eng. 2018, 140, 0845021–0845029. [Google Scholar] [CrossRef] [PubMed]
- Dhital, S.; Vyavahare, N.R. Nanoparticle-based targeted delivery of pentagalloyl glucose reverses elastase-induced abdominal aortic aneurysm and restores aorta to the healthy state in mice. PLoS ONE 2020, 15, e0227165. [Google Scholar] [CrossRef] [PubMed]
- Kloster, B.O.; Lund, L.; Lindholt, J.S. Inhibition of early AAA formation by aortic intraluminal pentagalloyl glucose (PGG) infusion in a novel porcine AAA model. Ann. Med. Surg. 2016, 7, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Simionescu, D.; Casco, M.; Turner, J.; Rierson, N.; Yue, J.; Ning, K. Chemical stabilization of the extracellular matrix attenuates growth of experimentally induced abdominal aorta aneurysms in a large animal model. JVS Vasc. Sci. 2020, 1, 69–80. [Google Scholar] [CrossRef]
- Isenburg, J.C.; Karamchandani, N.V.; Simionescu, D.T.; Vyavahare, N.R. Structural requirements for stabilization of vascular elastin by polyphenolic tannins. Biomaterials 2006, 27, 3645–3651. [Google Scholar] [CrossRef]
- Schack, A.S.; Stubbe, J.; Steffensen, L.B.; Mahmoud, H.; Laursen, M.S.; Lindholt, J.S. Intraluminal infusion of Penta-Galloyl Glucose reduces abdominal aortic aneurysm development in the elastase rat model. PLoS ONE 2020, 15, e0234409. [Google Scholar] [CrossRef]
- Patelis, N.; Moris, D.; Schizas, D.; Damaskos, C.; Perrea, D.; Bakoyiannis, C.; Liakakos, T.; Georgopoulos, S. Animal models in the research of abdominal aortic aneurysms development. Physiol. Res. 2017, 66, 899–915. [Google Scholar] [CrossRef]
- Anidjar, S.; Salzmann, J.L.; Gentric, D.; Lagneau, P.; Camilleri, J.P.; Michel, J.B. Elastase-induced experimental aneurysms in rats. Circulation 1990, 82, 973–981. [Google Scholar] [CrossRef]
- Bhamidipati, C.M.; Mehta, G.S.; Lu, G.; Moehle, C.W.; Barbery, C.; DiMusto, P.D.; Laser, A.; Kron, I.L.; Upchurch, G.R.; Ailawadi, G. Development of a novel murine model of aortic aneurysms using peri-adventitial elastase. Surgery 2012, 152, 238–246. [Google Scholar] [CrossRef]
- Gertz, S.D.; Kurgan, A.; Eisenberg, D. Aneurysm of the rabbit common carotid artery induced by periarterial application of calcium chloride in vivo. J. Clin. Investig. 1988, 81, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Romary, D.J.; Berman, A.G.; Goergen, C.J. High-frequency murine ultrasound provides enhanced metrics of BAPN-induced AAA growth. Am. J. Physiol. Heart Circ. Physiol. 2019, 317, H981–H990. [Google Scholar] [CrossRef]
- Daugherty, A.; Cassis, L.A. Mouse Models of Abdominal Aortic Aneurysms. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Updegrove, A.; Wilson, N.M.; Merkow, J.; Lan, H.; Marsden, A.L.; Shadden, S.C. SimVascular: An Open Source Pipeline for Cardiovascular Simulation. Ann. Biomed. Eng. 2017, 45, 525–541. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y.; Han, B.; Lamm, S.D.; Fierro, C.A.; Han, H.-C. Effects of elastin degradation and surrounding matrix support on artery stability. Am. J. Physiol. Heart Circ. Physiol. 2011, 302, H873–H884. [Google Scholar] [CrossRef] [PubMed]
- von Bornstädt, D.; Wang, H.; Paulsen, M.J.; Goldstone, A.B.; Eskandari, A.; Thakore, A.; Stapleton, L.; Steele, A.N.; Truong, V.N.; Jaatinen, K.; et al. Rapid Self-Assembly of Bioengineered Cardiovascular Bypass Grafts From Scaffold-Stabilized, Tubular Bilevel Cell Sheets. Circulation 2018, 138, 2130–2144. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Lane, B.A.; Eberth, J.F.; Lessner, S.M.; Vyavahare, N.R. Gold nanoparticles that target degraded elastin improve imaging and rupture prediction in an AngII mediated mouse model of abdominal aortic aneurysm. Theranostics 2019, 9, 4156–4167. [Google Scholar] [CrossRef] [PubMed]
- Gaul, R.T.; Nolan, D.R.; Ristori, T.; Bouten, C.V.C.; Loerakker, S.; Lally, C. Pressure-induced collagen degradation in arterial tissue as a potential mechanism for degenerative arterial disease progression. J. Mech. Behav. Biomed. Mater. 2020, 109, 103771. [Google Scholar] [CrossRef]
- Bhutda, S.; Surve, M.V.; Anil, A.; Kamath, K.; Singh, N.; Modi, D.; Banerjee, A. Histochemical Staining of Collagen and Identification of Its Subtypes by Picrosirius Red Dye in Mouse Reproductive Tissues. Bio-Protocol 2017, 7, e2592. [Google Scholar] [CrossRef]
- Wegner, K.A.; Keikhosravi, A.; Eliceiri, K.W.; Vezina, C.M. Fluorescence of Picrosirius Red Multiplexed With Immunohistochemistry for the Quantitative Assessment of Collagen in Tissue Sections. J. Histochem. Cytochem. 2017, 65, 479–490. [Google Scholar] [CrossRef]
- Gequelim, G.C.; da Luz Veronez, D.A.; Lenci Marques, G.; Tabushi, C.H.; da Rocha Loures Bueno, R. Thoracic aorta thickness and histological changes with aging: An experimental rat model. J. Geriatr. Cardiol. 2019, 16, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.A.; Rasband, W.S.; Eliceiri, K.W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 2012, 9, 671–675. [Google Scholar] [CrossRef] [PubMed]
- Le, V.P.; Cheng, J.K.; Kim, J.; Staiculescu, M.C.; Ficker, S.W.; Sheth, S.C.; Bhayani, S.A.; Mecham, R.P.; Yanagisawa, H.; Wagenseil, J.E. Mechanical factors direct mouse aortic remodelling during early maturation. J. R. Soc. Interface 2015, 12, 20141350. [Google Scholar] [CrossRef]
- Huang, W.; Sher, Y.-P.; Delgado-West, D.; Wu, J.T.; Peck, K.; Fung, Y.C. Tissue Remodeling of Rat Pulmonary Artery in Hypoxic Breathing. I. Changes of Morphology, Zero-Stress State, and Gene Expression. Ann. Biomed. Eng. 2001, 29, 535–551. [Google Scholar] [CrossRef] [PubMed]
- Holzapfel, G.A.; Gasser, T.C.; Ogden, R.W. A New Constitutive Framework for Arterial Wall Mechanics and a Comparative Study of Material Models. J. Elast. Phys. Sci. Solids 2000, 61, 1–48. [Google Scholar] [CrossRef]
- Laterreur, V.; Ruel, J.; Auger, F.A.; Vallières, K.; Tremblay, C.; Lacroix, D.; Tondreau, M.; Bourget, J.-M.; Germain, L. Comparison of the direct burst pressure and the ring tensile test methods for mechanical characterization of tissue-engineered vascular substitutes. J. Mech. Behav. Biomed. Mater. 2014, 34, 253–263. [Google Scholar] [CrossRef]
- Kuivaniemi, H.; Ryer, E.J.; Elmore, J.R.; Tromp, G. Understanding the pathogenesis of abdominal aortic aneurysms. Expert Rev. Cardiovasc. Ther. 2015, 13, 975–987. [Google Scholar] [CrossRef]
- Chuang, T.-H.; Stabler, C.; Simionescu, A.; Simionescu, D.T. Polyphenol-Stabilized Tubular Elastin Scaffolds for Tissue Engineered Vascular Grafts. Tissue Eng. Part A 2009, 15, 2837–2851. [Google Scholar] [CrossRef]
- Raut, S.S.; Chandra, S.; Shum, J.; Washington, C.B.; Muluk, S.C.; Finol, E.A.; Rodriguez, J.F. Biological, Geometric and Biomechanical Factors Influencing Abdominal Aortic Aneurysm Rupture Risk: A Comprehensive Review. Recent Pat. Med. Imaging 2013, 3, 44–59. [Google Scholar] [CrossRef]
- Pennel, T.; Fercana, G.; Bezuidenhout, D.; Simionescu, A.; Chuang, T.-H.; Zilla, P.; Simionescu, D. The performance of cross-linked acellular arterial scaffolds as vascular grafts; pre-clinical testing in direct and isolation loop circulatory models. Biomaterials 2014, 35, 6311–6322. [Google Scholar] [CrossRef]
- Johnson, M.S. Periadventitial Drug Delivery for the Prevention of Restenosis: Rationale and Results. J. Vasc. Interv. Radiol. 2002, 13, P263–P265. [Google Scholar] [CrossRef]
- Chaudhary, M.A.; Guo, L.-W.; Shi, X.; Chen, G.; Gong, S.; Liu, B.; Kent, K.C. Periadventitial Drug Delivery for the Prevention of Intimal Hyperplasia Following Open Surgery. J. Control. Release 2016, 233, 174–180. [Google Scholar] [CrossRef]
- Goergen, C.J.; Johnson, B.L.; Greve, J.M.; Taylor, C.A.; Zarins, C.K. Increased Anterior Abdominal Aortic Wall Motion: Possible Role in Aneurysm Pathogenesis and Design of Endovascular Devices. J. Endovasc. Ther. 2007, 14, 574–584. [Google Scholar] [CrossRef] [PubMed]
- Goergen, C.J.; Li, H.-H.; Francke, U.; Taylor, C.A. Induced Chromosome Deletion in a Williams-Beuren Syndrome Mouse Model Causes Cardiovascular Abnormalities. J. Vasc. Res. 2011, 48, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Pyo, R.; Lee, J.K.; Shipley, J.M.; Curci, J.A.; Mao, D.; Ziporin, S.J.; Ennis, T.L.; Shapiro, S.D.; Senior, R.M.; Thompson, R.W. Targeted gene disruption of matrix metalloproteinase-9 (gelatinase B) suppresses development of experimental abdominal aortic aneurysms. J. Clin. Investig. 2000, 105, 1641–1649. [Google Scholar] [CrossRef]
- Ailawadi, G.; Eliason, J.L.; Roelofs, K.J.; Sinha, I.; Hannawa, K.K.; Kaldjian, E.P.; Lu, G.; Henke, P.K.; Stanley, J.C.; Weiss, S.J.; et al. Gender Differences in Experimental Aortic Aneurysm Formation. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 2116–2122. [Google Scholar] [CrossRef] [PubMed]
- Chiou, A.C.; Chiu, B.; Pearce, W.H. Murine Aortic Aneurysm Produced by Periarterial Application of Calcium Chloride. J. Surg. Res. 2001, 99, 371–376. [Google Scholar] [CrossRef]
- Yamanouchi, D.; Morgan, S.; Stair, C.; Seedial, S.; Lengfeld, J.; Kent, K.C.; Liu, B. Accelerated aneurysmal dilation associated with apoptosis and inflammation in a newly developed calcium phosphate rodent abdominal aortic aneurysm model. J. Vasc. Surg. 2012, 56, 455–461. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anderson, J.L.; Niedert, E.E.; Patnaik, S.S.; Tang, R.; Holloway, R.L.; Osteguin, V.; Finol, E.A.; Goergen, C.J. Animal Model Dependent Response to Pentagalloyl Glucose in Murine Abdominal Aortic Injury. J. Clin. Med. 2021, 10, 219. https://doi.org/10.3390/jcm10020219
Anderson JL, Niedert EE, Patnaik SS, Tang R, Holloway RL, Osteguin V, Finol EA, Goergen CJ. Animal Model Dependent Response to Pentagalloyl Glucose in Murine Abdominal Aortic Injury. Journal of Clinical Medicine. 2021; 10(2):219. https://doi.org/10.3390/jcm10020219
Chicago/Turabian StyleAnderson, Jennifer L., Elizabeth E. Niedert, Sourav S. Patnaik, Renxiang Tang, Riley L. Holloway, Vangelina Osteguin, Ender A. Finol, and Craig J. Goergen. 2021. "Animal Model Dependent Response to Pentagalloyl Glucose in Murine Abdominal Aortic Injury" Journal of Clinical Medicine 10, no. 2: 219. https://doi.org/10.3390/jcm10020219
APA StyleAnderson, J. L., Niedert, E. E., Patnaik, S. S., Tang, R., Holloway, R. L., Osteguin, V., Finol, E. A., & Goergen, C. J. (2021). Animal Model Dependent Response to Pentagalloyl Glucose in Murine Abdominal Aortic Injury. Journal of Clinical Medicine, 10(2), 219. https://doi.org/10.3390/jcm10020219






