Initial Results after the Implementation of an Edge-To-Edge Transcatheter Tricuspid Valve Repair Program
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection and Follow-Up
2.2. Study Endpoints and Definitions
2.3. Statistical Analysis
3. Results
3.1. Patient Population
3.2. Procedural Results
3.3. Clinical Outcomes at Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Taramasso, M.; Gavazzoni, M.; Pozzoli, A.; Dreyfus, G.D.; Bolling, S.F.; George, I.; Kapos, I.; Tanner, F.C.; Zuber, M.; Maisano, F.; et al. Tricuspid regurgitation: Predicting the need for intervention, procedural success, and recurrence of disease. JACC Cardiovasc. Imaging 2019, 12, 605–621. [Google Scholar] [CrossRef]
- Orban, M.; Rommel, K.P.; Ho, E.C.; Unterhuber, M.; Pozzoli, A.; Connelly, K.A.; Deseive, S.; Besler, C.; Ong, G.; Braun, D.; et al. Transcatheter edge-to-edge tricuspid repair for severe tricuspid regurgitation reduces hospitalizations for heart failure. JACC Hear. Fail. 2020, 8, 265–276. [Google Scholar] [CrossRef]
- Prihadi, E.A.; Delgado, V.; Leon, M.B.; Enriquez-Sarano, M.; Topilsky, Y.; Bax, J.J. Morphologic types of tricuspid regurgitation: Characteristics and prognostic implications. JACC Cardiovasc. Imaging 2019, 12, 491–499. [Google Scholar] [CrossRef]
- LaPar, D.J.; Likosky, D.S.; Zhang, M.; Theurer, P.; Fonner, C.E.; Kern, J.A.; Bolling, S.F.; Drake, D.H.; Speir, A.M.; Rich, J.B.; et al. Development of a risk prediction model and clinical risk score for isolated tricuspid valve surgery. Ann. Thorac. Surg. 2018, 106, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Lurz, P.; Stephan von Bardeleben, R.; Weber, M.; Sitges, M.; Sorajja, P.; Hausleiter, J.; Denti, P.; Trochu, J.N.; Nabauer, M.; Tang, G.H.L.; et al. Transcatheter edge-to-edge repair for treatment of tricuspid regurgitation. J. Am. Coll. Cardiol. 2021, 77, 229–239. [Google Scholar] [CrossRef]
- Nickenig, G.; Weber, M.; Lurz, P.; von Bardeleben, R.S.; Sitges, M.; Sorajja, P.; Hausleiter, J.; Denti, P.; Trochu, J.N.; Näbauer, M.; et al. Transcatheter edge-to-edge repair for reduction of tricuspid regurgitation: 6-month outcomes of the TRILUMINATE single-arm study. Lancet 2019, 394, 2002–2011. [Google Scholar] [CrossRef]
- Fam, N.; Ali, F.; Hassanin, M.; Ong, G. Transcatheter tricuspid valve repair with the modified TriClip/MitraClip G4 system. EuroIntervention 2021, 17, e441–e442. [Google Scholar] [CrossRef] [PubMed]
- Muntané-Carol, G.; Alperi, A.; Faroux, L.; Bédard, E.; Philippon, F.; Rodés-Cabau, J. Transcatheter tricuspid valve intervention: Coaptation devices. Front. Cardiovasc. Med. 2020, 7, 139. [Google Scholar] [CrossRef] [PubMed]
- Tang, G.H.L. Tricuspid clip: Step-by-step and clinical data. Interv. Cardiol. Clin. 2018, 7, 37–45. [Google Scholar] [CrossRef]
- Hahn, R.T.; Zamorano, J.L. The need for a new tricuspid regurgitation grading scheme. Eur. Hear. J. Cardiovasc. Imaging 2017, 18, 1342–1343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Topilsky, Y.; Nkomo, V.T.; Vatury, O.; Michelena, H.I.; Letourneau, T.; Suri, R.M.; Pislaru, S.; Park, S.; Mahoney, D.W.; Biner, S.; et al. Clinical outcome of isolated tricuspid regurgitation. JACC Cardiovasc. Imaging 2014, 7, 1185–1194. [Google Scholar] [CrossRef] [Green Version]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Muñoz, D.R.; et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2017, 38, 2739–2786. [Google Scholar] [CrossRef]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: A report of the American college of Cardiology/American heart association joint committee on clinical practice guidelines. Circulation 2020, 143. [Google Scholar] [CrossRef]
- Zack, C.J.; Fender, E.A.; Chandrashekar, P.; Reddy, Y.N.V.; Bennett, C.E.; Stulak, J.M.; Miller, V.M.; Nishimura, R.A. National trends and outcomes in isolated tricuspid valve surgery. J. Am. Coll. Cardiol. 2017, 70, 2953–2960. [Google Scholar] [CrossRef]
- Blecker, S.; Paul, M.; Taksler, G.; Ogedegbe, G.; Katz, S. Heart failure-associated hospitalizations in the United States. J. Am. Coll. Cardiol. 2013, 61, 1259–1267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Latib, A.; Grigioni, F.; Hahn, R. Tricuspid regurgitation: What is the real clinical impact and how often should it be treated? EuroIntervention 2018, 14, AB101–AB111. [Google Scholar] [CrossRef]
- Utsunomiya, H.; Itabashi, Y.; Mihara, H.; Berdejo, J.; Kobayashi, S.; Siegel, R.J.; Shiota, T. Functional tricuspid regurgitation caused by chronic atrial fibrillation. Circ. Cardiovasc. Imaging 2017, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dietz, M.F.; Goedemans, L.; Vo, N.M.; Prihadi, E.A.; van der Bijl, P.; Gersh, B.J.; Ajmone Marsan, N.; Delgado, V.; Bax, J.J. Prognostic implications of significant isolated tricuspid regurgitation in patients with atrial fibrillation without left-sided heart disease or pulmonary hypertension. Am. J. Cardiol. 2020, 135, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Hausleiter, J.; Braun, D.; Orban, M.; Latib, A.; Lurz, P.; Boekstegers, P.; von Bardeleben, R.; Kowalski, M.; Hahn, R.; Maisano, F.; et al. Patient selection, echocardiographic screening and treatment strategies for interventional tricuspid repair using the edge-to-edge repair technique. EuroIntervention 2018, 14, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Mehr, M.; Taramasso, M.; Besler, C.; Ruf, T.; Connelly, K.A.; Weber, M.; Yzeiraj, E.; Schiavi, D.; Mangieri, A.; Vaskelyte, L.; et al. 1-year outcomes after edge-to-edge valve repair for symptomatic tricuspid regurgitation: Results from the TriValve registry. JACC Cardiovasc. Interv. 2019, 12, 1451–1461. [Google Scholar] [CrossRef]
- Taramasso, M.; Alessandrini, H.; Latib, A.; Asami, M.; Attinger-Toller, A.; Biasco, L.; Braun, D.; Brochet, E.; Connelly, K.A.; Denti, P.; et al. Outcomes after current transcatheter tricuspid valve intervention: Mid-term results from the international TriValve registry. JACC Cardiovasc. Interv. 2019, 12, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Rommel, K.P.; Besler, C.; Noack, T.; Blazek, S.; von Roeder, M.; Fengler, K.; Ender, J.; Gutberlet, M.; Desch, S.; Borger, M.A.; et al. Physiological and clinical consequences of right ventricular volume overload reduction after transcatheter treatment for tricuspid regurgitation. JACC Cardiovasc. Interv. 2019, 12, 1423–1434. [Google Scholar] [CrossRef] [PubMed]
| Age, years | 76.5 (71–81) |
| Female | 25 (89) |
| Body mass index, kg/m2 | 26.7 ± 4.89 |
| Hypertension | 17 (61) |
| Diabetes mellitus | 5 (18) |
| Atrial fibrillation | 26 (93) |
| Chronic obstructive pulmonary disease | 7 (25) |
| Coronary artery disease | 2 (7) |
| Stroke/TIA | 4 (14) |
| Estimated glomerular filtration rate | 59.5 ± 23.6 |
| PPM/ICD lead | 1 (3) |
Previous valve surgery
| 3 (10) 1 (4) |
| Previous transcatheter mitral valve intervention | 2 (6) |
| EuroSCORE II, % | 3.76 (1.99–7.03) |
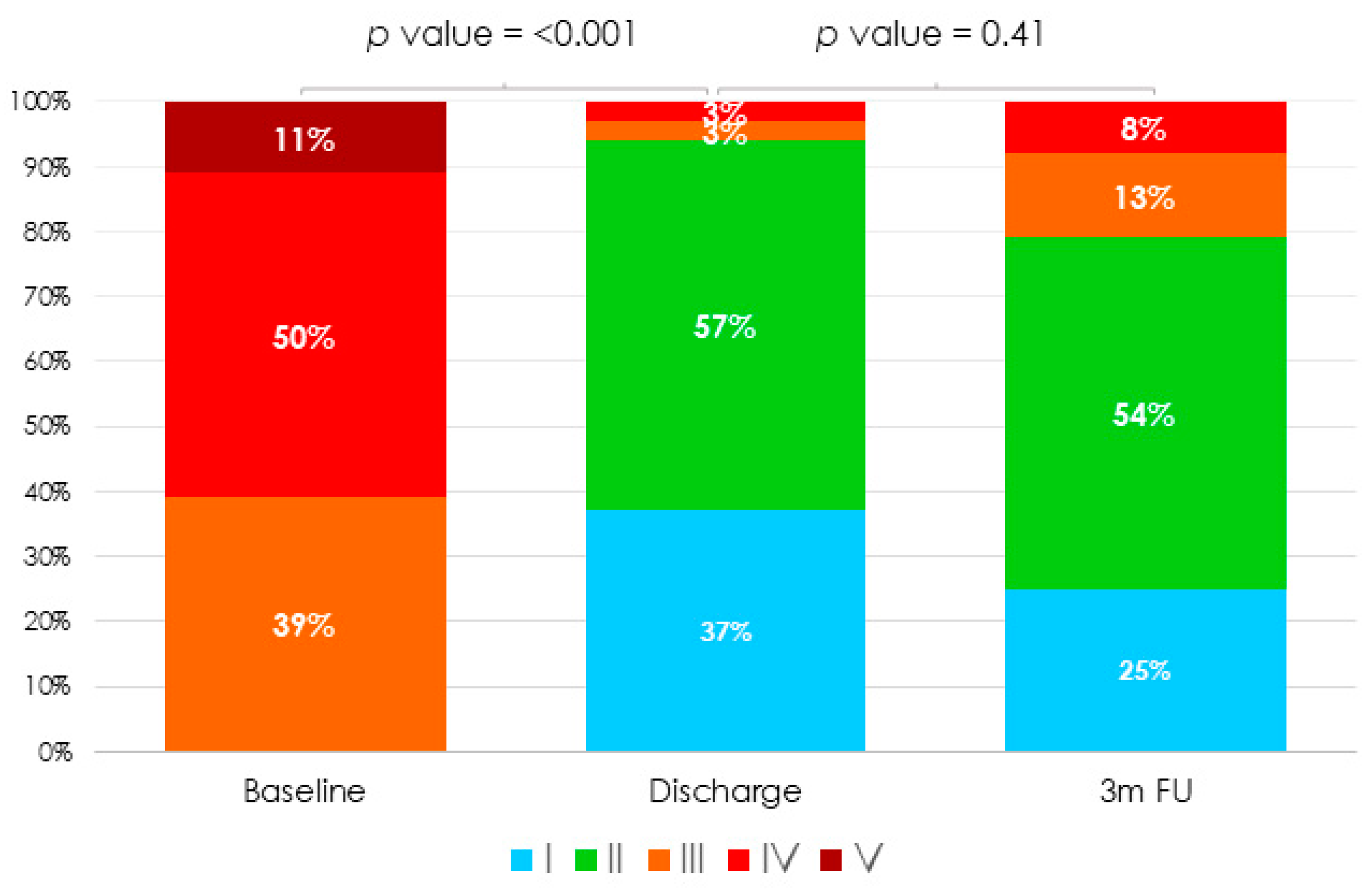
NYHA functional class
| 0 20 (18) 22 (72) 3 (10) |
| Peripheral oedema | 26 (93) |
| Ascites | 12 (43) |
| Previous hospitalization for heart failure * | 11 (40) |
| Number of admissions for heart failure * | 13 |
Medical treatment
| 18 (64) 9 (32) 9 (32) 1 (4) 15 (54) 8 (29) 1 (4) 25 (90) 10 (36) |
| Left ventricular ejection fraction, % | 59 (55–60) |
| Left ventricular end-diastolic diameter, mm | 44 (40–49.5) |
| Left ventricular end-systolic diameter, mm | 27.5 (25–31) |
Mitral regurgitation severity
| 3 (11) 21 (75) 3 (11) 1 (4) 0 |
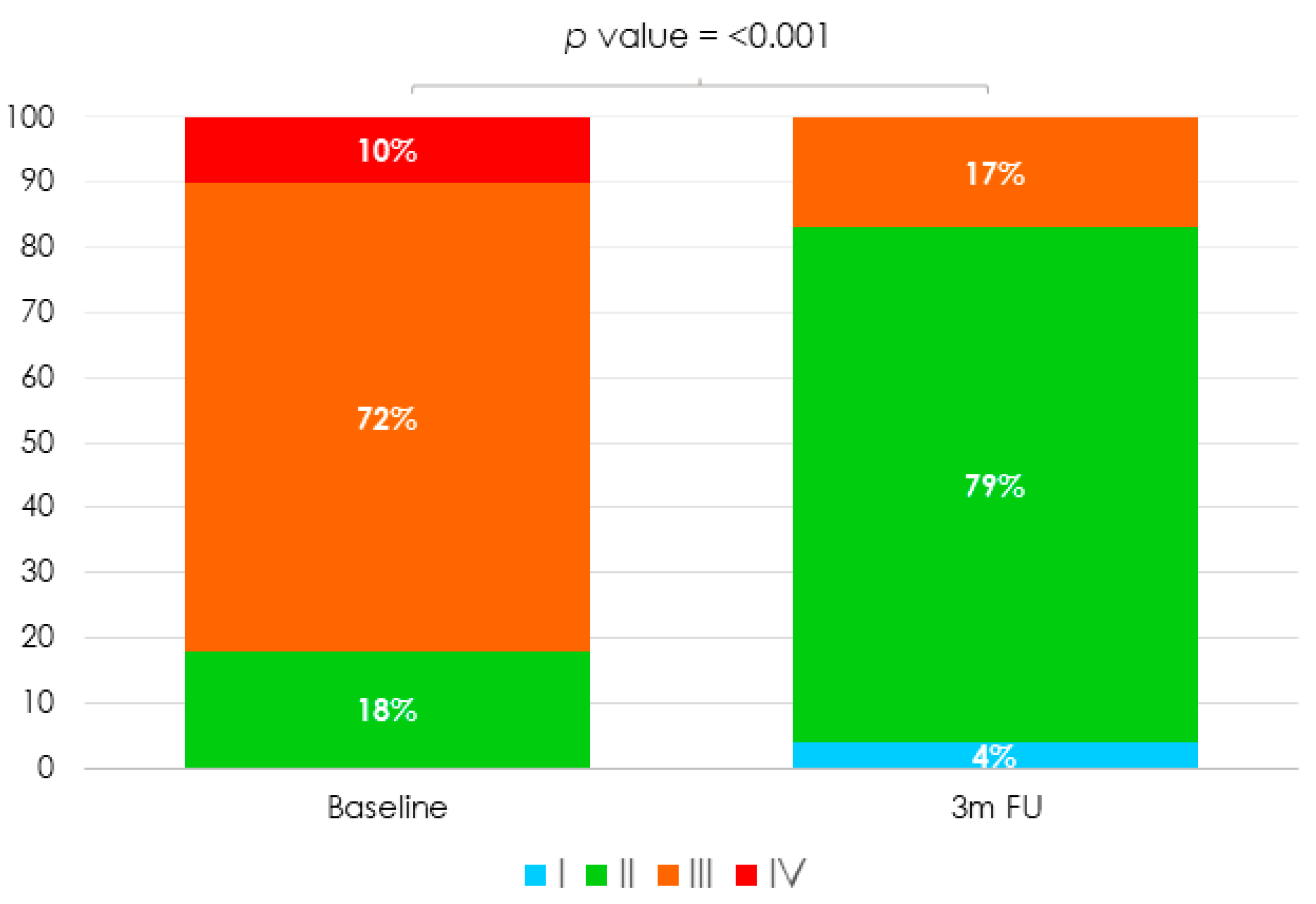
Tricuspid regurgitation severity
| 0 0 0 11 (39) 14 (50) 3 (11) |
Tricuspid regurgitation aetiology
| 26 (94) 1 (3) 1 (3) 46.2±0.8 |
| Pacemaker lead-associated tricuspid regurgitation | 1 (3) |
| Echocardiography systolic PAP, mmHg | 40 (35–47) |
| RHC systolic PAP, mmHg | 30.5 (24.5–36.5) |
| RHC right ventricular peak pressure, mmHg | 19 (14.5–21.5) |
| Implant success rate | 28 (100) |
Number of clips per patient
| 18 (64) 8 (29) 2 (7) |
Type of device
| 3 (11) 25 (89) |
Type of clip NT/XT (%)
| 15 (37) 25 (63) |
First clip location
| 23 (82) 5 (18) 0 |
Second clip location
| 7 (64) 4 (36) 0 |
| Post-procedure TV mean gradient, mmHg | 1.5 (0.8–1.6) |
| Procedural time, min | 130 (100–185) |
| Fluoroscopy time, min | 26 (22–37) |
Final in-lab TR severity
| 16 (57) 12 (43) 0 0 0 |
Technical complications
| 25 (90) 3 (11) 0 0 0 |
Procedure-related clinical adverse events
| 27 (96) 0 0 0 1 (4) 0 0 0 0 0 0 0 |
| Post-procedural length of hospital stay, days | 2 (2–3) |
| Successful implantation | 28 (100) |
Pre-discharge TR severity
| 10 (37) 16 (57) 1 (3) 1 (3) 0 |
Antithrombotic strategy at discharge
| 1 (3) 1 (3) 2 (6) 12 (44) 12 (44) |
| Clinical and Echocardiography Follow-Up at Three months | |
| All-cause mortality | 0 |
| Cardiovascular mortality | 0 |
| Hospitalization for heart failure | 1 (3) |
NYHA functional class
| 1 (4) 19 (79) 4 (17) 0 |
| Decrease of ≥1 NYHA functional class | 20 (77) |
Diuretic dose modification
| 9 (38) 14 (58) 1 (4) |
Tricuspid regurgitation severity
| 6 (25) 13 (54) 3 (13) 2 (8) 0 |
| Clinical Outcomes at Last Follow-Up | |
| Follow-up time, days | 372 (183–930) |
| All-cause mortality | 0 |
| Cardiovascular mortality | 0 |
| Hospitalization for heart failure | 4 (16) |
| Number of admissions for heart failure | 6 |
| Endocarditis | 0 |
| Tricuspid valve surgery | 1 (3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cepas-Guillen, P.L.; de la Fuente Mancera, J.C.; Guzman Bofarull, J.; Farrero, M.; Regueiro, A.; Brugaletta, S.; Ibañez, C.; Sanchis, L.; Sitges, M.; Sabate, M.; et al. Initial Results after the Implementation of an Edge-To-Edge Transcatheter Tricuspid Valve Repair Program. J. Clin. Med. 2021, 10, 4252. https://doi.org/10.3390/jcm10184252
Cepas-Guillen PL, de la Fuente Mancera JC, Guzman Bofarull J, Farrero M, Regueiro A, Brugaletta S, Ibañez C, Sanchis L, Sitges M, Sabate M, et al. Initial Results after the Implementation of an Edge-To-Edge Transcatheter Tricuspid Valve Repair Program. Journal of Clinical Medicine. 2021; 10(18):4252. https://doi.org/10.3390/jcm10184252
Chicago/Turabian StyleCepas-Guillen, Pedro Luis, Juan Carlos de la Fuente Mancera, Joan Guzman Bofarull, Marta Farrero, Ander Regueiro, Salvatore Brugaletta, Cristina Ibañez, Laura Sanchis, Marta Sitges, Manel Sabate, and et al. 2021. "Initial Results after the Implementation of an Edge-To-Edge Transcatheter Tricuspid Valve Repair Program" Journal of Clinical Medicine 10, no. 18: 4252. https://doi.org/10.3390/jcm10184252
APA StyleCepas-Guillen, P. L., de la Fuente Mancera, J. C., Guzman Bofarull, J., Farrero, M., Regueiro, A., Brugaletta, S., Ibañez, C., Sanchis, L., Sitges, M., Sabate, M., & Freixa, X. (2021). Initial Results after the Implementation of an Edge-To-Edge Transcatheter Tricuspid Valve Repair Program. Journal of Clinical Medicine, 10(18), 4252. https://doi.org/10.3390/jcm10184252






