Arterial Stiffness Assessment Using the Arteriograph in Patients with Moderate–Severe OSA and Metabolic Syndrome—A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
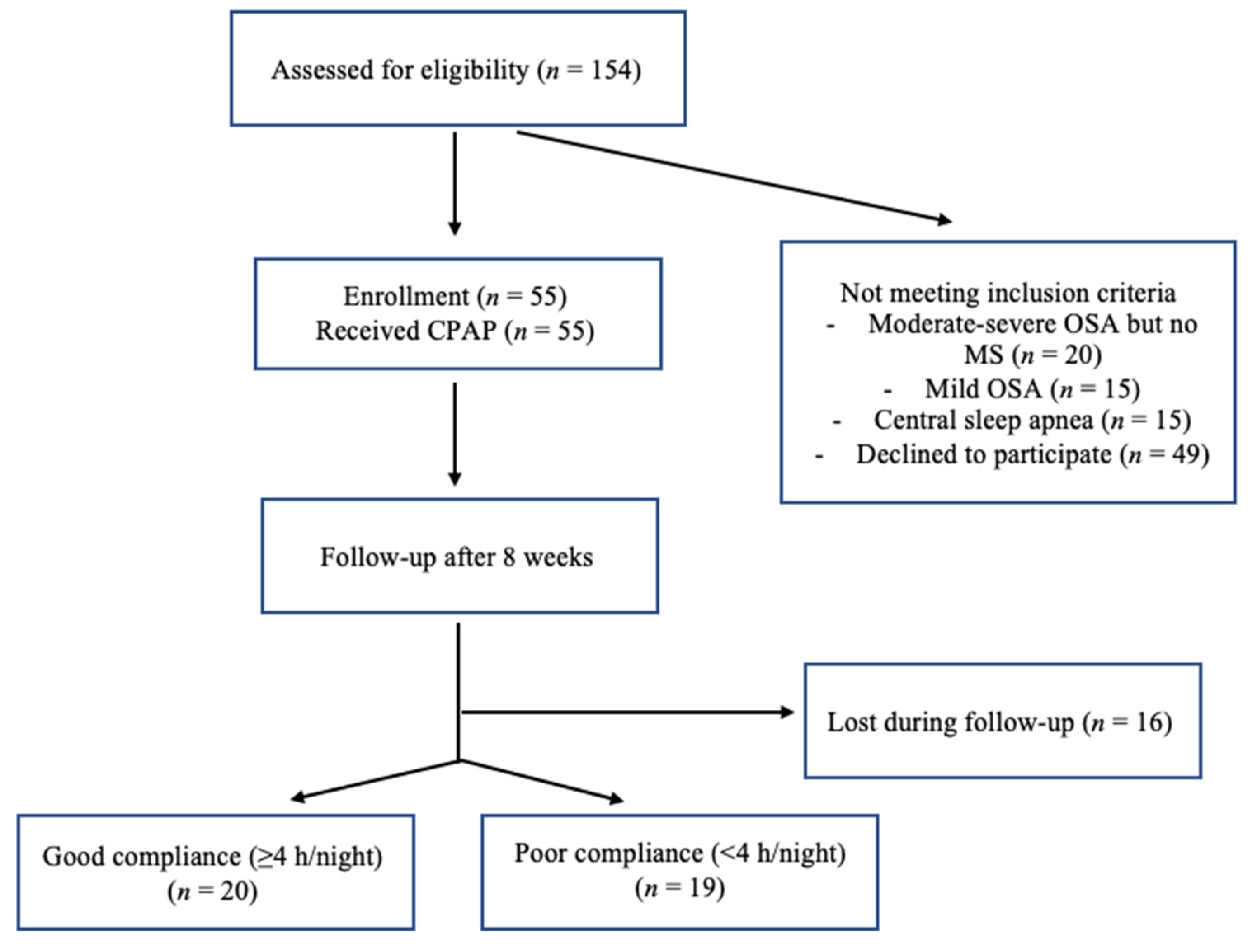
2.1. Patients
2.2. Study Design
2.3. Measurements
2.3.1. Body Measurements
2.3.2. Smoking Status
2.3.3. CPAP Adherence
2.3.4. ABPM
2.3.5. Holter-ECG
2.3.6. Assessment of Arterial Function
2.4. Statistical Analysis
3. Results
3.1. All Patients
3.2. Comparison between Groups
3.3. Correlations between Arterial Stiffness and OSA Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Akkus, O.; Sahin, D.Y.; Bozkurt, A.; Nas, K.; Ozcan, K.S.; Illyés, M.; Molnár, F.; Demir, S.; Tüfenk, M.; Acarturk, E. Evaluation of arterial stiffness for predicting future cardiovascular events in patients with st segment elevation and non-st segment elevation myocardial infarction. Sci. World J. 2013, 2013, 1–6. [Google Scholar] [CrossRef]
- Parati, G.; De Buyzere, M. Evaluating aortic stiffness through an arm cuff oscillometric device: Is validation against invasive measurements enough? J. Hypertens. 2010, 28, 2003–2006. [Google Scholar] [CrossRef] [PubMed]
- Laurent, S.; Boutouyrie, P.; Asmar, R.; Gautier, I.; Laloux, B.; Guize, L.; Ducimetiere, P.; Benetos, A. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001, 37, 1236–1241. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Boutouyrie, P.; Revera, M.; Parati, G. Obtaining arterial stiffness indices from simple arm cuff measurements: The holy grail? J. Hypertens. 2009, 27, 2159–2161. [Google Scholar] [CrossRef]
- Baibata, E.D.; Cosor, O.C.; Mitu, F.; Iurciuc, M.; Mancas, S. Arterial stiffness and cardiovascular risk. Rom. J. Cardiol. 2016, 26, 450–454. [Google Scholar]
- Jatoi, A.N.; Mahmud, A.; Bennett, K.; Feely, J. Assessment of arterial stiffness in hypertension: Comparison of oscillometric (Arteriograph), piezoelectronic (Complior) and tonometric (SphygmoCor) techniques*. J. Hypertens. 2009, 27, 2186–2191. [Google Scholar] [CrossRef]
- Baulmann, J.; Schillings, U.; Rickert, S.; Uen, S.; Düsing, R.; Illyes, M.; Cziraki, A.; Nickenig, G.; Mengden, T. A new oscillometric method for assessment of arterial stiffness: Comparison with tonometric and piezo-electronic methods. J. Hypertens. 2008, 26, 523–528. [Google Scholar] [CrossRef]
- Boutouyrie, P.; Tropeano, A.I.; Asmar, R.; Gautier, I.; Benetos, A.; Lacolley, P.; Laurent, S. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: A longitudinal study. Hypertension 2002, 39, 10–15. [Google Scholar] [CrossRef]
- Ring, M.; Eriksson, M.J.; Zierath, J.R.; Caidahl, K. Arterial stiffness estimation in healthy subjects: A validation of oscillometric (Arteriograph) and tonometric (SphygmoCor) techniques. Hypertens. Res. 2014, 37, 999–1007. [Google Scholar] [CrossRef]
- Phillips, C.L.; Butlin, M.; Wong, K.K.; Avolio, A.P. Is obstructive sleep apnoea causally related to arterial stiffness? A critical review of the experimental evidence. Sleep Med. Rev. 2013, 17, 7–18. [Google Scholar] [CrossRef]
- Mar, H.L.P.Y.; Hazen, S.L.; Tracy, R.P.; Strohl, K.P.; Auckley, D.; Bena, J.; Wang, L.; Walia, H.K.; Patel, S.; Mehra, R. Effect of Continuous Positive Airway Pressure on Cardiovascular Biomarkers. Chest 2016, 150, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Bercea, R.M.; Patacchioli, F.R.; Ghiciuc, C.M.; Cojocaru, E.; Mihaescu, T. Serum testosterone and depressive symptoms in severe OSA patients. Andrologia 2013, 45, 345–350. [Google Scholar] [CrossRef]
- Jones, A.; Vennelle, M.; Connell, M.; McKillop, G.; Newby, D.E.; Douglas, N.J.; Riha, R.L. The effect of continuous positive airway pressure therapy on arterial stiffness and endothelial function in obstructive sleep apnea: A randomized controlled trial in patients without cardiovascular disease. Sleep Med. 2013, 14, 1260–1265. [Google Scholar] [CrossRef] [PubMed]
- Ghiciuc, C.M.; Dima-Cozma, L.C.; Bercea, R.M.; Lupusoru, C.E.; Mihaescu, T.; Cozma, S.; Patacchioli, F.R. Imbalance in the diurnal salivary testosterone/cortisol ratio in men with severe obstructive sleep apnea: An observational study. Braz. J. Otorhinolaryngol. 2016, 82, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Ghiciuc, C.M.; Cozma, L.C.D.; Bercea, R.M.; Lupusoru, C.E.; Mihaescu, T.; Szalontay, A.; Gianfreda, A.; Patacchioli, F.R. Restoring the salivary cortisol awakening response through nasal continuous positive airway pressure therapy in obstructive sleep apnea. Chronobiol. Int. 2013, 30, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Doonan, R.J.; Scheffler, P.; Lalli, M.; Kimoff, R.J.; Petridou, E.; Daskalopoulos, E.M.; Daskalopoulou, S.S. Increased arterial stiffness in obstructive sleep apnea: A systematic review. Hypertens. Res. 2010, 34, 23–32. [Google Scholar] [CrossRef]
- Vlachantoni, I.-T.; Dikaiakou, E.; Antonopoulos, C.N.; Stefanadis, C.; Daskalopoulou, S.S.; Petridou, E.T. Effects of continuous positive airway pressure (CPAP) treatment for obstructive sleep apnea in arterial stiffness: A meta-analysis. Sleep Med. Rev. 2013, 17, 19–28. [Google Scholar] [CrossRef]
- Lin, X.; Chen, G.; Qi, J.; Chen, X.; Zhao, J.; Lin, Q. Effect of continuous positive airway pressure on arterial stiffness in patients with obstructive sleep apnea and hypertension: A meta-analysis. Eur. Arch. Oto Rhino Laryngol. 2016, 273, 4081–4088. [Google Scholar] [CrossRef]
- Drager, L.F.; Bortolotto, L.A.; Figueiredo, A.C.; Krieger, E.M.; Lorenzi-Filho, G. Effects of Continuous Positive Airway Pressure on Early Signs of Atherosclerosis in Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2007, 176, 706–712. [Google Scholar] [CrossRef]
- Ning, Y.; Zhang, T.-S.; Wen, W.-W.; Li, K.; Yang, Y.-X.; Qin, Y.-W.; Zhang, H.-N.; Du, Y.-H.; Li, L.-Y.; Yang, S.; et al. Effects of continuous positive airway pressure on cardiovascular biomarkers in patients with obstructive sleep apnea: A meta-analysis of randomized controlled trials. Sleep Breath. 2018, 23, 77–86. [Google Scholar] [CrossRef]
- Mineiro, M.A.; Da Silva, P.M.; Alves, M.; Papoila, A.L.; Gomes, M.J.M.; Cardoso, J. The role of sleepiness on arterial stiffness improvement after CPAP therapy in males with obstructive sleep apnea: A prospective cohort study. BMC Pulm. Med. 2017, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Drager, L.F.; Lorenzi-Filho, G. Is CPAP preventing the long-term progression of arterial stiffness in patients with obstructive sleep apnea? Hypertens. Res. 2010, 33, 788–789. [Google Scholar] [CrossRef] [PubMed]
- Kohler, M.; Pepperell, J.C.T.; Casadei, B.; Craig, S.; Crosthwaite, N.; Stradling, J.R.; Davies, R.J.O. CPAP and measures of cardiovascular risk in males with OSAS. Eur. Respir. J. 2008, 32, 1488–1496. [Google Scholar] [CrossRef] [PubMed]
- Yandieva, A.; Ovsyannikov, K. Effect of CPAP-Treatment on the arterial stiffness and systemic inflammation in patients with metabolic syndrome and obstructive sleep apnea. J. Clin. Exp. Cardiol. 2017, 8, C1–C086. [Google Scholar]
- Saito, T.; Saito, T.; Sugiyama, S.; Asai, K.; Yasutake, M.; Mizuno, K. Effects of long-term treatment for obstructive sleep apnea on pulse wave velocity. Hypertens. Res. 2010, 33, 844–849. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Punjabi, N.M.; Caffo, B.S.; Goodwin, J.L.; Gottlieb, D.J.; Newman, A.B.; O‘Connor, G.; Rapoport, D.; Redline, S.; Resnick, H.E.; Robbins, J.A.; et al. Sleep-Disordered Breathing and Mortality: A Prospective Cohort Study. PLoS Med. 2009, 6, e1000132. [Google Scholar] [CrossRef]
- Cozma, S.; Dima-Cozma, L.; Ghiciuc, C.; Pasquali, V.; Saponaro, A.; Patacchioli, F. Salivary cortisol and α-amylase: Subclinical indicators of stress as cardiometabolic risk. Braz. J. Med. Biol. Res. 2017, 50, e5577. [Google Scholar] [CrossRef]
- Topouchian, J.; Labat, C.; Gautier, S.; Bäck, M.; Achimastos, A.; Blacher, J.; Cwynar, M.; de la Sierra, A.; Pall, D.; Fantin, F.; et al. Effects of metabolic syndrome on arterial function in different age groups: The Advanced Approach to Arterial Stiffness Study. J. Hypertens. 2018, 36, 824–833. [Google Scholar] [CrossRef]
- Effects of CPAP on Metabolic Syndrome in Patients with Obstructive Sleep Apnea: The TREATOSA-MS Randomized Controlled trial. Available online: https://www.abstractsonline.com/pp8/#!/8998/presentation/17720 (accessed on 24 June 2020).
- Galerneau, L.-M.; Tamisier, R.; Benmerad, M.; Bonsignore, M.R.; Borel, J.-C.; Pepin, J.-L. Arterial stiffness in obese CPAP-treated obstructive sleep apnea (OSA): A seven years prospective longitudinal study. Eur. Respir. J. 2017, 50, PA4716. [Google Scholar] [CrossRef]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed]
- Sateia, M.J. International classification of sleep disorders-third edition. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association declaration of Helsinki: Ethical Principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Engleman, H.M.; Wild, M.R. Improving CPAP use by patients with the sleep apnoea/hypopnoea syndrome (SAHS). Sleep Med. Rev. 2003, 7, 81–99. [Google Scholar] [CrossRef]
- Ryan, H.; Trosclair, A.; Gfroerer, J. Adult current smoking: Differences in definitions and prevalence estimates—NHIS and NSDUH. J. Environ. Public Health 2012, 2012, 1–11. [Google Scholar] [CrossRef]
- Operator‘s Manual for DMS 300-4A Holter ECG Recorder. Available online: http://www.holterdms.com/manuals/300-4A%20Manual.pdf (accessed on 17 April 2021).
- Tensiomed. Innovative Method to Ease Arterial Stiffness Measurement. Available online: https://www.tensiomed.com (accessed on 17 April 2021).
- Nsair, A.; Hupin, D.; Chomette, S.; Barthélémy, J.C.; Roche, F. Factors influencing adherence to auto-CPAP: An observational monocentric study comparing patients with and without cardiovascular diseases. Front. Neurol. 2019, 10, 801. [Google Scholar] [CrossRef]
- Dorkova, Z.; Petrasova, D.; Molcanyiova, A.; Popovnakova, M.; Tkacova, R. Effects of Continuous positive airway pressure on cardiovascular risk profile in patients with severe obstructive sleep apnea and metabolic syndrome. Chest 2008, 134, 686–692. [Google Scholar] [CrossRef]
- Randerath, W.J.; Herkenrath, S.; Treml, M.; Grote, L.; Hedner, J.; Bonsignore, M.R.; Pépin, J.L.; Ryan, S.; Schiza, S.; Verbraecken, J.; et al. Evaluation of a multicomponent grading system for obstructive sleep apnoea: The Baveno classification. ERJ Open Res. 2021, 7, 00928–02020. [Google Scholar] [CrossRef]
- Alefishat, E.A.; Abu Farha, R.; Al-Debei, M.M. Self-Reported Adherence among Individuals at High Risk of Metabolic Syndrome: Effect of Knowledge and Attitude. Med. Princ. Pract. 2016, 26, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Trachet, B.; Reymond, P.; Kips, J.; Vermeersch, S.; Swillens, A.; Stergiopulos, N.; Segers, P. Validation of the Arteriograph working principle: Questions still remain. J. Hypertens. 2011, 29, 619. [Google Scholar] [CrossRef] [PubMed]
- Rajzer, M.W.; Wojciechowska, W.; Klocek, M.; Palka, I.; Brzozowska-Kiszka, M.; Kawecka-Jaszcz, K. Comparison of aortic pulse wave velocity measured by three techniques: Complior, SphygmoCor and Arteriograph. J. Hypertens. 2008, 26, 2001–2007. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by Representatives of 10 Societies and by Invited Experts)Developed with the Special Contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef] [PubMed]
- Protogerou, A.D.; Laaban, J.-P.; Czernichow, S.; Kostopoulos, C.; Lekakis, J.; E Safar, M.; Blacher, J. Structural and functional arterial properties in patients with obstructive sleep apnoea syndrome and cardiovascular comorbidities. J. Hum. Hypertens. 2007, 22, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Tamisier, R.; Borel, J.C.; Millasseau, S.; Galerneau, L.; Destors, M.; Perrin, M.; Pepin, J. Arterial stiffness in patients with obstructive sleep apnea syndrome: An individual meta-analysis of contributing factors. J. Hypertens. 2016, 34, e100. [Google Scholar] [CrossRef]
- Joyeux-Faure, M.; Tamisier, R.; Borel, J.-C.; Millasseau, S.; Galerneau, L.-M.; Destors, M.; Bailly, S.; Pepin, J.L. Contribution of obstructive sleep apnoea to arterial stiffness: A meta-analysis using individual patient data. Thorax 2018, 73, 1146–1151. [Google Scholar] [CrossRef] [PubMed]
- Buchner, N.J.; Quack, I.; Stegbauer, J.; Woznowski, M.; Kaufmann, A.; Rump, L.C. Treatment of obstructive sleep apnea reduces arterial stiffness. Sleep Breath. 2011, 16, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Picard, F.; Panagiotidou, P.; Weinig, L.; Steffen, M.; Tammen, A.-B.; Klein, R.M. Effect of CPAP therapy on nocturnal blood pressure fluctuations, nocturnal blood pressure, and arterial stiffness in patients with coexisting cardiovascular diseases and obstructive sleep apnea. Sleep Breath. 2020, 25, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, C.R.L.; Roderjan, C.N.; Cavalcanti, A.H.; Cortez, A.F.; Muxfeldt, E.S.; Salles, G.F. Effects of continuous positive airway pressure treatment on aortic stiffness in patients with resistant hypertension and obstructive sleep apnea: A randomized controlled trial. J. Sleep Res. 2020, 29, e12990. [Google Scholar] [CrossRef] [PubMed]
- Vlachopoulos, C.; Aznaouridis, K.; Stefanadis, C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 55, 1318–1327. [Google Scholar] [CrossRef]
- Schwartz, J.E.; Feig, P.U.; Izzo, J.L. Pulse wave velocities derived from cuff ambulatory pulse wave analysis. Hypertension 2019, 74, 111–116. [Google Scholar] [CrossRef]
- Salvi, P.; Scalise, F.; Rovina, M.; Moretti, F.; Salvi, L.; Grillo, A.; Gao, L.; Baldi, C.; Faini, A.; Furlanis, G.; et al. Noninvasive estimation of aortic stiffness through different approaches. Hypertension 2019, 74, 117–129. [Google Scholar] [CrossRef]
- Ryan, S. The effect of continuous positive airway pressure therapy on vascular function in obstructive sleep apnea: How much is enough? Sleep Med. 2013, 14, 1231–1232. [Google Scholar] [CrossRef] [PubMed]
- Drager, L.F.; Brunoni, A.R.; Jenner, R.; Lorenzi-Filho, G.; Benseñor, I.M.; Lotufo, P. Effects of CPAP on body weight in patients with obstructive sleep apnoea: A meta-analysis of randomised trials. Thorax 2014, 70, 258–264. [Google Scholar] [CrossRef]
- Tachikawa, R.; Ikeda, K.; Minami, T.; Matsumoto, T.; Hamada, S.; Murase, K.; Tanizawa, K.; Inouchi, M.; Oga, T.; Akamizu, T.; et al. Changes in energy metabolism after continuous positive airway pressure for obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 2016, 194, 729–738. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Li, G.-L.; Li, Y.; Wang, J.-G. Effects of various antihypertensive drugs on arterial stiffness and wave reflections. Pulse 2013, 1, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Dudenbostel, T.; Glasser, S. Effects of antihypertensive drugs on arterial stiffness. Cardiol. Rev. 2012, 20, 259–263. [Google Scholar] [CrossRef]



| All Patients (n = 39) | Adherent (n = 20) | Non-Adherent (n = 19) | p-Value # | |
|---|---|---|---|---|
| Age (years) | 57 ± 9 | 60 ± 7 | 55 ± 10 | 0.080 |
| Smoking status | ||||
| Current smoker (%) | 12.8% | 5% | 21.1% | 0.133 |
| Former smoker (%) | 56.4% | 55% | 57.9% | 0.857 |
| Never smoker | 30.8% | 40% | 21.1% | 0.200 |
| Weight (kg) | 101 ± 17 | 97 ± 17 | 105 ± 16 | 0.143 |
| BMI (kg/m2) | 33.8 ± 4.7 | 32.9 ± 4.8 | 34.7 ± 4.8 | 0.224 |
| WC (cm) | 114 ± 10 | 112 ± 10 | 116 ± 10 | 0.181 |
| Blood tests | ||||
| Fasting blood glucose (mg/dL) | 112.31 ± 19.84 | 111.77 ± 13.4 | 112.89 ± 25.31 | 0.863 |
| HDL-cholesterol (mg/dL) | 50.58 ± 12.87 | 52.80 ± 14.76 | 48.23 ± 10.41 | 0.274 |
| TG (mg/dL) | 167.44 ± 86.09 | 154.95 ± 98.88 | 180.60 ± 70.50 | 0.359 |
| OSA parameters | ||||
| AHI (events/h) | 39.7 ± 19.5 | 35.9 ± 15.9 | 45.4 ± 22.7 | 0.142 |
| DI (events/h) | 38.6 ± 18.4 | 35.6 ± 15.1 | 41.7 ± 21.4 | 0.312 |
| Mean nocturnal O2Sa (%) | 91.8 ± 2.6 | 91.8 ± 2.5 | 91.8 ± 2.7 | 0.907 |
| ESS (points) | 6.2 ± 3.9 | 6.9 ± 3.9 | 5.4 ± 3.9 | 0.245 |
| CPAP pressure (cmH20) | 10.9 ± 2.3 | 11.5 ± 2.1 | 10.4 ± 2.5 | 0.159 |
| All Patients (n = 39) | Adherent (n = 20) | Non-Adherent (n = 19) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | After 8-Week CPAP | p-Value | Baseline | After 8-Week CPAP | p-Value | Baseline | After 8-Week CPAP | p-Value | |
| Age (years) | 57 ± 9 | 60 ± 7 | 55 ± 10 | ||||||
| Weight (kg) | 101 ± 17 | 98 ± 16 | 0.007 | 97 ± 17 | 95 ± 16 | 0.002 | 105 ± 16 | 102 ± 16 | 0.016 |
| BMI (kg/m2) | 33.7 ± 4.7 | 33.0 ± 4.6 | 0.0001 | 32.9 ± 4.8 | 32.3 ± 4.5 | 0.002 | 34.7 ± 4.8 | 33.8 ± 4.8 | 0.018 |
| WC (cm) | 114 ± 10 | 111 ± 11 | <0.0001 | 112 ± 10 | 109 ± 10 | 0.000 | 116 ± 10 | 112 ± 12 | 0.002 |
| ESS (points) | 6.2 ± 3.9 | 3.1 ± 2.7 | 0.0001 | 6.9 ± 3.9 | 3.2 ± 2.5 | 0.0007 | 5.4 ± 3.9 | 3.1 ± 3.1 | 0.049 |
| ABPM (mmHg) | |||||||||
| Mean SBP/24 h | 129 ± 14 | 130 ± 13 | 0.597 | 129 ± 16 | 132 ± 9 | 0.372 | 129 ± 13 | 129 ± 15 | 0.965 |
| Mean DBP/24 h | 76 ± 8 | 75 ± 8 | 0.372 | 74 ± 7 | 75 ± 5 | 0.846 | 78 ± 8 | 75 ± 10 | 0.268 |
| Mean daytime SBP | 131 ± 16 | 133 ± 13 | 0.527 | 130 ± 19 | 134 ± 10 | 0.390 | 132 ± 13 | 132 ± 15 | 0.974 |
| Mean daytime DBP | 78 ± 9 | 77 ± 8 | 0.859 | 75 ± 10 | 77 ± 5 | 0.304 | 81 ± 8 | 78 ± 10 | 0.294 |
| Mean nighttime SBP | 122 ± 15 | 123 ± 14 | 0.877 | 125 ± 15 | 125 ± 11 | 0.936 | 120 ± 15 | 121 ± 17 | 0.796 |
| Mean nighttime SBP | 71 ± 10 | 68 ± 9 | 0.243 | 71 ± 8 | 69 ± 7 | 0.326 | 71 ± 12 | 68 ± 11 | 0.459 |
| Holter ECG monitoring | |||||||||
| Mean HR/24 h (bpm) | 71 ± 10 | 70 ± 9 | 0.641 | 70 ± 12 | 70 ± 10 | 0.526 | 70 ± 10 | 71 ± 8 | 0.175 |
| Arterial stiffness | |||||||||
| aoSBP (mmHg) | 122 ± 19 | 115 ± 13 | 0.029 | 125 ± 22 | 114 ± 15 | 0.009 | 118 ± 15 | 116 ± 13 | 0.696 |
| aoPP (mmHg) | 43.9 ± 11.9 | 41.9 ± 10.2 | 0.248 | 46.4 ± 13.4 | 42.4 ± 9.8 | 0.090 | 41.2 ± 9.9 | 41.6 ± 10.9 | 0.864 |
| aoAix (%) | 28.4 ± 15.2 | 24.7 ± 15.1 | 0.061 | 32.6 ± 16.2 | 24.3 ± 15.7 | 0.013 | 24.0 ± 13.1 | 25.2 ± 14.9 | 0.481 |
| aoPWV (m/s) | 9.3 ± 1.7 | 8.5 ± 1.4 | 0.004 | 9.2 ± 1.8 | 8.5 ± 1.3 | 0.036 | 9.3 ± 1.7 | 8.6 ± 1.6 | 0.057 |
| AHI r | p-Value | Mean Nocturnal O2Sa r | p-Value | |
|---|---|---|---|---|
| AHI | - | - | −0.353 | 0.027 |
| Mean nocturnal O2Sa (%) | −0.353 | 0.027 | − | - |
| Desaturation index (events/h) | 0.964 | <0.0000001 | −0.390 | 0.013 |
| Age | −0.009 | 0.956 | −0.101 | 0.537 |
| Weight | 0.257 | 0.112 | −0.402 | 0.010 |
| BMI | 0.294 | 0.069 | −0.469 | 0.002 |
| WC | 0.310 | 0.054 | −0.568 | 0.0001 |
| ESS | −0.088 | 0.598 | −0.248 | 0.133 |
| aoSBP (mmHg) | 0.026 | 0.872 | 0.015 | 0.923 |
| aoPP (mmHg) | −0.075 | 0.646 | 0.082 | 0.616 |
| aoAix (%) | −0.235 | 0.149 | 0.201 | 0.218 |
| aoPWV (m/s) | 0.264 | 0.103 | −0.507 | 0.0009 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zota, I.M.; Stătescu, C.; Sascău, R.A.; Roca, M.; Anghel, L.; Mitu, O.; Ghiciuc, C.M.; Boisteanu, D.; Anghel, R.; Cozma, S.R.; et al. Arterial Stiffness Assessment Using the Arteriograph in Patients with Moderate–Severe OSA and Metabolic Syndrome—A Pilot Study. J. Clin. Med. 2021, 10, 4238. https://doi.org/10.3390/jcm10184238
Zota IM, Stătescu C, Sascău RA, Roca M, Anghel L, Mitu O, Ghiciuc CM, Boisteanu D, Anghel R, Cozma SR, et al. Arterial Stiffness Assessment Using the Arteriograph in Patients with Moderate–Severe OSA and Metabolic Syndrome—A Pilot Study. Journal of Clinical Medicine. 2021; 10(18):4238. https://doi.org/10.3390/jcm10184238
Chicago/Turabian StyleZota, Ioana Mădălina, Cristian Stătescu, Radu Andy Sascău, Mihai Roca, Larisa Anghel, Ovidiu Mitu, Cristina Mihaela Ghiciuc, Daniela Boisteanu, Razvan Anghel, Sebastian Romica Cozma, and et al. 2021. "Arterial Stiffness Assessment Using the Arteriograph in Patients with Moderate–Severe OSA and Metabolic Syndrome—A Pilot Study" Journal of Clinical Medicine 10, no. 18: 4238. https://doi.org/10.3390/jcm10184238
APA StyleZota, I. M., Stătescu, C., Sascău, R. A., Roca, M., Anghel, L., Mitu, O., Ghiciuc, C. M., Boisteanu, D., Anghel, R., Cozma, S. R., Dima-Cozma, L. C., & Mitu, F. (2021). Arterial Stiffness Assessment Using the Arteriograph in Patients with Moderate–Severe OSA and Metabolic Syndrome—A Pilot Study. Journal of Clinical Medicine, 10(18), 4238. https://doi.org/10.3390/jcm10184238










