A Retrospective Cohort Study of Clinical Factors Associated with Transitions of Care among COVID-19 Patients
Abstract
:1. Introduction
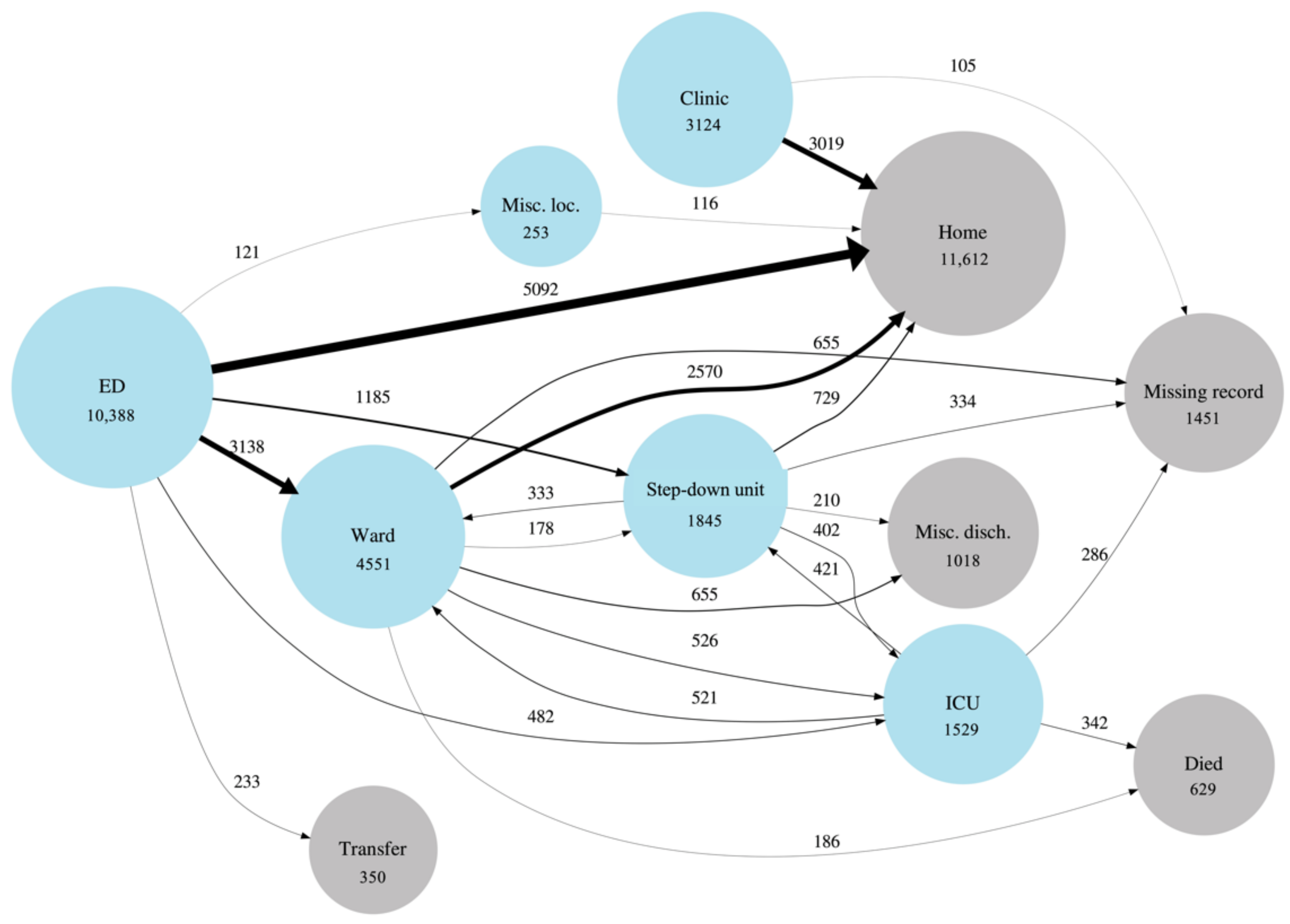
2. Materials and Methods
3. Results
3.1. Emergency Department (ED) Cohort
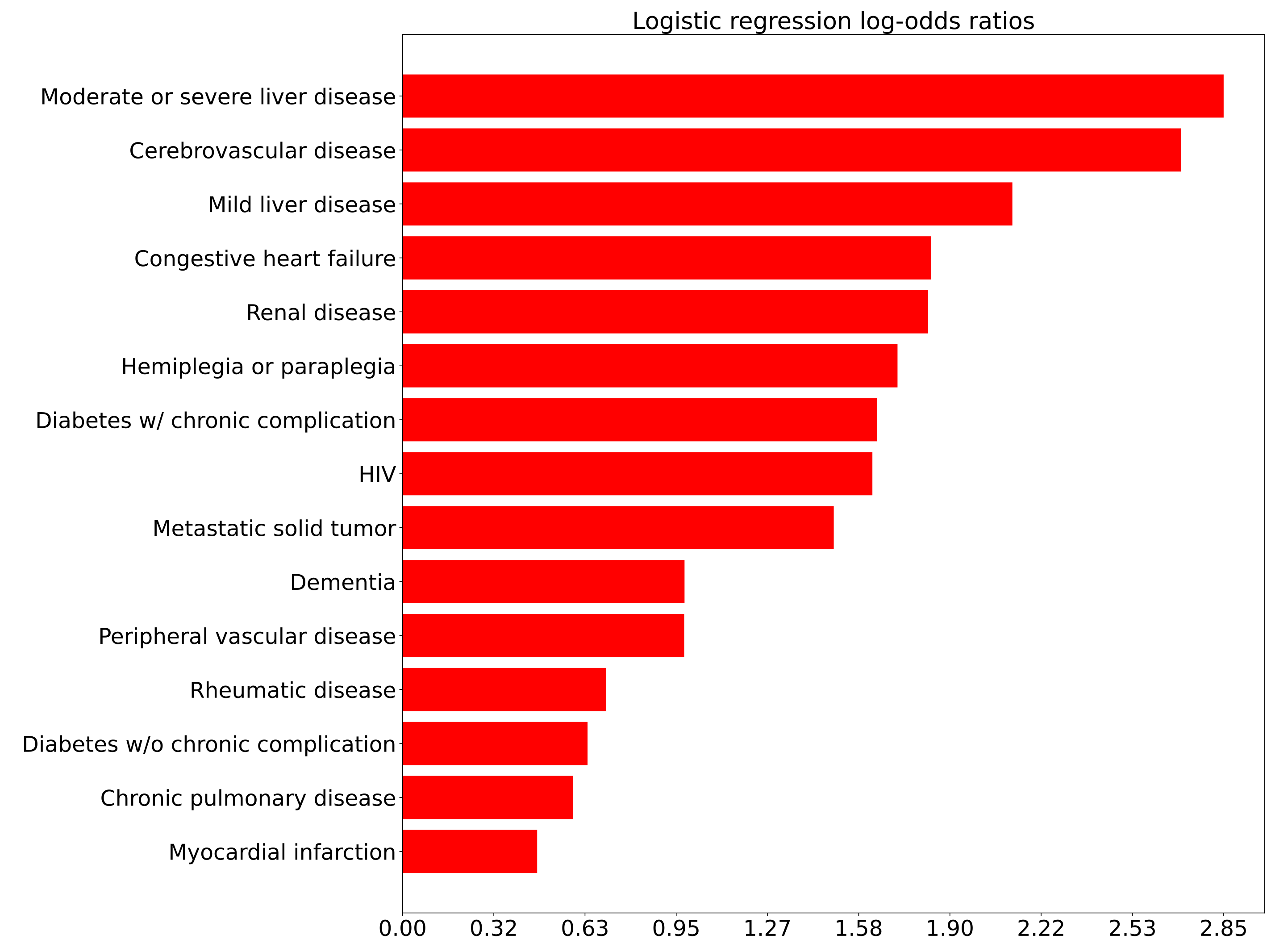
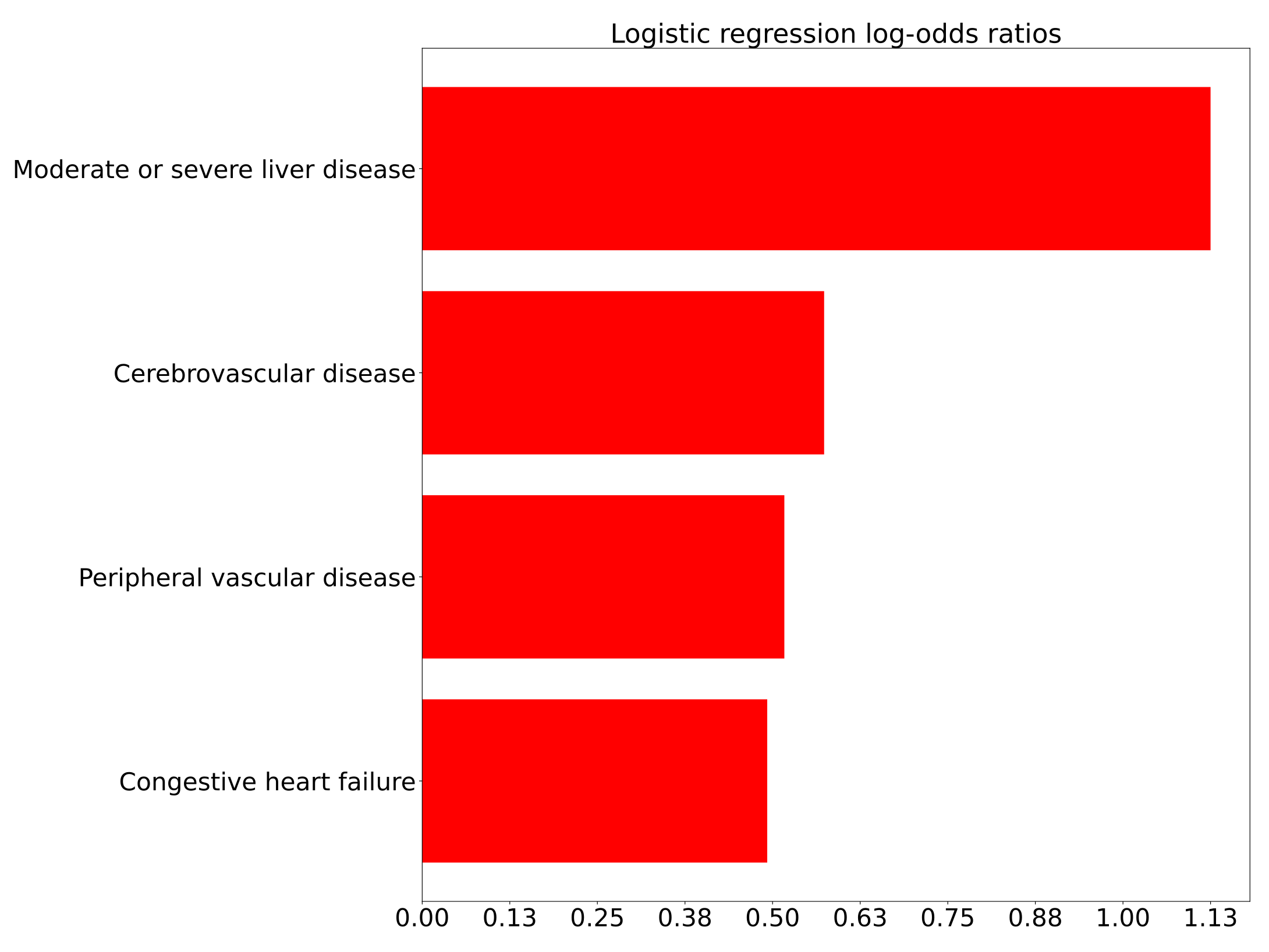
3.1.1. Comorbidities and ED Transitions
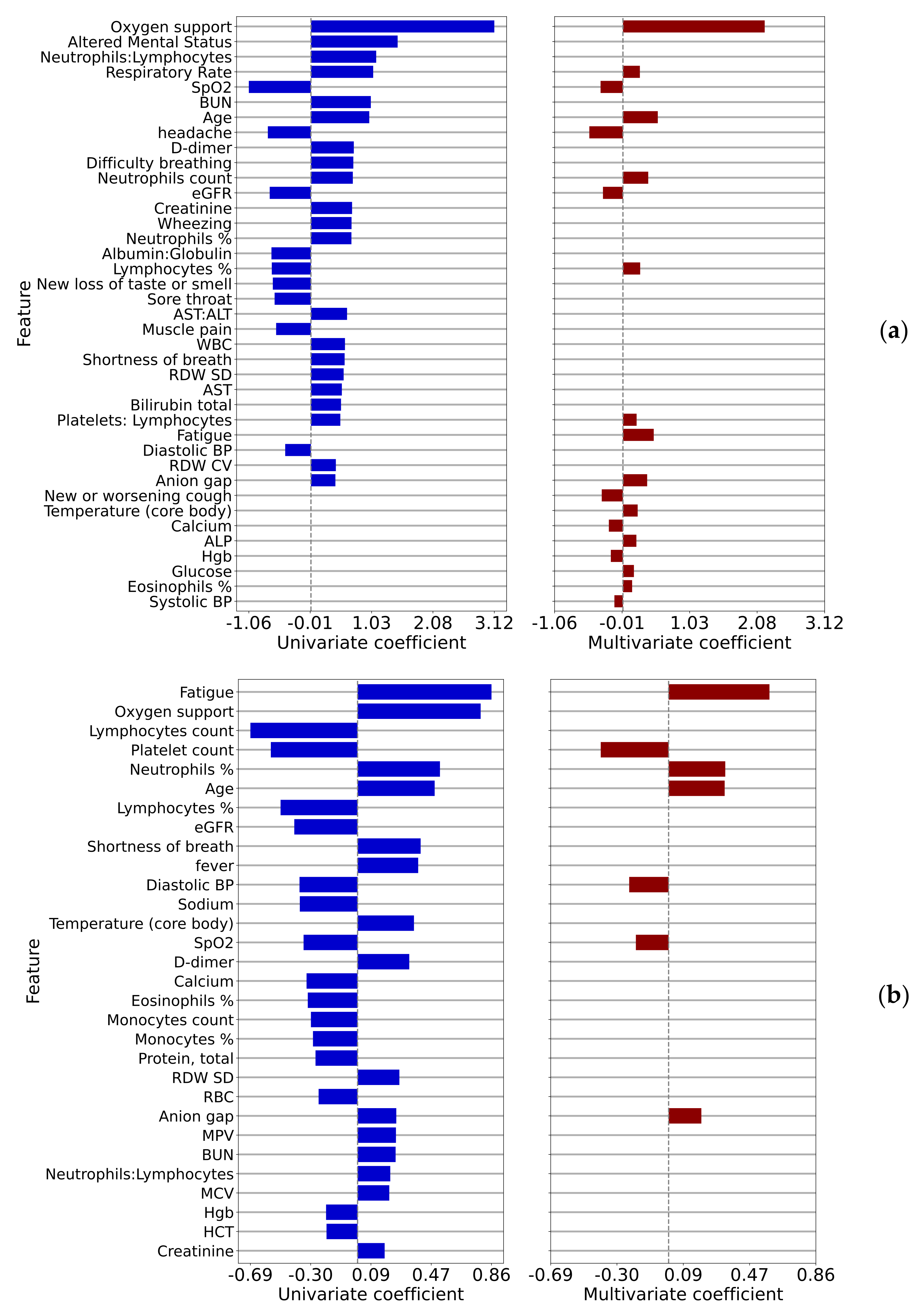
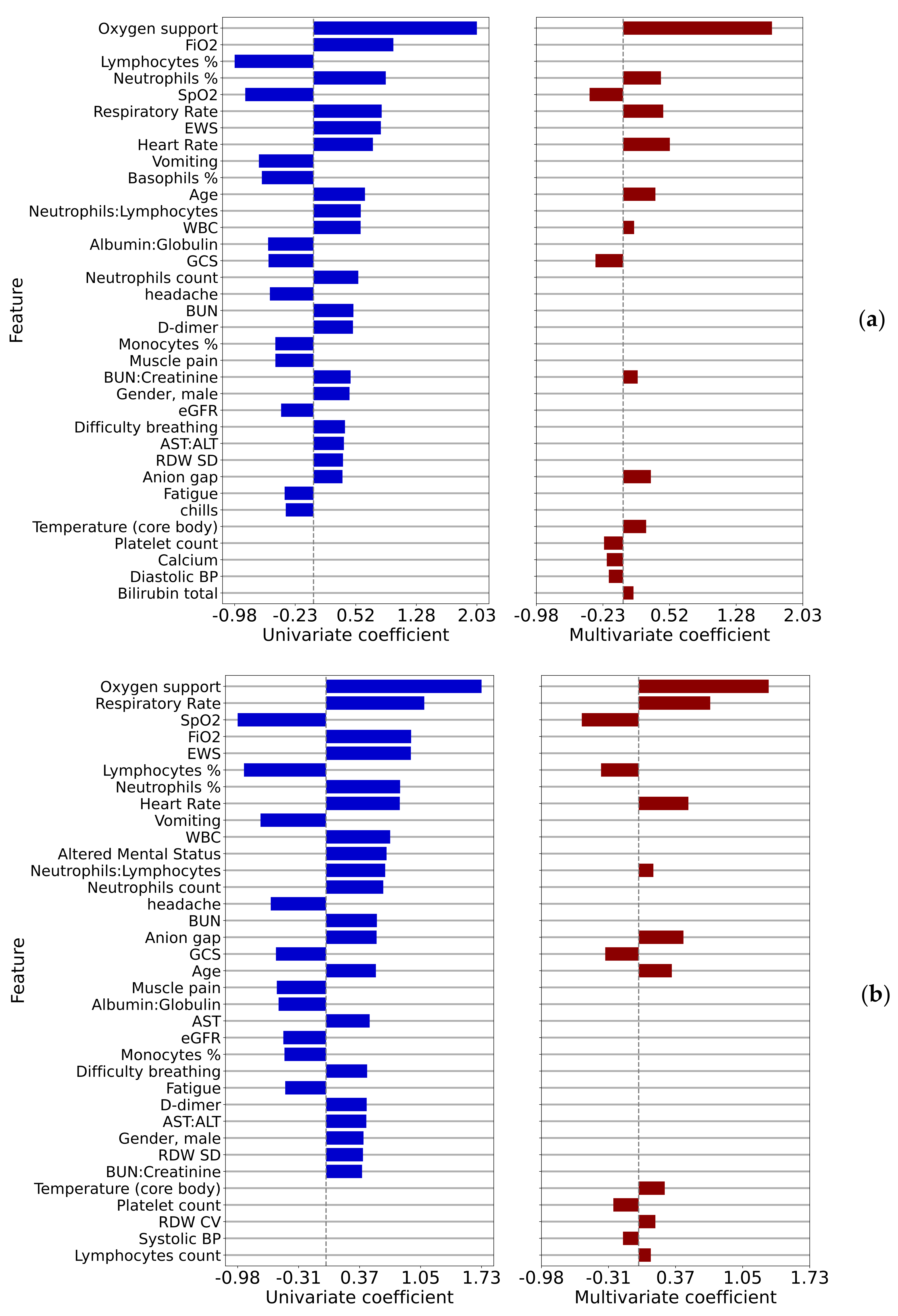
3.1.2. Correlates of Vital Signs, Symptoms, and Laboratory Results to ED Transitions
3.2. Non-Critical Inpatient Cohort
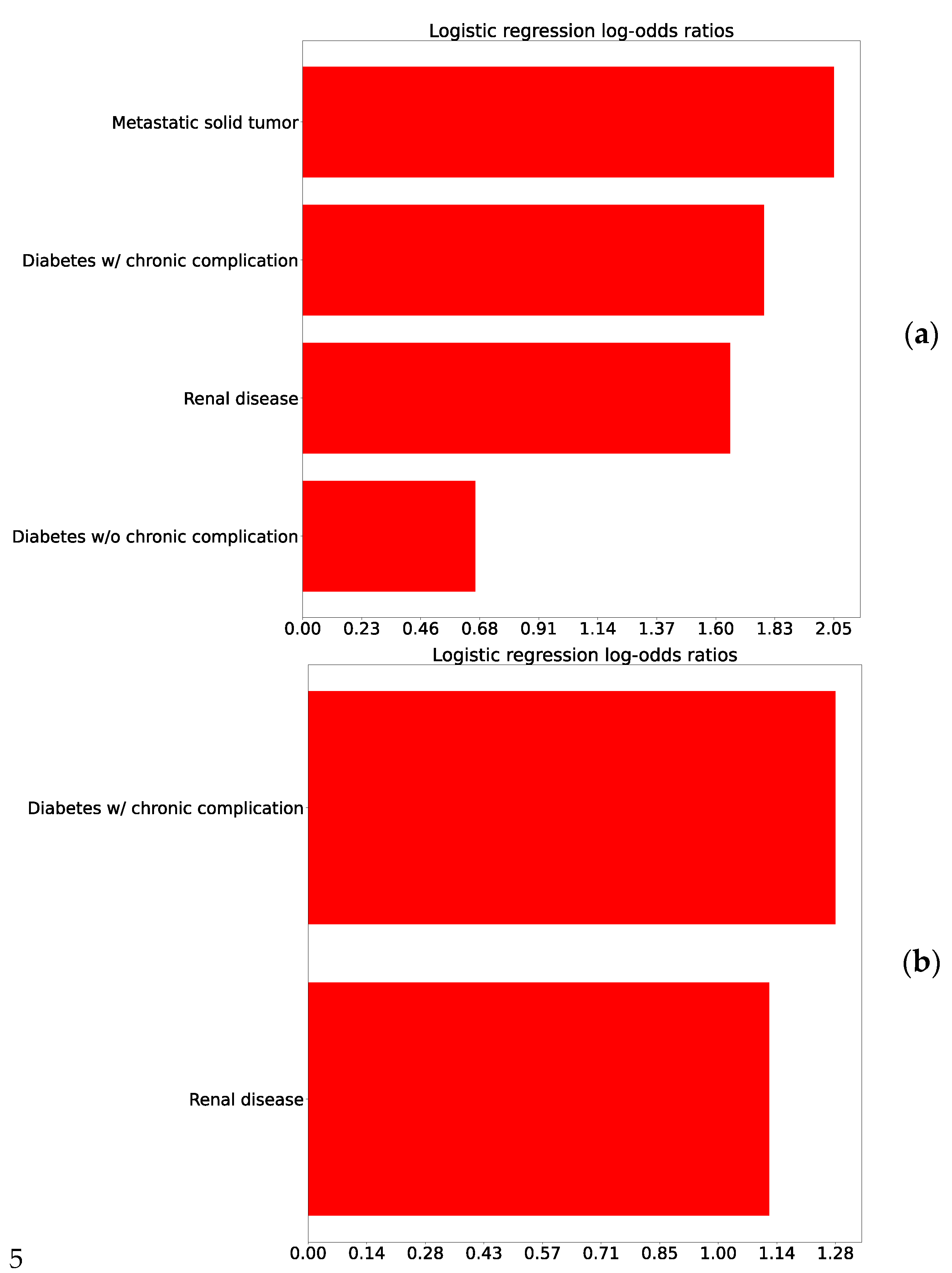
3.2.1. Correlations of Comorbidities with Inpatient Deterioration
3.2.2. Correlations of Symptoms, Vital Signs, and Laboratory Results with Inpatient Deterioration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Feature | Overall | Discharged to Home and Not Admitted within 72 h (A) | Discharged to Home and Admitted within 72 h (B) | Admitted within Same Encounter (C) | Admitted within 72 h (B&C) | Comparison 1 | Comparison 2 | |
|---|---|---|---|---|---|---|---|---|
| (A vs. B&C) | (A vs. B) | |||||||
| p-Value | p-Value | |||||||
| n | 10,079 | 4907 | 157 | 5015 | 5172 | |||
| Age (years), mean (SD) | 51.6 (19.5) | 42.4 (16.9) | 53.7 (17.2) | 60.5 (17.6) | 60.3 (17.6) | <0.001 | <0.001 | |
| Race, n (%) | American Indian or Alaska Native | 392 (4.6) | 185 (4.5) | † | † | 207 (4.6) | 0.15 | 0.961 |
| Black or African American | 606 (7.0) | 304 (7.5) | 302 (6.7) | |||||
| Other | 922 (10.7) | 460 (11.3) | 462 (10.2) | |||||
| White | 6692 (77.7) | 3128 (76.7) | 3564 (78.6) | |||||
| Missing | 1467 (-) | - | - | |||||
| Ethnicity, n (%) | Hispanic or Latino | 4623 (49.0) | 2526 (55.2) | † | † | 2097 (43.1) | < 0.001 | 0.114 |
| Not Hispanic or Latino | 4816 (51.0) | 2051 (44.8) | 2765 (56.9) | |||||
| Missing | 640 (-) | - | - | |||||
| Sex, n (%) | Female | 5359 (53.2) | 2797 (57.0) | † | † | 2562 (49.5) | < 0.001 | 0.206 |
| Male | 4719 (46.8) | 2110 (43.0) | 2609 (50.5) | |||||
| Missing | 1 (-) | - | - | |||||
| ED length of stay (h), mean (SD) | 7.3 (21.4) | 3.9 (6.4) | 4.9 (5.0) | 10.6 (29.1) | 10.5 (28.7) | < 0.001 | 0.023 | |
| Mortality, n (%) | -NA- | 11 (7.0) | 446 (8.9) | 457 (8.8) | ||||
| ICU admit, n (%) | -NA- | 27 (17.2) | 1081 (21.6) | 1108 (21.4) | ||||
| Hospital Length of Stay (h), mean (SD) | -NA- | 179.4 (152.0) | 157.5 (146.9) | 158.3 (147.1) |
| Feature | Overall | Admitted to ICU or Died in Hospital (E) | Not Admitted to ICU or Died in Hospital (D) | Comparison 3 (D vs. E)p-Value | |
|---|---|---|---|---|---|
| n | 4766 | 970 | 3796 | ||
| Age (years), mean (SD) | 59.8 (18.5) | 66.5 (18.3) | 58.1 (18.2) | <0.001 | |
| Race, n (%) | American Indian or Alaska Native | 261 (6.3) | 42 (5.0) | 219 (6.6) | 0.117 |
| Black or African American | 267 (6.4) | 44 (5.2) | 223 (6.7) | ||
| Other | 419 (10.0) | 86 (10.2) | 333 (10.0) | ||
| White | 3228 (77.3) | 673 (79.6) | 2555 (76.7) | ||
| Missing | 591 (-) | ||||
| Ethnicity, n (%) | Hispanic or Latino | 1792 (40.2) | 324 (35.9) | 1468 (41.3) | 0.004 |
| Not Hispanic or Latino | 2669 (59.8) | 579 (64.1) | 2090 (58.7) | ||
| Missing | 305 (-) | ||||
| Sex, n (%) | Female | 2456 (51.5) | 420 (43.3) | 2036 (53.6) | <0.001 |
| Male | 2310 (48.5) | 550 (56.7) | 1760 (46.4) | ||
| Missing | 0 (-) |
Appendix B
Appendix C
| Feature | Coefficient | p-Value |
|---|---|---|
| Oxygen support | 2.19 | <0.001 |
| Age | 0.54 | <0.001 |
| headache | −0.52 | <0.001 |
| Fatigue | 0.58 | <0.001 |
| Neutrophils count | 0.39 | <0.001 |
| Anion gap | 0.38 | <0.001 |
| SpO2 | −0.35 | <0.001 |
| New or worsening cough | −0.33 | <0.001 |
| eGFR | −0.31 | <0.001 |
| Lymphocytes % | 0.27 | <0.001 |
| Respiratory Rate | 0.26 | <0.001 |
| Temperature (core body) | 0.23 | <0.001 |
| Calcium | −0.22 | <0.001 |
| Platelets: Lymphocytes | 0.21 | <0.001 |
| ALP | 0.21 | <0.001 |
| Hgb | −0.19 | <0.001 |
| Glucose | 0.17 | <0.001 |
| Eosinophils % | 0.14 | <0.001 |
| Systolic BP | −0.13 | <0.001 |
| Feature | Coefficient | p-Value |
|---|---|---|
| Fatigue | 0.59 | 0.008 |
| Platelet count | −0.39 | <0.001 |
| Neutrophils % | 0.33 | <0.001 |
| Age | 0.33 | <0.001 |
| Diastolic BP | −0.23 | 0.009 |
| Anion gap | 0.19 | 0.006 |
| SpO2 | −0.19 | 0.003 |
Appendix D
| Feature | Coefficient | p-Value |
|---|---|---|
| Oxygen support | 1.68 | <0.001 |
| Heart Rate | 0.53 | <0.001 |
| Respiratory Rate | 0.45 | <0.001 |
| Neutrophils % | 0.43 | <0.001 |
| SpO2 | −0.38 | <0.001 |
| Age | 0.36 | <0.001 |
| Anion gap | 0.31 | <0.001 |
| GCS | −0.31 | <0.001 |
| Temperature (core body) | 0.26 | <0.001 |
| Platelet count | −0.22 | <0.001 |
| Calcium | −0.18 | 0.001 |
| BUN:Creatinine | 0.16 | 0.004 |
| Diastolic BP | −0.16 | 0.004 |
| RDW SD | 0.13 | 0.01 |
| WBC | 0.12 | <0.01 |
| Bilirubin total | 0.12 | 0.004 |
| Feature | Coefficient | p-Value |
|---|---|---|
| Oxygen support | 1.31 | <0.001 |
| Respiratory Rate | 0.72 | <0.001 |
| SpO2 | −0.58 | <0.001 |
| Heart Rate | 0.50 | <0.001 |
| Anion gap | 0.45 | <0.001 |
| Lymphocytes % | −0.38 | <0.001 |
| GCS | −0.34 | <0.001 |
| Age | 0.34 | <0.001 |
| Temperature (core body) | 0.26 | <0.001 |
| Platelet count | −0.26 | <0.001 |
| RDW CV | 0.17 | <0.001 |
| Systolic BP | −0.16 | 0.002 |
| Neutrophils:Lymphocytes | 0.15 | 0.006 |
| Lymphocytes count | 0.12 | 0.006 |
| Feature | Rank Comparison 1 | Rank Comparison 2 | Rank Comparison 3: 12 h | Rank Comparison 3: 4 h | Number of Models |
|---|---|---|---|---|---|
| SpO2 | 7 | 7 | 5 | 3 | 4 |
| Age | 2 | 4 | 6 | 8 | 4 |
| Anion gap | 6 | 6 | 7 | 5 | 4 |
| Oxygen support | 1 | 1 | 1 | 3 | |
| Platelet count | 2 | 10 | 10 | 3 | |
| Temperature (core body) | 12 | 9 | 9 | 3 | |
| Respiratory Rate | 11 | 3 | 2 | 3 | |
| Lymphocytes % | 10 | 6 | 2 | ||
| Diastolic BP | 5 | 13 | 2 | ||
| Calcium | 13 | 11 | 2 | ||
| Fatigue | 4 | 1 | 2 | ||
| GCS | 8 | 7 | 2 | ||
| Heart Rate | 2 | 4 | 2 | ||
| Systolic BP | 19 | 12 | 2 | ||
| Neutrophils % | 3 | 4 | 2 | ||
| Bilirubin total | 16 | 1 | |||
| WBC | 15 | 1 | |||
| RDW CV | 11 | 1 | |||
| RDW SD | 14 | 1 | |||
| BUN:Creatinine | 12 | 1 | |||
| Neutrophils:Lymphocytes | 13 | 1 | |||
| Hgb | 16 | 1 | |||
| Eosinophils % | 18 | 1 | |||
| Glucose | 17 | 1 | |||
| ALP | 15 | 1 | |||
| Platelets: Lymphocytes | 14 | 1 | |||
| eGFR | 9 | 1 | |||
| New or worsening cough | 8 | 1 | |||
| Neutrophils count | 5 | 1 | |||
| headache | 3 | 1 | |||
| Lymphocytes count | 14 | 1 |
References
- WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 22 June 2021).
- Chavez, S.; Long, B.; Koyfman, A.; Liang, S.Y. Coronavirus Disease (COVID-19): A Primer for Emergency Physicians. Am. J. Emerg. Med. 2020, 44, 220–229. [Google Scholar] [CrossRef]
- Whiteside, T.; Kane, E.; Aljohani, B.; Alsamman, M.; Pourmand, A. Redesigning Emergency Department Operations amidst a Viral Pandemic. Am. J. Emerg. Med. 2020, 38, 1448–1453. [Google Scholar] [CrossRef]
- Kleinpell, R.; Ferraro, D.M.; Maves, R.C.; Gill, S.L.K.; Branson, R.; Greenberg, S.; Doersam, J.K.; Raman, R.; Kaplan, L.J. Coronavirus Disease 2019 Pandemic Measures: Reports From a National Survey of 9,120 ICU Clinicians. Crit Care Med. 2020, 48, e846–e855. [Google Scholar] [CrossRef]
- Sprung, C.L.; Zimmerman, J.L.; Christian, M.D.; Joynt, G.M.; Hick, J.L.; Taylor, B.; Richards, G.A.; Sandrock, C.; Cohen, R.; Adini, B. Recommendations for Intensive Care Unit and Hospital Preparations for an Influenza Epidemic or Mass Disaster: Summary Report of the European Society of Intensive Care Medicine’s Task Force for Intensive Care Unit Triage during an Influenza Epidemic or Mass Disaster. Intensive Care Med. 2010, 36, 428–443. [Google Scholar] [CrossRef]
- Sprung, C.L.; Joynt, G.M.; Christian, M.D.; Truog, R.D.; Rello, J.; Nates, J.L. Adult ICU Triage During the Coronavirus Disease 2019 Pandemic: Who Will Live and Who Will Die? Recommendations to Improve Survival*. Crit Care Med. 2020, 48, 1196–1202. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical Course and Risk Factors for Mortality of Adult Inpatients with COVID-19 in Wuhan, China: A Retrospective Cohort Study. The Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef] [Green Version]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Consortium and the NC.-19 R.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef]
- Pollard, T.J.; Johnson, A.E.W.; Raffa, J.D.; Mark, R.G. Tableone: An Open Source Python Package for Producing Summary Statistics for Research Papers. JAMIA Open 2018, 1, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Van Rossum, G.; Drake, F.L. Python 3 Reference Manual; CreateSpace: Scotts Valley, CA, USA, 2009. [Google Scholar]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data from 6 Countries. Am. J. Epidemio. 2011, 173, 676–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Calmes, D.; Graff, S.; Maes, N.; Frix, A.-N.; Thys, M.; Bonhomme, O.; Berg, J.; Debruche, M.; Gester, F.; Henket, M.; et al. Asthma and COPD Are Not Risk Factors for ICU Stay and Death in Case of SARS-CoV2 Infection. J. Allergy Clin. Immunol. Pract. 2021, 9, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Sabatino, J.; Rosa, S.D.; Salvo, G.D.; Indolfi, C. Impact of Cardiovascular Risk Profile on COVID-19 Outcome. A Meta-Analysis. PLoS ONE 2020, 15, e0237131. [Google Scholar] [CrossRef]
- Velavan, T.P.; Meyer, C.G. Mild versus Severe COVID-19: Laboratory Markers. Int J. Infect. Dis 2020, 95, 304–307. [Google Scholar] [CrossRef]
- Zhang, L.; Yan, X.; Fan, Q.; Liu, H.; Liu, X.; Liu, Z.; Zhang, Z. D-Dimer Levels on Admission to Predict in-Hospital Mortality in Patients with Covid-19. J. Thromb Haemost 2020, 18, 1324–1329. [Google Scholar] [CrossRef]
- Yao, Y.; Cao, J.; Wang, Q.; Shi, Q.; Liu, K.; Luo, Z.; Chen, X.; Chen, S.; Yu, K.; Huang, Z.; et al. D-Dimer as a Biomarker for Disease Severity and Mortality in COVID-19 Patients: A Case Control Study. J. Intensive Care 2020, 8, 49. [Google Scholar] [CrossRef]
- Yu, H.-H.; Qin, C.; Chen, M.; Wang, W.; Tian, D.-S. D-Dimer Level Is Associated with the Severity of COVID-19. Thromb Res. 2020, 195, 219–225. [Google Scholar] [CrossRef]
- Foy, B.H.; Carlson, J.C.T.; Reinertsen, E.; Padros, I.; Valls, R.; Pallares Lopez, R.; Palanques-Tost, E.; Mow, C.; Westover, M.B.; Aguirre, A.D.; et al. Association of Red Blood Cell Distribution Width With Mortality Risk in Hospitalized Adults With SARS-CoV-2 Infection. JAMA Netw. Open 2020, 3, e2022058. [Google Scholar] [CrossRef]
- Lorente, L.; Martín, M.M.; Argueso, M.; Solé-Violán, J.; Perez, A.; Marcos, Y.; Ramos, J.A.; Ramos-Gómez, L.; López, S.; Franco, A.; et al. Association between Red Blood Cell Distribution Width and Mortality of COVID-19 Patients. Anaesth. Crit. Care Pain Med. 2020, 40, 100777. [Google Scholar] [CrossRef]
- Karampitsakos, T.; Akinosoglou, K.; Papaioannou, O.; Panou, V.; Koromilias, A.; Bakakos, P.; Loukides, S.; Bouros, D.; Gogos, C.; Tzouvelekis, A. Increased Red Cell Distribution Width Is Associated With Disease Severity in Hospitalized Adults With SARS-CoV-2 Infection: An Observational Multicentric Study. Front. Med. 2020, 7. [Google Scholar] [CrossRef] [PubMed]
- Bloom, P.P.; Meyerowitz, E.A.; Reinus, Z.; Daidone, M.; Gustafson, J.; Kim, A.Y.; Schaefer, E.; Chung, R.T. Liver Biochemistries in Hospitalized Patients With COVID-19. Hepatology 2021, 73, 890–900. [Google Scholar] [CrossRef] [PubMed]
- Razavian, N.; Major, V.J.; Sudarshan, M.; Burk-Rafel, J.; Stella, P.; Randhawa, H.; Bilaloglu, S.; Chen, J.; Nguy, V.; Wang, W.; et al. A Validated, Real-Time Prediction Model for Favorable Outcomes in Hospitalized COVID-19 Patients. NPJ Digit. Med. 2020, 3, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Carlino, M.V.; Valenti, N.; Cesaro, F.; Costanzo, A.; Cristiano, G.; Guarino, M.; Sforza, A. Predictors of Intensive Care Unit Admission in Patients with Coronavirus Disease 2019 (COVID-19). Monaldi Arch. Chest Dis. 2020, 90. [Google Scholar] [CrossRef] [PubMed]
- Tavakolpour, S.; Rakhshandehroo, T.; Wei, E.X.; Rashidian, M. Lymphopenia during the COVID-19 Infection: What It Shows and What Can Be Learned. Immunol. Lett. 2020, 225, 31–32. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Dong, L.; Cai, W. Predictive Value of Neutrophil to Lymphocyte and Platelet to Lymphocyte Ratio in COVID-19. Critical Care 2020, 24, 532. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Davis, P.B.; Gurney, M.E.; Xu, R. COVID-19 and Dementia: Analyses of Risk, Disparity, and Outcomes from Electronic Health Records in the US. Alzheimer’s Dement. 2021, 17, 1297–1306. [Google Scholar] [CrossRef]

| Cohort ID | Description | Endpoint |
|---|---|---|
| A | ED patients discharged to home and not admitted as inpatient within 72 h | 72 h after ED discharge |
| B | ED patients discharged to home and admitted as inpatient within 72 h | 72 h after ED discharge |
| C | ED patients admitted to hospital in same encounter | Hospital admit |
| D | Inpatients who do not go to ICU or die in-hospital | Hospital discharge |
| E | Inpatients who deteriorated (admitted to ICU or died in-hospital) | Deterioration |
| Comparison. ID and Label | Cohorts Compared | Long Description | Values Used for Non-Categorical Data |
|---|---|---|---|
| 1 “ED admission” | A | ED patients discharged to home and not admitted as inpatient within 72 h | Last value during ED stay |
| B & C | ED patients who were admitted to the hospital within 72 h | ||
| 2 “ED bounce-back” | A | ED patients discharged to home and not admitted as inpatient within 72 h | Last value during ED stay |
| B | ED patients discharged to home and admitted as inpatient within 72 h | ||
| 3 “Inpatient deterioration” | D | Inpatients who do not go to ICU or die in-hospital | Most recent value measured at midpoint of hospital stay |
| E | Inpatients who deteriorate (admitted to ICU or die in-hospital) | Most recent value measured X hours prior to deterioration (X = 4, 12) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Swearingen, D.; Boverman, G.; Tgavalekos, K.; Noren, D.P.; Ravindranath, S.; Ghosh, E.; Xu, M.; Wondrely, L.; Thompson, P.; Cowden, J.D.; et al. A Retrospective Cohort Study of Clinical Factors Associated with Transitions of Care among COVID-19 Patients. J. Clin. Med. 2021, 10, 4605. https://doi.org/10.3390/jcm10194605
Swearingen D, Boverman G, Tgavalekos K, Noren DP, Ravindranath S, Ghosh E, Xu M, Wondrely L, Thompson P, Cowden JD, et al. A Retrospective Cohort Study of Clinical Factors Associated with Transitions of Care among COVID-19 Patients. Journal of Clinical Medicine. 2021; 10(19):4605. https://doi.org/10.3390/jcm10194605
Chicago/Turabian StyleSwearingen, Dennis, Gregory Boverman, Kristen Tgavalekos, David P. Noren, Shreyas Ravindranath, Erina Ghosh, Minnan Xu, Lisa Wondrely, Pam Thompson, J. David Cowden, and et al. 2021. "A Retrospective Cohort Study of Clinical Factors Associated with Transitions of Care among COVID-19 Patients" Journal of Clinical Medicine 10, no. 19: 4605. https://doi.org/10.3390/jcm10194605
APA StyleSwearingen, D., Boverman, G., Tgavalekos, K., Noren, D. P., Ravindranath, S., Ghosh, E., Xu, M., Wondrely, L., Thompson, P., Cowden, J. D., & Antonescu, C. (2021). A Retrospective Cohort Study of Clinical Factors Associated with Transitions of Care among COVID-19 Patients. Journal of Clinical Medicine, 10(19), 4605. https://doi.org/10.3390/jcm10194605






