Clinical Significance of Intraoperative Exposure of Inferior Alveolar Nerve during Surgical Extraction of the Mandibular Third Molar in Nerve Injury
Abstract
:1. Introduction
2. Materials and Methods
2.1. Samples and Group Assignment
- (1)
- Patients who were medically healthy and over 16 years of age
- (2)
- Patients who underwent the surgical extraction of mandibular third molar under local anesthesia
- (3)
- Patients who visited the hospital for suture removal and follow-up check
- (4)
- Patients whose preoperative panoramic view was available and whose preoperative cone-beam computed tomography (CBCT) was available only when the mandibular third molar and the IAN canal overlapped on the panoramic radiograph
- (1)
- Patients who underwent the simple extraction of mandibular third molar or surgical extraction of mandibular third molar under general anesthesia
- (2)
- Patients whose adjacent molars were extracted simultaneously
- (3)
- Patients with mandibular third molar associated with periapical or cystic lesions or tumors
- (4)
- Patients taking steroids for medical problems
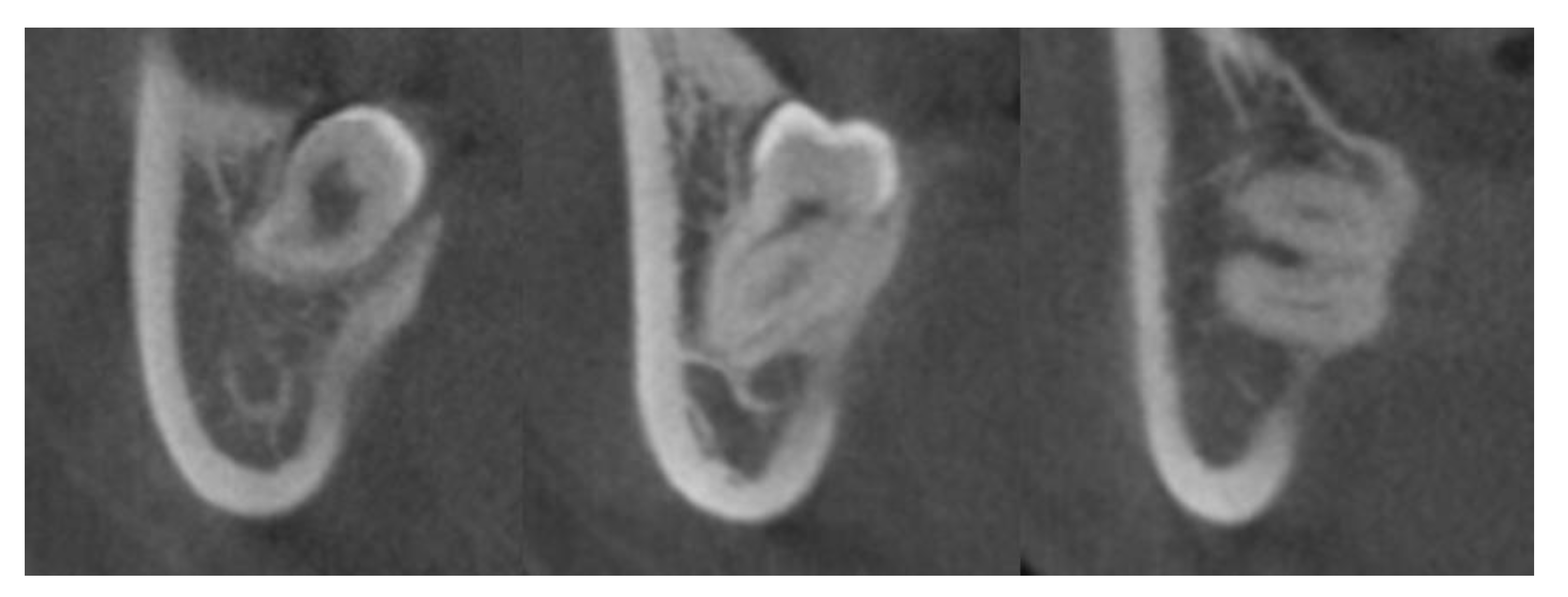
2.2. CBCT Image Acquisition and Assessment of the Relationship between the IAN Canal and Mandibular Third Molar in the Exposed Group
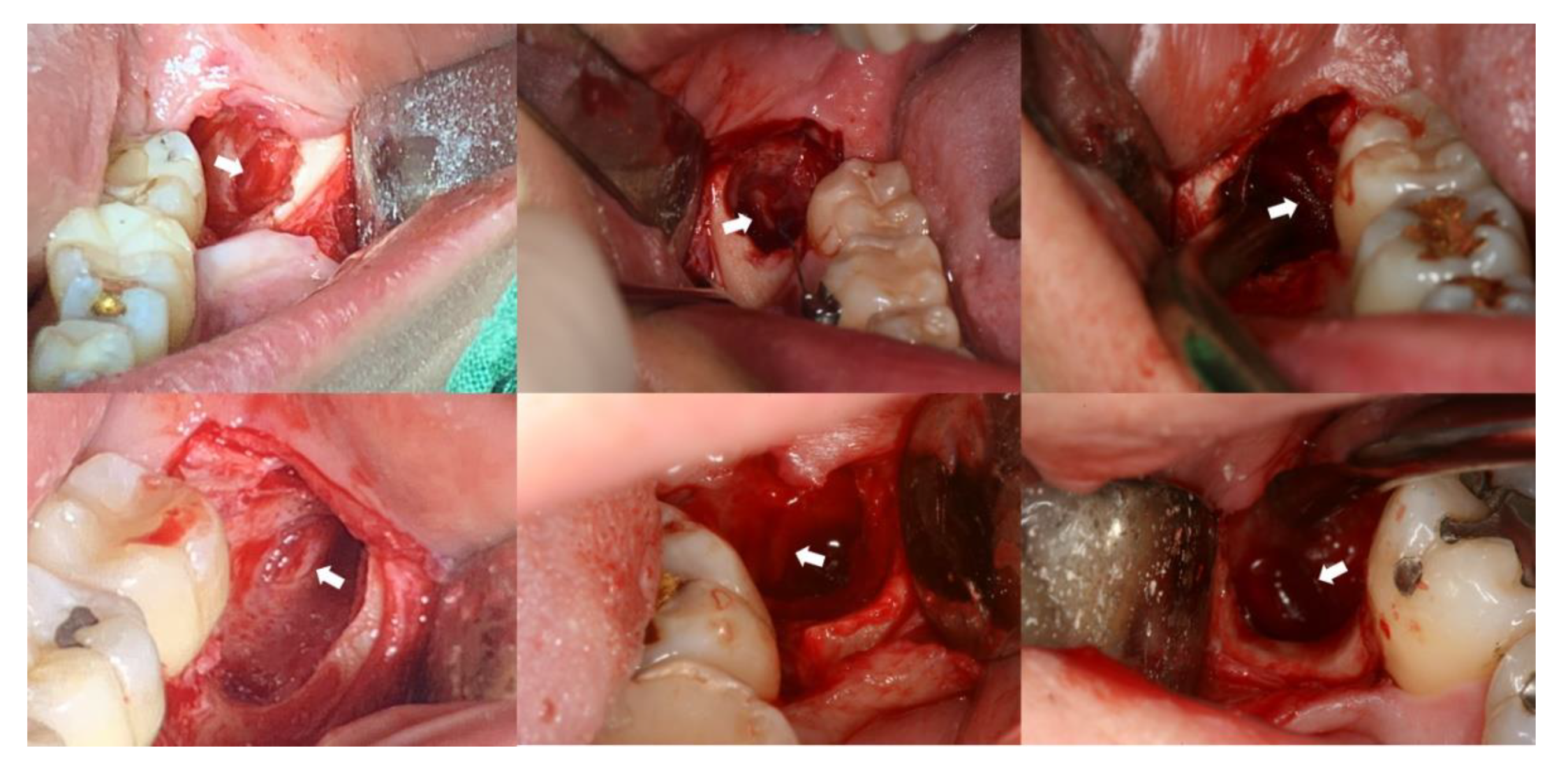
2.3. Surgical Procedure and Identification of IAN Exposure
2.4. Statistical Analysis
3. Results
3.1. Comparison of Demographic or Procedure-Related Variables and the Incidence of IAN Injury between the Two Groups
3.2. Radiographic Characteristics in the Exposed Group
3.3. Factors Affecting the Occurrence of IAN Injury after Surgical Extraction of Mandibular Third Molar in the Exposed Group
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cheung, L.K.; Leung, Y.Y.; Chow, L.K.; Wong, M.C.; Chan, E.K.; Fok, Y.H. Incidence of neurosensory deficits and recovery after lower third molar surgery: A prospective clinical study of 4338 cases. Int. J. Oral Maxillofac. Surg. 2010, 39, 320–326. [Google Scholar] [CrossRef] [Green Version]
- Haug, R.H.; Perrott, D.H.; Gonzalez, M.L.; Talwar, R.M. The American Association of Oral and Maxillofacial Surgeons Age-Related Third Molar Study. J. Oral Maxillofac. Surg. 2005, 63, 1106–1114. [Google Scholar] [CrossRef]
- Lopes, V.; Mumenya, R.; Feinmann, C.; Harris, M. Third molar surgery: An audit of the indications for surgery, post-operative complaints and patient satisfaction. Br. J. Oral Maxillofac. Surg. 1995, 33, 33–35. [Google Scholar] [CrossRef]
- Renton, T.; McGurk, M. Evaluation of factors predictive of lingual nerve injury in third molar surgery. Br. J. Oral Maxillofac. Surg. 2001, 39, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Roccuzzo, A.; Molinero-Mourelle, P.; Ferrillo, M.; Cobo-Vázquez, C.; Sanchez-Labrador, L.; Ammendolia, A.; Migliario, M.; de Sire, A. Type I Collagen-Based Devices to Treat Nerve Injuries after Oral Surgery Procedures. A Systematic Review. Appl. Sci. 2021, 11, 3927. [Google Scholar] [CrossRef]
- Tantanapornkul, W.; Okouchi, K.; Fujiwara, Y.; Yamashiro, M.; Maruoka, Y.; Ohbayashi, N.; Kurabayashi, T. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2007, 103, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, T.; Ri, S.; Umeda, M.; Komori, T. Multivariate relationships among risk factors and hypoesthesia of the lower lip after extraction of the mandibular third molar. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2011, 111, e1–e7. [Google Scholar] [CrossRef]
- Maegawa, H.; Sano, K.; Kitagawa, Y.; Ogasawara, T.; Miyauchi, K.; Sekine, J.; Inokuchi, T. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2003, 96, 639–646. [Google Scholar] [CrossRef]
- Tay, A.B.; Go, W.S. Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J. Oral Maxillofac. Surg. 2004, 62, 592–600. [Google Scholar] [CrossRef]
- Sedaghatfar, M.; August, M.A.; Dodson, T.B. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J. Oral Maxillofac. Surg. 2005, 63, 3–7. [Google Scholar] [CrossRef]
- Smith, W.P. The relative risk of neurosensory deficit following removal of mandibular third molar teeth: The influence of radiography and surgical technique. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2013, 115, 18–24. [Google Scholar] [CrossRef]
- Xu, G.Z.; Yang, C.; Fan, X.D.; Yu, C.Q.; Cai, X.Y.; Wang, Y.; He, D. Anatomic relationship between impacted third mandibular molar and the mandibular canal as the risk factor of inferior alveolar nerve injury. Br. J. Oral Maxillofac. Surg. 2013, 51, e215–e219. [Google Scholar] [CrossRef]
- Ohman, A.; Kivijarvi, K.; Blomback, U.; Flygare, L. Pre-operative radiographic evaluation of lower third molars with computed tomography. Dentomaxillofac. Radiol. 2006, 35, 30–35. [Google Scholar] [CrossRef] [Green Version]
- Jones, K.J. Steroid hormones and neurotrophism: Relationship to nerve injury. Metab. Brain Dis. 1988, 3, 1–18. [Google Scholar] [CrossRef]
- Kawata, M. Roles of steroid hormones and their receptors in structural organization in the nervous system. Neurosci. Res. 1995, 24, 1–46. [Google Scholar] [CrossRef]
- Tsai, S.Y.; Chiu, P.Y.; Yang, C.P.; Lee, Y.H. Synergistic effects of corticosterone and kainic acid on neurite outgrowth in axotomized dorsal root ganglion. Neuroscience 2002, 114, 55–67. [Google Scholar] [CrossRef]
- Yao, G.L.; Kiyama, H. Dexamethasone enhances level of GAP-43 mRNA after nerve injury and facilitates re-projection of the hypoglossal nerve. Brain Res. Mol. Brain Res. 1995, 32, 308–312. [Google Scholar] [CrossRef]
- Jerjes, W.; Upile, T.; Nhembe, F.; Gudka, D.; Shah, P.; Abbas, S.; McCarthy, E.; Patel, S.; Mahil, J.; Hopper, C. Experience in third molar surgery: An update. Br. Dent. J. 2010, 209, E1. [Google Scholar] [CrossRef] [PubMed]
- Bell, G.W. Use of dental panoramic tomographs to predict the relation between mandibular third molar teeth and the inferior alveolar nerve. Radiological and surgical findings, and clinical outcome. Br. J. Oral Maxillofac. Surg. 2004, 42, 21–27. [Google Scholar] [CrossRef]
- Ghai, S.; Choudhury, S. Role of Panoramic Imaging and Cone Beam CT for Assessment of Inferior Alveolar Nerve Exposure and Subsequent Paresthesia Following Removal of Impacted Mandibular Third Molar. J. Maxillofac. Oral Surg. 2018, 17, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Hasani, A.; Ahmadi Moshtaghin, F.; Roohi, P.; Rakhshan, V. Diagnostic value of cone beam computed tomography and panoramic radiography in predicting mandibular nerve exposure during third molar surgery. Int. J. Oral Maxillofac. Surg. 2017, 46, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Lin, T.; Wang, Y.; Sun, C.; Yang, L.; Jiang, H.; Cheng, J. Radiographic features of anatomic relationship between impacted third molar and inferior alveolar canal on coronal CBCT images: Risk factors for nerve injury after tooth extraction. Arch. Med. Sci. 2018, 14, 532–540. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Variables | Exposed Group | Unexposed Group | p-Value |
|---|---|---|---|
| (n = 69) | (n = 219) | ||
| Age (years) | 29.32 ± 8.75 (range: 17-61) | 29.25 ± 10.70 (range: 17-68) | 0.393 |
| Sex (male: female) | 30:34 | 94:82 | 0.370 |
| Side (right: left) | 43:26 | 112:107 | 0.104 |
| Procedural factors | |||
| Bone reduction (n) | 68 (98.6%) | 186 (84.9%) | 0.002 * |
| Odontomy (n) | 59 (85.5%) | 174 (79.5%) | 0.264 |
| Incidence of inferior alveolar nerve injury (n) | 3 (4.3%) | 0 (0%) | 0.013 † |
| Variables | Number of Samples | % |
|---|---|---|
| The course of the inferior alveolar nerve canal * | ||
| Buccal | 2 | 2.9 |
| Lingual | 41 | 59.4 |
| Inferior | 18 | 26.1 |
| Inter-radicular | 8 | 11.6 |
| The proximity of the mandibular third molar to the lingual cortex * | ||
| No contact | 0 | 0 |
| Contact, thinning | 43 | 62.3 |
| Contact, perforation | 26 | 37.7 |
| Variables | OR | 95% CI | p-Value |
|---|---|---|---|
| Age (year) | 1.108 | 1.001–1.228 | 0.048 * |
| Sex | |||
| Male | Ref. | ||
| Female | N/E | N/E | |
| Side | |||
| Right | Ref. | ||
| Left | 3.500 | 0.301–40.652 | 0.317 |
| The course of the inferior alveolar nerve canal | |||
| Buccal | Ref. | ||
| Lingual | N/E | N/E | |
| Inferior | 1.000 | 1.000 | |
| Inter-radicular | N/E | N/E | |
| The proximity of the mandibular third molar to the lingual cortex | |||
| Contact, thinning | Ref. | ||
| Contact, perforation | 3.500 | 0.301–40.652 | 0.317 |
| Bone reduction | N/E | N/E | |
| Odontomy | N/E | N/E |
| Variables | OR | 95% CI | p-Value |
|---|---|---|---|
| Age (year) | 1.108 | 1.001–1.228 | 0.048 * |
| Side (left) | 0.396 | ||
| The proximity of the mandibular third molar to the lingual cortex (contact, perforation) | 0.734 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
On, S.-W.; Cho, S.-W.; Byun, S.-H.; Yang, B.-E. Clinical Significance of Intraoperative Exposure of Inferior Alveolar Nerve during Surgical Extraction of the Mandibular Third Molar in Nerve Injury. J. Clin. Med. 2021, 10, 4379. https://doi.org/10.3390/jcm10194379
On S-W, Cho S-W, Byun S-H, Yang B-E. Clinical Significance of Intraoperative Exposure of Inferior Alveolar Nerve during Surgical Extraction of the Mandibular Third Molar in Nerve Injury. Journal of Clinical Medicine. 2021; 10(19):4379. https://doi.org/10.3390/jcm10194379
Chicago/Turabian StyleOn, Sung-Woon, Seoung-Won Cho, Soo-Hwan Byun, and Byoung-Eun Yang. 2021. "Clinical Significance of Intraoperative Exposure of Inferior Alveolar Nerve during Surgical Extraction of the Mandibular Third Molar in Nerve Injury" Journal of Clinical Medicine 10, no. 19: 4379. https://doi.org/10.3390/jcm10194379
APA StyleOn, S.-W., Cho, S.-W., Byun, S.-H., & Yang, B.-E. (2021). Clinical Significance of Intraoperative Exposure of Inferior Alveolar Nerve during Surgical Extraction of the Mandibular Third Molar in Nerve Injury. Journal of Clinical Medicine, 10(19), 4379. https://doi.org/10.3390/jcm10194379








