Frequency and Factors of Indeterminate QuantiFERON-TB Gold In-Tube and QuantiFERON-TB Gold PLUS Test Results in Rheumatic Diseases
Abstract
:1. Introduction
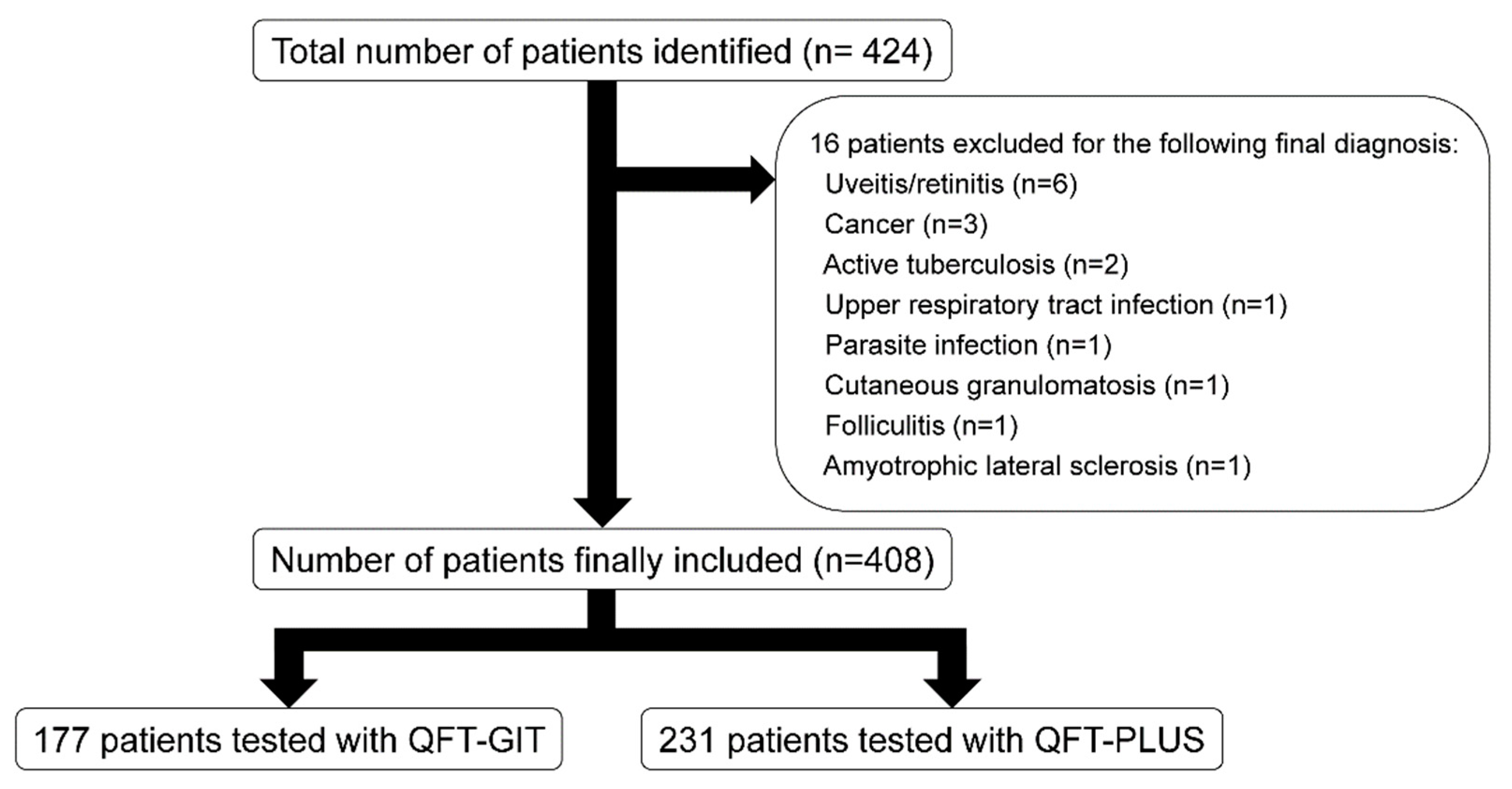
2. Materials and Methods
2.1. Data Collection
2.2. Analysis of Patient Data and Medication
2.3. QFT-GIT and QFT-PLUS Assay and Healthy Controls
2.4. Statistical Analysis
3. Results
3.1. Comparison of Patient Characteristics and Medications between the QFT-GIT and QFT-PLUS Groups
3.2. Indeterminate IGRA Results in Patients with Rheumatic Diseases and Healthy Controls
3.3. Patients with an Indeterminate IGRA and Factors Associated with the Occurrence of Indeterminate Results
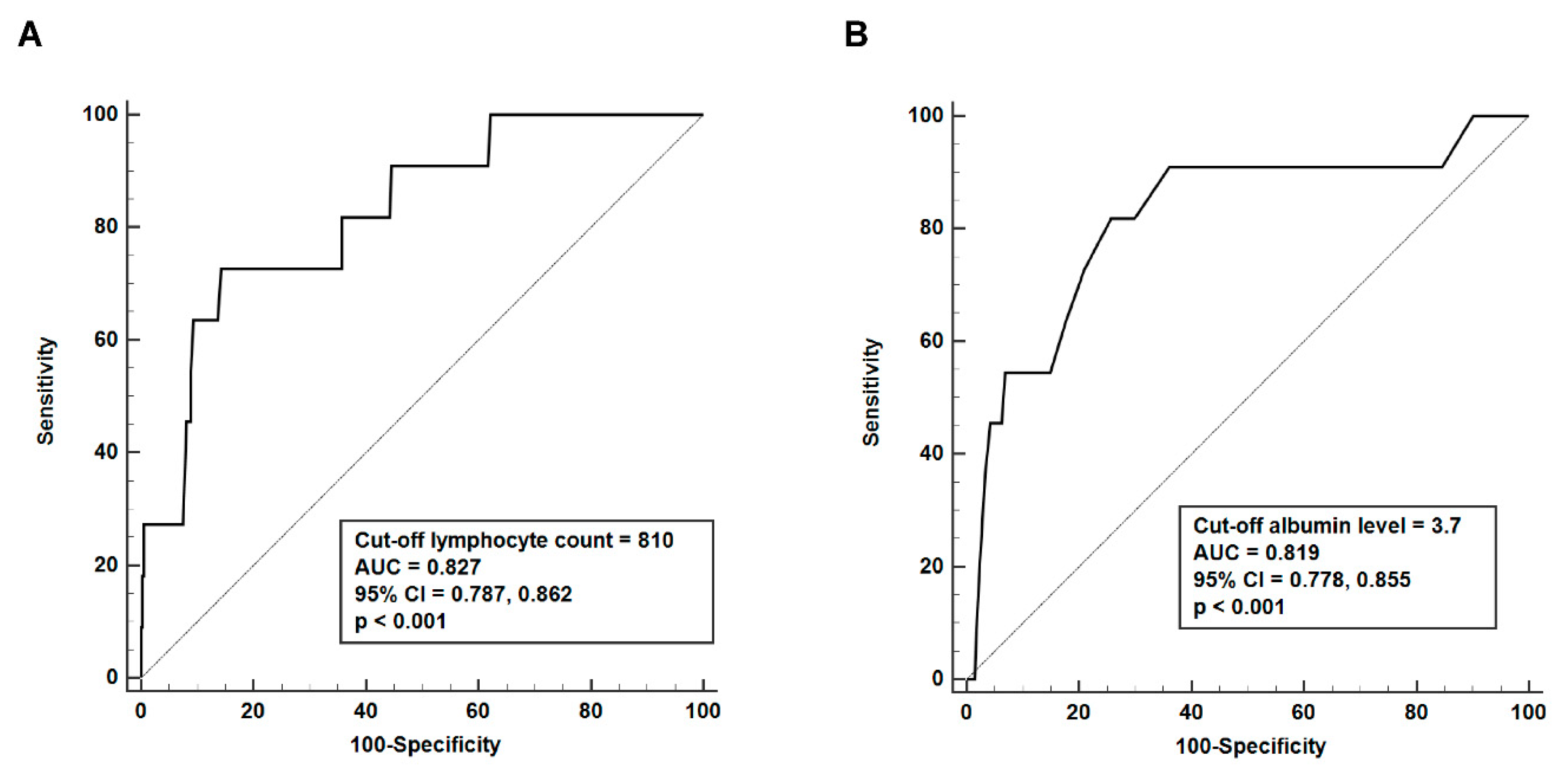
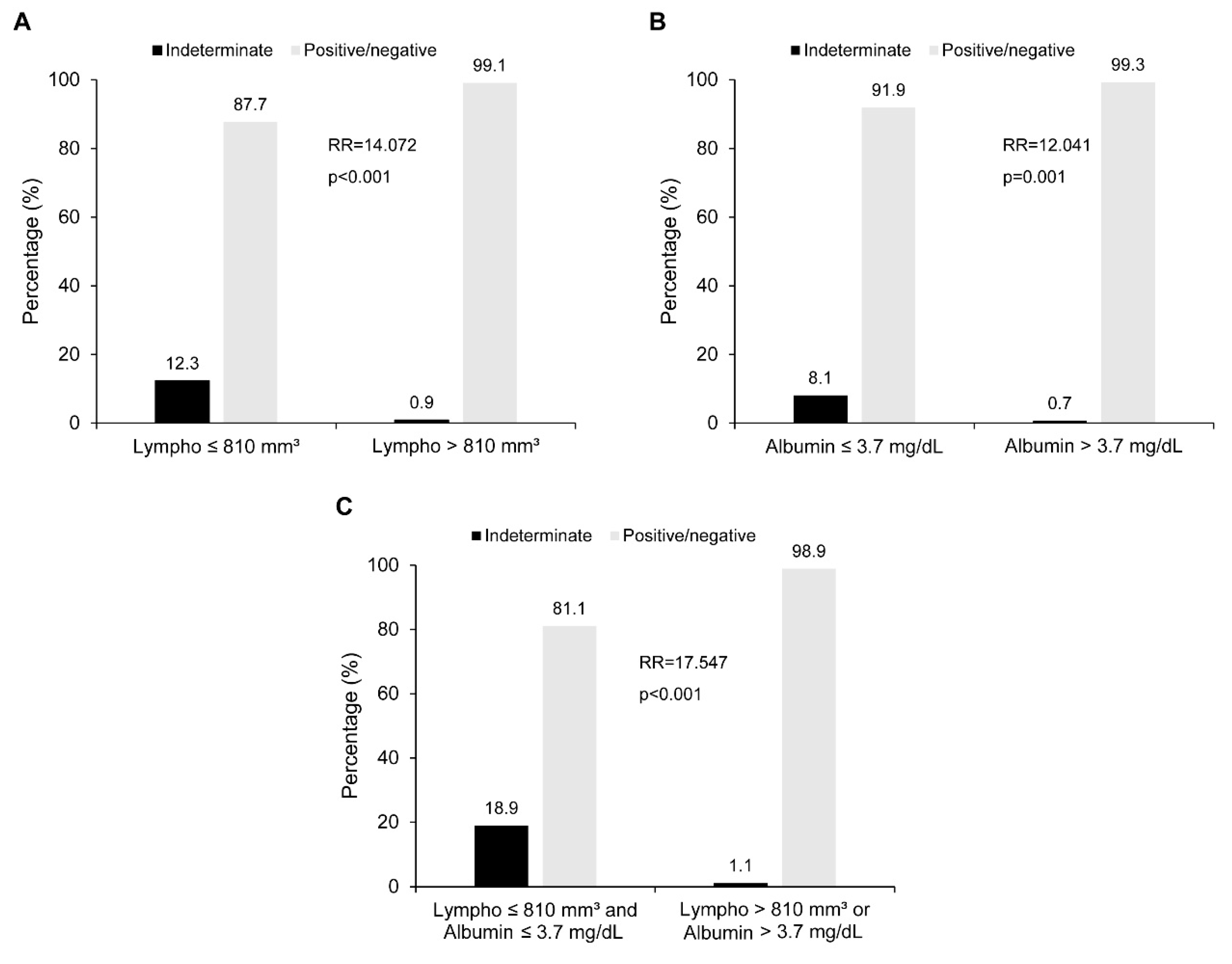
3.4. Estimating Ideal Cut-Off Value of Lymphocyte Count and Albumin Levels for Discrimination of Indeterminate Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Furin, J.; Cox, H.; Pai, M. Tuberculosis. Lancet 2019, 393, 1642–1656. [Google Scholar] [CrossRef]
- Carranza, C.; Pedraza-Sanchez, S.; de Oyarzabal-Mendez, E.; Torres, M. Diagnosis for Latent Tuberculosis Infection: New Alternatives. Front. Immunol. 2020, 11, 2006. [Google Scholar] [CrossRef] [PubMed]
- Zwerling, A.; van den Hof, S.; Scholten, J.; Cobelens, F.; Menzies, D.; Pai, M. Interferon-gamma release assays for tuberculosis screening of healthcare workers: A systematic review. Thorax 2012, 67, 62–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Theel, E.S.; Hilgart, H.; Breen-Lyles, M.; McCoy, K.; Flury, R.; Breeher, L.E.; Wilson, J.; Sia, I.G.; Whitaker, J.A.; Clain, J.; et al. Comparison of the QuantiFERON-TB Gold Plus and QuantiFERON-TB Gold In-Tube Interferon Gamma Release Assays in Patients at Risk for Tuberculosis and in Health Care Workers. J. Clin. Microbiol. 2018, 56, e00614-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moon, H.W.; Yi, A.; Yoon, S.; Kim, H.; Chung, H.J.; Hur, M.; Yun, Y.M.; Yoo, K.H. Serial Assays of QuantiFERON-TB Gold In-Tube and QuantiFERON-TB Gold-Plus in Subjects Exposed to Patients with Active Tuberculosis. Ann. Lab. Med. 2020, 40, 428–430. [Google Scholar] [CrossRef] [PubMed]
- Shafeque, A.; Bigio, J.; Hogan, C.A.; Pai, M.; Banaei, N. Fourth-Generation QuantiFERON-TB Gold Plus: What Is the Evidence? J. Clin. Microbiol. 2020, 58, e01950-19. [Google Scholar] [CrossRef] [PubMed]
- Sotgiu, G.; Saderi, L.; Petruccioli, E.; Aliberti, S.; Piana, A.; Petrone, L.; Goletti, D. QuantiFERON TB Gold Plus for the diagnosis of tuberculosis: A systematic review and meta-analysis. J. Infect. 2019, 79, 444–453. [Google Scholar] [CrossRef]
- Barcellini, L.; Borroni, E.; Brown, J.; Brunetti, E.; Codecasa, L.; Cugnata, F.; Dal Monte, P.; Di Serio, C.; Goletti, D.; Lombardi, G.; et al. First independent evaluation of QuantiFERON-TB Plus performance. Eur. Respir. J. 2016, 47, 1587–1590. [Google Scholar] [CrossRef]
- Gourley, M.; Miller, F.W. Mechanisms of disease: Environmental factors in the pathogenesis of rheumatic disease. Nat. Clin. Pract. Rheumatol. 2007, 3, 172–180. [Google Scholar] [CrossRef]
- Jeong, S.J.; Han, S.H.; Kim, C.O.; Baek, J.H.; Jin, S.J.; Ku, N.S.; Choi, J.Y.; Song, Y.G.; Kim, H.S.; Kim, J.M. Predictive factors for indeterminate result on the QuantiFERON test in an intermediate tuberculosis-burden country. J. Infect. 2011, 62, 347–354. [Google Scholar] [CrossRef]
- Solanich, X.; Fernández-Huerta, M.; Basaez, C.; Antolí, A.; Rocamora-Blanch, G.; Corbella, X.; Santin, M.; Alcaide, F. Clinical Significance of Indeterminate QuantiFERON-TB Gold Plus Assay Results in Hospitalized COVID-19 Patients with Severe Hyperinflammatory Syndrome. J. Clin. Med. 2021, 10, 918. [Google Scholar] [CrossRef]
- Darby, J.; Black, J.; Buising, K. Interferon-gamma release assays and the diagnosis of tuberculosis: Have they found their place? Intern. Med. J. 2014, 44, 624–632. [Google Scholar] [CrossRef]
- Jung, H.J.; Kim, T.J.; Kim, H.S.; Cho, Y.N.; Jin, H.M.; Kim, M.J.; Kang, J.H.; Park, K.J.; Lee, S.J.; Lee, S.S.; et al. Analysis of predictors influencing indeterminate whole-blood interferon-gamma release assay results in patients with rheumatic diseases. Rheumatol. Int. 2014, 34, 1711–1720. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, C.; Overman, R.A.; Dusetzina, S.B.; Hajj-Ali, R.A. Evaluating Indeterminate Interferon-γ-Release Assay Results in Patients With Chronic Inflammatory Diseases Receiving Immunosuppressive Therapy. Arthritis Care Res. (Hoboken) 2015, 67, 1063–1069. [Google Scholar] [CrossRef] [PubMed]
- Won, D.; Park, J.Y.; Kim, H.S.; Park, Y. Comparative Results of QuantiFERON-TB Gold In-Tube and QuantiFERON-TB Gold Plus Assays for Detection of Tuberculosis Infection in Clinical Samples. J. Clin. Microbiol. 2020, 58, e01854-19. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.T.; Ruan, S.Y.; Tsai, Y.J.; Kuo, P.H.; Ku, S.C.; Lee, P.L.; Kuo, L.C.; Hsu, C.L.; Huang, C.K.; Yang, C.Y.; et al. Effects of acute critical illnesses on the performance of interferon-gamma release assay. Sci. Rep. 2016, 6, 19972. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Lim, J.E.; Jung, J.Y.; Son, J.Y.; Lee, K.J.; Yoon, Y.W.; Park, B.H.; Moon, J.W.; Park, M.S.; Kim, Y.S.; et al. Performance of the tuberculin skin test and interferon-gamma release assay for detection of tuberculosis infection in immunocompromised patients in a BCG-vaccinated population. BMC Infect. Dis. 2009, 9, 207. [Google Scholar] [CrossRef] [Green Version]
- Jeon, D. Latent tuberculosis infection: Recent progress and challenges in South Korea. Korean J. Intern. Med. 2020, 35, 269–275. [Google Scholar] [CrossRef]
- Ncayiyana, J.R.; Bassett, J.; West, N.; Westreich, D.; Musenge, E.; Emch, M.; Pettifor, A.; Hanrahan, C.F.; Schwartz, S.R.; Sanne, I.; et al. Prevalence of latent tuberculosis infection and predictive factors in an urban informal settlement in Johannesburg, South Africa: A cross-sectional study. BMC Infect. Dis. 2016, 16, 661. [Google Scholar] [CrossRef] [Green Version]
- Yeon, J.H.; Seong, H.; Hur, H.; Park, Y.; Kim, Y.A.; Park, Y.S.; Han, C.H.; Lee, S.M.; Seo, J.H.; Kang, J.G. Prevalence and risk factors of latent tuberculosis among Korean healthcare workers using whole-blood interferon-γ release assay. Sci. Rep. 2018, 8, 10113. [Google Scholar] [CrossRef]
- Castro, F.; Cardoso, A.P.; Gonçalves, R.M.; Serre, K.; Oliveira, M.J. Interferon-Gamma at the Crossroads of Tumor Immune Surveillance or Evasion. Front. Immunol. 2018, 9, 847. [Google Scholar] [CrossRef] [Green Version]
- Luetkemeyer, A.F.; Charlebois, E.D.; Flores, L.L.; Bangsberg, D.R.; Deeks, S.G.; Martin, J.N.; Havlir, D.V. Comparison of an interferon-gamma release assay with tuberculin skin testing in HIV-infected individuals. Am. J. Respir. Crit. Care Med. 2007, 175, 737–742. [Google Scholar] [CrossRef] [Green Version]
- Oni, T.; Gideon, H.P.; Bangani, N.; Tsekela, R.; Seldon, R.; Wood, K.; Wilkinson, K.A.; Goliath, R.T.; Ottenhoff, T.H.; Wilkinson, R.J. Risk factors associated with indeterminate gamma interferon responses in the assessment of latent tuberculosis infection in a high-incidence environment. Clin. Vaccine Immunol. 2012, 19, 1243–1247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.H.; Kwon, J.Y.; Kim, S.Y.; Jung, K.; Cho, M.L. Interferon-gamma regulates inflammatory cell death by targeting necroptosis in experimental autoimmune arthritis. Sci. Rep. 2017, 7, 10133. [Google Scholar] [CrossRef] [PubMed]
- Khalil, R.H.; Al-Humadi, N. Types of acute phase reactants and their importance in vaccination. Biomed. Rep. 2020, 12, 143–152. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.H.; Kang, J.M.; Ahn, J.G. Low-dose steroids are associated with indeterminate QuantiFERON-TB Gold In-Tube assay results in immunocompetent children. Sci. Rep. 2021, 11, 6468. [Google Scholar] [CrossRef] [PubMed]
- Kobashi, Y.; Sugiu, T.; Mouri, K.; Obase, Y.; Miyashita, N.; Oka, M. Indeterminate results of QuantiFERON TB-2G test performed in routine clinical practice. Eur. Respir. J. 2009, 33, 812–815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| QFT-GIT Group (n = 177) | QFT-PLUS Group (n = 231) | p-Value | |
|---|---|---|---|
| Demographics | |||
| Age (years), mean ± SD | 48.9 ± 15.4 | 47.8 ± 15.0 | 0.473 |
| Sex, n (%) | 0.036 | ||
| Female | 125 (70.6) | 140 (60.6) | |
| Male | 52 (29.4) | 91 (39.4) | |
| Primary diagnosis, n (%) | 0.052 | ||
| Rheumatoid arthritis | 81 (45.8) | 79 (34.2) | |
| Ankylosing spondylitis | 22 (12.4) | 48 (20.8) | |
| Behcet disease | 21 (11.9) | 33 (14.3) | |
| Systemic lupus erythematosus | 18 (10.2) | 23 (10.0) | |
| Adult-onset Still disease | 13 (7.3) | 6 (2.6) | |
| Systemic necrotizing vasculitis | 7 (4.0) | 17 (7.4) | |
| Psoriatic arthritis | 6 (3.4) | 12 (5.2) | |
| Dermatomyositis/polymyositis | 4 (2.3) | 4 (1.7) | |
| Polymyalgia rheumatica | 2 (1.1) | 3 (1.3) | |
| Systemic sclerosis | 2 (1.1) | 2 (0.9) | |
| IgG4-related disease | 1 (0.6) | 4 (1.7) | |
| Laboratory data, mean ± SD | |||
| White blood cell count (/mm3) | 7661.6 ± 3921.2 | 7765.2 ± 3611.6 | 0.782 |
| Neutrophil count (/mm3) | 5222.2 ± 3347.4 | 5396.9 ± 4092.6 | 0.636 |
| Lymphocyte count (/mm3) | 1621.8 ± 976.2 | 1705.8 ± 920.0 | 0.374 |
| Hemoglobin (g/dL) | 12.4 ± 1.9 | 12.6 ± 2.0 | 0.221 |
| Platelet count (×1000/mm3) | 276.6 ± 120.1 | 286.5 ± 105.1 | 0.378 |
| Blood urea nitrogen (mg/dL) | 16.1 ± 9.2 | 16.9 ± 12.9 | 0.462 |
| Creatinine (mg/dL) | 0.9 ± 1.4 | 0.9 ± 0.9 | 0.557 |
| Albumin (mg/dL) | 3.9 ± 0.5 | 4.0 ± 0.6 | 0.751 |
| Aspartate aminotransferase (IU/L) | 22.4 ± 13.3 | 29.0 ± 80.5 | 0.219 |
| Alanine aminotransferase (IU/L) | 19.7 ± 16.4 | 24.6 ± 36.7 | 0.072 |
| Erythrocyte sedimentation rate (mm/h) | 49.1 ± 37.1 | 38.5 ± 32.4 | 0.002 |
| C-reactive protein (mg/L) | 23.7 ± 46.1 | 21.8 ± 42.9 | 0.681 |
| IGRA results, n (%) | 0.226 | ||
| Indeterminate | 4 (2.3) | 7 (3.0) | |
| Positive | 44 (24.9) | 40 (17.3) | |
| Negative | 129 (72.9) | 184 (79.7) |
| Medications, n (%) | QFT-GIT Group (n = 177) | QFT-PLUS Group (n = 231) | p-Value |
|---|---|---|---|
| Glucocorticoid | 0.040 | ||
| No | 76 (42.9) | 124 (53.7) | |
| Yes | 101 (57.1) | 107 (46.3) | |
| Methotrexate | 0.241 | ||
| No | 104 (58.8) | 150 (64.9) | |
| Yes | 73 (41.2) | 81 (35.1) | |
| Hydroxychloroquine | 0.459 | ||
| No | 157 (88.7) | 198 (85.7) | |
| Yes | 20 (11.3) | 33 (14.3) | |
| Sulfasalazine | 0.452 | ||
| No | 131 (74.0) | 162 (70.1) | |
| Yes | 46 (26.0) | 69 (29.9) | |
| Tacrolimus | 0.028 | ||
| No | 162 (91.5) | 224 (97.0) | |
| Yes | 15 (8.5) | 7 (3.0) | |
| Leflunomide | 1.000 | ||
| No | 151 (85.3) | 197 (85.3) | |
| Yes | 26 (14.7) | 34 (14.7) | |
| 5-acetylsalicylic acid | 0.798 | ||
| No | 166 (93.8) | 214 (92.6) | |
| Yes | 11 (6.2) | 17 (7.4) | |
| Azathioprine | 0.524 | ||
| No | 171 (96.6) | 219 (94.8) | |
| Yes | 6 (3.4) | 12 (5.2) | |
| Mycophenolate mofetil | 1.000 | ||
| No | 172 (97.2) | 224 (97.0) | |
| Yes | 5 (2.8) | 7 (3.0) | |
| Cyclophosphamide | 1.000 | ||
| No | 176 (99.4) | 230 (99.6) | |
| Yes | 1 (0.6) | 1 (0.4) | |
| Cyclosporine | 1.000 | ||
| No | 174 (98.3) | 228 (98.7) | |
| Yes | 3 (1.7) | 3 (1.3) | |
| bDMARDs/tsDMARDs | 0.353 | ||
| No | 162 (91.5) | 218 (94.4) | |
| Yes | 15 (8.5) | 13 (5.6) |
| QFT-GIT (RD) (n = 177) | QFT-PLUS (RD) (n = 231) | QFT-GIT (HC) (n = 2511) | QFT-PLUS (HC) (n = 1614) | p-Value | |
|---|---|---|---|---|---|
| IGRA results, n (%) | <0.001 | ||||
| Indeterminate | 4 (2.3) | 7 (3.0) | 5 (0.2) | 4 (0.2) | |
| Positive/negative | 173 (97.7) | 224 (97.0) | 2506 (99.8) | 1610 (99.8) |
| Patient | Age | Sex | Diagnosis | Lymphocyte Count (/mm3) | Albumin (mg/dL) | ESR (mm/h) | CRP (mg/L) | Current Medication Usage | IGRA Test | IFN-γ Level in Nil Tube | IFN-γ Level in Mitogen Tube |
|---|---|---|---|---|---|---|---|---|---|---|---|
| #1 | 49 | F | DM | 71 | 2.6 | 25 | 40.3 | mPD 40 mg, TAC, RTX | QFT-GIT | 0.04 | 0.06 |
| #2 | 48 | F | DM | 640 | 3.5 | 95 | 47.9 | mPD 12 mg, MMF, HCQ | QFT-PLUS | 0.15 | 0.43 |
| #3 | 68 | M | DM | 710 | 2.7 | 16 | 8.8 | PL 10 mg | QFT-PLUS | 0.02 | 0.12 |
| #4 | 7 | M | RA | 1330 | 3.6 | 31 | 57.6 | PL 20 mg | QFT-GIT | 0.08 | 0.29 |
| #5 | 54 | F | RA | 1460 | 3.7 | 120 | 36.7 | MTX, HCQ | QFT-GIT | 0.04 | 0.06 |
| #6 | 69 | F | RA | 720 | 2.3 | 120 | 341.1 | None | QFT-PLUS | 0.04 | 0.44 |
| #7 | 39 | F | SLE | 650 | 2.6 | 57 | 62.3 | None | QFT-GIT | 0.95 | 1.07 |
| #8 | 36 | F | SLE | 30 | 2.9 | 24 | 35.6 | PL 50 mg, HCQ | QFT-PLUS | ≥10 | ≥10 |
| #9 | 37 | F | SLE | 810 | 3.9 | 120 | 31.1 | mPD 62.5 mg | QFT-PLUS | 0.09 | 0.25 |
| #10 | 31 | M | SLE | 1830 | 4.5 | 17 | 0.3 | mPD 4 mg, MMF | QFT-PLUS | ≥10 | ≥10 |
| #11 | 47 | F | SLE | 260 | 2.2 | 116 | 114 | PL 30 mg, MMF | QFT-PLUS | 0.1 | 0.25 |
| Univariate Analysis | Multivariate Analysis ‡ | |||||
|---|---|---|---|---|---|---|
| Variables | HR | 95% CI | p-Value | HR | 95% CI | p-Value |
| Age | 0.982 | 0.944, 1.021 | 0.353 | |||
| Female sex | 0.688 | 0.180, 2.636 | 0.586 | |||
| White blood cell count | 1.000 | 1.000, 1.000 | 0.461 | |||
| Neutrophil count | 1.000 | 1.000, 1.000 | 0.109 | |||
| Lymphocyte count | 0.998 | 0.996, 0.999 | <0.001 | 0.998 | 0.997, 1.000 | 0.012 |
| Hemoglobin | 0.592 | 0.442, 0.793 | <0.001 | |||
| Platelet count | 0.992 | 0.985, 0.998 | 0.013 | |||
| Blood urea nitrogen | 1.013 | 0.976, 1.053 | 0.492 | |||
| Creatinine | 0.936 | 0.483, 1.812 | 0.844 | |||
| Albumin | 0.220 | 0.105, 0.463 | <0.001 | 0.366 | 0.150, 0.890 | 0.027 |
| Aspartate aminotransferase | 1.013 | 0.998, 1.027 | 0.081 | |||
| Alanine aminotransferase | 1.011 | 1.003, 1.019 | 0.009 | |||
| Erythrocyte sedimentation rate | 1.018 | 1.002, 1.034 | 0.026 | |||
| C-reactive protein | 1.010 | 1.004, 1.017 | 0.002 | |||
| Glucocorticoid usage | 2.627 | 0.687, 10.046 | 0.158 | |||
| Immunosuppressive agent usage | 0.372 | 0.111, 1.247 | 0.109 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, S.S.; Kim, H.W.; Park, Y. Frequency and Factors of Indeterminate QuantiFERON-TB Gold In-Tube and QuantiFERON-TB Gold PLUS Test Results in Rheumatic Diseases. J. Clin. Med. 2021, 10, 4357. https://doi.org/10.3390/jcm10194357
Ahn SS, Kim HW, Park Y. Frequency and Factors of Indeterminate QuantiFERON-TB Gold In-Tube and QuantiFERON-TB Gold PLUS Test Results in Rheumatic Diseases. Journal of Clinical Medicine. 2021; 10(19):4357. https://doi.org/10.3390/jcm10194357
Chicago/Turabian StyleAhn, Sung Soo, Hyung Woo Kim, and Younhee Park. 2021. "Frequency and Factors of Indeterminate QuantiFERON-TB Gold In-Tube and QuantiFERON-TB Gold PLUS Test Results in Rheumatic Diseases" Journal of Clinical Medicine 10, no. 19: 4357. https://doi.org/10.3390/jcm10194357
APA StyleAhn, S. S., Kim, H. W., & Park, Y. (2021). Frequency and Factors of Indeterminate QuantiFERON-TB Gold In-Tube and QuantiFERON-TB Gold PLUS Test Results in Rheumatic Diseases. Journal of Clinical Medicine, 10(19), 4357. https://doi.org/10.3390/jcm10194357






