Postnatal Repair of Open Neural Tube Defects: A Single Center with 90-Month Interdisciplinary Follow-Up
Abstract
:1. Introduction
2. Materials and Methods
2.1. Presurgical Treatment
2.2. Surgical Repair
2.3. Postoperative Care
2.4. Statistics
3. Results
3.1. Hydrocephalus
3.2. Chiari II
3.3. Secondary Tethered Cord
3.4. Additional NTDs
3.5. Nephro-Urological Follow-Up
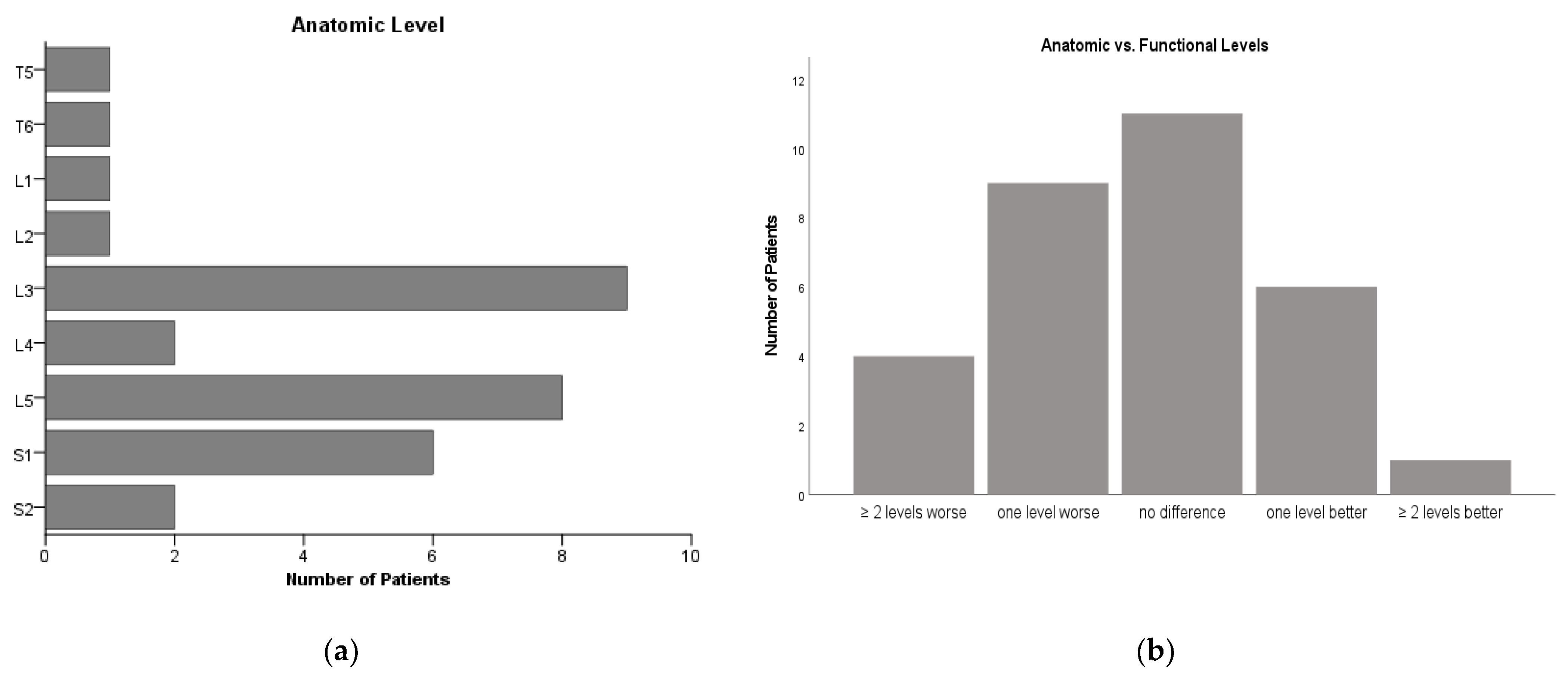
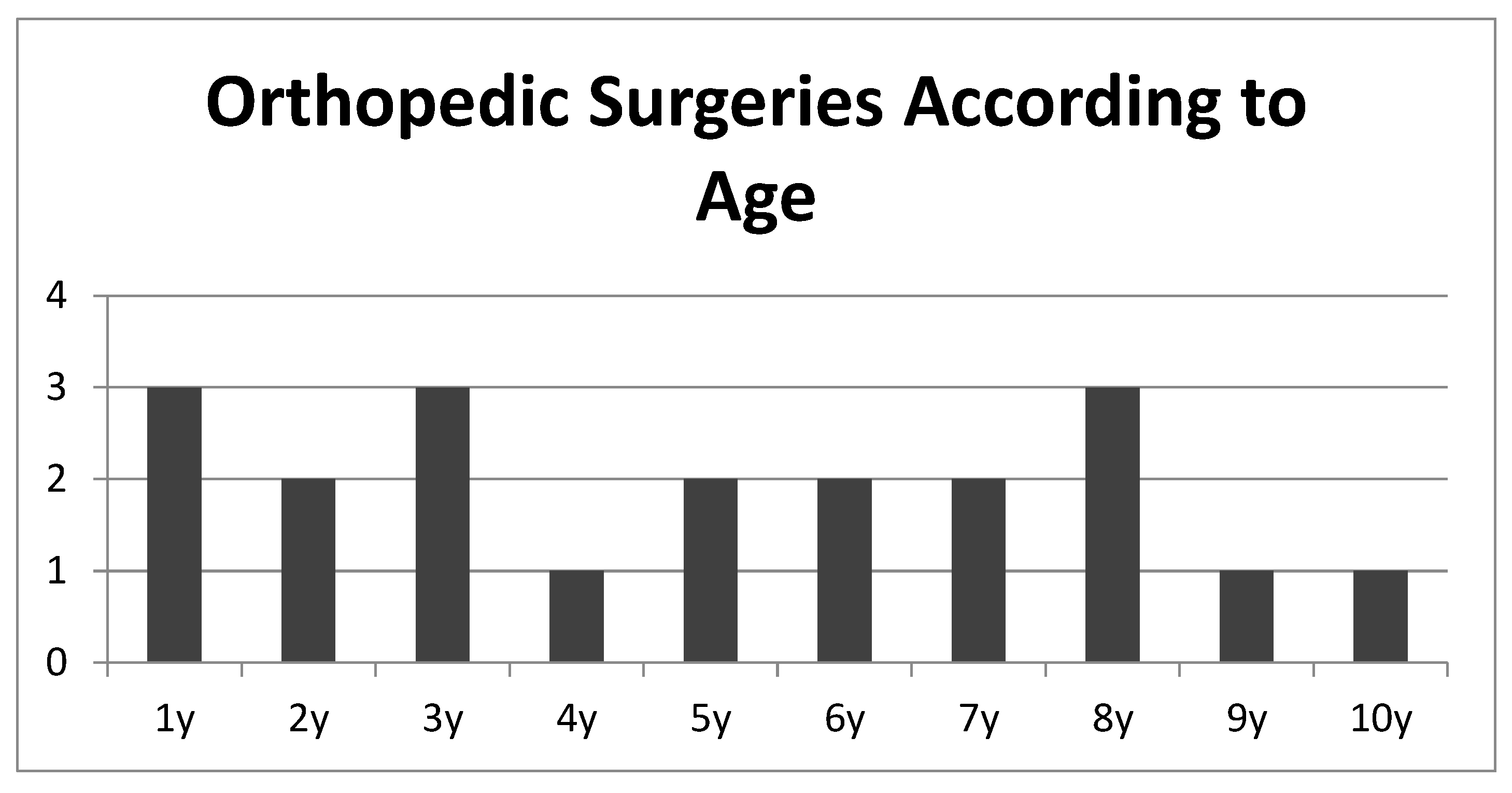
3.6. Orthopedic Follow-Up
3.7. Ambulation
3.8. Status Post Prenatal Repair
4. Discussion
4.1. Morbidity and Mortality
4.2. Hydrocephalus
4.3. Chiari II
4.4. Secondary Tethered Cord
4.5. Nephrourological
4.6. Orthopedic
4.7. Independent Ambulation
4.8. Status Post Prenatal Repair
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heffez, D.S.; Aryanpur, J.; Hutchins, G.M.; Freeman, J.M. The paralysis associated with myelomeningocele: Clinical and experimental data implicating a preventable spinal cord injury. Neurosurgery 1990, 26, 987–992. [Google Scholar] [CrossRef]
- Adzick, N.S.; Thom, E.A.; Spong, C.Y.; Brock, J.W., 3rd; Burrows, P.K.; Johnson, M.P.; Howel, L.J.; Farrell, J.A.; Mary, M.S.N.; Sutton, L.N.; et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N. Engl. J. Med. 2011, 364, 993–1004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meuli, M.; Moehrlen, U. Fetal surgery for myelomeningocele is effective: A critical look at the whys. Pediatr. Surg. Int. 2014, 30, 689–697. [Google Scholar] [CrossRef] [PubMed]
- Grivell, R.M.; Andersen, C.; Dodd, J.M. Prenatal versus postnatal repair procedures for spina bifida for improving infant and maternal outcomes. Cochrane Database Syst. Rev. 2014, 28, CD008825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weaver, K.J.; McDowell, M.M.; White, M.D.; Tempel, Z.J.; Zwagerman, N.T.; Deibert, C.P.; Bonfield, C.M.; Johnson, S.; Greene, S. Comparison of Follow-Up Length-Matched Single-Center Myelomeningocele Postnatal Closure Cohort to the Management of Myelomeningocele Study (MOMS) Trial Results. Pediatr. Neurosurg. 2021, 56, 229–238. [Google Scholar] [CrossRef]
- Shurtleff, D. Fetal endoscopic myelomeningocele repair. Dev. Med. Child Neurol. 2012, 54, 4–5. [Google Scholar] [CrossRef]
- Zarutskie, A.; Guimaraes, C.; Yepez, M.; Torres, P.; Shetty, A.; Sangi-Haghpeykar, H.; Lee, W.; Espinoza, J.; Shamshirsaz, A.A.; Nassr, A.; et al. Prenatal brain imaging for predicting need for postnatal hydrocephalus treatment in fetuses that had neural tube defect repair in utero. Ultrasound Obstet. Gynecol. 2019, 53, 324–334. [Google Scholar] [CrossRef] [Green Version]
- Moldenhauer, S.; Soni, S.; Rintoul, N.E.; Spinner, S.S.; Khalek, N.; Martinez-Poyer, J.; Flake, A.W.; Hedrick, H.L.; Peranteau, W.H.; Rendon, N.; et al. Fetal myelomeningocele repair: The post-MOMS experience at the Children’s Hospital of Philadelphia. Fetal Diagn. Ther. 2015, 37, 235–240. [Google Scholar] [CrossRef]
- Moldenhauer, J.S.; Adzick, N.S. Fetal surgery for myelomeningocele: After the Management of Myelomeningocele Study (MOMS). Semin. Fetal. Neonatal. Med. 2017, 22, 360–366. [Google Scholar] [CrossRef]
- Bruner, J.P.; Richards, W.O.; Tulipan, N.B.; Arney, T.L. Endoscopic coverage of fetal myelomeningocele in utero. Am. J. Obstet. Gynecol. 1999, 180, 153–158. [Google Scholar] [CrossRef]
- Houtrow, A.J.; Thom, E.A.; Fletcher, J.M.; Burrows, P.K.; Adzick, N.S.; Thomas, N.H.; Brock, J.W.; Cooper, T.; Lee, H.; Bilaniuk, L.; et al. Prenatal Repair of Myelomeningocele and School-age Functional Outcomes. Pediatrics 2020, 145, e20191544. [Google Scholar] [CrossRef] [PubMed]
- Diehl, D.; Belke, F.; Kohl, T.; Axt-Fliedner, R.; Degenhardt, J.; Khaleeva, A.; Oehmke, F.; Faas, D.; Ehrhardt, H.; Kolodziej, M.; et al. Fully percutaneous fetoscopic repair of myelomeningocele: 30-month follow-up data. Ultrasound Obstet. Gynecol. 2021, 57, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Lapa, D.A. Endoscopic fetal surgery for neural tube defects. Best Pract. Res. Clin. Obstet. Gynaecol. 2019, 58, 133–141. [Google Scholar] [CrossRef]
- Sacco, A.; van der Veeken, L.; Bagshaw, E.; Ferguson, C.; van Mieghem, T.; David, A.L.; Deprest, J. Maternal complications following open and fetoscopic fetal surgery: A systematic review and meta-analysis. Prenat. Diagn. 2019, 39, 251–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radic, J.A.E.; Illes, J.; McDonald, P.J. Fetal Repair of Open Neural Tube Defects: Ethical, Legal, and Social Issues. Camb. Q. Healthc. Ethics 2019, 28, 476–487. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.D.; Pollack, I.F.; Pang, D.; Albright, A.L. Comparison of simultaneous versus delayed ventriculoperitoneal shunt insertion in children undergoing myelomeningocele repair. J. Child Neurol. 1996, 11, 370–372. [Google Scholar] [CrossRef] [PubMed]
- Januschek, E.; Rohrig, A.; Kunze, S.; Fremerey, C.; Wiebe, B.; Messing-Junger, M. Myelomeningocele—A single institute analysis of the years 2007 to 2015. Childs Nerv. Syst. 2016, 32, 1281–1287. [Google Scholar] [CrossRef]
- Laskay, N.M.B.; Arynchyna, A.A.; McClugage, S.G., 3rd; Hopson, B.; Shannon, C.; Ditty, B.; Wellons, J.C., III; Blount, J.P.; Rocque, B.G. A comparison of the MOMS trial results to a contemporaneous, single-institution, postnatal closure cohort. Childs Nerv. Syst. 2017, 33, 639–646. [Google Scholar] [CrossRef] [Green Version]
- Kim, I.; Hopson, B.; Aban, I.; Rizk, E.B.; Dias, M.S.; Bowman, R.; Ackerman, L.L.; Partington, M.D.; Castillo, H.; Castillo, J. Treated hydrocephalus in individuals with myelomeningocele in the National Spina Bifida Patient Registry. J. Neurosurg. Pediatr. 2018, 22, 646–651. [Google Scholar] [CrossRef]
- Marreiros, H.; Loff, C.; Calado, E. Who needs surgery for pediatric myelomeningocele? A retrospective study and literature review. J. Spinal Cord Med. 2015, 38, 626–640. [Google Scholar] [CrossRef] [Green Version]
- Hilton, S.A.; Hodges, M.M.; Dewberry, L.C.; Handler, M.; Galan, H.L.; Zaretsky, M.V.; Behrendt, N.; Marwan, A.I.; Liechty, K.W. MOMS Plus: Single-Institution Review of Outcomes for Extended BMI Criteria for Open Fetal Repair of Myelomeningocele. Fetal Diagn. Ther. 2019, 46, 411–414. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, A.; Crimmins, D.; Hayward, R.; Thompson, D. Toward reducing shunt placement rates in patients with myelomeningocele. J. Neurosurg. Pediatr. 2008, 1, 361–365. [Google Scholar] [CrossRef]
- Kohl, T. Percutaneous minimally invasive fetoscopic surgery for spina bifida aperta. Part I: Surgical technique and perioperative outcome. Ultrasound Obstet. Gynecol. 2014, 44, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Kohl, T.; Tchatcheva, K.; Merz, W.; Wartenberg, H.C.; Heep, A.; Muller, A.; Franz, A.; Stressig, R.; Willinek, W.; Gembruch, U. Percutaneous fetoscopic patch closure of human spina bifida aperta: Advances in fetal surgical techniques may obviate the need for early postnatal neurosurgical intervention. Surg. Endosc. 2009, 23, 890–895. [Google Scholar] [CrossRef]
- Brock, J.W., 3rd; Thomas, J.C.; Baskin, L.S.; Zderic, S.A.; Thom, E.A.; Burrows, P.K.; Lee, H.; Houtrow, A.J.; MacPherson, P.; Adzick, N.S. Effect of Prenatal Repair of Myelomeningocele on Urological Outcomes at School Age. J. Urol. 2019, 202, 812–818. [Google Scholar] [CrossRef]
- Flanders, T.M.; Madsen, P.J.; Pisapia, J.M.; Hudgins, E.D.; Mackell, C.M.; Alexander, E.E.; Moldenhauer, J.S.; Zarnow, D.M.; Flake, A.W.; Adzick, N.S.; et al. Improved Postoperative Metrics with Modified Myofascial Closure in Fetal Myelomeningocele Repair. Oper. Neurosurg. 2020, 18, 158–165. [Google Scholar] [CrossRef] [PubMed]


| Symptom Complex | Investigations |
|---|---|
| Hydrocephalus |
|
| Tethered Cord |
|
| Urological |
|
| Orthopedic |
|
| Hydrocephalus | Criteria for hydrocephalus treatment were the same that were implemented in the MOMS trial [2]. In patients meeting these criteria after 12 months of age, endoscopic third ventriculostomy (ETV) was performed instead of shunt implantation. |
| Secondary tethered cord | Untethering is performed for symptomatic tethered cord, which includes loss of motor function, a reduction in somatosensory evoked potentials, progressive syringomyelia or spasticity, higher frequency of bladder infection, changes in bladder pressure, and/or progressive development of deformities of lower extremities. |
| Chiari malformation | Indication for Chiari decompression was based on cranial nerve palsy, central apnea, and progressive syringomyelia, not solely on radiological findings. |
| Orthopedic surgeries | Indications for lower limb surgery were dependent on the functional status of the children, as some are limited to ambulating patients. Spine surgeries are indicated for thoracic insufficiency syndrome or progressive scoliosis or kyphosis. |
| Urologic surgeries | Urologic surgeries were indicated for reflux, upper urinary tract deterioration, catheterization problems, and bowel management. |
| Pat. Nr. | Gestational Age at Birth (weeks) | Anatomical Level | Hydrocephalus; Shunt/ETV; (Age) | Ambulation | Urological | Other Neurosurgical Surgeries | FU (Months) |
|---|---|---|---|---|---|---|---|
| 1 | 26 | sacral | Yes; Shunt (3.5 months) | Pat. 1 year old | Antichol. Meds; no self-cath | 15 CSF surgeries total | 16 |
| 2 | 36 | L2/3 | Yes; ETV (16 months) | Crawls with orthosis, Pat. < 2 yrs | No meds; no self-cath | none | 18 |
| 3 | 35 | sacral | No | Freely | No meds; no self-cath | CSF fistula repair on day of birth; see Figure 4 | 94 |
| 4 | 30 | L4-S1 | No | With orthosis | unknown | None | 67 |
| 5 | 31 | L5 | Yes; Shunt (0.5 months) | With walker + orthosis | Antichol. Meds; self-cath | None | 49 |
| 6 | 30 | T12-L1 | Yes; Shunt (4 days) | Wheelchair | Antichol. Meds; no self-cath | Detethering at age 11 | 183 |
| 7 | 38 | L4/5 | No | With orthosis | Antichol. Meds; self-cath | None | 69 |
| 8 | 24 | L4/5 | Yes; Shunt (within first year of life) | Antichol. Meds; self-cath | Detethering recently indicated | 109 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hagemann, C.; Krajewski, K.; Henne, T.; Stücker, R.; Kunkel, P. Postnatal Repair of Open Neural Tube Defects: A Single Center with 90-Month Interdisciplinary Follow-Up. J. Clin. Med. 2021, 10, 4510. https://doi.org/10.3390/jcm10194510
Hagemann C, Krajewski K, Henne T, Stücker R, Kunkel P. Postnatal Repair of Open Neural Tube Defects: A Single Center with 90-Month Interdisciplinary Follow-Up. Journal of Clinical Medicine. 2021; 10(19):4510. https://doi.org/10.3390/jcm10194510
Chicago/Turabian StyleHagemann, Christian, Kara Krajewski, Thomas Henne, Ralf Stücker, and Philip Kunkel. 2021. "Postnatal Repair of Open Neural Tube Defects: A Single Center with 90-Month Interdisciplinary Follow-Up" Journal of Clinical Medicine 10, no. 19: 4510. https://doi.org/10.3390/jcm10194510
APA StyleHagemann, C., Krajewski, K., Henne, T., Stücker, R., & Kunkel, P. (2021). Postnatal Repair of Open Neural Tube Defects: A Single Center with 90-Month Interdisciplinary Follow-Up. Journal of Clinical Medicine, 10(19), 4510. https://doi.org/10.3390/jcm10194510





