Challenges and Controversies in the Surgical Treatment of Cervical Cancer: Open Radical Hysterectomy versus Minimally Invasive Radical Hysterectomy
Abstract
:1. Introduction
2. Methods
2.1. Study Selection
- Population: patients with early-stage cervical cancer
- Intervention/comparator: ORH, MIS, robotic radical hysterectomy (RRH), and/or laparoscopic radical hysterectomy (LRH)
- Outcomes: overall survival (OS), disease-free survival (DFS), measures of surgery (e.g., operating time, blood loss, length of hospital stay), rates of intra and postoperative complications
- Study design: systematic reviews (SRs), meta-analyses, literature reviews, and randomized controlled trials (RCTs)
2.2. Searches
2.3. Data Extraction
2.4. Reviewing Expert Opinions from Large-Volume Centers
2.5. Quality (Risk of Bias) Assessment
2.6. Data Synthesis
3. Results
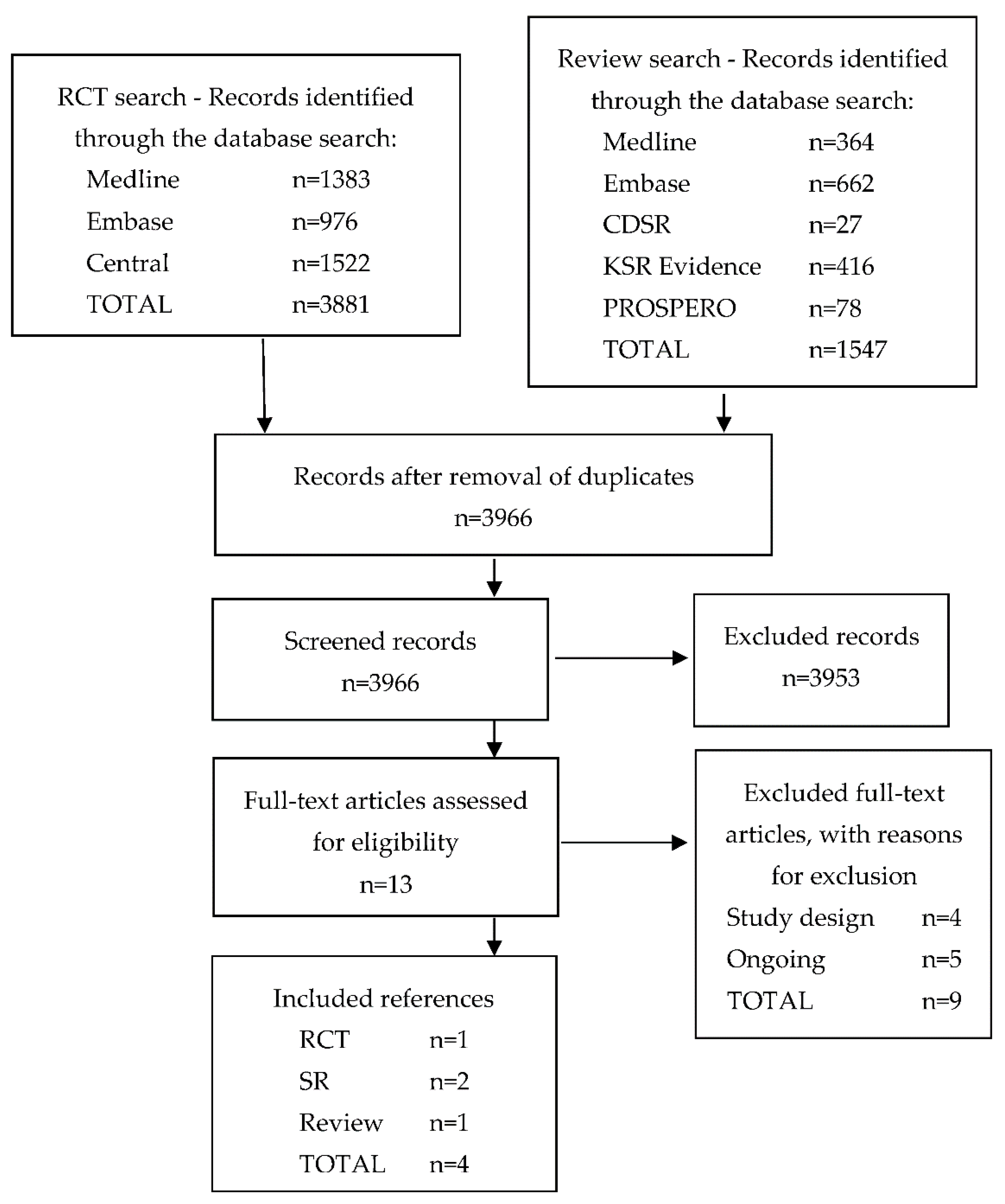
3.1. Literature Searches and Inclusion Assessment
3.2. Overview of Included References
3.3. Methods of LACC Trial
3.4. Results of the LACC Trial
3.5. Overview of the Results
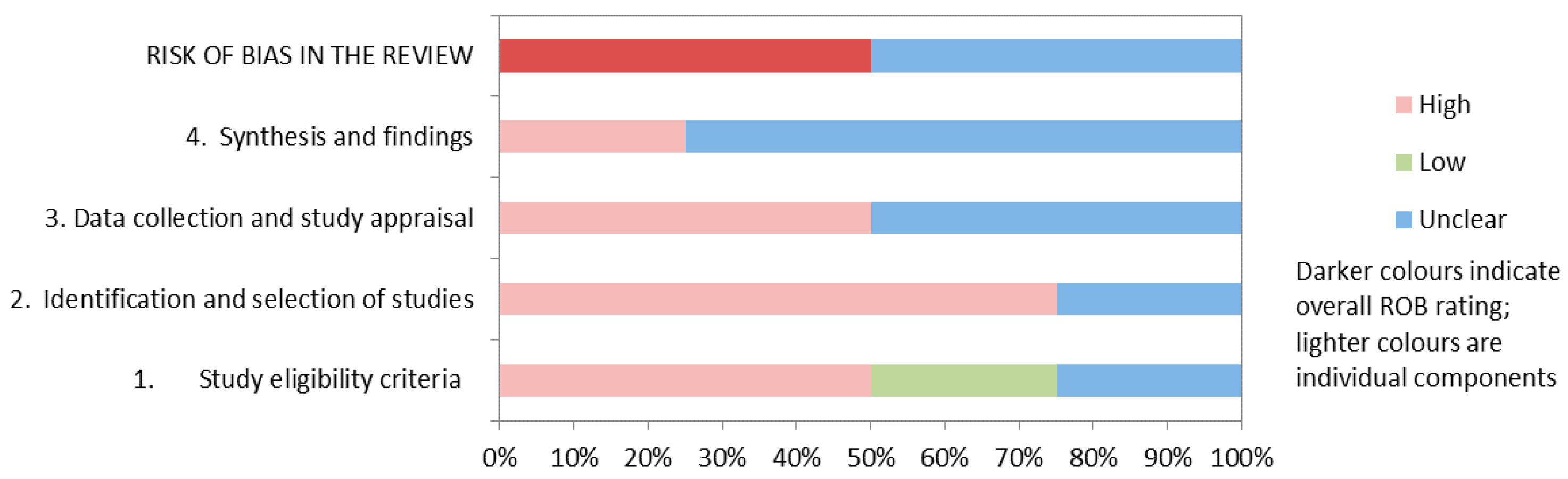
3.6. Risk of Bias
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. Responses by Clinical Experts
Appendix A.1.1. Professor D. Bauerschlag, University Hospital Schleswig-Holstein, Campus Kiel, Germany
- Based on my experience I do overview by fare more minimal invasive procedures than open radicals. However, I cannot report any differences in survival regarding the technique used.
- Although the LACC trail is a multicenter randomized trial it has some caveats lowering the power of its results. But since it is Level Ib evidence one should be cautious not considering these results when discussing the surgical procedure with the patient. To me the results of LACC overweigh the results from mostly retrospective observational studies.
- Patients need to be informed about the results of LACC during the informed consent procedure prior to treatment. Having said that, I would perform robotic assisted minimal invasive surgery in cases such as ≤FIGO Ia2, no evidence of lymphvascular invasion and no adenocarcinoma differentiation. Furthermore, we do have to inform the patient that radio-therapy is a valid option curing patients from low stage cervical cancer.
- To me local recurrences within the lower pelvis, explicitly in the area of the internal iliac artery seems higher to me in minimal invasive surgery.
- I doubt that CO2 plays a role in cell proliferation. However, I can imagine that the increased intra-abdominal pressure could potentially affect the tumor cell that way that residual cells are pushed into niches.
- The facts are weakening the LACC results but overall the results seem to be reliable.
Appendix A.1.2. Professor H. Ferreira, University Hospital Center of, Portugal
- The LACC trial outcomes should be taken into account critically and meticulously compared with other scientific validated studies that several oncological referral centres have already published. It may have a problematic premise and surgeon bias. The LACC trial seems to have methodology limitations, and the inclusion criteria are questionable (pe. surgeon proficiency criteria for minimally invasive surgery in the trial were only 10 cases and a total of 2 un-edited videos; the participation of countries where minimally invasive surgery has become the treatment of choice was low, and the LACC trial did not report the operational technique, etc.). The surgical related morbidity and mortality may be worse in the laparotomy arm. There is missing data in the LACC trial like surgical cohorts well balanced for all demographic variables, all tumours variables, stage, the overall number of lymph nodes removed, number of positive lymph nodes, post-treatment receipt of adjuvant radiation and chemotherapy, …
- After the LACC trial, we developed a new informed consent form in the department. The patients should be clearly informed and allowed to choose. If patients consent, we offer a minimally invasive surgical approach in cases of squamous cell carcinoma in stage IB1 cervical cancer with tumour size ≤ 2 cm. We’ve implemented routine vaginal closure before colpotomy (vaginal cuff from below, by laparoscopy using a linear stapler).
- Our data and covering intra-operative complications do not report any significant difference between radical laparoscopic hysterectomy and open radical hysterectomy. Concerning postoperative complications, they have been more common in the open radical hysterectomy group (namely urinary retention, sexual and bowel dysfunction). Probably, because by laparoscopic/robotics approach, it is possible to identify better the anatomy, and a nerve-sparing approach is more feasible. Seeing better, we also can treat better. The pneumodissection offered by laparoscopy/robotics facilitates the access of the retroperitoneal space, where the lymphatic nodes are located.
- With a well-trained team and following the standard steps, MIS enhances the pelvic lymph node dissection. The surgeon has a better anatomical vision by laparoscopy or robotics and can be more efficient in the lymphatic tissue excision respecting anatomical and surgical landmarks. The precision offered by laparoscopy/robotics allows a more precise approach, sparing the nerves, the small vessels and even, in some cases, the lymphatics (eventually causing less lymphedema/lymphocysts).
Appendix A.1.3. Professor P. Hillemanns, University Hospital Hannover, Germany
- The LACC study is a large international randomized study that included 631 patients in around 33 centres (USA, Central/South America, Eastern Europe, Australia, China, etc.).The question was whether laparoscopic radical hysterectomy is not inferior to open surgery. The study was terminated early because the data security committee showed a significant superiority of open surgery. The study is very informative regarding the question of which surgical procedure is better for early cervical cancer of up to 4 cm size. Due to the study design with randomization and multicentre approach in connection with the number of different design (retrospective, comparison with historical cohorts, one-arm studies, register and population avaluations).
- Based on the reported funding of $121.250 from Medtronic in the original publication, it must be doubted that sufficient funding for management, data collection and quality assurance with appropriate validation of the many parameters was possible.
- The main point of criticism, in my opinion, is the failure to observational studies from the last two years, can have a significant influence on tumour cell dissemination and thus on the locoregional recurrence rate in laparoscopic radical hysterectomy. In particular, the use of the uterine manipulator and abdominal colpotomy are associated with an increased risk. The formation of a vaginal cuff over the portio is another protective maneuver.
- The brief follow-up observation of the study can in principle be viewed as a point of criticism. It was shown that in the study evaluation in 2019, i.e., one year after the publication in the NEJM the HR decreased from 6.0 to 2.9. However, the differences are still clearly significant!
- Some critics question the operative expertise of the respective centres, especially with reference to the learning curve of laparoscopic radical hysterectomy, which became established as a routine procedure worldwide only a few years before the start of the study.
- I am convinced that the validity of the only larger randomized multicentre study to date is very high and with regard to its evidence, outweighs the retrospective observational studies. The results of the retrospective observational studies are, however, generating hypotheses, so that, in my opinion, further larger multicentre randomized studies should urgently be initiated.
- In everyday clinical practice, our patients are very openly informed about the two methodological approaches in the treatment of early cervical cancer. We point out that the LACC study has the highest informative value and emphasize the significantly better results in terms of overall survival and disease-free survival. However, we also mention the operational and technical points of criticism of the study and refer to the publications by Professor Köhler and my senior physician, Professor Hertel, in the International Journal of Gynaecology Cancer 2019 and to the results of the SUCCOR study (Chiva, 2019). The retrospective evaluation of our laparoscopic radical hysterectomy compared to open surgery yielded similar high DFS/OS rates compared to the open LARRarm and the Köhler and Chiva-protectivemaneuver-arms.Nevertheless, we stress the power of an RCT in this question about the operative approach.
Appendix A.1.4. Professor N. Maass, University Hospital Schleswig-Holstein, Campus Kiel, Germany
- During the last ten years, we didn’t notice any difference between the two approaches in University Hospital Kiel, although we didn’t collect out data. In University Hospital Aachen, Germany in the early 2000s we noticed a difference. But at that time, we could not define the reason for the worse outcome after the minimally invasive surgery.
- The LACC trial by Ramirez et al. was a very well performed and well-structured study. The medical centres taking part had a high standard. We have to take the results seriously although smaller, mostly retrospective studies, inferior to the LACC trial, showed different results. In my opinion, every medical centre must keep an eye on their own outcome data.
- I don’t think, that the different experience of the involved surgeons had an outstanding impact on the results of the LACC trial. The effect on the outcome was remarkable even with well trained and very experienced surgeons. The usage of the uterine manipulator might be one of the main reasons for the worse outcome data after minimally invasive surgery. One could easily imagine that tumour cells might migrate into the pelvis once the tumour is broken by the manipulator. Data from Köhler et al. support that concept.
- Trocar metastasis as well as CO2 must be considered as possible reasons for the worse outcome data after MIC.
- After the publication of the LACC trial one must inform the patient very well about the existing data and based on that, one should perform a shared decision making considering the advantages and disadvantages of both approaches. For patients with tumours > 2 cm we must offer the open radical hysterectomy, based on the findings of Ramirez et al. And one should avoid the uterine manipulator.
Appendix A.1.5. Dr. M. Elessawy, University Hospital Schleswig-Holstein, Campus Kiel, Germany
- The critical factor with the level of the experience of the surgeons remain underestimated in the literature, one of the drawbacks of the LACC trial is the absence of a unique parameter for the inclusion of the surgeons and difficulty to reach a unique evaluation of the quality of the surgery performed.Moreover, the different number of dissected pelvic lymph nodes with in the surgery shows the need for a universal definition, however the risks profile and the cofactors are different from one case to the other.The role presented by the Co2 demands a detailed investigation in the near future, however it increases the propensity for cervical cancer to implant.The uterine manipulator plays a role for increasing the recurrence rate at the vaginal vault, probably through invasion of the vaginal mucosa, resulting in the spread and spillage of the tumour cells.
- Since the publication of the results of the LACC study, we perform a detailed consultation of the patients showing the results published by the LACC study and the discrepancy to our individual results. The decision for the surgery is based on shared decision making with the help of decision panels which shows the different literature and experience. I emphasise the unknown role of the manipulator and the fact that also non vaginal vault pelvic recurrences occurred in the minimally invasive surgery group.The importance to have a standard uniform adequate staging examination of the patients before planning the entire treatment in order to avoid the discrepancy and the heterogenicity by risk of recurrence, which is one of the drawbacks of the LACC study, with variation and sometimes lack of presurgical assessment of the staging examination.The need for a more detailed decisions aid presented by the oncology society would results in a more confidence at the process of decision making and avoid any sort of prevalence by the centres, which emphasize the need to organize more training sessions to improve and retrain the training skills of the medical personals to perform those sophisticated consultation.
| Studies | Greggi 2020 [20] | Zhang 2019 [22] | Zhao 2017 [21] |
|---|---|---|---|
| Abu-Rustum 2003 Gynecol Oncol | ✓ | ||
| Asciutto 2015 Acta Obstet Gynecol Scand | ✓ | ||
| Boggess 2008 Am J Obstet Gynecol | ✓ | ||
| Cao 2015 J Laparoendoc Adv Surg Tech A | ✓ | ||
| Chen 2012 J Sanxi Med Univ | ✓ | ||
| Chen 2014 Int J Gynecol Cancer | ✓ | ||
| Chiva 2019 ESGO conference | ✓ | ||
| Choi 2012 Ann Surg Oncol | ✓ | ||
| Chong 2013 Int J Gynecol Cancer | ✓ | ||
| Corrado 2016 Int J Gynecol Cancer | ✓ | ||
| Corrado 2018 Int J Gynecol Cancer | ✓ | ||
| Cusimano 2019 Am J Obstet Gynecol | ✓ | ||
| Dao 2012 Matern Child Health Care China | ✓ | ||
| Desille 2013 Eur J Obstet Gynecol Reprod Biol | ✓ | ||
| Diaz- Feijoo 2014 Gynecol Oncol | ✓ | ||
| Ditto 2015 Eur J Surg Oncol | ✓ | ✓ | |
| Diver 2017 J Minim Invasive Gynecol | ✓ | ✓ | |
| Doo 2019 Gynecol Oncol | ✓ | ||
| Estape 2009 Gynecol Oncol | ✓ | ✓ | |
| Frumovitz 2007 Obstet Gynecol | ✓ | ||
| Geisler 2010 Int J Gynecol CancerV | ✓ | ||
| Ghezzi 2007 Gynecol Oncol | ✓ | ||
| Gil-Moreno 2019 J Minim Invasive Gynecol | ✓ | ||
| Guo 2018 Onco Targets Ther | ✓ | ||
| Kim 2019 Cancer Res Treat | ✓ | ||
| Kim 2019a Gynecol Oncol | ✓ | ||
| Kim 2019b Gynecol Oncol | ✓ | ||
| Kim JY 2015 Anticancer Res | ✓ | ||
| Kim TH 2015 Anticancer Res | ✓ | ||
| Ko 2008 Gynecol Oncol | ✓ | ||
| Kong 2014 Int J Gynecol Cancer | ✓ | ||
| Lambaudie 2010 Eur J Surg Oncol | ✓ | ||
| Laterza 2016 Int J Gynecol Cancer | ✓ | ||
| Lee 2011 Eur J Obstet Gynecol Reprod Biol | ✓ | ✓ | |
| Li 2013 Shaanxi Med J | ✓ | ||
| Lim 2019 Gynecol Minim Invasive Ther | ✓ | ||
| Malzoni 2009 Ann Surg Oncol | ✓ | ✓ | |
| Melamed 2018 N Eng J Med | ✓ | ||
| Mendivil 2016 Surg Oncol | ✓ | ✓ | |
| Nam 2010 Int J Gynecol Cancer | ✓ | ||
| Nam 2012 Ann Oncol | ✓ | ||
| Nezhat 1992 Am J Obstet Gynecol | ✓ | ||
| Paik 2019 Gynecol Oncol | ✓ | ||
| Park 2013 J Surg Oncol | ✓ | ||
| Pellegrino 2017 Acta Biomed | ✓ | ||
| Sert 2011 Gynecol Oncol | ✓ | ✓ | |
| Sert 2016 Eur J Surg Oncol | ✓ | ✓ | |
| Shah 2017 J Gynecol Oncol | ✓ | ||
| Simsek 2011 Eur J Gynaecol Oncol | ✓ | ||
| Soliman 2011 Gynecol Oncol | ✓ | ✓ | |
| Tinelli 2011 Ann Surg Oncol | ✓ | ||
| Toptas 2014 J Laparoendosc Adv Surg Tech A | ✓ | ||
| Uccella 2007 Gynecol Oncol | ✓ | ||
| Uppal 2019 J Clin Oncol | ✓ | ||
| Vizzielli 2016 J Minim Invasive Gynecol | ✓ | ||
| Wang 2015 BMC Cancer | ✓ | ||
| Wright 2012 Gynecol Oncol | ✓ | ||
| Xiong 2013 Mod Med J China | ✓ | ||
| Yim 2014 Yonsei Med J | ✓ | ||
| Zanagnolo 2016 Int J Gynecol Cancer | ✓ | ||
| Zhao 2017 J Laparoendosc Adv Surg Tech A | ✓ | ||
| Zhu 2013 Zhejiang J Trauma Surg | ✓ | ||
| Zhu 2015 Henan J Surg | ✓ |
References
- Ramirez, P.T.; Frumovitz, M.; Pareja, R.; Lopez, A.; Vieira, M.; Ribeiro, R.; Buda, A.; Yan, X.; Shuzhong, Y.; Chetty, N.; et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N. Engl. J. Med. 2018, 379, 1895–1904. [Google Scholar] [CrossRef]
- Huscher, C.G.; Mingoli, A.; Sgarzini, G.; Sansonetti, A.; Di Paola, M.; Recher, A.; Ponzano, C. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: Five-year results of a randomized prospective trial. Ann. Surg 2005, 241, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Lacy, A.M.; García-Valdecasas, J.C.; Delgado, S.; Castells, A.; Taurá, P.; Piqué, J.M.; Visa, J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: A randomised trial. Lancet 2002, 359, 2224–2229. [Google Scholar] [CrossRef]
- Nelson, H.; Sargent, D.J.; Wieand, H.S.; Fleshman, J.; Anvari, M.; Stryker, S.J.; Beart, R.W., Jr.; Hellinger, M.; Flanagan, R., Jr.; Peters, W.; et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N. Engl. J. Med. 2004, 350, 2050–2059. [Google Scholar] [CrossRef]
- Walker, J.L.; Piedmonte, M.R.; Spirtos, N.M.; Eisenkop, S.M.; Schlaerth, J.B.; Mannel, R.S.; Barakat, R.; Pearl, M.L.; Sharma, S.K. Recurrence and survival after random assignment to laparoscopy versus laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group LAP2 Study. J. Clin. Oncol. 2012, 30, 695–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marth, C.; Landoni, F.; Mahner, S.; McCormack, M.; Gonzalez-Martin, A.; Colombo, N. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, vii27–vii32. [Google Scholar] [CrossRef] [PubMed]
- ESMO Guidelines Committee. eUpdate—Cervical Cancer Treatment Recommendations: Management of Local/Locoregional Disease; Primary Treatment (Clinical Practice Guidelines) [Internet]; European Society for Medical Oncology: Lugano, Switzerland, 2020. [Google Scholar]
- Hillemanns, P.; Brucker, S.; Holthaus, B.; Kimmig, R.; Lampe, B.; Runnebaum, I.; Ulrich, U.; Wallwiener, M.; Fehm, T.; Tempfer, C.; et al. Updated opinion of the uterus commission of the gynecological oncology working group (AGO) and the gynecological endoscopy working group (AGE) of the German society of gynecology and obstetrics (DGGG) on the randomized study comparing minimally invasive with abdominal radical hysterectomy for early-stage cervical cancer (LACC). Geburtshilfe Frauenheilkd 2019, 79, 145–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nezhat, F.R.; Ananth, C.V.; Vintzileos, A.M. The two Achilles heels of surgical randomized controlled trials: Differences in surgical skills and reporting of average performance. Am. J. Obstet. Gynecol. 2019, 221, 230–232. [Google Scholar] [CrossRef]
- Park, J.Y.; Nam, J.H. How should gynecologic oncologists react to the unexpected results of LACC trial? J. Gynecol. Oncol. 2018, 29, e74. [Google Scholar] [CrossRef] [PubMed]
- Jensen, P.T.; Schnack, T.H.; Froding, L.P.; Bjorn, S.F.; Lajer, H.; Markauskas, A.; Jochumsen, K.M.; Fuglsang, K.; Dinesen, J.; Sogaard, C.H.; et al. Survival after a nationwide adoption of robotic minimally invasive surgery for early-stage cervical cancer —A population-based study. Eur. J. Cancer 2020, 128, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions [Internet]; The Cochrane Collaboration: Oxford, UK, 2011. [Google Scholar] [CrossRef] [Green Version]
- Centre for Reviews and Dissemination. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care [Internet]; University of York: York, UK, 2009. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whiting, P.; Savovic, J.; Higgins, J.P.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 2016, 69, 225–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obermair, A.; Asher, R.; Frumovitz, M.; Pareja, R.; Lopez, A.; Viera, M.; Ribeiro, R.; Buda, A.; Yan, X.; Robledo, K.P.; et al. Incidence of adverse events comparing abdominal vs. minimally invasive radical hysterectomy in patients with early-stage cervical cancer: LACC trial. In Proceedings of the 17th Biennial Meeting of the International Gynecologic Cancer Society (IGCS), Kyoto, Japan, 14–16 September 2018. [Google Scholar]
- Ramirez, P.T.; Obermair, A.; Frumovitz, M.; Gebski, V. A Phase III Randomized Clinical Trial Comparing Laparoscopic or Robotic Radical Hysterectomy Versus Abdominal Radical Hysterectomy in Patients with Early Stage Cervical Cancer: Study Protocol (Version 4) [PDF Provided by the Author]; University of Texas M.D. Anderson Cancer Center: Houston, TX, USA, 2014; p. 105. [Google Scholar]
- Greggi, S.; Casella, G.; Scala, F.; Falcone, F.; Visconti, S.; Scaffa, C. Surgical management of early cervical cancer: When is laparoscopic appropriate? Curr. Oncol. Rep. 2020, 22, 7. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Hang, B.; Xiong, G.-W.; Zhang, X.-W. Laparoscopic radical hysterectomy in early stage cervical cancer: A systematic review and meta-analysis. J. Laparoendosc. Adv. Surg. Tech. 2017, 27, 1132–1144. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.-S.; Ding, T.; Cui, Z.-H.; Lv, Y.; Jiang, R.-A. Efficacy of robotic radical hysterectomy for cervical cancer compared with that of open and laparoscopic surgery: A separate meta-analysis of high-quality studies. Medicine 2019, 98, e14171. [Google Scholar] [CrossRef]
- Obermair, A.; Asher, R.; Pareja, R.; Frumovitz, M.; Lopez, A.; Moretti-Marques, R.; Rendon, G.; Ribeiro, R.; Tsunoda, A.; Behan, V.; et al. Incidence of adverse events in minimally invasive vs open radical hysterectomy in early cervical cancer: Results of a randomized controlled trial. Am. J. Obstet. Gynecol. 2020, 222, 249. [Google Scholar] [CrossRef]
- Cairo, F.; Carnevale, G.; Buti, J.; Nieri, M.; Mervelt, J.; Tonelli, P.; Pagavino, G.; Tonetti, M. Soft-tissue re-growth following fibre retention osseous resective surgery or osseous resective surgery: A multilevel analysis. J. Clin. Periodontol. 2015, 42, 373–379. [Google Scholar] [CrossRef]
- Purwanti, L.; Numthavaj, P.; Charakorn, C.; Thakkinstian, A. Network meta-analysis of survival outcomes between open, laparoscopic and robotic surgery in the early stages of cervical cancer. In Proceedings of the 6th Annual International Conference on New Voices in Global Health and Development, Pathumthani, Thailand, 5 April 2019. [Google Scholar]
- Choi, C.H.; Lee, J.W.; Lee, Y.Y.; Kim, H.J.; Song, T.; Kim, M.K.; Kim, T.J.; Kim, B.G.; Bae, D.S. Comparison of laparoscopic-assisted radical vaginal hysterectomy and laparoscopic radical hysterectomy in the treatment of cervical cancer. Ann. Surg. Oncol. 2012, 19, 3839–3848. [Google Scholar] [CrossRef]
- Kong, T.W.; Chang, S.J.; Piao, X.; Paek, J.; Lee, Y.; Lee, E.J.; Chun, M.; Ryu, H.S. Patterns of recurrence and survival after abdominal versus laparoscopic/robotic radical hysterectomy in patients with early cervical cancer. J. Obstet. Gynaecol. Res. 2016, 42, 77–86. [Google Scholar] [CrossRef]
- Chiva, L.; Zanagnolo, V.; Querleu, D.; Martin-Calvo, N.; Arévalo-Serrano, J.; Căpîlna, M.E.; Fagotti, A.; Kucukmetin, A.; Mom, C.; Chakalova, G.; et al. SUCCOR study: An international European cohort observational study comparing minimally invasive surgery versus open abdominal radical hysterectomy in patients with stage IB1 cervical cancer. Int. J. Gynecol. Cancer 2020, 30, 1269–1277. [Google Scholar] [CrossRef] [PubMed]
- Uppal, S.; Gehrig, P.A.; Peng, K.; Bixel, K.L.; Matsuo, K.; Vetter, M.H.; Davidson, B.A.; Cisa, M.P.; Lees, B.F.; Brunette, L.L.; et al. Recurrence rates in patients with cervical cancer treated with abdominal versus minimally invasive radical hysterectomy: A multi-institutional retrospective review study. J. Clin. Oncol. 2020, 38, 1030–1040. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, H.H.B.; Smolders, R.G.V.; Beltman, J.J.; Lambrechts, S.; Trum, H.W.; Yigit, R.; Zusterzeel, P.L.M.; Zweemer, R.P.; Mom, C.H.; Bekkers, R.L.M.; et al. Survival of patients with early-stage cervical cancer after abdominal or laparoscopic radical hysterectomy: A nationwide cohort study and literature review. Eur. J. Cancer 2020, 133, 14–21. [Google Scholar] [CrossRef]
- Kohler, C.; Hertel, H.; Herrmann, J.; Marnitz, S.; Mallmann, P.; Favero, G.; Plaikner, A.; Martus, P.; Gajda, M.; Schneider, A. Laparoscopic radical hysterectomy with transvaginal closure of vaginal cuff—A multicenter analysis. Int. J. Gynecol. Cancer 2019, 29, 845–850. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef] [PubMed]
| Outcome | MIS | ORH | MIS vs. ORH (95% CI) |
|---|---|---|---|
| Intention to treat (ITT) | n = 319 | n = 312 | |
| DFS at 4.5 years (%) (95% CI) | 86.0 (79.7 to 90.4) | 96.5 (92.7 to 98.4) | −10.6 (−16.4 to −4.7) * |
| Disease recurrence or death from cervical cancer; n (%) | 27 (8.5) | 7 (2.2) | HR 3.74 (1.63 to 8.58) ** |
| Disease recurrence or death from any cause (PFS); n (%) | 32 (10.0) | 8 (2.6) | HR 3.88 (1.79 to 8.41) |
| Locoregional recurrence; n (%) | 18 (5.6) | 4 (1.3) | HR 4.26 (1.44 to 12.60) |
| Death from any cause; n (%) | 19 (6.0) | 3 (1.0) | HR 6.00 (1.77 to 20.30) |
| Death from cervical cancer; n (%) | 14 (4.4) | 2 (0.6) | HR 6.56 (1.48 to 29.00) |
| Per-protocol (PP) | |||
| DFS at 4.5 years; (%) (95% CI), n = 289 | 87.1 (81.0 to 91.3) | 97.6 (94.1 to 99.0) | −10.5 (−16.0 to −5.0) |
| Laparoscopic only; (%) (95% CI), n = 244 | 87.0 (80.5 to 91.5) | 97.6 (94.1 to 99.0) | −10.6 (−16.4 to −4.7) |
| Robotic only; (%) (95% CI), n = 45 | 87.2 (64.0 to 95.9) | 97.6 (94.1 to 99.0) | −10.4 (−24.7 to 3.9) |
| Outcome | MIS (n = 279) | ORH (n = 257) | MIS vs. ORH (95% CI) |
|---|---|---|---|
| Any AE; n (%) | 164 (59) | 136 (53) | 5.9 (−2.5 to 14.3) |
| Intraoperative AE; n (%) | 34 (12) | 26 (10) | 2.1 (−3.3 to 7.4) |
| Postoperative AE; n (%) | 152 (54) | 124 (48) | 6.3 (−2.2 to 14.7) |
| Major AE; n (%) | 50 (18) | 41 (16) | 2.0 (−4.4 to 8.3) |
| Serious AE; n (%) | 39 (14) | 30 (12) | 2.3 (−3.3 to 8.0) |
| Duration of surgery (min); geometric mean (range) | 216 (75 to 441) | 187 (61 to 425) | p < 0.001 * |
| Estimated blood loss (mL); geometric mean (range) | 101 (10 to 1500) | 209 (10 to 2200) | p < 0.001 * |
| Length of hospital stay (days); median (range) | 3 (0 to 72) | 5 (1 to 69) | p = 0.002 * |
| Greggi 2020 [20] | Zhang 2019 [22] | Zhao 2017 [21] | |
|---|---|---|---|
| Search dates | NR * | February 2018 | February 2016 |
| Databases | NR * | Pubmed, Embase, Cochrane Library, and Web of Science English only | Medline, Web of Knowledge, Cochrane Library, and Chinese National Knowledge Infrastructure No language restrictions |
| Population | Cervical cancer (stage IA1 to stage IB) | Cervical cancer Studies in patients with malignant gynecological lesions other than cervical cancer were excluded. | Cervical cancer stage IA1 to IIA treated with radical hysterectomy with or without lymphadenectomy Radical trachelectomy, radical vaginal hysterectomy, abdominal assisted vaginal hysterectomy, and recurrent cervical cancer cases were excluded |
| Intervention | MIS | RRH | LRH |
| Comparators | ORH | LRH and ORH | ORH (abdominal) |
| Outcomes prespecified | NR * | Surgical outcomes (not specified) | Intra and postoperative outcomes (listed in outcomes reported) |
| Study designs | NR * | Prospective and retrospective cohort | Prospective and retrospective comparative |
| Quality assessment | NR | MINORS and Newcastle–Ottawa scale (only MINORS was reported and used to select studies for the meta-analysis, scores < 12 were excluded) | Newcastle–Ottawa scale |
| Number of studies | 24 (MIS vs. ORH 5, LRH vs. ORH 14, RRH vs. ORH 3, LRH vs. RRH vs. ORH 2) | 25, 13 included in MA (RRH vs. ORH 4, RRH vs. LRH 6, RRH vs. LRH or ORH 3) | 23 |
| Study design | MA (3), retrospective (17) and prospective (1) observational studies, epidemiological studies (3) | Cohort (9, with no details) Matched (4, with no details) | RCT (1), prospective (2), retrospective (matched case–control 2), retrospective (18) |
| Outcomes reported | DFS, OS, recurrence rate | DFS, OS, operating time, blood loss, transfusion, conversion, intraoperative complications, postoperative complications, length of hospital stay, retrieved lymph nodes, recurrence | Operating time, blood loss, transfusion rate, length of hospital stay, return to normal bowel activity, duration of bladder catheterization, intestinal injury, retrieved lymph nodes, length of follow-up, recurrence, specific types of complications and injury |
| Conclusion | ORH should be considered the standard of care. Patients should be counseled carefully before MIS, which can be considered safe only for sentinel lymph node mapping in a fertility-sparing setting and could be considered after preoperative conization and for small tumors, preventive surgical maneuvers, and in reference centers. | RRH was safe, effective, and comparable to ORH and LRH with respect to outcomes in regard of surgical trauma and postoperative recovery. | LRH was effective, safe, and superior to the abdominal approach in terms of the most essential short- and long-term surgical outcomes. For some terminal parameters, such as 5 year survival or mortality, more data will be needed. |
| LACC [1,18,19] | Greggi 2020 [20] | Zhang 2019 [22] | Zhao 2017 [24] | |
|---|---|---|---|---|
| DFS (HR/RR) (95% CI) | HR 3.74 (1.63 to 8.58), MIS vs. ORH | HR 0.97 (NR), p = 0.91. LRH vs. ORH | NR | NR |
| DFS up to 5 years (%) | 86.0 vs. 96.5, difference −10.6 (−16.4 to −4.7), MIS vs. ORH | Prospective studies: 92.8 vs. 81.3, p = 0.03, MIS vs. ORH Epidemiological studies: 92.8 vs. 94.4, p = 0.499, LRH vs. ORH | Matched studies: 91.3 vs. 89.9, 90 vs. 89, 97 vs. 89, all RRH vs. LRH Cohort studies: 95.6 to 100 vs. 93.5 to 100 (depending on stage), 96.4 vs. 91.9, 89.7 vs. 89.8, all RRH vs. LRH; 89.7 vs. 84.6, RRH vs. ORH | NR |
| OS to 3 years (%) (HR/RR) (95% CI) | 93.8 vs. 99.0; HR 6.00 (1.77 to 20.30), MIS vs. ORH | Meta-analyses: HR 0.98 (95% CI NR), p = 0.73, HR 0.91 (95% CI NR), p = 0.76, both LRH vs. ORH Prospective studies: 91.0 vs. 78.9, p = 0.026, MIS vs. ORH Epidemiological studies: 95.2 vs. 96.4, p = 0.451, LRH vs. ORH 90.9 vs. 94.7, p = 0.002, MIS vs. ORH | Matched studies: 100 vs. 83.4, RRH vs. LRH; 97 vs. 98, RRH vs. ORH Cohort studies: 96.6 vs. 95.9, RRH vs. LRH; 96.6 vs. 92.3, RRH vs. ORH | NR |
| Recurrence to 3 years (%) (HR/RR) (95% CI) | 5.6 vs. 1.3, HR 4.26 (95% CI 1.44 to 12.60), MIS vs. ORH | Meta-analyses: 8.77 vs. 11.93 (95% CI NR) p = 0.2, 8.3% vs. 11.9 (95% CI NR), p = 0.16, both LRH vs. ORH Prospective studies: 15.1 vs. 14.4 (95% CI NR), p = 0.64, MIS vs. ORH Epidemiological studies: 6.1 vs. 5.7 (95% CI NR), p = NS, LRH vs. ORH | OR 0.85 (95% CI 0.58 to 1.27), 5 studies, RRH vs. ORH; OR 0.96 (95% CI 0.50 to 1.87), 7 studies, RRH vs. LRH | OR 0.74 (95% CI 0.49 to 1.13), 8 studies, LRH vs. ORH |
| LACC [1,23] | Greggi 2020 [20] | Zhang 2019 [22] | Zhao 2017 [21] | |
|---|---|---|---|---|
| Estimated blood loss (mL) (geometric mean (range), MD (95% CI)) | 101 (10 to 1500) vs. 209 (10 to 2200), p < 0.001, MIS vs. ORH | NR | MD −322.59 (−502.75 to −142.43) 5 studies, RRH vs. ORH MD −22.25 (−81.38 to 36.87) 8 studies, RRH vs. LRH | MD −178.41 (−214.89 to −141.94), 13 studies, LRH vs. ORH |
| Duration of surgery (min) (geometric mean (range), MD (95% CI)) | 216 (75 to 441) vs. 187 (61 to 425), p < 0.001, MIS vs. ORH | NR | MD 36.07 (5.83 to 66.31) 6 studies, RRH vs. ORH MD 18.10 (−14.94 to 51.13) 9 studies, RRH vs. LRH | MD 43.68 (29.42 to 57.95), 15 studies, LRH vs. ORH |
| Blood transfusion (%) (OR (95% CI)) | 3.6 vs. 7.8, p = 0.03 *, MIS vs. ORH | NR | OR 0.19 (0.09 to 0.39) 6 studies, RRH vs. ORH OR 0.53 (0.16 to 1.75) 5 studies, RRH vs. LRH | OR 0.47 (0.30 to 0.73), 13 studies, LRH vs. ORH |
| Intraoperative complications (%) (OR (95% CI)) | 12.2 vs. 10.1, p = 0.45, MIS vs. ORH | NR | OR 0.52 (0.27 to 0.98) 5 studies, RRH vs. ORH OR 1.17 (0.44 to 3.10) 7 studies, RRH vs. LRH | OR 1.14 (0.68 to 1.93), 8 studies, LRH vs. ORH |
| Postoperative complications (%) (OR (95% CI)) | 59 vs. 53, p = 0.17, MIS vs. ORH | NR | OR 0.74 (0.45 to 1.22) 7 studies, RRH vs. ORH OR 0.66 (0.39 to 1.12) 9 studies, RRH vs. LRH | NR |
| Length of hospital stay (days) (median (range), MD (95% CI)) | 3 (0 to 72) vs. 5 (1 to 69), p = 0.002, MIS vs. ORH | NR | MD −2.71 (−3.74 to −1.68) 6 studies, RRH vs. open RRH MD −0.24 (−1.33 to 0.85) 9 studies, RRH vs. LRH | MD −3.17 (−4.06 to −2.29), 14 studies, LRH vs. ORH |
| Retrieved lymph nodes (n) | Median: 20 (15 to 26) vs. 21 (16 to 30), MIS vs. ORH | NR | MD −3.43 (−7.74 to 0.88) 6 studies, RRH vs. ORH MD 2.46 (−0.46 to 5.38) 9 studies, RRH vs. LRH | MD −1.65 (−3.19 to −0.11), 8 studies, LRH vs. ORH |
| DVT/PE (%) (OR (95% CI)) | 0.4 vs. 0, p = 0.64, MIS vs. ORH | NR | NR | OR 1.31 (0.48 to 3.57), 5 studies, LRH vs. ORH |
| Ileus (%) (OR (95% CI)) | 0 vs. 0.8, p = 0.35, MIS vs. ORH | NR | NR | OR 0.34 (0.12 to 0.91), 7 studies, LRH vs. ORH |
| Lymphocele/lymphedema (%) (OR (95% CI)) | 0 vs. 1.2, p = 0.2 (lymphocele), 0.4 vs. 0.8, p = 0.52 (lymphedema), MIS vs. ORH | NR | NR | OR 1.46 (0.49 to 4.36), 5 studies, LRH vs. ORH |
| Duration of bladder catheterization (days) (MD (95% CI)) | Delay in bladder function (%), 4.7 vs. 5, p = 0.87, MIS vs. ORH | NR | NR | MD −1.69 (−2.83 to −0.55), 3 studies, LRH vs. ORH |
| UTI (OR (95% CI)) | NR | NR | NR | OR 0.58 (0.22 to 1.57), 4 studies, LRH vs. ORH |
| Ureteral/vaginal fistulas (OR (95% CI)) | Genitourinary fistula/stricture (%) 3.6 vs. 2.7, p = 0.57, MIS vs. ORH | NR | NR | OR 3.67 (1.08 to 12.47), 5 studies, LRH vs. ORH |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Röseler, J.; Wolff, R.; Bauerschlag, D.O.; Maass, N.; Hillemanns, P.; Ferreira, H.; Debrouwere, M.; Scheibler, F.; Geiger, F.; Elessawy, M. Challenges and Controversies in the Surgical Treatment of Cervical Cancer: Open Radical Hysterectomy versus Minimally Invasive Radical Hysterectomy. J. Clin. Med. 2021, 10, 3761. https://doi.org/10.3390/jcm10173761
Röseler J, Wolff R, Bauerschlag DO, Maass N, Hillemanns P, Ferreira H, Debrouwere M, Scheibler F, Geiger F, Elessawy M. Challenges and Controversies in the Surgical Treatment of Cervical Cancer: Open Radical Hysterectomy versus Minimally Invasive Radical Hysterectomy. Journal of Clinical Medicine. 2021; 10(17):3761. https://doi.org/10.3390/jcm10173761
Chicago/Turabian StyleRöseler, Jona, Robert Wolff, Dirk O. Bauerschlag, Nicolai Maass, Peter Hillemanns, Helder Ferreira, Marie Debrouwere, Fülöp Scheibler, Friedemann Geiger, and Mohamed Elessawy. 2021. "Challenges and Controversies in the Surgical Treatment of Cervical Cancer: Open Radical Hysterectomy versus Minimally Invasive Radical Hysterectomy" Journal of Clinical Medicine 10, no. 17: 3761. https://doi.org/10.3390/jcm10173761
APA StyleRöseler, J., Wolff, R., Bauerschlag, D. O., Maass, N., Hillemanns, P., Ferreira, H., Debrouwere, M., Scheibler, F., Geiger, F., & Elessawy, M. (2021). Challenges and Controversies in the Surgical Treatment of Cervical Cancer: Open Radical Hysterectomy versus Minimally Invasive Radical Hysterectomy. Journal of Clinical Medicine, 10(17), 3761. https://doi.org/10.3390/jcm10173761






