Hysterolaparoscopy: A Gold Standard for Diagnosing and Treating Infertility and Benign Uterine Pathology
Abstract
1. Introduction
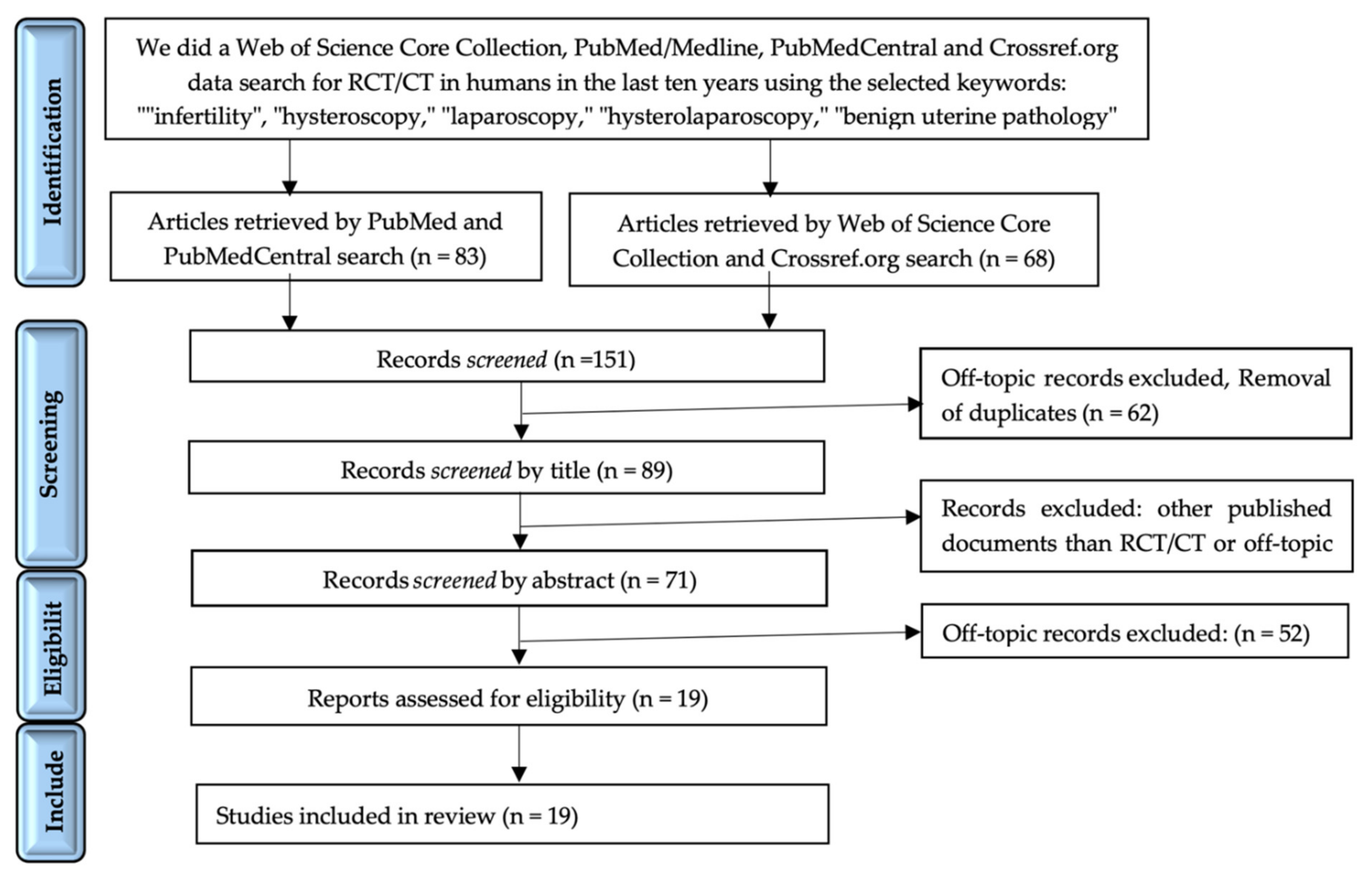
2. Materials and Methods
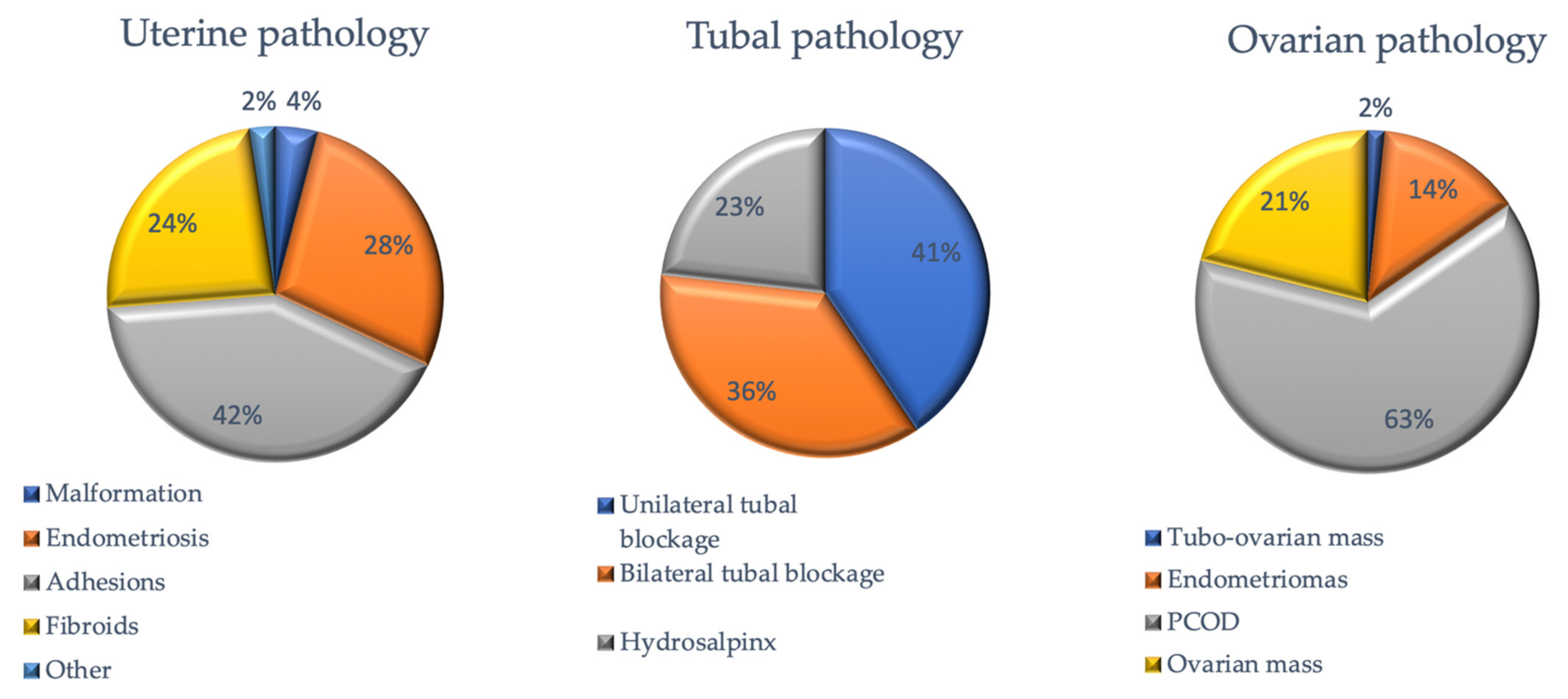
3. Results
Study Selection
4. Assessment of Tubal Patency Using the One-Step Procedure on Hysteroscopy and Laparoscopic Approaches
5. Hysterolaparoscopy (HL) Is a Diagnostic and Therapeutic Tool for Benign Uterine Pathology
6. How Can HL Manage Uterine Malformations?
7. The Complementary Role of Hysterolaparoscopy Procedures in the Management of Ovarian Abnormalities
8. Hysterolaparoscopy—A Therapeutic Challenge in the Management of Endometriosis
9. Discussion
10. Conclusions
11. Practice Key Points
- HL is a safe and effective therapeutic tool for benign uterine pathology and correctable uterine malformations.
- HL is a daycare procedure for the evaluation and treatment of female infertility.
- HL can diagnose undetectable imaging disorders in asymptomatic infertile patients or patients with mild symptoms.
- HL is a useful diagnostic method if the imaging techniques (3D-SIS ultrasound, MRI, or HyCoSy) are not accessible [114].
- HL is superior to HSG in diagnosing the tubal and uterine pathology but with similar accuracy to HyCoSy.
- HL is the first-line therapeutic option prior to ART in minimal/mild forms of endometriosis.
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| HL | hysterolaparoscopy |
| ART | assisted reproduction techniques |
| IVF | in vitro fertilization |
| VCI | volume contrast imaging |
| MRI | magnetic resonance imaging |
| AMH | antimüllerian hormone |
| UBESS | ultrasound-based endometriosis staging system |
| RCT | randomized clinical trial |
| CT | clinical trial |
| SR | systematic review |
| MA | meta-analysis |
| PCOS | polycystic ovary syndrome |
| EFI | endometriosis fertility index |
| TVS | transvaginal sonography |
| DIE | deep infiltrating endometriosis |
| HSG | hysterosalpingography |
| 3D-SIS | 3D-saline infusion sonography |
| HyCoSy | hysterosalpingo-contrast-sonography |
| HyFoSy | hysterosalpingo-foam-sonography |
References
- Fard, S.A.; Gharabaghi, P.M.; Montazeri, F.; Mashrabi, O. Hysteroscopy as a Minimally Invasive Surgery, a Good Substitute for Invasive Gynecological Procedures. Iran. J. Reprod. Med. 2012, 10, 377–382. [Google Scholar]
- Vander Borght, M.; Wyns, C. Fertility and Infertility: Definition and Epidemiology. Clin. Biochem. 2018, 62, 2–10. [Google Scholar] [CrossRef]
- Inhorn, M.C.; Patrizio, P. Infertility around the Globe: New Thinking on Gender, Reproductive Technologies and Global Movements in the 21st Century. Hum. Reprod. Update 2015, 21, 411–426. [Google Scholar] [CrossRef]
- Wallach, E.E.; Seibel, M.M.; Taymor, M.L. Emotional Aspects of Infertility. Fertil. Steril. 1982, 37, 137–145. [Google Scholar] [CrossRef]
- Deshpande, P.S.; Gupta, A.S. Causes and Prevalence of Factors Causing Infertility in a Public Health Facility. J. Hum. Reprod. Sci. 2019, 12, 287–293. [Google Scholar] [CrossRef]
- Mahran, A.; Abdelraheim, A.R.; Eissa, A.; Gadelrab, M. Does Laparoscopy Still Has a Role in Modern Fertility Practice? Int. J. Reprod. Biomed. 2017, 15, 787–794. [Google Scholar] [CrossRef]
- Buia, A.; Stockhausen, F.; Hanisch, E. Laparoscopic Surgery: A Qualified Systematic Review. World J. Methodol. 2015, 5, 238–254. [Google Scholar] [CrossRef] [PubMed]
- Zhang, E.; Zhang, Y.; Fang, L.; Li, Q.; Gu, J. Combined Hysterolaparoscopy for the Diagnosis of Female Infertility: A Retrospective Study of 132 Patients in China. Mater. Socio Medica 2014, 26, 156. [Google Scholar] [CrossRef]
- Nayak, P.K.; Mahapatra, P.C.; Mallick, J.; Swain, S.; Mitra, S.; Sahoo, J. Role of Diagnostic Hystero-Laparoscopy in the Evaluation of Infertility: A Retrospective Study of 300 Patients. J. Hum. Reprod. Sci. 2013, 6, 32–34. [Google Scholar] [CrossRef] [PubMed]
- Moro, F.; Tropea, A.; Selvaggi, L.; Scarinci, E.; Lanzone, A.; Apa, R. Hysterosalpingo-Contrast-Sonography (HyCoSy) in the Assessment of Tubal Patency in Endometriosis Patients. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 186, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Dishuck, C.F.; Perchik, J.D.; Porter, K.K.; Gunn, D.D. Advanced Imaging in Female Infertility. Curr. Urol. Rep. 2019, 20, 77. [Google Scholar] [CrossRef]
- Bhagavath, B.; Benjamin, A. Minimally Invasive Gynecologic Surgery for Benign Conditions: Progress and Challenges. Obstet. Gynecol. Surv. 2015, 70, 656–666. [Google Scholar] [CrossRef]
- Pantou, A.; Simopoulou, M.; Sfakianoudis, K.; Giannelou, P.; Rapani, A.; Maziotis, E.; Grigoriadis, S.; Tsioulou, P.; Syrkos, S.; Souretis, K.; et al. The Role of Laparoscopic Investigation in Enabling Natural Conception and Avoiding in Vitro Fertilization Overuse for Infertile Patients of Unidentified Aetiology and Recurrent Implantation Failure Following in Vitro Fertilization. J. Clin. Med. 2019, 8, 548. [Google Scholar] [CrossRef]
- Tsuji, I.; Ami, K.; Miyazaki, A.; Hujinami, N.; Hoshiai, H. Benefit of diagnostic laparoscopy for patients with unexplained infertility and normal hysterosalpingography findings. Tohoku J. Exp. Med. 2009, 219, 39–42. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dawle, S.; Bhalerao, A.; Kumare, B.; Bhalerao, K. ROLE OF HYSTEROLAPAROSCOPY IN THE EVALUATION OF PRIMARY INFERTILITY. J. Evol. Med. Dent. Sci. 2014, 3, 5496–5500. [Google Scholar] [CrossRef]
- Jain, K. Role of Laporoscopy-Hysteroscopy in Cases of Infertility with Pregnancy Outcome. J. Indian Med. Assoc. 2014, 112, 85–86, 88. [Google Scholar]
- Firmal, P.; Yadav, R.; Agrawal, S. A Prospective Study to Evaluate the Role of Laparohysteroscopy in Unexplained Infertility. J. Obstet. Gynaecol. J. Inst. Obstet. Gynaecol. 2015, 35, 386–388. [Google Scholar] [CrossRef]
- Puri, S.; Puri, S.; Deol, S.; Jain, D.; Kaushal, S. Laparohysteroscopy in Female Infertility: A Diagnostic Cum Therapeutic Tool in Indian Setting. Int. J. Appl. Basic Med. Res. 2015, 5, 46. [Google Scholar] [CrossRef] [PubMed]
- Chavan, N.N.; Gawai, S.; Raj, N.; Changede, P. An Observational Study of the Use of Hystero—Laparoscopy in the Diagnosis and Management of Infertility Patients. MedPulse Int. Med J. 2016. [Google Scholar] [CrossRef]
- Mehta, A.; Modi, A.; Raval, B.; Munshi, S.; Patel, S.; Dedharotiya, S. Role of Diagnostic Hysterolaparoscopy in the Evaluation of Infertility. Int. J. Reprod. Contracept. Obstet. Gynecol. 2016, 5, 437–440. [Google Scholar] [CrossRef]
- Nandhini, V.; Murugalakshmi, M.D. Role of Diagnostic Hysterolaparoscopy in Primary Infertility. IOSR J. Dent. Med. Sci. 2016, 15, 25–28. [Google Scholar] [CrossRef]
- Kabadi, Y.M.; Harsha, B. Hysterolaparoscopy in the Evaluation and Management of Female Infertility. J. Obstet. Gynecol. India 2016, 66, 478–481. [Google Scholar] [CrossRef] [PubMed]
- Avula, K.; Mahalaxmi, G.; Arige, S.K.; Arig, S.K. A Retrospective Study of Role of Hysterolaparoscopy In The Evaluation Of Female Infertility, In 100 Patients In A Private Hospital Over A Period of Two Years. J. Evol. Med. Dent. Sci. 2017, 6, 3955–3958. [Google Scholar] [CrossRef]
- Sharma, A.; Bhalla, R.; O’Donovan, P. Endoscopic Procedures in ART: An Overview. Gynecol. Surg. 2004, 1, 3–10. [Google Scholar] [CrossRef]
- Mariyam, S.A.; Anand, N.B. Role of Diagnostic Hysterolaparoscopy in Evaluation of Female Infertility. Int. J. Reprod. Contracept. Obstet. Gynecol. 2017, 6, 4048–4051. [Google Scholar] [CrossRef][Green Version]
- Sapneswar, B.; Dandapat, A.B.; Sahoo, S.S. A Study On Hysterolaparoscopy In Female Infertility—A Diagnostic Cum Therapeutic Tool. J. Evol. Med. Dent. Sci. 2018, 7, 3750–3754. [Google Scholar]
- Shinde, M.; Sable, U.; Shitole, R. Should Diagnostic Hysteroscopy and Diagnostic Laparoscopy Be a Combined Primary Work up in Evaluating Primary & Secondary Infertile Women? Int. J. Clin. Obstet. Gynaecol. 2019, 3, 84–87. [Google Scholar] [CrossRef]
- Wadadekar, G.S.; Inamdar, D.B.; Nimbargi, V.R. Role of Hysterolaparoscopy in Management of Infertility a Retrospective Clinical Analysis. Int. J. Reprod. Contracept. Obstet. Gynecol. 2020, 9, 4437. [Google Scholar] [CrossRef]
- Ugboaja, J.; Oguejiofor, C.; Ogelle, O. Hysterolaparoscopy (Pan-Endoscopy) in the Management of Female Infertility in Nigeria: A Report of 230 Cases. Niger. J. Gen. Pract. 2020, 18, 53. [Google Scholar] [CrossRef]
- Ekine, A.A.; Fülöp, I.; Tekse, I.; Rúcz, Á.; Jeges, S.; Koppán, Á.; Koppán, M. The Surgical Benefit of Hysterolaparoscopy in Endometriosis-Related Infertility: A Single Centre Retrospective Study with a Minimum 2-Year Follow-Up. J. Clin. Med. 2020, 9, 507. [Google Scholar] [CrossRef]
- Ravikanth, G.O.; Sullia, D.K. Role of Diagnostic Hysterolaparoscopy in Female Infertility: A Retrospective Study. J. Med. Sci. Clin. Res. 2019, 7, 2450–2455. [Google Scholar] [CrossRef]
- Kavitha, G.; Renukadevi, B. Role of Hystero-Laparoscopy with Chromopertubation as a Diagnostic Cum Therapeutic Tool in Evaluation and Treatment of Female Infertility. New Indian J. OBGYN 2019, 6, 15–19. [Google Scholar] [CrossRef]
- Briceag, I.; Costache, A.; Purcarea, V.L.; Cergan, R.; Dumitru, M.; Briceag, I.; Sajin, M.; Ispas, A.T. Fallopian tubes--literature review of anatomy and etiology in female infertility. J. Med. Life 2015, 8, 129–131. [Google Scholar] [PubMed]
- Schlegel, P.N.; Fauser, B.C.; Carrel, D.T.; Racowsky, C.P. Biennial Review of Infertility; Springer: London, UK, 2013. [Google Scholar]
- Allam, I.S.; Rashed, A.M.; Sweedan, K.H.; El Bishry, G.A.; Ahmed, W.E. Role of Hysteroscopy in the Evaluation of Tubal Patency in Infertile Women. Middle East Fertil. Soc. J. 2014, 19, 215–220. [Google Scholar] [CrossRef]
- Holzer, I.; Ott, J.; Kurz, C.; Hofstetter, G.; Hager, M.; Kuessel, L.; Parry, J.P. Is Chronic Endometritis Associated with Tubal Infertility? A Prospective Cohort Study. J. Minim. Invasive Gynecol. 2021, in press. [Google Scholar] [CrossRef]
- Agrawal, N.; Fayyaz, S. Can Hysterolaparoscopic Mediated Chromopertubation Obviate the Need for Hysterosalpingography for Proximal Tubal Blockage?: An Experience at a Single Tertiary Care Center. J. Gynecol. Obstet. Hum. Reprod. 2019, 48, 241–245. [Google Scholar] [CrossRef]
- Ngowa, J.D.; Kasia, J.M.; Georges, N.T.; Nkongo, V.; Sone, C.; Fongang, E. Comparison of hysterosalpingograms with laparoscopy in the diagnostic of tubal factor of female infertility at the Yaoundé General Hospital, Cameroon. Pan Afr. Med. J. 2015, 22, 264. [Google Scholar] [CrossRef]
- Vaid, K.; Mehra, S.; Verma, M.; Jain, S.; Sharma, A.; Bhaskaran, S. Pan Endoscopic Approach “Hysterolaparoscopy” as an Initial Procedure in Selected Infertile Women. J. Clin. Diagn. Res. JCDR 2014, 8, 95–98. [Google Scholar] [CrossRef]
- Ott, J.; Hager, M.; Nouri, K.; Marschalek, J.; Kurz, C. Assessment of Tubal Patency: A Prospective Comparison of Diagnostic Hysteroscopy and Laparoscopic Chromopertubation. J. Minim. Invasive Gynecol. 2020, 27, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Ludwin, I.; Ludwin, A.; Wiechec, M.; Nocun, A.; Banas, T.; Basta, P.; Pitynski, K. Accuracy of Hysterosalpingo-Foam Sonography in Comparison to Hysterosalpingo-Contrast Sonography with Air/Saline and to Laparoscopy with Dye. Hum. Reprod. 2017, 32, 758–769. [Google Scholar] [CrossRef]
- Alcázar, J.L.; Martinez, A.; Duarte, M.; Welly, A.; Marín, A.; Calle, A.; Garrido, R.; Pascual, M.A.; Guerriero, S. Two-Dimensional Hysterosalpingo-Contrast-Sonography Compared to Three/Four-Dimensional Hysterosalpingo-Contrast-Sonography for the Assessment of Tubal Occlusion in Women with Infertility/Subfertility: A Systematic Review with Meta-Analysis. Hum. Fertil. Camb. Engl. 2020, 2, 1–13. [Google Scholar] [CrossRef]
- Chen, S.; Du, X.; Chen, Q.; Chen, S. Combined Real-Time Three-Dimensional Hysterosalpingo-Contrast Sonography with B Mode Hysterosalpingo-Contrast Sonography in the Evaluation of Fallopian Tube Patency in Patients Undergoing Infertility Investigations. BioMed Res. Int. 2019, 2019, 9408141. [Google Scholar] [CrossRef]
- Vignarajan, C.P.; Malhotra, N.; Singh, N. Ovarian Reserve and Assisted Reproductive Technique Outcomes After Laparoscopic Proximal Tubal Occlusion or Salpingectomy in Women with Hydrosalpinx Undergoing in Vitro Fertilization: A Randomized Controlled Trial. J. Minim. Invasive Gynecol. 2019, 26, 1070–1075. [Google Scholar] [CrossRef] [PubMed]
- El-Mazny, A.; Abou-Salem, N.; Hammam, M.; Saber, W. Hysteroscopic Tubal Electrocoagulation versus Laparoscopic Tubal Ligation for Patients with Hydrosalpinges Undergoing in Vitro Fertilization. Int. J. Gynaecol. Obstet. 2015, 130, 250–252. [Google Scholar] [CrossRef]
- Munro, M.G. Uterine Polyps, Adenomyosis, Leiomyomas, and Endometrial Receptivity. Fertil. Steril. 2019, 111, 629–640. [Google Scholar] [CrossRef]
- Pritts, E.A. Fibroids and Infertility: A Systematic Review of the Evidence. Obstet. Gynecol. Surv. 2001, 56, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Carranza-Mamane, B.; Havelock, J.; Hemmings, R. Reproductive Endocrinology and Infertility Committee; special contributor. The Management of Uterine Fibroids in Women with Otherwise Unexplained Infertility. J. Obstet. Gynaecol. Can. JOGC 2015, 37, 277–285. [Google Scholar] [CrossRef]
- Lewis, E.I.; Gargiulo, A.R. The Role of Hysteroscopic and Robot-Assisted Laparoscopic Myomectomy in the Setting of Infertility. Clin. Obstet. Gynecol. 2016, 59, 53–65. [Google Scholar] [CrossRef]
- Lin, S.; Xie, X.; Guo, Y.; Zhang, H.; Liu, C.; Yi, J.; Su, Y.; Deng, Q.; Zhu, W. Clinical Characteristics and Pregnancy Outcomes of Infertile Patients with Endometriosis and Endometrial Polyps: A Retrospective Cohort Study. Taiwan. J. Obstet. Gynecol. 2020, 59, 916–921. [Google Scholar] [CrossRef] [PubMed]
- Shen, L.; Wang, Q.; Huang, W.; Wang, Q.; Yuan, Q.; Huang, Y.; Lei, H. High Prevalence of Endometrial Polyps in Endometriosis-Associated Infertility. Fertil. Steril. 2011, 95, 2722–2724.e1. [Google Scholar] [CrossRef] [PubMed]
- Tardieu, A.; Sire, F.; Gauthier, T. Diagnosis accuracy of endoscopy (laparoscopy, hysteroscopy, fertiloscopy, cystoscopy, colonoscopy) in case of endometriosis: CNGOF-HAS Endometriosis Guidelines. Gynecol. Obstet. Fertil. Senol. 2018, 46, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J.; Nisolle, M.; Casanas-Roux, F.; Bassil, S.; Anaf, V. Rectovaginal Septum, Endometriosis or Adenomyosis: Laparoscopic Management in a Series of 231 Patients. Hum. Reprod. 1995, 10, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Struble, J.; Reid, S.; Bedaiwy, M.A. Adenomyosis: A Clinical Review of a Challenging Gynecologic Condition. J. Minim. Invasive Gynecol. 2016, 23, 164–185. [Google Scholar] [CrossRef]
- De Cicco, S.; Tagliaferri, V.; Selvaggi, L.; Romualdi, D.; Di Florio, C.; Immediata, V.; Lanzone, A.; Guido, M. Expectant Management May Reduce Overtreatment in Women Affected by Unexplained Infertility Confirmed by Diagnostic Laparoscopy. Arch. Gynecol. Obstet. 2017, 295, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.Y.; Jayaprakasan, K.; Zamora, J.; Thornton, J.G.; Raine-Fenning, N.; Coomarasamy, A. The Prevalence of Congenital Uterine Anomalies in Unselected and High-Risk Populations: A Systematic Review. Hum. Reprod. Update 2011, 17, 761–771. [Google Scholar] [CrossRef] [PubMed]
- Grimbizis, G.F.; Gordts, S.; Di Spiezio Sardo, A.; Brucker, S.; De Angelis, C.; Gergolet, M.; Li, T.-C.; Tanos, V.; Brölmann, H.; Gianaroli, L.; et al. The ESHRE/ESGE Consensus on the Classification of Female Genital Tract Congenital Anomalies. Hum. Reprod. 2013, 28, 2032–2044. [Google Scholar] [CrossRef] [PubMed]
- Saravelos, S.H.; Cocksedge, K.A.; Li, T.-C. Prevalence and Diagnosis of Congenital Uterine Anomalies in Women with Reproductive Failure: A Critical Appraisal. Hum. Reprod. Update 2008, 14, 415–429. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Muñoz, E.; Vitale, S.G.; Alvarado-Rosales, D.; Iyune-Cojab, E.; Vitagliano, A.; Lohmeyer, F.M.; Guevara-Gómez, Y.P.; Villarreal-Barranca, A.; Romo-Yañez, J.; Montoya-Estrada, A.; et al. Müllerian Anomalies Prevalence Diagnosed by Hysteroscopy and Laparoscopy in Mexican Infertile Women: Results from a Cohort Study. Diagnostics 2019, 9, 149. [Google Scholar] [CrossRef]
- Siam, S.; Soliman, B.S. Combined Laparoscopy and Hysteroscopy for the Detection of Female Genital System Anomalies Results of 3,811 Infertile Women. J. Reprod. Med. 2014, 59, 542–546. [Google Scholar]
- Grimbizis, G.F.; Di Spiezio Sardo, A.; Saravelos, S.H.; Gordts, S.; Exacoustos, C.; Van Schoubroeck, D.; Bermejo, C.; Amso, N.N.; Nargund, G.; Timmerman, D.; et al. The Thessaloniki ESHRE/ESGE Consensus on Diagnosis of Female Genital Anomalies. Hum. Reprod. 2016, 31, 2–7. [Google Scholar] [CrossRef]
- Ludwin, A.; Pityński, K.; Ludwin, I.; Banas, T.; Knafel, A. Two- and Three-Dimensional Ultrasonography and Sonohysterography versus Hysteroscopy with Laparoscopy in the Differential Diagnosis of Septate, Bicornuate, and Arcuate Uteri. J. Minim. Invasive Gynecol. 2013, 20, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Kougioumtsidou, A.; Mikos, T.; Grimbizis, G.F.; Karavida, A.; Theodoridis, T.D.; Sotiriadis, A.; Tarlatzis, B.C.; Athanasiadis, A.P. Three-Dimensional Ultrasound in the Diagnosis and the Classification of Congenital Uterine Anomalies Using the ESHRE/ESGE Classification: A Diagnostic Accuracy Study. Arch. Gynecol. Obstet. 2019, 299, 779–789. [Google Scholar] [CrossRef] [PubMed]
- Berger, A.; Batzer, F.; Lev-Toaff, A.; Berry-Roberts, C. Diagnostic Imaging Modalities for Müllerian Anomalies: The Case for a New Gold Standard. J. Minim. Invasive Gynecol. 2014, 21, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Acién, P.; Acién, M. The Presentation and Management of Complex Female Genital Malformations. Hum. Reprod. Update 2016, 22, 581–585. [Google Scholar] [CrossRef]
- Dhar, H. Ruptured Rudimentary Horn at 22 Weeks. Niger. Med. J. J. Niger. Med. Assoc. 2012, 53, 175–177. [Google Scholar] [CrossRef]
- Lennox, G.; Pantazi, S.; Keunen, J.; Van Mieghem, T.; Allen, L. Minimally Invasive Surgical Management of a Second Trimester Pregnancy in a Rudimentary Uterine Horn. J. Obstet. Gynecol. Can. JOGC 2013, 35, 468–472. [Google Scholar] [CrossRef]
- Kanno, Y.; Suzuki, T.; Nakamura, E.; Goya, K.; Nishijima, Y.; Shinoda, M.; Hayashi, M.; Izumi, S. Successful Term Delivery after Laparoscopic Resection of a Non-Communicating Rudimentary Horn in a Patient with a Unicornuate Uterus: A Case Report. Tokai J. Exp. Clin. Med. 2014, 39, 59–63. [Google Scholar]
- Spitzer, R.F.; Caccia, N.; Kives, S.; Allen, L.M. Hysteroscopic Unification of a Complete Obstructing Uterine Septum: Case Report and Review of the Literature. Fertil. Steril. 2008, 90, 2016.e17–2016.e20. [Google Scholar] [CrossRef]
- Alborzi, S.; Asefjah, H.; Amini, M.; Vafaei, H.; Madadi, G.; Chubak, N.; Tavana, Z. Laparoscopic Metroplasty in Bicornuate and Didelphic Uteri: Feasibility and Outcome. Arch. Gynecol. Obstet. 2015, 291, 1167–1171. [Google Scholar] [CrossRef]
- Alborzi, S.; Asadi, N.; Zolghadri, J.; Alborzi, S.; Alborzi, M. Laparoscopic Metroplasty in Bicornuate and Didelphic Uteri. Fertil. Steril. 2009, 92, 352–355. [Google Scholar] [CrossRef]
- Bailey, A.P.; Jaslow, C.R.; Kutteh, W.H. Minimally Invasive Surgical Options for Congenital and Acquired Uterine Factors Associated with Recurrent Pregnancy Loss. Womens Health 2015, 11, 161–167. [Google Scholar] [CrossRef]
- Wang, S.; Shi, X.; Hua, X.; Gu, X.; Yang, D. Hysteroscopic Transcervical Resection of Uterine Septum. JSLS 2013, 17, 517–520. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Legendre, G.; Catala, L.; Morinière, C.; Lacoeuille, C.; Boussion, F.; Sentilhes, L.; Descamps, P. Relationship between Ovarian Cysts and Infertility: What Surgery and When? Fertil. Steril. 2014, 101, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Kilicdag, E.B.; Haydardedeoglu, B.; Cok, T.; Parlakgumus, A.H.; Simsek, E.; Bolat, F.A. Polycystic Ovary Syndrome and Increased Polyp Numbers as Risk Factors for Malignant Transformation of Endometrial Polyps in Premenopausal Women. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2011, 112, 200–203. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.K.; Kim, S.H.; Yun, S.-C.; Kim, D.Y.; Chae, H.D.; Kim, C.-H.; Kang, B.M. Decline of Serum Antimüllerian Hormone Levels after Laparoscopic Ovarian Cystectomy in Endometrioma and Other Benign Cysts: A Prospective Cohort Study. Fertil. Steril. 2014, 101, 435–441. [Google Scholar] [CrossRef]
- Gomez, R.; Schorsch, M.; Gerhold-Ay, A.; Hasenburg, A.; Seufert, R.; Skala, C. Fertility After Ovarian Cystectomy: How Does Surgery Affect IVF/ICSI Outcomes? Geburtshilfe Frauenheilkde 2019, 79, 72–78. [Google Scholar] [CrossRef]
- Vercellini, P.; Consonni, D.; Barbara, G.; Buggio, L.; Frattaruolo, M.P.; Somigliana, E. Adenomyosis and Reproductive Performance after Surgery for Rectovaginal and Colorectal Endometriosis: A Systematic Review and Meta-Analysis. Reprod. Biomed. Online 2014, 28, 704–713. [Google Scholar] [CrossRef]
- Viganò, P.; Parazzini, F.; Somigliana, E.; Vercellini, P. Endometriosis: Epidemiology and Aetiological Factors. Best Pract. Res. Clin. Obstet. Gynaecol. 2004, 18, 177–200. [Google Scholar] [CrossRef]
- Parasar, P.; Ozcan, P.; Terry, K.L. Endometriosis: Epidemiology, Diagnosis and Clinical Management. Curr. Obstet. Gynecol. Rep. 2017, 6, 34–41. [Google Scholar] [CrossRef]
- Nnoaham, K.E.; Hummelshoj, L.; Webster, P.; d’Hooghe, T.; Nardone, F.d.C.; Nardone, C.d.C.; Jenkinson, C.; Kennedy, S.H.; Zondervan, K.T. Impact of Endometriosis on Quality of Life and Work Productivity: A Multicenter Study across Ten Countries. Fertil. Steril. 2011, 96, 366–373.e8. [Google Scholar] [CrossRef]
- Filip, L.; Duică, F.; Prădatu, A.; Crețoiu, D.; Suciu, N.; Crețoiu, S.M.; Predescu, D.-V.; Varlas, V.N.; Voinea, S.-C. Endometriosis Associated Infertility: A Critical Review and Analysis on Etiopathogenesis and Therapeutic Approaches. Med. Kaunas Lith. 2020, 56, 460. [Google Scholar] [CrossRef]
- Casals, G.; Carrera, M.; Domínguez, J.A.; Abrão, M.S.; Carmona, F. Impact of Surgery for Deep Infiltrative Endometriosis before In Vitro Fertilization: A Systematic Review and Meta-Analysis. J. Minim. Invasive Gynecol. 2021, 28, 1303–1312.e5. [Google Scholar] [CrossRef]
- Donnez, O.; Donnez, J. Deep Endometriosis: The Place of Laparoscopic Shaving. Best Pract. Res. Clin. Obstet. Gynaecol. 2021, 71, 100–113. [Google Scholar] [CrossRef]
- Fadhlaoui, A.; Bouquet de la Jolinière, J.; Feki, A. Endometriosis and Infertility: How and When to Treat? Front. Surg. 2014, 1, 24. [Google Scholar] [CrossRef]
- Orazov, M.R.; Radzinsky, V.Y.; Ivanov, I.I.; Khamoshina, M.B.; Shustova, V.B. Oocyte Quality in Women with Infertility Associated Endometriosis. Gynecol. Endocrinol. 2019, 35 (Suppl. S1), 24–26. [Google Scholar] [CrossRef]
- Shaltout, M.F.; Elsheikhah, A.; Maged, A.M.; Elsherbini, M.M.; Zaki, S.S.; Dahab, S.; Elkomy, R.O. A Randomized Controlled Trial of a New Technique for Laparoscopic Management of Ovarian Endometriosis Preventing Recurrence and Keeping Ovarian Reserve. J. Ovarian Res. 2019, 12, 66. [Google Scholar] [CrossRef]
- Rius, M.; Gracia, M.; Ros, C.; Martínez-Zamora, M.-Á.; deGuirior, C.; Quintas, L.; Carmona, F. Impact of Endometrioma Surgery on Ovarian Reserve: A Prospective, Randomized, Pilot Study Comparing Stripping with CO2 Laser Vaporization in Patients with Bilateral Endometriomas. J. Int. Med. Res. 2020, 48, 300060520927627. [Google Scholar] [CrossRef]
- Sweed, M.S.; Makled, A.K.; El-Sayed, M.A.; Shawky, M.E.; Abd-Elhady, H.A.; Mansour, A.M.; Mohamed, R.M.; Hemeda, H.; Nasr-Eldin, E.A.; Attia, N.S.; et al. Ovarian Reserve Following Laparoscopic Ovarian Cystectomy vs Cyst Deroofing for Endometriomas. J. Minim. Invasive Gynecol. 2019, 26, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Keckstein, J.; Saridogan, E.; Ulrich, U.A.; Sillem, M.; Oppelt, P.; Schweppe, K.W.; Krentel, H.; Janschek, E.; Exacoustos, C.; Malzoni, M.; et al. The #Enzian Classification: A Comprehensive Non-Invasive and Surgical Description System for Endometriosis. Acta Obstet. Gynecol. Scand. 2021. [Google Scholar] [CrossRef]
- Guzick, D.S.; Silliman, N.P.; Adamson, G.D.; Buttram, V.C.; Canis, M.; Malinak, L.R.; Schenken, R.S. Prediction of Pregnancy in Infertile Women Based on the American Society for Reproductive Medicine’s Revised Classification of Endometriosis. Fertil. Steril. 1997, 67, 822–829. [Google Scholar] [CrossRef]
- Vesali, S.; Razavi, M.; Rezaeinejad, M.; Maleki-Hajiagha, A.; Maroufizadeh, S.; Sepidarkish, M. Endometriosis Fertility Index for Predicting Non-Assisted Reproductive Technology Pregnancy after Endometriosis Surgery: A Systematic Review and Meta-Analysis. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 800–809. [Google Scholar] [CrossRef]
- Mascarenhas, M.N.; Flaxman, S.R.; Boerma, T.; Vanderpoel, S.; Stevens, G.A. National, Regional, and Global Trends in Infertility Prevalence Since 1990: A Systematic Analysis of 277 Health Surveys. PLoS Med. 2012, 9, e1001356. [Google Scholar] [CrossRef] [PubMed]
- Thoma, M.; Fledderjohann, J.; Cox, C.; Adageba, R.K. Biological and Social Aspects of Human Infertility: A Global Perspective. Available online: https://oxfordre.com/publichealth/view/10.1093/acrefore/9780190632366.001.0001/acrefore-9780190632366-e-184 (accessed on 3 June 2021). [CrossRef]
- Zhang, Y.; Gu, X.; Meng, Y.; Guo, H.; Du, J.; Xing, W. Analysis of the Effect of Laparoscopy and Hysteroscopy on Ovarian Function, Immune Function and Quality of Sexual Life of Patients with Hysteromyoma at Different Ages. Oncol. Lett. 2018, 15, 2929–2934. [Google Scholar] [CrossRef] [PubMed]
- Kodaman, P.H. Hysteroscopic Polypectomy for Women Undergoing IVF Treatment: When Is It Necessary? Curr. Opin. Obstet. Gynecol. 2016, 28, 184–190. [Google Scholar] [CrossRef]
- Zhang, H.; He, X.; Tian, W.; Song, X.; Zhang, H. Hysteroscopic Resection of Endometrial Polyps and Assisted Reproductive Technology Pregnancy Outcomes Compared with No Treatment: A Systematic Review. J. Minim. Invasive Gynecol. 2019, 26, 618–627. [Google Scholar] [CrossRef] [PubMed]
- Pundir, J.; Pundir, V.; Omanwa, K.; Khalaf, Y.; El-Toukhy, T. Hysteroscopy Prior to the First IVF Cycle: A Systematic Review and Meta-Analysis. Reprod. Biomed. Online 2014, 28, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Di Spiezio Sardo, A.; Di Carlo, C.; Minozzi, S.; Spinelli, M.; Pistotti, V.; Alviggi, C.; De Placido, G.; Nappi, C.; Bifulco, G. Efficacy of Hysteroscopy in Improving Reproductive Outcomes of Infertile Couples: A Systematic Review and Meta-Analysis. Hum. Reprod. Update 2016, 22, 479–496. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; You, D.; Yuan, M.; Xi, M. Hysteroscopy after Repeated Implantation Failure of Assisted Reproductive Technology: A Meta-Analysis. J. Obstet. Gynaecol. Res. 2018, 44, 365–373. [Google Scholar] [CrossRef]
- El-Toukhy, T.; Campo, R.; Khalaf, Y.; Tabanelli, C.; Gianaroli, L.; Gordts, S.S.; Gordts, S.; Mestdagh, G.; Mardesic, T.; Voboril, J.; et al. Hysteroscopy in Recurrent In-Vitro Fertilisation Failure (TROPHY): A Multicentre, Randomised Controlled Trial. Lancet 2016, 387, 2614–2621. [Google Scholar] [CrossRef]
- Smit, J.G.; Kasius, J.C.; Eijkemans, M.J.C.; Koks, C.A.M.; van Golde, R.; Nap, A.W.; Scheffer, G.J.; Manger, P.A.P.; Hoek, A.; Schoot, B.C.; et al. Hysteroscopy before In-Vitro Fertilisation (InSIGHT): A Multicentre, Randomised Controlled Trial. Lancet 2016, 387, 2622–2629. [Google Scholar] [CrossRef]
- Metwally, M.; Raybould, G.; Cheong, Y.C.; Horne, A.W. Surgical Treatment of Fibroids for Subfertility. Cochrane Database Syst. Rev. 2020, 1, CD003857. [Google Scholar] [CrossRef]
- Bosteels, J.; van Wessel, S.; Weyers, S.; Broekmans, F.J.; D’Hooghe, T.M.; Bongers, M.Y.; Mol, B.W.J. Hysteroscopy for Treating Subfertility Associated with Suspected Major Uterine Cavity Abnormalities. Cochrane Database Syst. Rev. 2018, 12, CD009461. [Google Scholar] [CrossRef] [PubMed]
- Bordewijk, E.M.; Ng, K.Y.B.; Rakic, L.; Mol, B.W.J.; Brown, J.; Crawford, T.J.; van Wely, M. Laparoscopic Ovarian Drilling for Ovulation Induction in Women with Anovulatory Polycystic Ovary Syndrome. Cochrane Database Syst. Rev. 2020, 2, CD001122. [Google Scholar] [CrossRef] [PubMed]
- Fauconnier, A.; Borghese, B.; Huchon, C.; Thomassin-Naggara, I.; Philip, C.-A.; Gauthier, T.; Bourdel, N.; Denouel, A.; Torre, A.; Collinet, P.; et al. Epidemiology and diagnosis strategy: CNGOF-HAS Endometriosis Guidelines. Gynecol. Obstet. Fertil. Senol. 2018, 46, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Collinet, P.; Fritel, X.; Revel-Delhom, C.; Ballester, M.; Bolze, P.A.; Borghese, B.; Bornsztein, N.; Boujenah, J.; Brillac, T.; Chabbert-Buffet, N.; et al. Management of Endometriosis: CNGOF/HAS Clinical Practice Guidelines—Short Version. J. Gynecol. Obstet. Hum. Reprod. 2018, 47, 265–274. [Google Scholar] [CrossRef]
- Daniilidis, A.; Pados, G. Comments on the ESHRE Recommendations for the Treatment of Minimal Endometriosis in Infertile Women. Reprod. Biomed. Online 2018, 36, 84–87. [Google Scholar] [CrossRef]
- Bafort, C.; Beebeejaun, Y.; Tomassetti, C.; Bosteels, J.; Duffy, J.M. Laparoscopic Surgery for Endometriosis. Cochrane Database Syst. Rev. 2020, 10, CD011031. [Google Scholar] [CrossRef]
- Jacobson, T.Z.; Duffy, J.M.; Barlow, D.; Farquhar, C.; Koninckx, P.R.; Olive, D. Laparoscopic Surgery for Subfertility Associated with Endometriosis. Cochrane Database Syst. Rev. 2010, 1, CD001398. [Google Scholar] [CrossRef]
- Begum, J.; Samal, S.; Ghose, S.; Palai, P.; Samal, R. Combined hysterolaparoscopy as an early option for initial evaluation of female infertility: A retrospective study of 135 patients. Int. J. Reprod. Contracept. Obstet. Gynecol. 2015, 4, 584–588. [Google Scholar] [CrossRef]
- Mathieu d’Argent, E.; Cohen, J.; Chauffour, C.; Pouly, J.L.; Boujenah, J.; Poncelet, C.; Decanter, C.; Santulli, P. Deeply infiltrating endometriosis and infertility: CNGOF-HAS Endometriosis Guidelines. Gynecol. Obstet. Fertil. Senol. 2018, 46, 357–367. [Google Scholar] [CrossRef]
- Farquhar, C.; Marjoribanks, J. Assisted Reproductive Technology: An Overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2018, 8, CD010537. [Google Scholar] [CrossRef]
- Kamath, M.S.; Rikken, J.F.W.; Bosteels, J. Does Laparoscopy and Hysteroscopy Have a Place in the Diagnosis of Unexplained Infertility? Semin. Reprod. Med. 2020, 38, 29–35. [Google Scholar] [CrossRef]
| Study | Uterine Pathology | Tubal Pathology | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cervical Stenosis | Synechiae | Submucosal Fibroids | Polyps | Asherman Syndrome | Uterine Septum | Malformation | Atrophy | Others | Adhesions in the Tubal Ostium | |
| Dawle [15] | 7 | 3 | 2 | 1 | ||||||
| Neerja [16] | 58 | 20 | 20 | 5 | 25 | 22 | ||||
| Firmal [17] | 1 * | 1 | 1 ** | |||||||
| Puri [18] | 4 | 2 | ||||||||
| Niranjan [19] | 6 | 5 | 3 | 2 | 2 | 8 | 2 | |||
| Mehta [20] | 1 | 8 | 16 | 29 | 6 | |||||
| Nandhini [21] | 1 | 1 | 4 | 1 | 1 | 3 | ||||
| Kabadi [22] | 5 | 6 | 13 | |||||||
| Avula [23] | 1 | 4 | 6 | 4 | 5 | 14 *** | ||||
| Sharma [24] | 5 | 10 | 14 | |||||||
| Ahmed [25] | 4 | 4 | 3 **** | |||||||
| Sapneswar [26] | 4 | 5 | ||||||||
| Shinde [27] | 4 | 7 | 1 | 2 | 8 | |||||
| Wadadekar [28] | 2 | 1 | 4 | 1 | 1 | |||||
| Ugboaja [29] | 95 | 37 | 46 | 34 | 14 ***** | |||||
| Ekine [30] | 28 | 5 | 39 | 1 | ||||||
| Ravikanth [31] | 4 | 1 | ||||||||
| Kavitha [32] | 2 | 5 | 13 | 3 | ||||||
| Study | Anomalies | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Uterine Pathology | Tubal Pathology | Ovarian Pathology | |||||||||||
| Malformation | Endometriosis | Adhesions | Fibroids | Others | Tubal Blockage | Unilateral Tubal Block | Bilateral Tubal Block | Hydro-Salpinx | Tubo-Ovarian Mass | Endometriod Chistae | PCOS | Ovarian Mass | |
| Dawle | 2 | 2 | 7 | 2 | 18 | 7 | 11 | 2 | |||||
| Neerja | |||||||||||||
| Firmal | 6 | 7 | 1 | 1 | 1 | ||||||||
| Puri | 9 | 3 | 9 | 3 | 1 | 11 | 5 | ||||||
| Niranjan | 2 | 2 | 5 | 4 | 5 | 4 | 2 | 4 | 8 | 11 | |||
| Mehta | 3 | 41 | 29 * | 15 | 61 | 30 | 31 | 22 | |||||
| Nandhini | 1 | 6 | 5 | 2 ** | 1 | 10 | 5 | 5 | 5 | 1 | 4 | 13 | |
| Kabadi | 5 | 18 | 6 | 7 | 3 | 4 | 6 | 13 | |||||
| Avula | 7 | 11 | 12 * | 5 | 32 | 14 | 18 | 48 | 7 | ||||
| Sharma | 9 | 38 | 8 | 12 | 6 | 7 | 10 | 31 | |||||
| Ahmed | 2 | 8 | 3 | 5 | 1 | 4 | |||||||
| Agrawal | 67 | 34 | 78 | ||||||||||
| Sapneswar | 9 | 5 | 9 | 3 | |||||||||
| Ravikanth | 1 | 7 | 8 | 3 | 6 | 6 | 1 | ||||||
| Kavitha G | 5 | 32 | 17 | 16 | 25 | ||||||||
| Shinde | 9 | 12 | 4 | 9 (TB) | 6 | 4 | |||||||
| Wadadekar | 2 | 3 | 15 | 18 | 4 | 2 | |||||||
| Ugboaja | 19 | 91 | 130 | 84 | 46 | 96 | |||||||
| Ekine | 80 | 13 | 20 | ||||||||||
| Nr | Authors | Year | Inclusion Period | Study Design | Age | Nr | Type of Infertility | Hysteroscopy | Laparoscopy | Management | Pregnancy Rate | Conclusion | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P | S | N | A | N | A | D | O | |||||||||
| 1 | Dawle | 2014 | 2011–2013 | PS | 18–40 | 100 | 100 | 0 | 83 | 13 | 66 | 34 | D | 21% |
| |
| 2 | Neerja | 2014 | NR | PS | 20–30 | 200 | 125 | 75 | 50 | 150 | 60 | 140 | D | O | 45.71% |
|
| 3 | Firmal | 2014 | 2009–2011 | PS | 27.6 (mean) | 30 | 24 | 6 | 28 | 2 | 19 | 11 | D | O | - |
|
| 4 | Puri | 2015 | NR | PS | 30 (mean) | 50 | 24 | 26 | 44 | 6 | 0 | 50 | D | O | 28.2% |
|
| 5 | Niranjan | 2016 | 2013–2015 | PS | 20–40 | 100 | 87 | 13 | 74 | 26 | 53 | 47 | D | O | 35–45% |
|
| 6 | Mehta | 2016 | 2013–2015 | PS | 28.8; 31.1 | 300 | 206 | 94 | 244 | 56 | 199 | 101 | D |
| ||
| 7 | Nandhini | 2016 | 2015–2016 | PS | 21–40 | 50 | 50 | 0 | 37 | 13 | 43 | 7 | D |
| ||
| 8 | Kabadi | 2016 | 2014–2015 | RS | 18–40 | 94 | 50 * | 16 | 43 | 17 | 44 | 47 | D | O |
| |
| 9 | Avula | 2017 | 2015–2016 | RS | 20–35 | 100 | 72 | 28 | 66 | 34 | 48 | 52 | D | O |
| |
| 10 | Sharma | 2017 | 2012–2015 | RS | 20–40 | 130 | 82 | 48 | 101 | 29 | 48 | 82 | D |
| ||
| 11 | Ahmed | 2017 | 2015–2016 | PS | 20–40 | 30 | 21 | 9 | 19 | 11 | 17 | 13 | D | O |
| |
| 12 | Agrawal | 2018 | 2016–2017 | PS | 19–35 (27.7) | 157 | 93 | 64 | 32 HL | 125 | D | O | 57.3% |
| ||
| 13 | Sapneswar | 2018 | NR | PS | 29.5 (mean) | 40 | 24 | 16 | 2 HL | 38 | D | O |
| |||
| 14 | Ravikanth | 2019 | NR | RS | 20–45 | 24 | 21 | 3 | 19 | 5 | NR | D | O |
| ||
| 15 | Kavitha G | 2019 | 2013–2018 | RS | 19–40 | 125 | 104 | 21 | 101 | 24 | 53 | 72 | D | O |
| |
| 16 | Shinde | 2019 | 2018–2019 | PS | 25–38 (33) | 100 | 50 | 50 | 80 | 20 | 57 | 43 | D | O |
| |
| 17 | Wadadekar | 2020 | 2019 | RS | 20–40 | 41 | 32 | 9 | 32 | 9 | 13 | 28 | D | O | 21.05% |
|
| 18 | Ugboaja | 2020 | NR | Cross-sectional survey | 35.6 mean | 230 | 106 | 124 | 78 | 152 | 59 | 171 | D | O |
| |
| 19 | Ekine | 2020 | 2010–2016 | RS | 25–46; (34.3) | 455 | 319 | 136 | NR | NR | 272 HL | 168 | D | O |
| |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Varlas, V.; Rhazi, Y.; Cloțea, E.; Borș, R.G.; Mirică, R.M.; Bacalbașa, N. Hysterolaparoscopy: A Gold Standard for Diagnosing and Treating Infertility and Benign Uterine Pathology. J. Clin. Med. 2021, 10, 3749. https://doi.org/10.3390/jcm10163749
Varlas V, Rhazi Y, Cloțea E, Borș RG, Mirică RM, Bacalbașa N. Hysterolaparoscopy: A Gold Standard for Diagnosing and Treating Infertility and Benign Uterine Pathology. Journal of Clinical Medicine. 2021; 10(16):3749. https://doi.org/10.3390/jcm10163749
Chicago/Turabian StyleVarlas, Valentin, Yassin Rhazi, Eliza Cloțea, Roxana Georgiana Borș, Radu Mihail Mirică, and Nicolae Bacalbașa. 2021. "Hysterolaparoscopy: A Gold Standard for Diagnosing and Treating Infertility and Benign Uterine Pathology" Journal of Clinical Medicine 10, no. 16: 3749. https://doi.org/10.3390/jcm10163749
APA StyleVarlas, V., Rhazi, Y., Cloțea, E., Borș, R. G., Mirică, R. M., & Bacalbașa, N. (2021). Hysterolaparoscopy: A Gold Standard for Diagnosing and Treating Infertility and Benign Uterine Pathology. Journal of Clinical Medicine, 10(16), 3749. https://doi.org/10.3390/jcm10163749







