Diagnostic Accuracy Study Comparing Hysterosalpingo-Foam Sonography and Hysterosalpingography for Fallopian Tube Patency Assessment
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Technique
2.3. Clinical Outcomes
2.4. Statistical Analysis
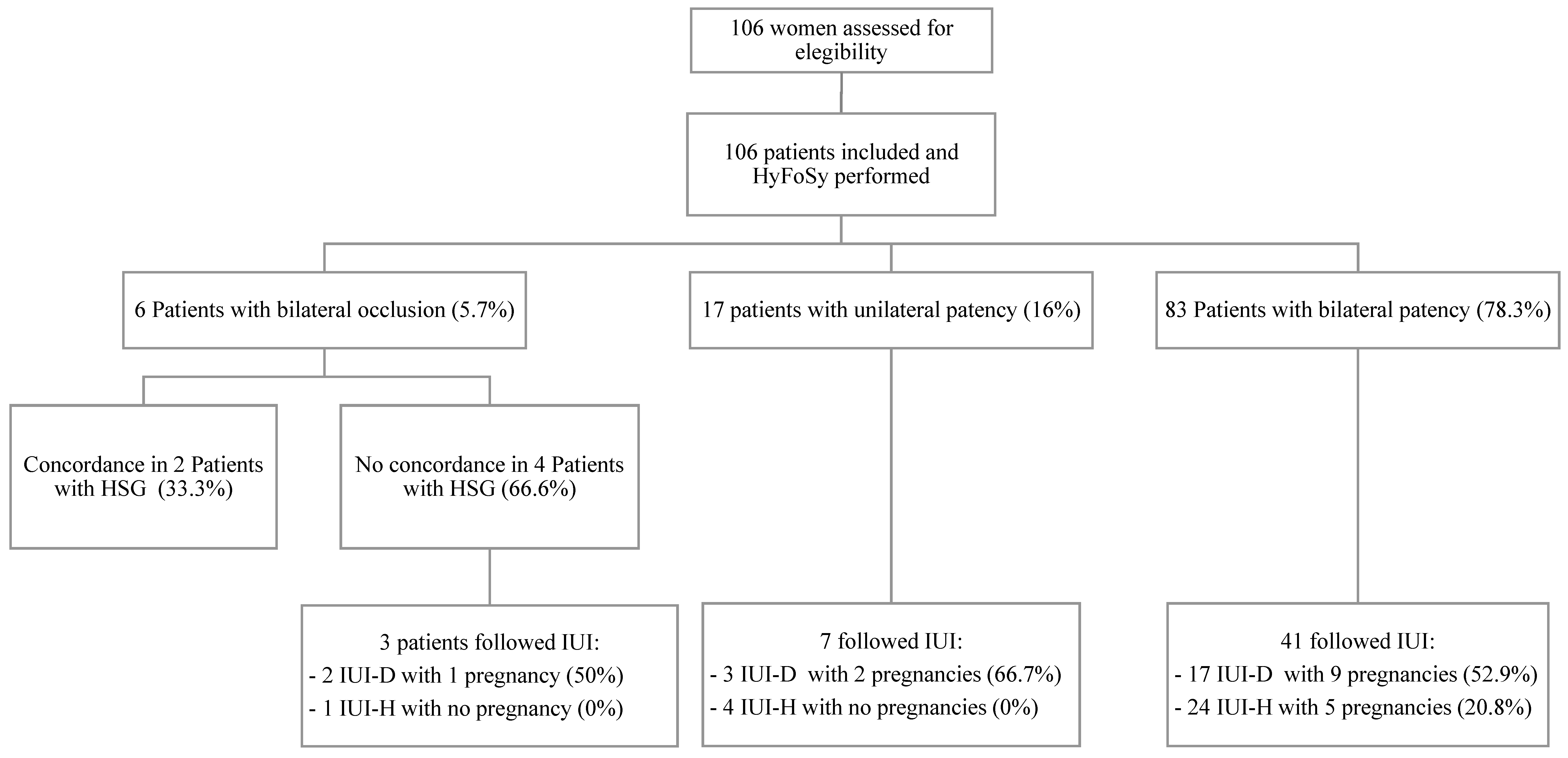
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Rajesh, H.; Lim, S.L.; Yu, S.L. Hysterosalpingo-foam sonography: Patient selection and perspectives. Int. J. Women’s Health 2016, ume 9, 23–32. [Google Scholar] [CrossRef][Green Version]
- Mol, B.W.J.; Lijmer, J.; Dijkman, B.; van der Veen, F.; Wertheim, P.; Boss, P.M.M. The accuracy of serum chlamydial antibodies in the diagnosis of tubal pathology: A meta-analysis. Fertil. Steril. 1997, 67, 1031–1037. [Google Scholar] [CrossRef]
- Dun, E.C.; Nezhat, C.H. Tubal Factor Infertility. Obstet. Gynecol. Clin. N. Am. 2012, 39, 551–566. [Google Scholar] [CrossRef] [PubMed]
- Saunders, R.D.; Shwayder, J.M.; Nakajima, S.T. Current methods of tubal patency assessment. Fertil. Steril. 2011, 95, 2171–2179. [Google Scholar] [CrossRef]
- Adelusi, B.; Al-Nuaim, L.; Makanjuola, R.; Khashoggi, T.; Chowdhury, N.; Kangave, D. Accuracy of hysterosalpingography and laparoscopic hydrotubation in diagnosis of tubal patency. Fertil. Steril. 1995, 63, 1016–1020. [Google Scholar] [CrossRef]
- Maheux-Lacroix, S.; Boutin, A.; Moore, L.; Bergeron, M.-E.; Bujold, E.; Laberge, P.; Lemyre, M.; Dodin, S. Hysterosalpingosonography for diagnosing tubal occlusion in subfertile women: A systematic review with meta-analysis. Hum. Reprod. 2014, 29, 953–963. [Google Scholar] [CrossRef] [PubMed]
- Exacoustos, C.; Zupi, E.; Carusotti, C.; Lanzi, G.; Marconi, D.; Arduini, D. Hysterosalpingo-Contrast Sonography Compared with Hysterosalpingography and Laparoscopic Dye Pertubation to Evaluate Tubal Patency. J. Am. Assoc. Gynecol. Laparosc. 2003, 10, 367–372. [Google Scholar] [CrossRef]
- Lopes, V.M.; Barguil, J.P.; Lacerda, T.S.; Souza, A.L.M.; Filho, A.M.D.R.; Roller, M.F.; Barbosa, E.A.; Tierno, N.Z.; Lopes, J.R.C. An overview of the results of hysterosonography prior to in vitro fertilization. JBRA Assist. Reprod. 2017, 21, 302–305. [Google Scholar] [CrossRef]
- Emanuel, M.H.; Exalto, N. Hysterosalpingo-foam sonography (HyFoSy): A new technique to visualize tubal patency. Ultrasound Obstet. Gynecol. 2011, 37, 498–499. [Google Scholar] [CrossRef]
- Exalto, N.; Emanuel, M.H. Clinical Aspects of HyFoSy as Tubal Patency Test in Subfertility Workup. BioMed Res. Int. 2019, 2019, 1–12. [Google Scholar] [CrossRef]
- Dreyer, K.; Out, R.; Hompes, P.G.; Mijatovic, V. Hysterosalpingo-foam sonography, a less painful procedure for tubal patency testing during fertility workup compared with (serial) hysterosalpingography: A randomized controlled trial. Fertil. Steril. 2014, 102, 821–825. [Google Scholar] [CrossRef]
- Lim, S.L.; Jung, J.J.; Yu, S.L.; Rajesh, H. A comparison of hysterosalpingo-foam sonography (HyFoSy) and hysterosalpingo-contrast sonography with saline medium (HyCoSy) in the assessment of tubal patency. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 195, 168–172. [Google Scholar] [CrossRef]
- Engels, V.; Medina, M.; Antolín, E.; Ros, C.; Amaro, A.; De-Guirior, C.; Manzour, N.; Sotillo, L.; De la Cuesta, R.; Rodríguez, R.; et al. Feasibility, tolerability, and safety of hysterosalpingo-foam sonography (hyfosy). multicenter, prospective Spanish study. J. Gynecol. Obstet. Hum. Reprod. 2020, 50, 102004. [Google Scholar] [CrossRef]
- Emanuel, M.H.; Van Vliet, M.; Weber, M.; Exalto, N. First experiences with hysterosalpingo-foam sonography (HyFoSy) for office tubal patency testing. Hum. Reprod. 2011, 27, 114–117. [Google Scholar] [CrossRef]
- Van Schoubroeck, D.; Bosch, T.V.D.; Ameye, L.; Boes, A.S.; D’Hooghe, T.; Timmerman, D. Pain during Fallopian-tube patency testing by hysterosalpingo-foam sonography. Ultrasound Obstet. Gynecol. 2015, 45, 346–350. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef]
- Luciano, D.E.; Exacoustos, C.; Johns, D.A.; Luciano, A.A. Can hysterosalpingo-contrast sonography replace hysterosalpingography in confirming tubal blockage after hysteroscopic sterilization and in the evaluation of the uterus and tubes in infertile patients? Am. J. Obstet. Gynecol. 2011, 204, 79.e1–79.e5. [Google Scholar] [CrossRef] [PubMed]
- Van Schoubroeck, D.; Bosch, T.V.D.; Meuleman, C.; Tomassetti, C.; D’Hooghe, T.; Timmerman, D. The Use of a New Gel Foam for the Evaluation of Tubal Patency. Gynecol. Obstet. Investig. 2013, 75, 152–156. [Google Scholar] [CrossRef]
- Piccioni, M.; Riganelli, L.; Filippi, V.; Fuggetta, E.; Colagiovanni, V.; Imperiale, L.; Caccetta, J.; Panici, P.B.; Porpora, M.G. Sonohysterosalpingography: Comparison of foam and saline solution. J. Clin. Ultrasound 2016, 45, 67–71. [Google Scholar] [CrossRef]
- Exalto, N.; Stassen, M.; Emanuel, M.H. Safety aspects and side-effects of ExEm-gel and foam for uterine cavity distension and tubal patency testing. Reprod. Biomed. Online 2014, 29, 534–540. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Luciano, D.E.; Exacoustos, C.; Luciano, A.A. Contrast Ultrasonography for Tubal Patency. J. Minim. Invasive Gynecol. 2014, 21, 994–998. [Google Scholar] [CrossRef]
- Ludwin, I.; Ludwin, A.; Wiechec, M.; Nocun, A.; Banas, T.; Basta, P.; Pitynski, K. Accuracy of hysterosalpingo-foam sonography in comparison to hysterosalpingo-contrast sonography with air/saline and to laparoscopy with dye. Hum. Reprod. 2017, 1–12. [Google Scholar] [CrossRef]
- Exacoustos, C.; Tiberio, F.; Szabolcs, B.; Romeo, V.; Romanini, E.; Zupi, E. Can Tubal Flushing with Hysterosalpingo-Foam Sonography (HyFoSy) Media Increase Women’s Chances of Pregnancy? J. Minim. Invasive Gynecol. 2015, 22, S238. [Google Scholar] [CrossRef]
- Levaillant, J.-M.; Pasquier, M.; Massin, N. A novel concept for female infertility exploration: The Fertiliscan©, a dedicated all-in-one 3D ultrasound exploration. J. Gynecol. Obstet. Hum. Reprod. 2019, 48, 363–367. [Google Scholar] [CrossRef] [PubMed]
| Mean (n = 106) | Standard Deviation | |
|---|---|---|
| Age (y) | 34.71 | ±3.68 |
| Body mass index (kg/m2) | 24.11 | ±4.54 |
| Infertility duration (y) | 2.30 | ±1.70 |
| n = 106 Patients | Patency during HyFoSy | |||
|---|---|---|---|---|
| Bilateral Obstruction (n = 6; 5.7%) | Unilateral Obstruction (n = 17; 16%) | Bilateral Patency (n = 83; 78.3%) | ||
| Patency during HSG | Bilateral obstruction (n = 5; 4.7%) | 2 (1.9%) * | 3 (2.8%) | 0 (0.0%) ** |
| Unilateral obstruction (n = 15; 14.2%) | 0 (0.0%) | 3 (2.8%) * | 11 (10.4%) | |
| 1 (0.9%) ** | ||||
| Bilateral patency (n = 86; 81.1%) | 4 (3.8%) ** | 10 (9.4%) | 72 (67.9%) * | |
| n = 106 Patients | Pain during HyFoSy | ||||
|---|---|---|---|---|---|
| No Pain (n = 55; 51.9%) | Mild Pain (n = 44; 41.5%) | Moderate Pain (n = 6; 5.7%) | Severe Pain (n = 1; 0.9%) | ||
| Pain during HSG | No pain (n = 37; 34.9%) | 31 (29.2%) | 6 (5.6%) | 0 (0.0%) | 0 (0.0%) |
| Mild pain (n = 22; 20.8%) | 2 (2.0%) | 19 (17.9%) | 1 (0.9%) | 0 (0.0%) | |
| Moderate pain (n = 33; 31.1%) | 14 (13.2%) | 17 (16.0%) | 2 (2.0%) | 0 (0.0%) | |
| Severe pain (n = 14; 13.2%) | 8 (7.5%) | 2 (2.0%) | 3 (2.8%) | 1 (0.9%) | |
| IUI-D (n = 22) | IUI-H (n = 29) | Total (n = 51) | |
|---|---|---|---|
| Clinical pregnancy rate at first IUI | 27.3% | 10.3% | 17.7% |
| Clinical pregnancy rate after two IUI | 45.5% | 17.2% | 29.4% |
| Cumulative clinical pregnancy rate | 54.6% | 17.2% | 33.3% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramos, J.; Caligara, C.; Santamaría-López, E.; González-Ravina, C.; Prados, N.; Carranza, F.; Blasco, V.; Fernández-Sánchez, M. Diagnostic Accuracy Study Comparing Hysterosalpingo-Foam Sonography and Hysterosalpingography for Fallopian Tube Patency Assessment. J. Clin. Med. 2021, 10, 4169. https://doi.org/10.3390/jcm10184169
Ramos J, Caligara C, Santamaría-López E, González-Ravina C, Prados N, Carranza F, Blasco V, Fernández-Sánchez M. Diagnostic Accuracy Study Comparing Hysterosalpingo-Foam Sonography and Hysterosalpingography for Fallopian Tube Patency Assessment. Journal of Clinical Medicine. 2021; 10(18):4169. https://doi.org/10.3390/jcm10184169
Chicago/Turabian StyleRamos, Julia, Cinzia Caligara, Esther Santamaría-López, Cristina González-Ravina, Nicolás Prados, Francisco Carranza, Víctor Blasco, and Manuel Fernández-Sánchez. 2021. "Diagnostic Accuracy Study Comparing Hysterosalpingo-Foam Sonography and Hysterosalpingography for Fallopian Tube Patency Assessment" Journal of Clinical Medicine 10, no. 18: 4169. https://doi.org/10.3390/jcm10184169
APA StyleRamos, J., Caligara, C., Santamaría-López, E., González-Ravina, C., Prados, N., Carranza, F., Blasco, V., & Fernández-Sánchez, M. (2021). Diagnostic Accuracy Study Comparing Hysterosalpingo-Foam Sonography and Hysterosalpingography for Fallopian Tube Patency Assessment. Journal of Clinical Medicine, 10(18), 4169. https://doi.org/10.3390/jcm10184169






