Acute Hypoxemic Respiratory Failure in Children at the Start of COVID-19 Outbreak: A Nationwide Experience
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design and Patients
2.2. Data Collection
2.3. General Management
2.4. Statistical Analysis
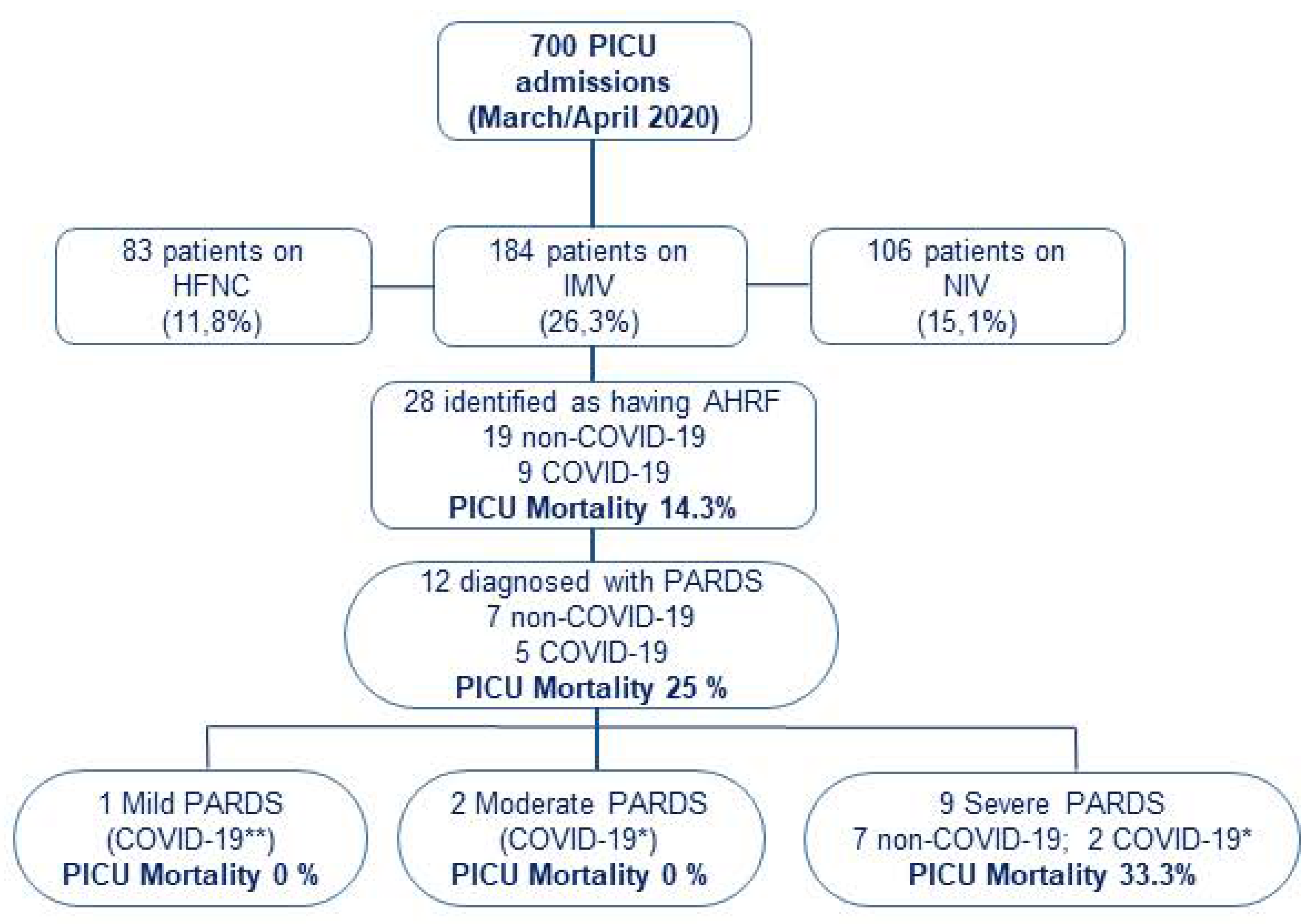
3. Results
3.1. Patient Characteristics
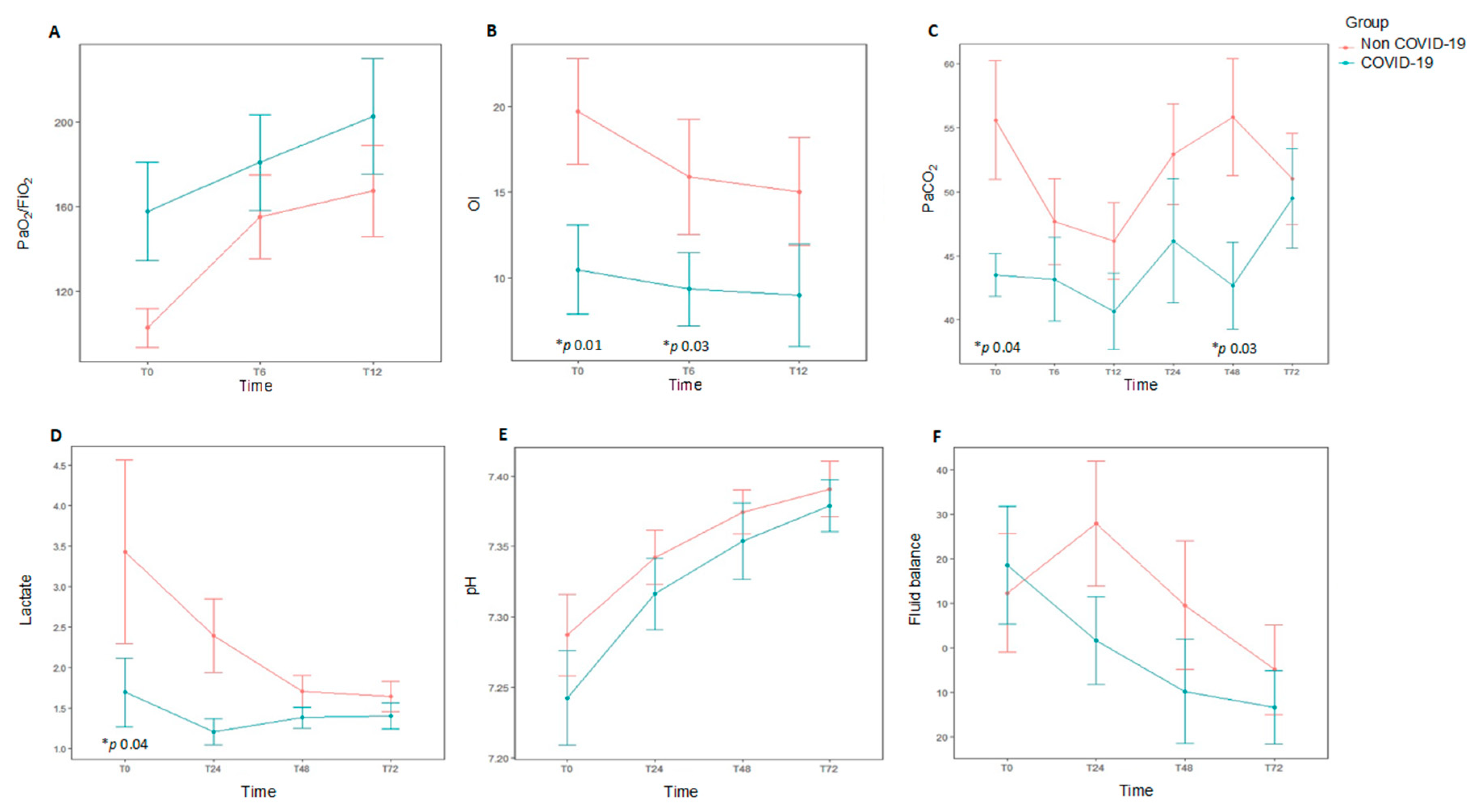
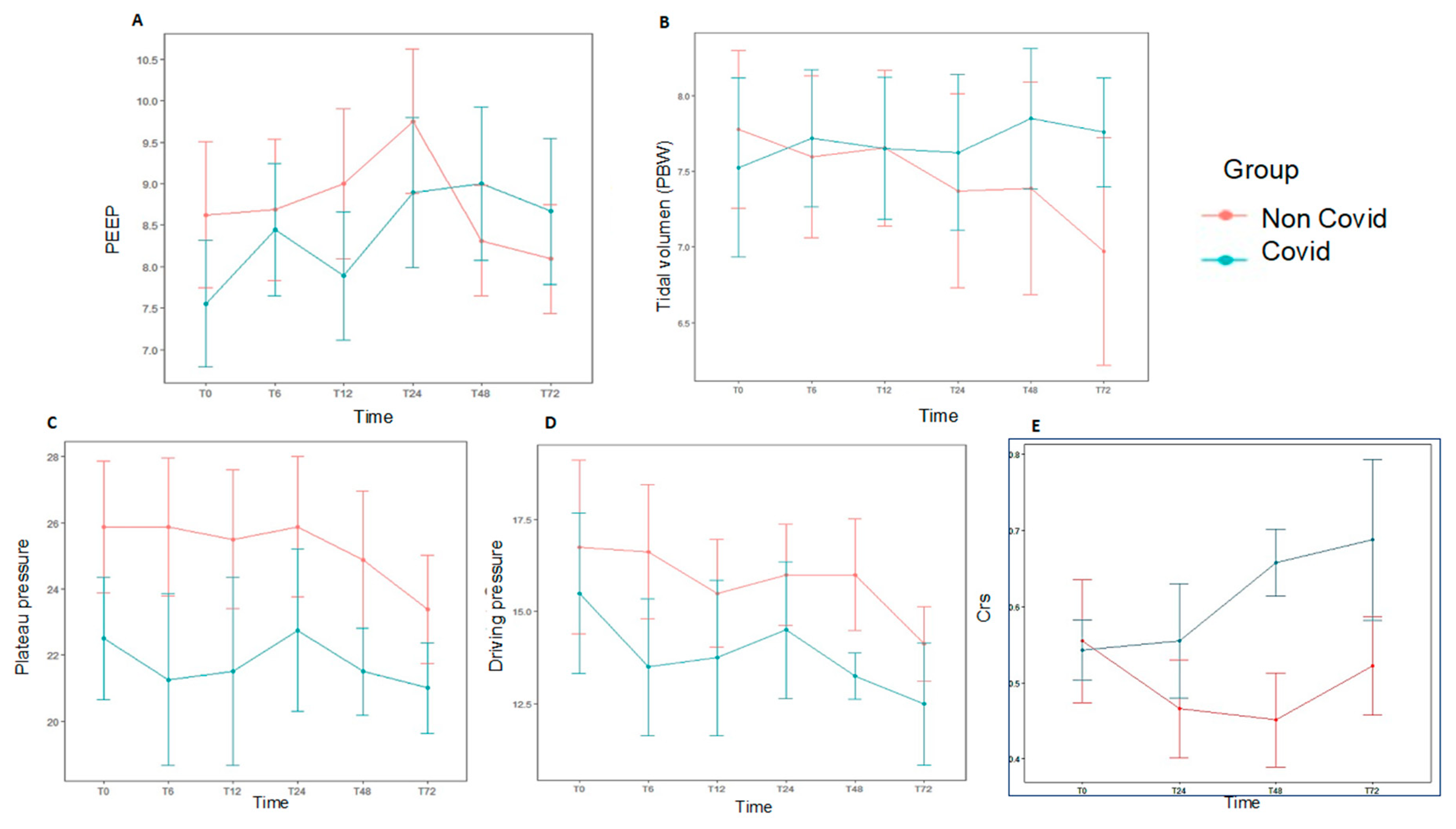
3.2. Ventilatory Settings and Adjunctive Measures
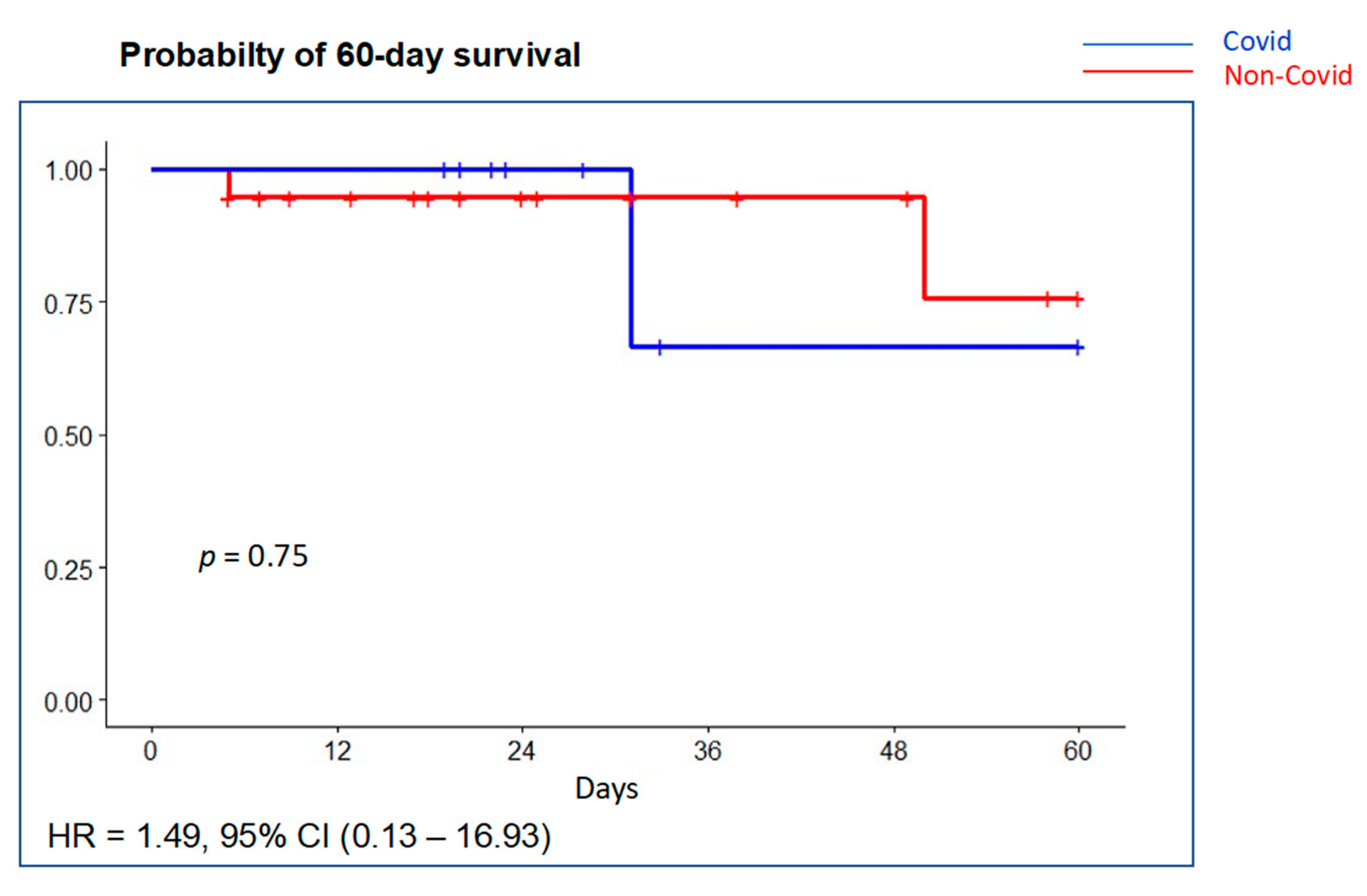
3.3. Clinical Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Members of the PANDORA-CHILD Network
References
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- World Health Organisation. Timeline: WHO’s COVID-19 Response. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed on 21 February 2021).
- Lu, X.; Zhang, L.; Du, H.; Zhang, J.; Li, Y.Y.; Qu, J.; Zhang, W.; Wang, Y.; Bao, S.; Li, Y.; et al. SARS-CoV-2 Infection in Children. N. Engl. J. Med. 2020, 382, 1663–1665. [Google Scholar] [CrossRef] [Green Version]
- Dong, Y.; Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; Jiang, Z.; Tong, S.; Tong, S.; et al. Epidemiology of COVID-19 among children in China. Pediatrics 2020, 145, e20200702. [Google Scholar] [CrossRef] [Green Version]
- World Health Organisation. Multisystem Inflammatory Syndrome in Children and Adolescents with COVID-19. Available online: https://www.who.int/publications/i/item/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-COVID-19 (accessed on 21 February 2021).
- Riphagen, S.; Gomez, X.; Gonzalez-Martinez, C.; Wilkinson, N.; Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020, 395, 1607–1608. [Google Scholar] [CrossRef]
- Whittaker, E.; Bamford, A.; Kenny, J.; Kaforou, M.; Jones, C.E.; Shah, P.; Ramnarayan, P.; Fraisse, A.; Miller, O.; Davies, P.; et al. Clinical Characteristics of 58 Children with a Pediatric Inflammatory Multisystem Syndrome Temporally Associated with SARS-CoV-2. JAMA 2020, 324, 259–269. [Google Scholar] [CrossRef]
- García-Salido, A.; de Carlos Vicente, J.C.; Belda Hofheinz, S.; Balcells Ramírez, J.; Slöcker Barrio, M.; Leóz Gordillo, I.; Hernández Yuste, A.; Guitart Pardellans, C.; Cuervas-Mons Tejedor, M.; Huidobro Labarga, B.; et al. Severe manifestations of SARS-CoV-2 in children and adolescents: From COVID-19 pneumonia to multisystem inflammatory syndrome: A multicentre study in pediatric intensive care units in Spain. Crit. Care 2020, 24, 666. [Google Scholar] [CrossRef] [PubMed]
- Swann, O.V.; Holden, K.A.; Turtle, L.; Pollock, L.; Fairfield, C.J.; Drake, T.M.; Seth, S.; Egan, C.; Hardwick, H.E.; Halpin, S.; et al. Clinical characteristics of children and young people admitted to hospital with COVID-19 in United Kingdom: Prospective multicentre observational cohort study. BMJ 2020, 370, m3249. [Google Scholar] [CrossRef]
- Feldstein, L.R.; Tenforde, M.W.; Friedman, K.G.; Newhams, M.; Rose, E.B.; Dapul, H.; Soma, V.L.; Maddux, A.B.; Mourani, P.M.; Bowens, C.; et al. Characteristics and Outcomes of US Children and Adolescents with Multisystem Inflammatory Syndrome in Children (MIS-C) Compared with Severe Acute COVID-19. JAMA 2021, 325, 1074. [Google Scholar] [CrossRef]
- Dufort, E.M.; Koumans, E.H.; Chow, E.J.; Rosenthal, E.M.; Muse, A.; Rowlands, J.; Barranco, M.A.; Maxted, A.M.; Rosenberg, E.S.; Easton, D.; et al. Multisystem Inflammatory Syndrome in Children in New York State. N. Engl. J. Med. 2020, 383, 347–358. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Grasselli, G.; Tonetti, T.; Protti, A.; Langer, T.; Girardis, M.; Bellani, G.; Laffey, J.; Carrafiello, G.; Carsana, L.; Rizzuto, C.; et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: A multicentre prospective observational study. Lancet Respir. Med. 2020, 8, 1201–1218. [Google Scholar] [CrossRef]
- Ferrando, C.; Suarez-Sipmann, F.; Mellado-Artigas, R.; Hernández, M.; Gea, A.; Arruti, E.; Aldecoa, C.; Martínez-Pallí, G.; Martínez-González, M.A.; Slutsky, A.S.; et al. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med. 2020, 46, 2200–2211. [Google Scholar] [CrossRef]
- Spanish National Statistics Institute. 2020 Census Data. Available online: https://www.ine.es/jaxiT3/Tabla.htm?t=31304 (accessed on 31 January 2021).
- World Health Organisation. Spain: WHO Coronavirus Disease (COVI-19) Dashboard. Available online: https://COVID19.who.int/region/euro/country/es (accessed on 15 February 2021).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [Green Version]
- Khemani, R.G.; Thomas, N.J.; Venkatachalam, V.; Scimeme, J.P.; Berutti, T.; Schneider, J.B.; Ross, P.A.; Willson, D.F.; Hall, M.W.; Newth, C.J.L.; et al. Comparison of SF ratio with PF ratio based markers of lung disease severity for children with acute lung injury. Crit. Care Med. 2012, 40, 1309–1316. [Google Scholar] [CrossRef]
- Martin, D.C.; Richards, G.N. Predicted body weight relationships for protective ventilation-unisex proposals from pre-term through to adult. BMC Pulm. Med. 2017, 17, 85. [Google Scholar] [CrossRef] [Green Version]
- Amato, M.B.P.; Meade, M.O.; Slutsky, A.S.; Brochard, L.; Costa, E.L.V.; Schoenfeld, D.A.; Stewart, T.E.; Briel, M.; Talmor, D.; Mercat, A.; et al. Driving Pressure and Survival in the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2015, 372, 747–755. [Google Scholar] [CrossRef] [Green Version]
- Khemani, R.G.; Smith, L.S.; Zimmerman, J.J.; Erickson, S.; Pediatric Acute Lung Injury Consensus Conference Group. Pediatric acute respiratory distress syndrome: Definition, incidence, and epidemiology: Proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatric Crit. Care Med. 2015, 16 (Suppl. S5), S23–S40. [Google Scholar] [CrossRef]
- Guidance: Paediatric Multisystem Inflammatory Syndrome Temporally Associated with COVID-19. Available online: https://www.rcpch.ac.uk/resources/paediatric-multisystem-inflammatory-syndrome-temporally-associated-COVID-19-pims-guidance (accessed on 15 February 2021).
- Pollack, M.M.; Patel, K.M.; Ruttimann, U.E. PRISM III: An updated Pediatric Risk of Mortality Score. Crit. Care Med. 1996, 24, 743–752. [Google Scholar] [CrossRef]
- Leteurtre, S.; Duhamel, A.; Salleron, J.; Grandbastien, B.; Lacroix, J.; Leclerc, F. PELOD-2: An update of the PEdiatric logistic organ dysfunction score. Crit. Care Med. 2013, 41, 1761–1773. [Google Scholar] [CrossRef]
- Yehya, N.; Harhay, M.O.; Curley, M.A.Q.; Schoenfeld, D.A.; Reeder, R.W. Reappraisal of ventilator-free days in critical care research. Am. J. Respir. Crit. Care Med. 2019, 200, 828–836. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Consumo y Bienestar Social—Profesionales—Situación Actual Coronavirus. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/situacionActual (accessed on 25 February 2021).
- González Cortés, R.; García-Salido, A.; Roca Pascual, D.; Slöcker Barrio, M.; de Carlos Vicente, J.C.; Bustinza Arriortua, A.; López-Herce Cid, J.; Cuervas-Mons Tejedor, M.; Oyágüez Ugidos, P.P.; Jordan, I.; et al. A multicenter national survey of children with SARS-CoV-2 infection admitted to Spanish Pediatric Intensive Care Units. Intensive Care Med. 2020, 46, 1774–1776. [Google Scholar] [CrossRef]
- Wang, F.; Lai, C.X.; Huang, P.Y.; Liu, J.M.; Wang, X.F.; Tang, Q.Y.; Zhou, X.; Xian, W.J.; Chen, R.K.; Li, X.; et al. Comparison of Clinical Characteristics and Outcomes of Pediatric and Adult Patients with Coronavirus Disease 2019 in Shenzhen, China. Biomed. Environ. Sci. 2020, 33, 906–915. [Google Scholar] [CrossRef]
- Shekerdemian, L.S.; Mahmood, N.R.; Wolfe, K.K.; Riggs, B.J.; Ross, C.E.; McKiernan, C.A.; Heidemann, S.M.; Kleinman, L.C.; Sen, A.I.; Hall, M.W.; et al. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020, 174, 868–873. [Google Scholar] [CrossRef]
- CDCMMWR. Coronavirus Disease 2019 in Children—United States, 12 February–2 April 2020. MMWR Morb Mortal Wkly Rep [Internet]; 2020. Available online: https://www.cdc.gov/mmwr/volumes/69/wr/mm6914e4.htm (accessed on 21 February 2021).
- López-Fernández, Y.; De Azagra, A.M.; De La Oliva, P.; Modesto, V.; Sánchez, J.I.; Parrilla, J.; Arroyo, M.J.; Reyes, S.B.; Pons-Ódena, M.; López-Herce, J.; et al. Pediatric acute lung injury epidemiology and natural history study: Incidence and outcome of the acute respiratory distress syndrome in children. Crit. Care Med. 2012, 40, 3238–3245. [Google Scholar] [CrossRef]
- Wong, J.J.M.; Tan, H.L.; Lee, S.W.; Chang, K.T.E.; Mok, Y.H.; Lee, J.H. Characteristics and trajectory of patients with pediatric acute respiratory distress syndrome. Pediatr. Pulmonol. 2020, 55, 1000–1006. [Google Scholar] [CrossRef]
- Rimensberger, P.C.; Kneyber, M.C.J.; Deep, A.; Bansal, M.; Hoskote, A.; Javouhey, E.; Jourdain, G.; Latten, L.; MacLaren, G.; Morin, L.; et al. Caring for Critically Ill Children with Suspected or Proven Coronavirus Disease 2019 Infection: Recommendations by the Scientific Sections’ Collaborative of the European Society of Pediatric and Neonatal Intensive Care. Pediatr. Crit. Care Med. 2021, 22, 56–67. [Google Scholar] [CrossRef]
- Khemani, R.G.; Smith, L.; Lopez-Fernandez, Y.M.; Kwok, J.; Morzov, R.; Klein, M.J.; Yehya, N.; Willson, D.; Kneyber, M.C.J.; Lillie, J.; et al. Paediatric acute respiratory distress syndrome incidence and epidemiology (PARDIE): An international, observational study. Lancet Respir. Med. 2019, 7, 115–128. [Google Scholar] [CrossRef]
- Girona-Alarcon, M.; Bobillo-Perez, S.; Sole-Ribalta, A.; Hernandez, L.; Guitart, C.; Suarez, R.; Balaguer, M.; Cambra, F.J.; Jordan, I. The different manifestations of COVID-19 in adults and children: A cohort study in an intensive care unit. BMC Infect. Dis. 2021, 21, 87. [Google Scholar] [CrossRef]
- Duarte-Salles, T.; Vizcaya, D.; Pistillo, A.; Casajust, P.; Sena, A.G.; Lai, L.Y.H.; Prats-Uribe, A.; Ahmed, W.-U.-R.; Alshammari, T.M.; Alghoul, H.; et al. Baseline Characteristics, Management, and Outcomes of 55,270 Children and Adolescents Diagnosed with COVID-19 and 1,952,693 with Influenza in France, Germany, Spain, South Korea and the United States: An International Network Cohort Study. medRxiv 2020. [Google Scholar] [CrossRef]
- Götzinger, F.; Santiago-García, B.; Noguera-Julián, A.; Lanaspa, M.; Lancella, L.; Calò Carducci, F.I.; Gabrovska, N.; Velizarova, S.; Prunk, P.; Osterman, V.; et al. COVID-19 in children and adolescents in Europe: A multinational, multicentre cohort study. Lancet Child Adolesc. Heal. 2020, 4, 653–661. [Google Scholar] [CrossRef]
- Gattinoni, L.; Chiumello, D.; Rossi, S. COVID-19 pneumonia: ARDS or not? Crit. Care 2020, 24, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Non-COVID n = 19 | COVID-19 n = 9 | Total n = 28 | p Value | |
|---|---|---|---|---|
| Demographics | ||||
| Age, median (P25–P75), mo | 15 (3–84) | 106 (6–122) | 26 (4.75–108) | 0.168 |
| Males/females (% males) | 10/9 (52.6) | 8/1 (88.9) | 18/10 (64.3) | 0.098 |
| Weight, Kg | 10 (4.05–23.5) | 37(7.4–42) | 11.1 (6.3–34.5) | 0.061 |
| PBW, Kg | 10.4 (3.95–23) | 32.3 (7.5–38.8) | 13 (5.9–32.75) | 0.140 |
| Comorbidities | ||||
| Any comorbidity | 15 (78.9%) | 4 (44.4%) | 19 (67.8%) | 0.097 |
| Chronic neurologic disease | 6 (31.6%) | 0 | 6 (21.4%) | 0.136 |
| Congenital heart disease | 3 (15.8%) | 0 | 3 (10.7%) | 0.530 |
| Cancer | 3 (15.8%) | 0 | 3 (10.7%) | 0.530 |
| Immune suppression | 3 (15.8%) | 2 (22.2%) | 5 (17.8%) | 1 |
| Chronic lung disease | 3 (15.8%) | 2 (22.2%) | 5 (17.8%) | 1 |
| Prematurity | 4 (21%) | 0 | 4 (14.3%) | 0.273 |
| Other | 0 | 1 (11.1%) | 1 (3.6%) | 0.321 |
| Etiological factor of AHRF | ||||
| Pneumonia or LRTI | 8 (42.1%) | 6 (66.7%) | 14 (50%) | 0.420 |
| Sepsis/septic shock | 3 (15.8%) | 1 (11.1%) | 4 (14.3%) | 1 |
| Non-septic shock | 0 | 1 (11.1%) | 1 (3.6%) | 0.321 |
| Neurologic dysfunction | 3 (15.8%) | 1 (11.1%) | 4 (14.3%) | 1 |
| Surgery | 2 (10.5%) | 0 | 2 (7.1%) | 1 |
| Aspiration | 2 (10.5%) | 0 | 2 (7.1%) | 1 |
| Drowning | 1 (5.3%) | 0 | 1 (3.6%) | 1 |
| Time from PICU admission to intubation | 0.769 | |||
| <24 h | 11(57.9%) | 4 (44.4%) | 15 (53.6%) | |
| 24–48 h | 5 (26.3%) | 4 (44.4%) | 9 (32.1%) | |
| >48 h | 3(15.8%) | 1(11.2%) | 4(14.3%) | |
| Severity of illness | ||||
| PRISM III | 7 (3–17) | 7 (2–11) | 7 (3–16) | 0.693 |
| PELOD 2 | 5 (4.5–9) | 6 (6–7) | 6 (4.7–7.5) | 0.941 |
| On vasoactive medication * | 13 (68.4%) | 7 (77.8%) | 20 (71.4%) | |
| Inotropic Score | 49 (15–57.5) | 50 (30.5–83.0) | 49.5 (20.2–65.6) | 0.781 |
| Prior respiratory support | ||||
| HFNC | 4 (21.1%) | 4 (44.4%) | 8 (28.6%) | 0.371 |
| NIV | 9 (47.4%) | 2 (22.2%) | 11 (39.3%) | 0.249 |
| Oxigenation at onset | ||||
| PaO2/FiO2 ** | 95 (65.5–133) | 150 (105–220) | 106 (66–150) | 0.046 |
| Oxygenation index ** | 15.9 (11–28.4) | 9.3 (6.7–10.6) | 11.2 (8.8–23.9) | 0.01 |
| PALICC groups, % | 7/19 (36.8%) | 5/9 (55.5%) | 12/28 (42.8%) | 0.045 |
| Mild | 0 | 1 (11.1%) | 1 (3.6%) | |
| Moderate | 0 | 2(22.2%) | 2 (7.1%) | |
| Severe | 7 (36.8%) | 2(22.2%) | 9 (32.1%) | |
| Length of stay, days | ||||
| PICU | 16 (11–26) | 19 (12–23) | 16.5 (12–26) | 0.902 |
| Hospital | 24 (15–49.5) | 23 (22–31) | 23.5 (19–41) | 0.749 |
| At Study Entry | Day 1 | Day 2 | Day 3 | |
|---|---|---|---|---|
| pH | ||||
| Non-COVID-19 (n = 14) | 7.29 (7.28, 7.37) | 7.34 (7.3, 7.38) | 7.37 (7.34, 7.42) | 7.39 (7.32, 7.44) |
| COVID-19 (n = 8) | 7.24 (7.22, 7.31) | 7.32 (7.26, 7.37) | 7.35 (7.31, 7.4) | 7.38 (7.34, 7.42) |
| Mean difference (CI 95%) | −0.04 (−0.11, 0.02) | −0.03 (−0.09, 0.04) | −0.02 (−0.09, 0.04) | −0.01 (−0.08, 0.05) |
| p value | 0.18 | 0.44 | 0.54 | 0.72 |
| PaCO2, mm Hg | ||||
| Non-COVID-19 (n = 13) | 56 (48, 71) | 53 (40, 61) | 56 (43, 59) | 51 (43, 57) |
| COVID-19 (n = 6) | 43.5 (40, 46) | 46 (39, 55) | 43 (39.5, 46) | 49.5 (43, 56) |
| Mean difference (CI 95%) | −12.2 (−23.7, −0.5) | −6.8 (−18.3, 4.8) | −13.2 (−24.8, 1.6) | −1.5 (−13.1, 10.1) |
| p value | 0.04 | 0.25 | 0.03 | 0.8 |
| Lactate (mmol/L) | ||||
| Non-COVID-19 (n = 17) | 3.4 (1.2–2.7) | 2.4 (1.3–2.6) | 1.7 (1.1, 2.1) | 1.6 (1–2.1) |
| COVID-19 (n = 9) | 1.7 (0.8–2.1) | 1.2 (1–1.3) | 1.4 (1.2–1.7) | 1.4 (1.2–1.7) |
| Mean difference (CI 95%) | −1.7 (−3.4, −0.1) | −1.2 (−2.9, 0.5) | −0.3 (−2–1.3) | −0.2 (−1.9, 1.4) |
| p value | 0.04 | 0.16 | 0.71 | 0.78 |
| Fluid balance (mL/Kg) | ||||
| Non-COVID-19 (n = 9) | 12.4 (−21, 26) | 27.9 (−0.2, 22.8) | 9.6 (−13.5, 19.6) | −4.8 (−16.7, 4) |
| COVID-19 (n = 8) | 18.6 (6.5, 44.4) | 1.6 (−10.9, 27.5) | −9.8 (−20.5, 7.5) | −13.4 (−15.8, −1.8) |
| Mean difference (CI 95%) | 6.2 (−25.6, 38.05) | −26.3 (−58.1, 5.5) | −19.4 (−51.2, 12.4) | −8.6 (−40.4, 23.2) |
| p value | 0.7 | 0.11 | 0.23 | 0.6 |
| Non-COVID-19 (n = 19) | COVID-19 (n = 9) | All (n = 28) | p Value | |
|---|---|---|---|---|
| Neuromuscular blockade * | ||||
| At study entry | 12/19 (67.9%) | 4/9 (44.4%) | 16/28 (57.1%) | 0.432 |
| Day 1 | 10/18 (55.6%) | 8/9 (88.9%) | 18/27 (66.7%) | 0.193 |
| Day 2 | 10/18 (55.6%) | 7/9 (77.8%) | 17/27 (63%) | 0.406 |
| Day 3 | 8/17 (47.1%) | 5/9 (55.6%) | 13/26 (50%) | 1 |
| Prone positioning | 3/19 (15.8%) | 3/9 (33.3%) | 6/28 (21.4%) | 0.352 |
| Inhaled nitric oxide | 6/19 (31.6%) | 1/9 (11.1%) | 7/28 (25%) | 0.371 |
| ECMO | 2/19 (10.5%) | 1/9 (11.1%) | 3/28 (10.7%) | 1 |
| Corticosteroids | 11/19 (57.9%) | 8/9 (88.9%) | 19/28 (67.9%) | 0.195 |
| Non-COVID-19 (n = 19) | COVID-19 (n = 9) | All (n = 28) | p Value | |
|---|---|---|---|---|
| Pneumothorax after initiating mechanical ventilation | 2 (10.5%) | 1 (11.1%) | 3 (10.7%) | 1 |
| PICU mortality | 2 (10.5%) | 2 (22.2%) | 4 (14.3%) | 0.574 |
| Hospital mortality | 3 (15.8%) | 2 (22.2%) | 5 (17.9%) | 1 |
| Ventilator-free days | (18–24) | 21 (5.5–23) | 19 (5.5–24) | 0.749 |
| PICU length of stay, days | 16 (11–26) | 19 (12–23) | 16.5 (12–26) | 0.902 |
| Hospital length of stay, days | 24 (15–49.5) | 23 (22–31) | 23.5 (9–41) | 0.749 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Fernández, Y.M.; Martínez-de-Azagra, A.; González-Gómez, J.M.; Pérez-Caballero Macarrón, C.; García-González, M.; Parrilla-Parrilla, J.; Miñambres-Rodríguez, M.; Madurga-Revilla, P.; Gómez-Zamora, A.; Rodríguez-Campoy, P.; et al. Acute Hypoxemic Respiratory Failure in Children at the Start of COVID-19 Outbreak: A Nationwide Experience. J. Clin. Med. 2021, 10, 4301. https://doi.org/10.3390/jcm10194301
López-Fernández YM, Martínez-de-Azagra A, González-Gómez JM, Pérez-Caballero Macarrón C, García-González M, Parrilla-Parrilla J, Miñambres-Rodríguez M, Madurga-Revilla P, Gómez-Zamora A, Rodríguez-Campoy P, et al. Acute Hypoxemic Respiratory Failure in Children at the Start of COVID-19 Outbreak: A Nationwide Experience. Journal of Clinical Medicine. 2021; 10(19):4301. https://doi.org/10.3390/jcm10194301
Chicago/Turabian StyleLópez-Fernández, Yolanda M., Amelia Martínez-de-Azagra, José M. González-Gómez, César Pérez-Caballero Macarrón, María García-González, Julio Parrilla-Parrilla, María Miñambres-Rodríguez, Paula Madurga-Revilla, Ana Gómez-Zamora, Patricia Rodríguez-Campoy, and et al. 2021. "Acute Hypoxemic Respiratory Failure in Children at the Start of COVID-19 Outbreak: A Nationwide Experience" Journal of Clinical Medicine 10, no. 19: 4301. https://doi.org/10.3390/jcm10194301
APA StyleLópez-Fernández, Y. M., Martínez-de-Azagra, A., González-Gómez, J. M., Pérez-Caballero Macarrón, C., García-González, M., Parrilla-Parrilla, J., Miñambres-Rodríguez, M., Madurga-Revilla, P., Gómez-Zamora, A., Rodríguez-Campoy, P., Mayordomo-Colunga, J., Butragueño-Laiseca, L., Núñez-Borrero, R., González-Martín, J. M., Slutsky, A. S., Villar, J., & on behalf the Prevalence and Outcome of Acute Hypoxemic Respiratory Failure in Children (PANDORA-CHILD) Network. (2021). Acute Hypoxemic Respiratory Failure in Children at the Start of COVID-19 Outbreak: A Nationwide Experience. Journal of Clinical Medicine, 10(19), 4301. https://doi.org/10.3390/jcm10194301







