Proposal of a New Definition of “Very Early” Intrahepatic Cholangiocarcinoma—A Retrospective Single-Center Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Definition of “Very Early” and “Advanced” Intrahepatic Cholangiocarcinoma
2.3. Definition of Variables
2.4. Statistical Analysis
3. Results
3.1. Patient Cohort
3.2. Surgical Details
3.3. Histopathological Results
3.4. Postoperative Course and Survival
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Banales, J.M.; Marin, J.J.G.; Lamarca, A.; Rodrigues, P.M.; Khan, S.A.; Roberts, L.R.; Cardinale, V.; Carpino, G.; Andersen, J.B.; Braconi, C.; et al. Cholangiocarcinoma 2020: The next horizon in mechanisms and management. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 557–588. [Google Scholar] [CrossRef]
- Khan, S.A.; Tavolari, S.; Brandi, G. Cholangiocarcinoma: Epidemiology and risk factors. Liver Int. Off. J. Int. Assoc. Study Liver 2019, 39 (Suppl. 1), 19–31. [Google Scholar] [CrossRef] [Green Version]
- Saxena, A.; Chua, T.C.; Sarkar, A.; Chu, F.; Morris, D.L. Clinicopathologic and treatment-related factors influencing recurrence and survival after hepatic resection of intrahepatic cholangiocarcinoma: A 19-year experience from an established Australian hepatobiliary unit. J. Gastrointest. Surg. Off. J. Soc. Surg. Aliment. Tract 2010, 14, 1128–1138. [Google Scholar] [CrossRef]
- Hyder, O.; Marques, H.; Pulitano, C.; Marsh, J.W.; Alexandrescu, S.; Bauer, T.W.; Gamblin, T.C.; Sotiropoulos, G.C.; Paul, A.; Barroso, E.; et al. A nomogram to predict long-term survival after resection for intrahepatic cholangiocarcinoma: An Eastern and Western experience. JAMA Surg. 2014, 149, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Beetz, O.; Weigle, C.A.; Cammann, S.; Vondran, F.W.R.; Timrott, K.; Kulik, U.; Bektas, H.; Klempnauer, J.; Kleine, M.; Oldhafer, F. Preoperative leukocytosis and the resection severity index are independent risk factors for survival in patients with intrahepatic cholangiocarcinoma. Langenbeck’s Arch. Surg. 2020, 405, 977–988. [Google Scholar] [CrossRef]
- Bartsch, F.; Baumgart, J.; Hoppe-Lotichius, M.; Straub, B.K.; Heinrich, S.; Lang, H. Intrahepatic cholangiocarcinoma—Influence of resection margin and tumor distance to the liver capsule on survival. BMC Surg. 2020, 20, 61. [Google Scholar] [CrossRef]
- Ribero, D.; Pinna, A.D.; Guglielmi, A.; Ponti, A.; Nuzzo, G.; Giulini, S.M.; Aldrighetti, L.; Calise, F.; Gerunda, G.E.; Tomatis, M.; et al. Surgical Approach for Long-term Survival of Patients With Intrahepatic Cholangiocarcinoma: A Multi-institutional Analysis of 434 Patients. Arch. Surg. 2012, 147, 1107–1113. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.J.; Chun, Y.S. Intrahepatic cholangiocarcinoma: The AJCC/UICC 8th edition updates. Chin. Clin. Oncol. 2018, 7, 52. [Google Scholar] [CrossRef] [PubMed]
- Spolverato, G.; Bagante, F.; Weiss, M.; Alexandrescu, S.; Marques, H.P.; Aldrighetti, L.; Maithel, S.K.; Pulitano, C.; Bauer, T.W.; Shen, F.; et al. Comparative performances of the 7th and the 8th editions of the American Joint Committee on Cancer staging systems for intrahepatic cholangiocarcinoma. J. Surg. Oncol. 2017, 115, 696–703. [Google Scholar] [CrossRef]
- Sakamoto, Y.; Kokudo, N.; Matsuyama, Y.; Sakamoto, M.; Izumi, N.; Kadoya, M.; Kaneko, S.; Ku, Y.; Kudo, M.; Takayama, T.; et al. Proposal of a new staging system for intrahepatic cholangiocarcinoma: Analysis of surgical patients from a nationwide survey of the Liver Cancer Study Group of Japan. Cancer 2016, 122, 61–70. [Google Scholar] [CrossRef] [Green Version]
- Sapisochin, G.; Facciuto, M.; Rubbia-Brandt, L.; Marti, J.; Mehta, N.; Yao, F.Y.; Vibert, E.; Cherqui, D.; Grant, D.R.; Hernandez-Alejandro, R.; et al. Liver transplantation for very early intrahepatic cholangiocarcinoma: International retrospective study supporting a prospective assessment. Hepatology 2016, 64, 1178–1188. [Google Scholar] [CrossRef]
- Sapisochin, G.; Rodríguez de Lope, C.; Gastaca, M.; Ortiz de Urbina, J.; Suarez, M.A.; Santoyo, J.; Castroagudín, J.F.; Varo, E.; López-Andujar, R.; Palacios, F.; et al. Very early intrahepatic cholangiocarcinoma in cirrhotic patients: Should liver transplantation be reconsidered in these patients? Am. J. Transplant. 2014, 14, 660–667. [Google Scholar] [CrossRef]
- Molina, V.; Ferrer-Fábrega, J.; Sampson-Dávila, J.; Díaz, A.; Ayuso, C.; Forner, A.; Fondevila, C.; García-Valdecasas, J.C.; Bruix, J.; Fuster, J. Intention-to-treat curative liver resection in patients with "very early" intrahepatic cholangiocarcinoma. Langenbeck’s Arch. Surg. 2020, 405, 967–975. [Google Scholar] [CrossRef] [PubMed]
- Spolverato, G.; Ejaz, A.; Kim, Y.; Sotiropoulos, G.C.; Pau, A.; Alexandrescu, S.; Marques, H.; Pulitano, C.; Barroso, E.; Clary, B.M.; et al. Tumor size predicts vascular invasion and histologic grade among patients undergoing resection of intrahepatic cholangiocarcinoma. J. Gastrointest. Surg. 2014, 18, 1284–1291. [Google Scholar] [CrossRef]
- Kim, G.H.; Kim, P.H.; Kim, J.H.; Kim, P.N.; Won, H.J.; Shin, Y.M.; Choi, S.H. Thermal ablation in the treatment of intrahepatic cholangiocarcinoma: A systematic review and meta-analysis. Eur. Radiol. 2021, 1–11. [Google Scholar] [CrossRef]
- Kang, S.H.; Hwang, S.; Lee, Y.J.; Kim, K.H.; Ahn, C.S.; Moon, D.B.; Ha, T.Y.; Song, G.W.; Jung, D.H.; Lee, S.G. Prognostic comparison of the 7th and 8th editions of the American Joint Committee on Cancer staging system for intrahepatic cholangiocarcinoma. J. Hepato-Biliary-Pancreat. Sci. 2018, 25, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.M.; Clark, C.J.; Mounajjed, T.; Wu, T.T.; Harmsen, W.S.; Reid-Lombardo, K.M.; Truty, M.J.; Kendrick, M.L.; Farnell, M.B.; Nagorney, D.M.; et al. Model to predict survival after surgical resection of intrahepatic cholangiocarcinoma: The Mayo Clinic experience. HPB 2015, 17, 244–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doussot, A.; Gonen, M.; Wiggers, J.K.; Groot-Koerkamp, B.; DeMatteo, R.P.; Fuks, D.; Allen, P.J.; Farges, O.; Kingham, T.P.; Regimbeau, J.M.; et al. Recurrence Patterns and Disease-Free Survival after Resection of Intrahepatic Cholangiocarcinoma: Preoperative and Postoperative Prognostic Models. J. Am. Coll. Surg. 2016, 223, 493–505.e2. [Google Scholar] [CrossRef] [Green Version]
- Jin, B.; Hu, W.; Su, S.; Xu, H.; Lu, X.; Sang, X.; Yang, H.; Mao, Y.; Du, S. The Prognostic Value of Systemic Inflammation Response Index in Cholangiocarcinoma Patients. Cancer Manag. Res. 2021, 13, 6263–6277. [Google Scholar] [CrossRef]
- Altman, A.M.; Kizy, S.; Marmor, S.; Hui, J.Y.C.; Tuttle, T.M.; Jensen, E.H.; Denbo, J.W. Adjuvant chemotherapy for intrahepatic cholangiocarcinoma: Approaching clinical practice consensus? Hepatobiliary Surg. Nutr. 2020, 9, 577–586. [Google Scholar] [CrossRef]
- Nepal, C.; O’Rourke, C.J.; Oliveira, D.; Taranta, A.; Shema, S.; Gautam, P.; Calderaro, J.; Barbour, A.; Raggi, C.; Wennerberg, K.; et al. Genomic perturbations reveal distinct regulatory networks in intrahepatic cholangiocarcinoma. Hepatology 2018, 68, 949–963. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, H.; Arai, Y.; Totoki, Y.; Shirota, T.; Elzawahry, A.; Kato, M.; Hama, N.; Hosoda, F.; Urushidate, T.; Ohashi, S.; et al. Genomic spectra of biliary tract cancer. Nat. Genet. 2015, 47, 1003–1010. [Google Scholar] [CrossRef]
- Ruys, A.T.; Groot Koerkamp, B.; Wiggers, J.K.; Klümpen, H.J.; ten Kate, F.J.; van Gulik, T.M. Prognostic biomarkers in patients with resected cholangiocarcinoma: A systematic review and meta-analysis. Ann. Surg. Oncol. 2014, 21, 487–500. [Google Scholar] [CrossRef]
| Variables | “Very Early” ICC (Single Tumor ≤ 3 cm; n = 21) | “Advanced” ICC (n = 276) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| n (%) | Mean, Median (Range) | M.v. (n (%)) | n (%) | Mean, Median (Range) | M.v. (n (%)) | ||
| Biometrics | |||||||
| Age (in years) | 62.8, 62 (45–78) | 0 (0) | 61.6, 62 (24–84) | 0 (0) | 0.728 | ||
| Male | 17 (81.0) | 0 (0) | 138 (50.0) | 0 (0) | 0.006 | ||
| BMI (in kg/m2) | 25.9, 25.2 (19.2–38.2) | 0 (0) | 25.8, 25.2 (16.4–55.4) | 5 (1.8) | 0.962 | ||
| Preoperative data | |||||||
| Hemoglobin (in g/dL) | 13.6, 13.5 (10.7–16.4) | 0 (0) | 13.2, 13.4 (8.2–17.2) | 1 (0.4) | 0.359 | ||
| Leukocytes (×103/µL) | 6.8, 6.5 (3.6–14.4) | 0 (0) | 8.4, 7.9 (1.7–24.1) | 1 (0.4) | 0.003 | ||
| Platelets (×103/µL) | 257.5, 247 (134–495) | 0 (0) | 280.5, 255 (69–902) | 2 (0.7) | 0.322 | ||
| Quick (in %) | 98.9, 101 (67–120) | 0 (0) | 99.1, 100 (46–147) | 3 (1.1) | 0.924 | ||
| ASAT (in U/L) | 36.3, 30.5 (10–140) | 1 (4.8) | 39.5, 31 (4–304) | 6 (2.2) | 0.625 | ||
| Bilirubin (in µmol/L) | 15.2, 9 (4–100) | 0 (0) | 21.5, 9 (3–445) | 11 (4.0) | 0.902 | ||
| Creatinine (in µmol/L) | 71.1, 67 (46–102) | 0 (0) | 70.5, 66 (39–165) | 6 (2.2) | 0.598 | ||
| Primary sclerosing cholangitis | 2 (9.5) | 0 (0) | 7 (2.5) | 2 (0.7) | 0.128 | ||
| Surgical details | |||||||
| Operating times (in min) | 183.1, 175 (82–314) | 0 (0) | 205.5, 190 (67–780) | 4 (1.4) | 0.453 | ||
| Hepatic pedicle clamping | 16 (76.2) | 3 (14.3) | 215 (77.9) | 23 (8.3) | 1.000 | ||
| Hepatic pedicle clamping (in min) | 16.5, 17.5 (0–34) | 3 (14.3) | 22.8, 22 (0–110) | 24 (8.7) | 0.066 | ||
| Lymphadenectomy | 13 (61.9) | 0 (0) | 180 (65.2) | 0 (0) | 0.814 | ||
| Number of lymph nodes removed | 4.5, 3 (1–15) | 8 (38.1) | 5.1, 4 (1–23) | 97 (35.1) | 0.535 | ||
| Major hepatectomy | 14 (66.7) | 0 (0) | 229 (83.0) | 0 (0) | 0.077 | ||
| Extended hepatectomy | 1 (4.8) | 0 (0) | 101 (36.6) | 0 (0) | 0.003 | ||
| Perihilar bile duct resection | 5 (23.8) | 0 (0) | 53 (19.2) | 0 (0) | 0.574 | ||
| Vascular resection | 0 (0) | 0 (0) | 16 (5.8) | 0 (0) | 0.614 | ||
| Extrahepatic resection | 0 (0) | 0 (0) | 18 (6.5) | 0 (0) | 0.626 | ||
| Intraoperative transfusion | 6 (28.6) | 0 (0) | 135 (48.9) | 6 (2.2) | 0.071 | ||
| Intraoperative units of PRBC | 0.9, 0 (0–5) | 0 (0) | 2.1, 1 (0–17) | 6 (2.2) | 0.051 | ||
| Histopathological details | |||||||
| Tumor size (in cm) | 2.2, 2.5 (0.5–3.0) | 0 (0) | 7.9, 7.1 (0.9–21.0) | 1 (0.4) | <0.001 | ||
| Multifocality | 0 (0) | 0 (0) | 106 (38.4) | 0 (0) | 0.001 | ||
| Vascular invasion | 1 (4.8) | 7 (33.3) | 66 (23.9) | 102 (37.0) | 0.020 | ||
| N1 | 5 (23.8) | 8 (38.1) | 80 (29.0) | 96 (34.8) | 0.777 | ||
| M1 | 0 (0) | 0 (0) | 10 (3.6) | 0 (0) | 1.000 | ||
| G > 2 | 0 (0) | 0 (0) | 83 (30.1) | 5 (1.8) | 0.005 | ||
| R1 | 1 (4.8) | 1 (4.8) | 45 (16.3) | 7 (2.5) | 0.218 | ||
| Time Frame | Total Cases Resected (n = 297) | “Very early” ICC Resected (n = 21) | “Advanced” ICC Resected (n = 276) |
|---|---|---|---|
| 1996–2000 | 57 (19.2%) | 0 (0%) | 57 (20.7%) |
| 2001–2005 | 43 (14.5%) | 7 (16.3%) | 36 (13.0%) |
| 2006–2010 | 72 (24.2%) | 7 (9.7%) | 65 (23.6%) |
| 2011–2015 | 57 (19.2%) | 5 (8.8%) | 52 (18.8%) |
| 2016–2021 | 68 (22.9%) | 2 (2.9%) | 66 (23.9%) |
| Variables | “Very Early” ICC (Single Tumor ≤ 3 cm; n = 21) | “Advanced” ICC (n = 276) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| n (%) | Mean, Median (Range) | M.v. (n (%)) | n (%) | Mean, Median (Range) | M.v. (n (%)) | ||
| Postoperative course | |||||||
| Postoperative transfusion | 5 (23.8) | 0 (0) | 80 (29.0) | 10 (3.6) | 0.628 | ||
| Postoperative units of PRBC | 0.5, 0 (0–2) | 0 (0) | 1.6, 0 (0–29) | 10 (3.6) | 0.367 | ||
| Postoperative complications ≥ CD3 | 4 (19.0) | 0 (0) | 97 (35.1) | 2 (0.7) | 0.156 | ||
| Biliary leakage ISGLS Grade C | 1 (4.8) | 0 (0) | 12 (4.3) | 2 (0.7) | 1.000 | ||
| Hemorrhage ISGLS Grade C | 1 (4.8) | 0 (0) | 9 (3.3) | 2 (0.7) | 0.528 | ||
| PHLF ISGLS Grade C | 0 (0) | 0 (0) | 15 (5.4) | 2 (0.7) | 0.611 | ||
| ICU stay (in days) | 3.2, 2 (1–13) | 0 (0) | 4.7, 2 (0–91) | 0 (0) | 0.495 | ||
| Hospital stay (in days) | 21.4, 20 (7–43) | 0 (0) | 23.2, 20 (4–95) | 0 (0) | 0.792 | ||
| Intrahospital mortality | 0 (0) | 0 (0) | 21 (7.6) | 0 (0) | 0.379 | ||
| 30-day mortality | 0 (0) | 0 (0) | 13 (4.7) | 4 (1.4) | 0.609 | ||
| 90-day mortality | 0 (0) | 0 (0) | 25 (9.1) | 5 (1.8) | 0.234 | ||
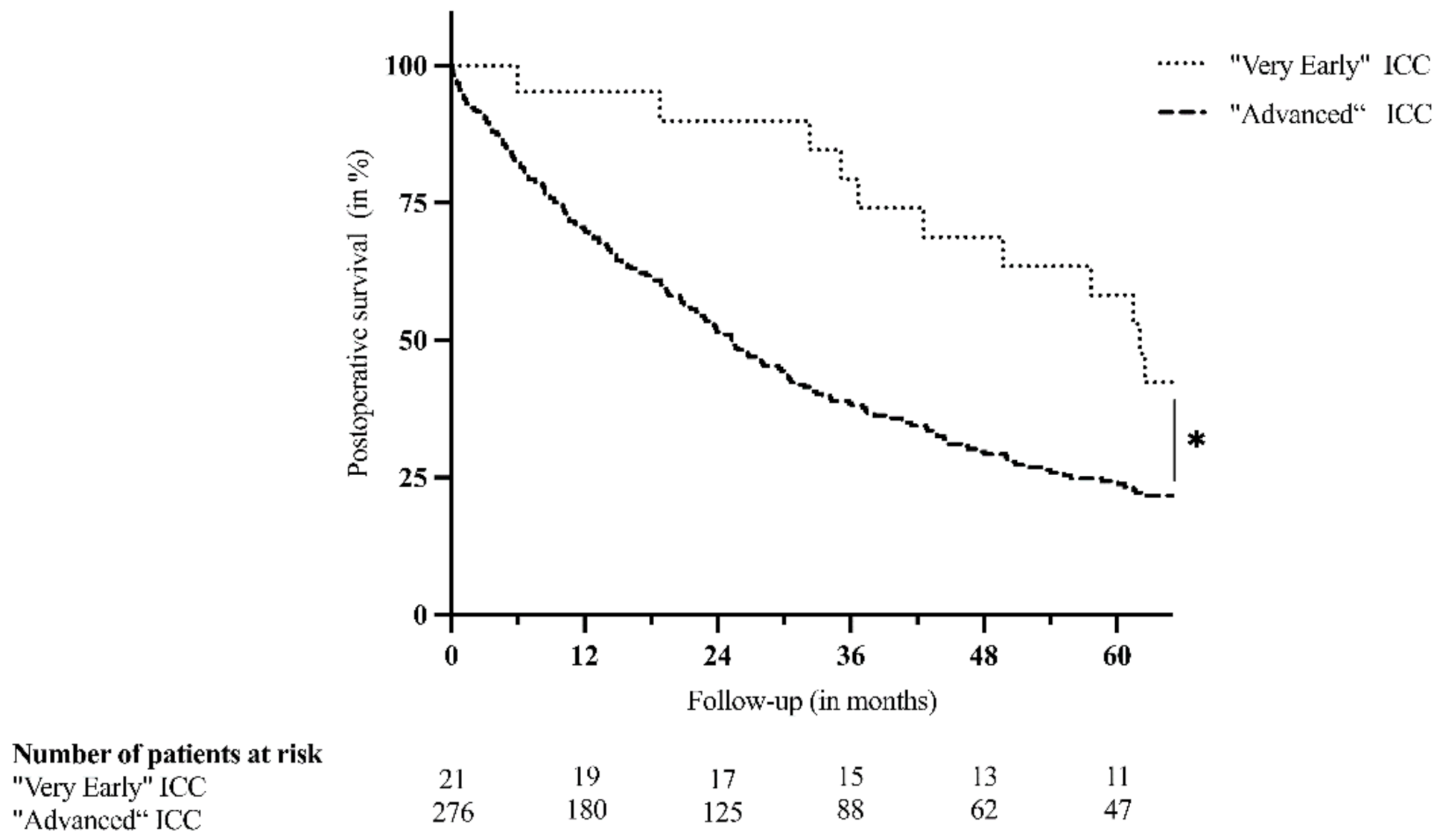
| Postoperative survival | |||||||
| Follow-up (in months) | 66.8, 61.5 (5.9–165.8) | 0 (0) | 37.0, 20.8 (0.1–301.7) | 0 (0) | <0.001 | ||
| Dead at time of last follow-up | 15 (71.4) | 0 (0) | 218 (79.0) | 0 (0) | 0.414 | ||
| KM Survival | 80.0, 62.1 (n.a.) | 0 (0) | 51.3, 25.3 (n.a.) | 0 (0) | 0.013 | ||
| KM 1-year survival (in %) | 95.2 | 0 (0) | 70.1 | 0 (0) | n.a. | ||
| KM 3-year survival (in %) | 79.4 | 0 (0) | 38.5 | 0 (0) | n.a. | ||
| KM 5-year survival (in %) | 58.2 | 0 (0) | 24.3 | 0 (0) | n.a. | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beetz, O.; Timrott, A.; Weigle, C.A.; Schroeter, A.; Cammann, S.; Klempnauer, J.; Vondran, F.W.R.; Oldhafer, F. Proposal of a New Definition of “Very Early” Intrahepatic Cholangiocarcinoma—A Retrospective Single-Center Analysis. J. Clin. Med. 2021, 10, 4073. https://doi.org/10.3390/jcm10184073
Beetz O, Timrott A, Weigle CA, Schroeter A, Cammann S, Klempnauer J, Vondran FWR, Oldhafer F. Proposal of a New Definition of “Very Early” Intrahepatic Cholangiocarcinoma—A Retrospective Single-Center Analysis. Journal of Clinical Medicine. 2021; 10(18):4073. https://doi.org/10.3390/jcm10184073
Chicago/Turabian StyleBeetz, Oliver, Angelica Timrott, Clara A. Weigle, Andreas Schroeter, Sebastian Cammann, Juergen Klempnauer, Florian W. R. Vondran, and Felix Oldhafer. 2021. "Proposal of a New Definition of “Very Early” Intrahepatic Cholangiocarcinoma—A Retrospective Single-Center Analysis" Journal of Clinical Medicine 10, no. 18: 4073. https://doi.org/10.3390/jcm10184073
APA StyleBeetz, O., Timrott, A., Weigle, C. A., Schroeter, A., Cammann, S., Klempnauer, J., Vondran, F. W. R., & Oldhafer, F. (2021). Proposal of a New Definition of “Very Early” Intrahepatic Cholangiocarcinoma—A Retrospective Single-Center Analysis. Journal of Clinical Medicine, 10(18), 4073. https://doi.org/10.3390/jcm10184073





