Challenges Related to Surgical Site Infection Prevention—Results after Standardized Bundle Implementation
Abstract
:1. Introduction
2. Methods
2.1. Patients and Data Management
2.2. Intervention
2.3. Outcomes/Study Endpoints
2.4. Impact of Covid 19 Pandemic
2.5. Statistical Analysis
3. Results
3.1. Patients
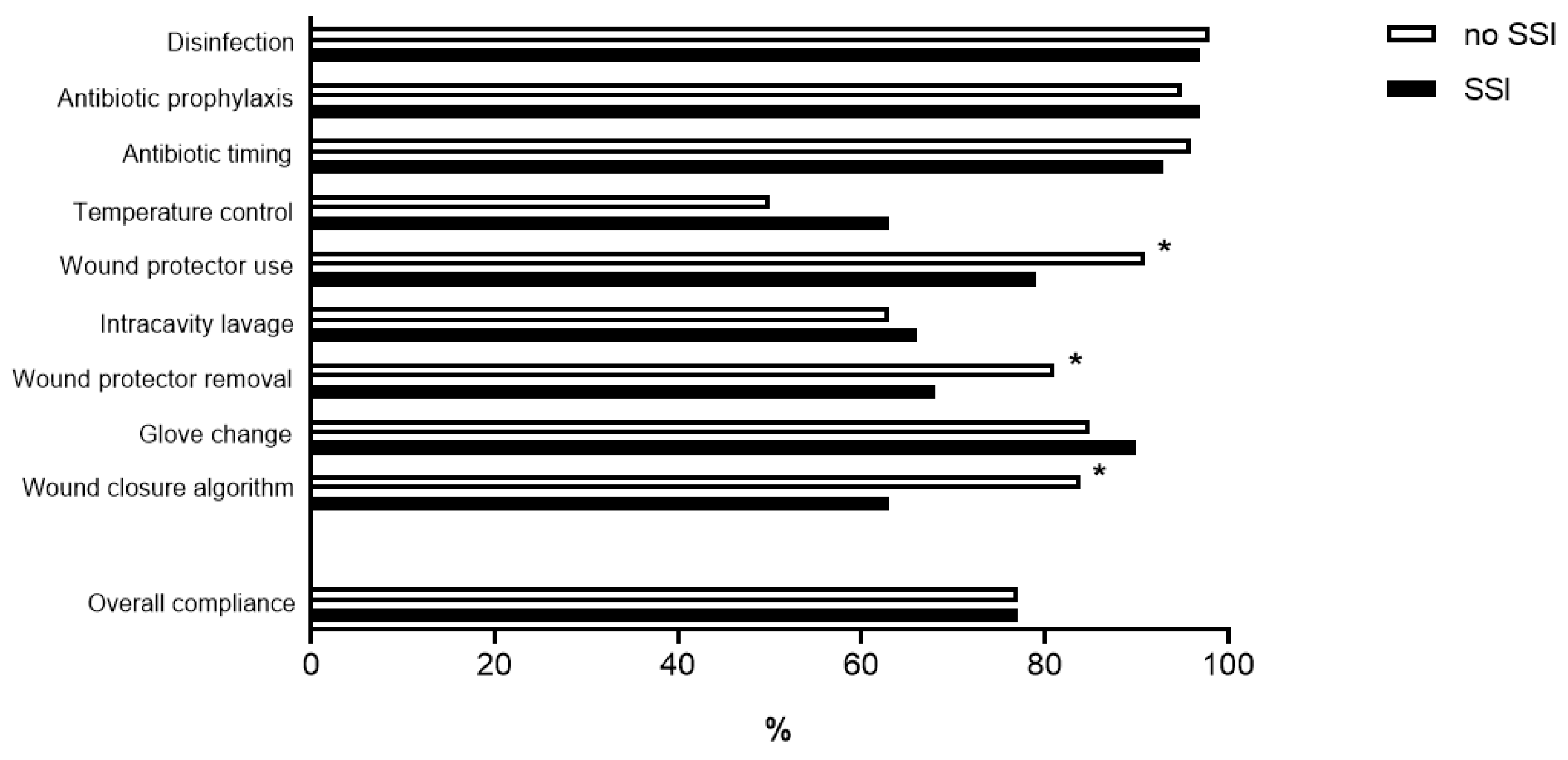
3.2. Compliance with Care Bundle
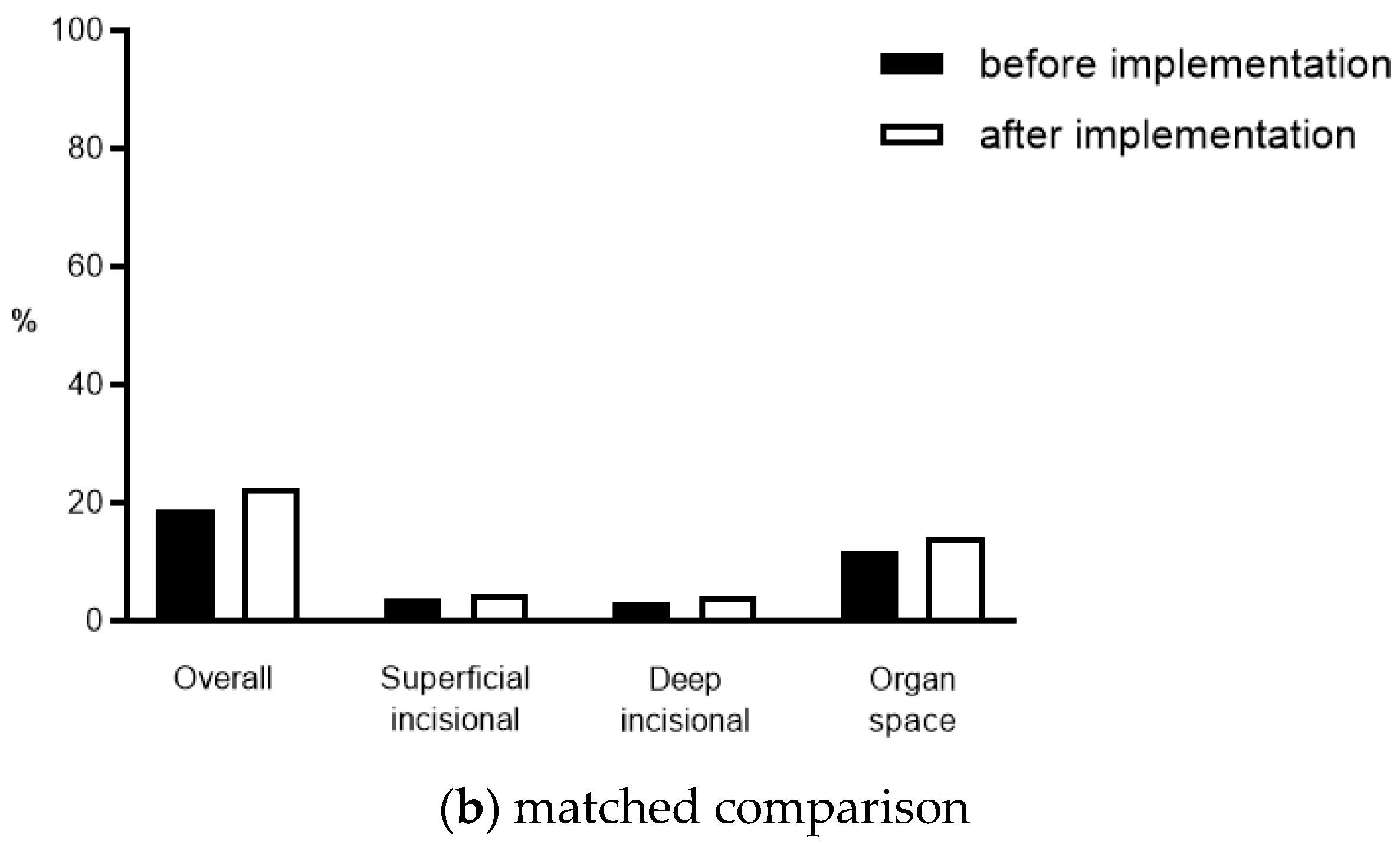
3.3. SSIs
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
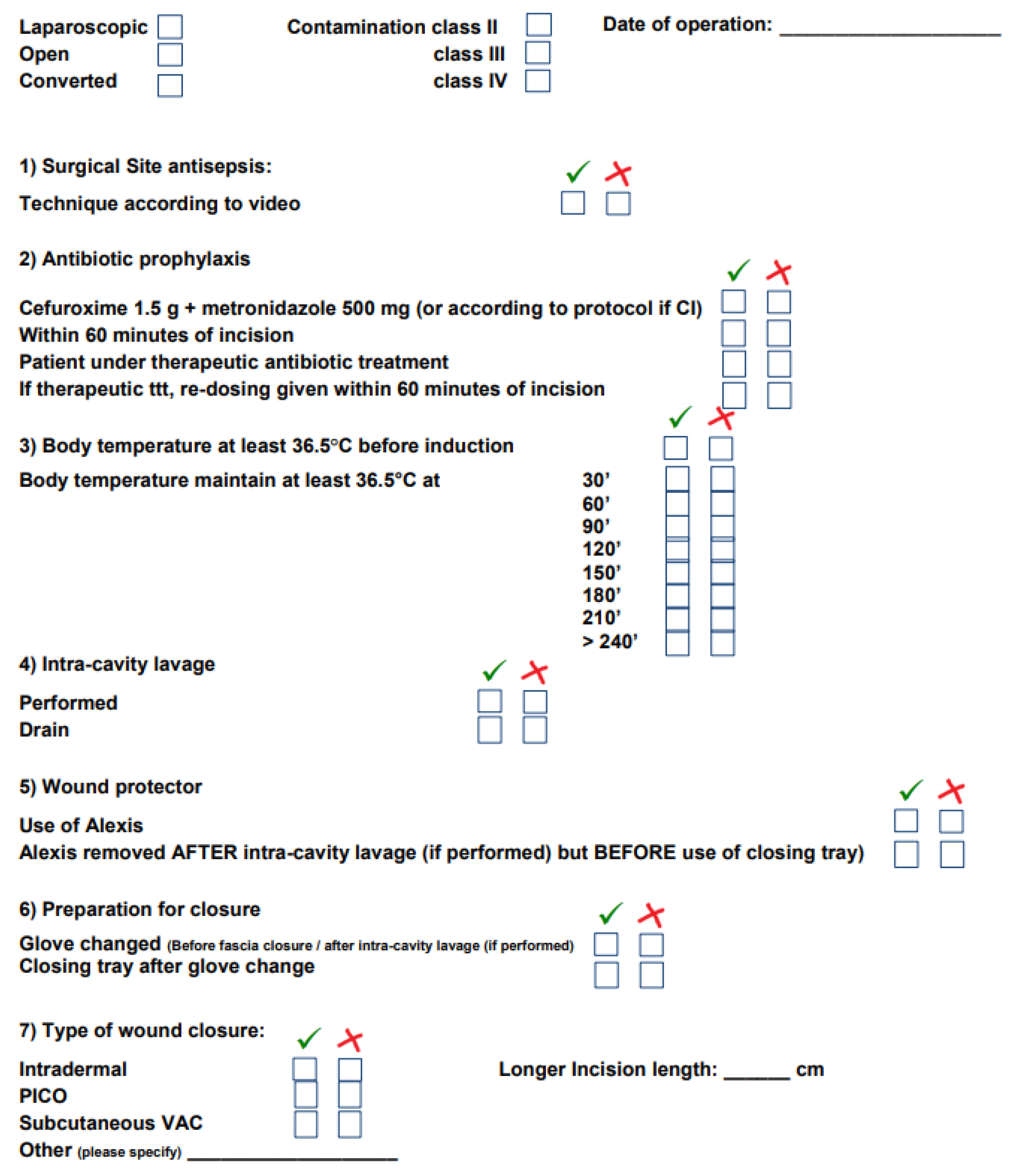
Appendix A. Core Measures
| (1) Disinfection | Chlorhexidine WAIT UNTIL DRY! |
| (2) Antibiotic prophylaxis | Cefuroxime 1.5 g + metronidazole 500 mg (or according to protocol if contra-indication) Within 60 min of incision (upon start of anesthesia) Preexisting antibiotic treatment: Redosing within 60 min of incision |
| (3) Prevent hypothermia | Maintain body temperature of at least 36.5 °C (documented every 30 min) using a forced-air warming device Induction of anesthesia should not begin unless the patient’s temperature is >36 °C (unless clinical urgency) Ambient temperature of at least 21 °C Intravenous fluids and blood products warmed to 37 °C Irrigation fluids should be warmed to 38–40 °C |
| (4) Wound protection | Systematic use of wound protector (Alexis) Remove Alexis after intra-cavity lavage (if performed) but BEFORE use of closing tray |
| (5) Intracavity lavage | Not routinely (no dilution of host defense) Lavage only in contaminated areas (i.e., pelvis), consider use of gauze instead If complete lavage performed (III–IV): use saline leave drain until patient mobilized for 24 h or consider 2nd look (algorithm staged procedure) |
| (6) Use of closing tray | Before fascia closure/after intra-cavity lavage (if performed): GLOVE CHANGE Systematic reminder by scrub nurse |
| (7) Appropriate closure strategy (see Appendix B) | |
Appendix B. Wound Closure Strategy

Appendix C. Checklist
References
- National Collaborating Centre for Women’s and Children’s Health (UK). Surgical Site Infection: Prevention and Treatment of Surgical Site Infection; National Institute for Health and Clinical Excellence: Guidance: London, UK, 2008. [Google Scholar]
- Murphy, P.B.; Knowles, S.; Chadi, S.A.; Vogt, K.; Brackstone, M.; Koughnett, J.A.V.; Ott, M.C. Negative Pressure Wound Therapy Use to Decrease Surgical Nosocomial Events in Colorectal Resections (NEPTUNE): A Randomized Controlled Trial. Ann. Surg. 2019, 270, 38–42. [Google Scholar] [CrossRef]
- Weber, W.P.; Zwahlen, M.; Reck, S.; Feder-Mengus, C.; Misteli, H.; Rosenthal, R.; Brandenberger, D.; Oertli, D.; Widmer, A.F.; Marti, W.R. Economic burden of surgical site infections at a European university hospital. Infect. Control. Hosp. Epidemiol. 2008, 29, 623–629. [Google Scholar] [CrossRef] [Green Version]
- Berríos-Torres, S.I.; Umscheid, C.A.; Bratzler, D.; Leas, B.; Stone, E.C.; Kelz, R.R.; Reinke, C.E.; Morgan, S.; Solomkin, J.; Mazuski, J.E.; et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017, 152, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.J.; Podgorny, K.; Berrios-Torres, S.I.; Bratzler, D.W.; Dellinger, E.P.; Greene, L.; Nyquist, A.-C.; Saiman, L.; Yokoe, D.S.; Maragakis, L.L.; et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect. Control. Hosp. Epidemiol. 2014, 35, 605–627. [Google Scholar] [CrossRef] [Green Version]
- Tanner, J.; Padley, W.; Assadian, O.; Leaper, D.; Kiernan, M.; Edmiston, C. Do surgical care bundles reduce the risk of surgical site infections in patients undergoing colorectal surgery? A systematic review and cohort meta-analysis of 8515 patients. Surgery 2015, 158, 66–77. [Google Scholar] [CrossRef]
- Leaper, D.J.; Tanner, J.; Kiernan, M.; Assadian, O.; Edmiston, C.E., Jr. Surgical site infection: Poor compliance with guidelines and care bundles. Int. Wound J. 2014, 12, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Leaper, D.; Burman-Roy, S.; Palanca, A.; Cullen, K.; Worster, D.; Gautam-Aitken, E.; Whittle, M.; Group, G.D. Prevention and treatment of surgical site infection: Summary of NICE guidance. BMJ 2008, 337, a1924. [Google Scholar] [CrossRef] [PubMed]
- Diana, M.; Hübner, M.; Eisenring, M.-C.; Zanetti, G.; Troillet, N.; Demartines, N. Measures to Prevent Surgical Site Infections: What Surgeons (Should) Do. World J. Surg. 2010, 35, 280–288. [Google Scholar] [CrossRef] [Green Version]
- Martin, D.; Hubner, M.; Moulin, E.; Pache, B.; Clerc, D.; Hahnloser, D.; Demartines, D.; Grass, F. Timing, diagnosis, and treatment of surgical site infections after colonic surgery: Prospective surveillance of 1263 patients. J. Hosp. Infect. 2018, 100, 393–399. [Google Scholar] [CrossRef]
- Gustafsson, U.O.; Scott, M.J.; Schwenk, W.; Demartines, N.; Roulin, D.; Francis, N.; McNaught, C.E.; Macfie, J.; Liberman, A.S.; Soop, M.; et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS((R))) Society recommendations. World J. Surg. 2013, 37, 259–284. [Google Scholar] [CrossRef]
- Staszewicz, W.; Eisenring, M.-C.; Bettschart, V.; Harbarth, S.; Troillet, N. Thirteen years of surgical site infection surveillance in Swiss hospitals. J. Hosp. Infect. 2014, 88, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Horan, T.C.; Gaynes, R.P.; Martone, W.J.; Jarvis, W.R.; Emori, T.G. CDC definitions of nosocomial surgical site infections, 1992: A modification of CDC definitions of surgical wound infections. Am. J. Infect. Control. 1992, 20, 271–274. [Google Scholar] [CrossRef]
- Cima, R.; Dankbar, E.; Lovely, J.; Pendlimari, R.; Aronhalt, K.; Nehring, S.; Hyke, R.; Tyndale, D.; Rogers, J.; Quast, L. Colorectal Surgery Surgical Site Infection Reduction Program: A National Surgical Quality Improvement Program–Driven Multidisciplinary Single-Institution Experience. J. Am. Coll. Surg. 2013, 216, 23–33. [Google Scholar] [CrossRef]
- Keenan, J.E.; Speicher, P.J.; Thacker, J.K.; Walter, M.; Kuchibhatla, M.; Mantyh, C.R. The preventive surgical site infection bundle in colorectal surgery: An effective approach to surgical site infection reduction and health care cost savings. JAMA Surg. 2014, 149, 1045–1052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanner, J.; Kiernan, M.; Hilliam, R.; Davey, S.; Collins, E.; Wood, T.; Ball, J.; Leaper, D. Effectiveness of a care bundle to reduce surgical site infections in patients having open colorectal surgery. Ann. R. Coll. Surg. Engl. 2016, 98, 270–274. [Google Scholar] [CrossRef] [Green Version]
- Zywot, A.; Lau, C.S.; Fletcher, H.S.; Paul, S. Bundles Prevent Surgical Site Infections After Colorectal Surgery: Meta-analysis and Systematic Review. J. Gastrointest. Surg. 2017, 21, 1915–1930. [Google Scholar] [CrossRef]
- Gomila, A.; Carratalà, J.; Biondo, S.; Badia, J.; Fraccalvieri, D.; Shaw, E.; Diaz-Brito, V.; Pagespetit, L.; Freixas, N.; Brugués, M.; et al. Predictive factors for early- and late-onset surgical site infections in patients undergoing elective colorectal surgery. A multicentre, prospective, cohort study. J. Hosp. Infect. 2018, 99, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; ElSolh, B.; Patel, S.V. Wound protectors in reducing surgical site infections in lower gastrointestinal surgery: An updated meta-analysis. Surg. Endosc. 2017, 32, 1111–1122. [Google Scholar] [CrossRef]
- Chen, C.-F.; Tsai, H.-L.; Huang, C.-W.; Yeh, Y.-S.; Ma, C.-J.; Chang, T.-K.; Su, W.-C.; Wang, J.-Y. Impact of a Dual-Ring Wound Protector on Outcome After Elective Surgery for Colorectal Cancer. J. Surg. Res. 2019, 244, 136–145. [Google Scholar] [CrossRef]
- Pinkney, T.D.; Calvert, M.; Bartlett, D.C.; Gheorghe, A.; Redman, V.; Dowswell, G.; Hawkins, W.; Mak, T.; Youssef, H.; Richardson, C.; et al. Impact of wound edge protection devices on surgical site infection after laparotomy: Multicentre random-ised controlled trial (ROSSINI Trial). BMJ 2013, 347, f4305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webster, J.; Liu, Z.; Norman, G.; Dumville, J.C.; Chiverton, L.; Scuffham, P.; Stankiewicz, M.; Chaboyer, W.P. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst. Rev. 2019, 3, CD009261. [Google Scholar] [CrossRef] [Green Version]
- Sahebally, S.M.; McKevitt, K.; Stephens, I.; Fitzpatrick, F.; Deasy, J.; Burke, J.P.; McNamara, D. Negative Pres-sure Wound Therapy for Closed Laparotomy Incisions in General and Colorectal Surgery: A Sys-tematic Review and Meta-analysis. JAMA Surg. 2018, 153, e183467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strugala, V.; Martin, R. Meta-Analysis of Comparative Trials Evaluating a Prophylactic Single-Use Negative Pressure Wound Therapy System for the Prevention of Surgical Site Complications. Surg. Infect. 2017, 18, 810–819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuper, T.M.; Murphy, P.B.; Kaur, B.; Ott, M.C. Prophylactic Negative Pressure Wound Therapy for Closed Laparotomy Incisions: A Meta-analysis of Randomized Controlled Trials. Ann. Surg. 2020, 271, 67–74. [Google Scholar] [CrossRef]
- Lau, A.; Lowlaavar, N.; Cooke, E.M.; West, N.; German, A.; Morse, D.J.; Görges, M.; Merchant, R.N. Effect of preoperative warming on intraoperative hypothermia: A randomized-controlled trial. Can. J. Anesth. 2018, 65, 1029–1040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsuchida, T.; Takesue, Y.; Ichiki, K.; Uede, T.; Nakajima, K.; Ikeuchi, H.; Uchino, M. Influence of Peri-Operative Hypothermia on Surgical Site Infection in Prolonged Gastroenterological Surgery. Surg. Infect. 2016, 17, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Sessler, D.I. Perioperative thermoregulation and heat balance. Lancet 2016, 387, 2655–2664. [Google Scholar] [CrossRef]

| Pre-Implementation n = 1256 | Post-Implementation n = 260 | Total n = 1516 | p-Value | |
|---|---|---|---|---|
| Age, median (IQR) | 67 (53–76) | 65 (53–75) | 66 (53–76) | 0.588 |
| Male gender (%) | 667 (53.1) | 156 (60) | 823 (54.3) | 0.041 |
| ASA class ≥ 3 (%) | 556 (44.3) | 114 (43.8) | 670 (44.2) | 0.901 |
| BMI (kg/m2, mean ± SD) | 24.7 ± 5.5 | 25.1 ± 5.3 | 24.9 ± 5.4 | 0.427 |
| Emergency (%) | 530 (42.2) | 85 (32.7) | 615 (40.6) | 0.004 |
| Laparoscopy (%) | 729 (58.0) | 136 (52.3) | 865 (57.1) | 0.09 |
| Conversion (%) | 187 (14.9) | 29 (11.1) | 216 (14.2) | 0.107 |
| Surgical duration (min, mean ± SD) | 170 ± 100 | 172 ± 102 | 170 ± 100 | 0.857 |
| Contamination class (%) | <0.001 | |||
| II | 566 (45.1) | 156 (60) | 722 (47.6) | |
| III | 388 (30.9) | 32 (12.3) | 420 (27.7) | |
| IV | 302 (24.0) | 72 (27.7) | 374 (24.7) | |
| NNIS score (%) | <0.001 | |||
| 0 | 188 (15.0) | 74 (28.5) | 262 (17.3) | |
| 1 | 455 (36.2) | 97 (37.3) | 552 (36.4) | |
| 2 | 484 (38.5) | 79 (30.4) | 563 (37.1) | |
| 3 | 129 (10.3) | 10 (3.8) | 139 (9.2) |
| Pre-Implementation n = 520 | Post-Implementation n = 260 | Total n = 780 | p-Value McNemar | |
|---|---|---|---|---|
| Age, median (IQR) | 66 (5–75) | 65 (53–75) | 66 (54–75) | 0.706 * |
| Male gender (%) | 305 (58.7) | 156 (60) | 461 (59.1) | 0.928 |
| Emergency (%) | 164 (31.5) | 85 (32.7) | 249 (31.9) | >0.99 |
| Laparoscopy (%) | 279 (53.7) | 136 (52.3) | 415 (53.2) | >0.99 |
| Conversion (%) | 49 (17.6) | 29 (21.3) | 78 (18.8) | 0.542 |
| NNIS score (%) | 0.402 | |||
| 0 | 131 (25.2) | 74 (28.5) | 205 (26.3) | |
| 1 | 227 (43.7) | 97 (37.3) | 324 (41.5) | |
| 2 | 139 (26.7) | 79 (30.4) | 218 (27.9) | |
| 3 | 23 (4.4) | 10 (3.8) | 33 (4.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jurt, J.; Hübner, M.; Clerc, D.; Curchod, P.; Abd El Aziz, M.A.; Hahnloser, D.; Senn, L.; Demartines, N.; Grass, F. Challenges Related to Surgical Site Infection Prevention—Results after Standardized Bundle Implementation. J. Clin. Med. 2021, 10, 4524. https://doi.org/10.3390/jcm10194524
Jurt J, Hübner M, Clerc D, Curchod P, Abd El Aziz MA, Hahnloser D, Senn L, Demartines N, Grass F. Challenges Related to Surgical Site Infection Prevention—Results after Standardized Bundle Implementation. Journal of Clinical Medicine. 2021; 10(19):4524. https://doi.org/10.3390/jcm10194524
Chicago/Turabian StyleJurt, Jonas, Martin Hübner, Daniel Clerc, Pauline Curchod, Mohamed A. Abd El Aziz, Dieter Hahnloser, Laurence Senn, Nicolas Demartines, and Fabian Grass. 2021. "Challenges Related to Surgical Site Infection Prevention—Results after Standardized Bundle Implementation" Journal of Clinical Medicine 10, no. 19: 4524. https://doi.org/10.3390/jcm10194524
APA StyleJurt, J., Hübner, M., Clerc, D., Curchod, P., Abd El Aziz, M. A., Hahnloser, D., Senn, L., Demartines, N., & Grass, F. (2021). Challenges Related to Surgical Site Infection Prevention—Results after Standardized Bundle Implementation. Journal of Clinical Medicine, 10(19), 4524. https://doi.org/10.3390/jcm10194524







