Bi-Centric Independent Validation of Outcome Prediction after Radioembolization of Primary and Secondary Liver Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Statistical Analysis
2.2.1. Independent Validation
2.2.2. Feature Importance and Influence on Outcome
3. Results
3.1. Patients
3.2. Statistical Analysis
3.2.1. Independent Validation
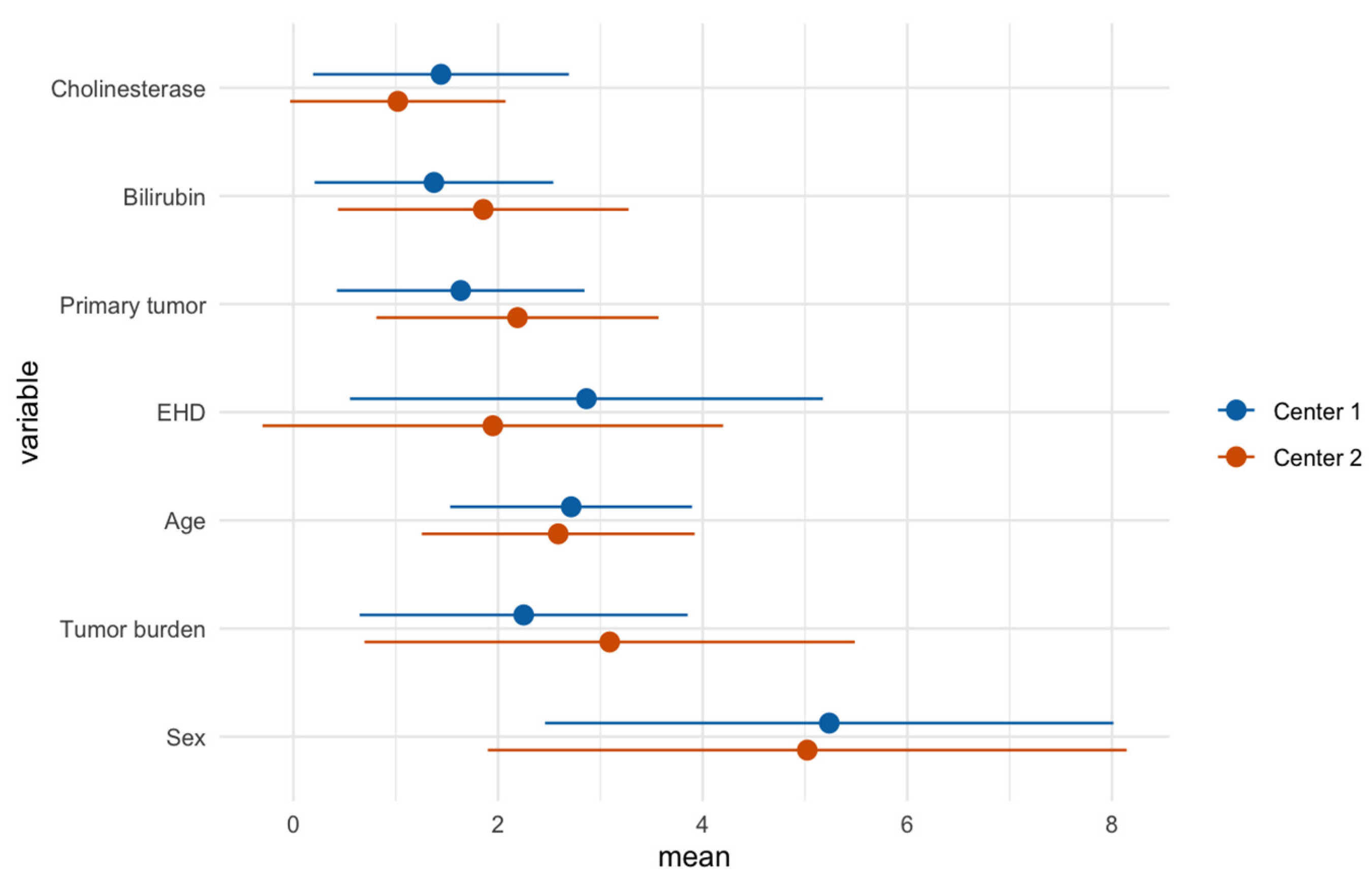
3.2.2. Feature Importance
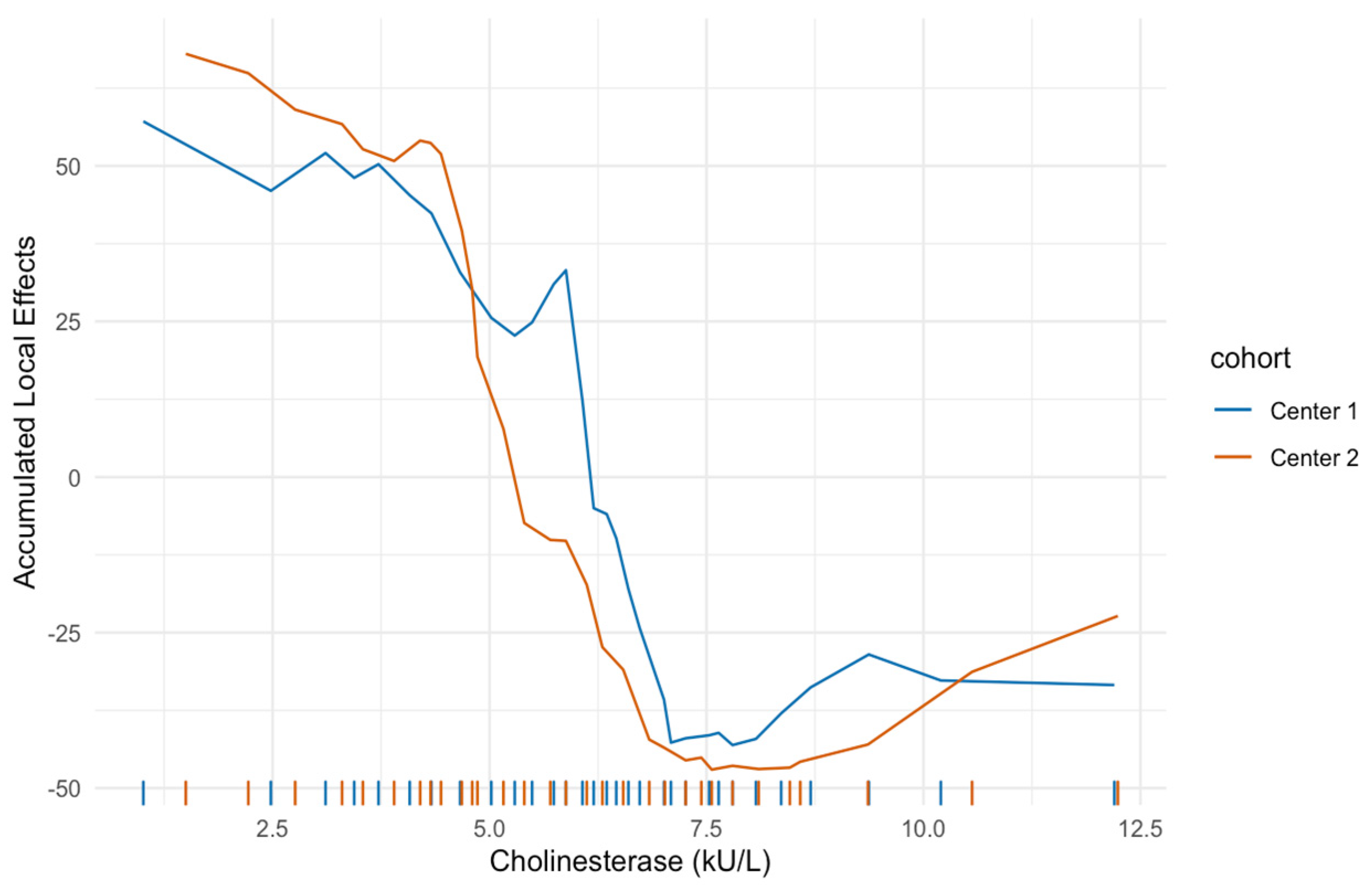
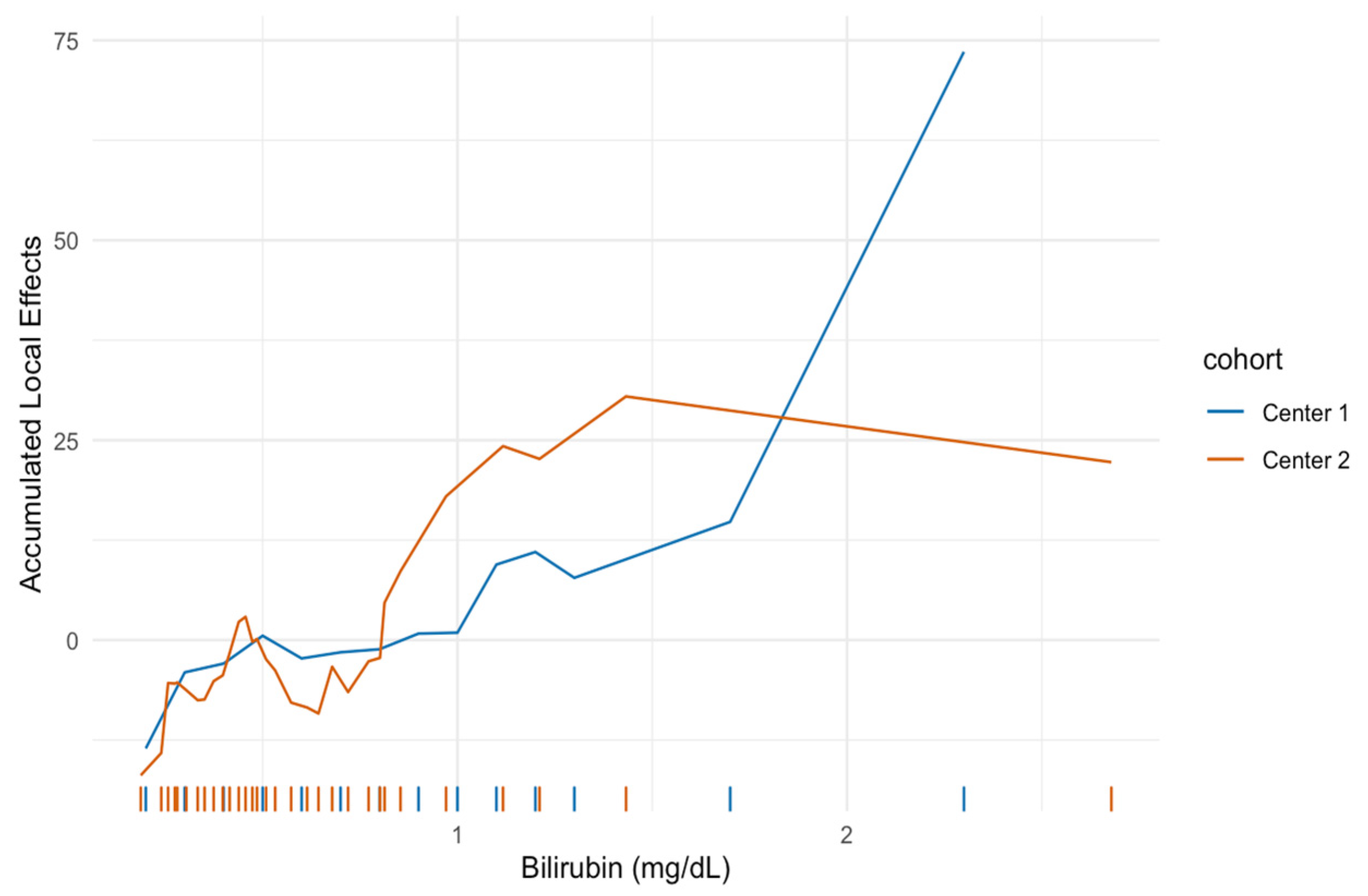
3.2.3. Feature Importance on Predicted Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bester, L.; Meteling, B.; Pocock, N.; Pavlakis, N.; Chua, T.C.; Saxena, A.; Morris, D.L. Radioembolization versus Standard Care of Hepatic Metastases: Comparative Retrospective Cohort Study of Survival Outcomes and Adverse Events in Salvage Patients. J. Vasc. Interv. Radiol. 2012, 23, 96–105. [Google Scholar] [CrossRef]
- Evans, K.A.; Richardson, M.G.; Pavlakis, N.; Morris, D.L.; Liauw, W.; Bester, L. Survival Outcomes of a Salvage Patient Population after Radioembolization of Hepatic Metastases with Yttrium-90 Microspheres. J. Vasc. Interv. Radiol. 2010, 21, 1521–1526. [Google Scholar] [CrossRef]
- Padia, S.A.; Johnson, G.E.; Horton, K.J.; Ingraham, C.R.; Kogut, M.J.; Kwan, S.; Vaidya, S.; Monsky, W.L.; Park, J.O.; Bhattacharya, R.; et al. Segmental Yttrium-90 Radioembolization versus Segmental Chemoembolization for Localized Hepatocellular Carcinoma: Results of a Single-Center, Retrospective, Propensity Score—Matched Study. J. Vasc. Interv. Radiol. 2017, 28, 777–785. [Google Scholar] [CrossRef]
- Ponti, A.; Denys, A.; Digklia, A.; Schaefer, N.; Hocquelet, A.; Knebel, J.-F.; Michielin, O.; Dromain, C.; Duran, R. First-Line Selective Internal Radiation Therapy in Patients with Uveal Melanoma Metastatic to the Liver. J. Nucl. Med. 2020, 61, 350–356. [Google Scholar] [CrossRef]
- Rosenbaum, C.E.N.M.; Verkooijen, H.M.; Lam, M.G.E.H.; Smits, M.L.J.; Koopman, M.; von Seeters, T.; Vermoolen, M.A.; von den Bosch, M.A.A.J. Radioembolization for Treatment of Salvage Patients with Colorectal Cancer Liver Metastases: A Systematic Review. J. Nucl. Med. 2013, 54, 1890–1895. [Google Scholar] [CrossRef]
- Salem, R.; Gabr, A.; Riaz, A.; Mora, R.; Ali, R.; Abecassis, M.; Hickey, R.; Kulik, L.; Ganger, D.; Flamm, S.; et al. Institutional decision to adopt Y90 as primary treatment for hepatocellular carcinoma informed by a 1,000-patient 15-year experience. Hepatology 2018, 68, 1429–1440. [Google Scholar] [CrossRef] [PubMed]
- Salem, R.; Lewandowski, R.J.; Kulik, L.; Wang, E.; Riaz, A.; Ryu, R.K.; Sato, K.T.; Gupta, R.; Nikolaidis, P.; Miller, F.H.; et al. Radioembolization Results in Longer Time-to-Progression and Reduced Toxicity Compared With Chemoembolization in Patients With Hepatocellular Carcinoma. Gastroenterology 2011, 140, 497–507. [Google Scholar] [CrossRef] [PubMed]
- Seidensticker, R.; Denecke, T.; Kraus, P.; Seidensticker, M.; Mohnike, K.; Fahlke, J.; Kettner, E.; Hildebrandt, B.; Dudeck, O.; Pech, M.; et al. Matched-Pair Comparison of Radioembolization Plus Best Supportive Care Versus Best Supportive Care Alone for Chemotherapy Refractory Liver-Dominant Colorectal Metastases. Cardiovasc. Interv. Radiol. 2012, 35, 1066–1073. [Google Scholar] [CrossRef] [PubMed]
- Marqueen, K.E.; Kim, E.; Ang, C.; Mazumdar, M.; Buckstein, M.; Ferket, B.S. Cost-Effectiveness Analysis of Selective Internal Radiotherapy With Yttrium-90 Versus Sorafenib in Locally Advanced Hepatocellular Carcinoma. JCO Oncol. Pract. 2021, 17, e266–e277. [Google Scholar] [CrossRef] [PubMed]
- Chow, P.K.H.; Gandhi, M.; Tan, S.-B.; Khin, M.W.; Khasbazar, A.; Ong, J.; Choo, S.P.; Cheow, P.C.; Chotipanich, C.; Lim, K.; et al. SIRveNIB: Selective Internal Radiation Therapy Versus Sorafenib in Asia-Pacific Patients with Hepatocellular Carcinoma. J. Clin. Oncol. 2018, 36, 1913–1921. [Google Scholar] [CrossRef]
- Ricke, J.; Klümpen, H.J.; Amthauer, H.; Bargellini, I.; Bartenstein, P.; de Toni, E.N.; Gasbarrini, A.; Pech, M.; Peck-Radosavljevic, M.; Popovič, P.; et al. Impact of combined selective internal radiation therapy and sorafenib on survival in advanced hepatocellular carcinoma. J. Hepatol. 2019, 71, 1164–1174. [Google Scholar] [CrossRef] [PubMed]
- van Hazel, G.A.; Heinemann, V.; Sharma, N.K.; Findlay, M.P.N.; Ricke, J.; Peeters, M.; Perez, D.; Robinson, B.A.; Strickland, A.H.; Ferguson, T.; et al. SIRFLOX: Randomized Phase III Trial Comparing First-Line mFOLFOX6 (Plus or Minus Bevacizumab) Versus mFOLFOX6 (Plus or Minus Bevacizumab) Plus Selective Internal Radiation Therapy in Patients With Metastatic Colorectal Cancer. J. Clin. Oncol. 2016, 34, 1723–1731. [Google Scholar] [CrossRef] [PubMed]
- Vilgrain, V.; Pereira, H.; Assenat, E.; Guiu, B.; Ilonca, A.D.; Pageaux, G.-P.; Sibert, A.; Bouattour, M.; Lebtahi, R.; Allaham, W.; et al. Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): An open-label randomised controlled phase 3 trial. Lancet Oncol. 2017, 18, 1624–1636. [Google Scholar] [CrossRef]
- Wasan, H.S.; Gibbs, P.; Sharma, N.K.; Taieb, J.; Heinemann, V.; Ricke, J.; Peeters, M.; Findlay, M.; Weaver, A.; Mills, J.; et al. First-line selective internal radiotherapy plus chemotherapy versus chemotherapy alone in patients with liver metastases from colorectal cancer (FOXFIRE, SIRFLOX, and FOXFIRE-Global): A combined analysis of three multicentre, randomised, phase 3 trials. Lancet Oncol. 2017, 18, 1159–1171. [Google Scholar] [CrossRef]
- Gibbs, P.; Heinemann, V.; Sharma, N.K.; Taieb, J.; Ricke, J.; Peeters, M.; Findlay, M.; Robinson, B.; Jackson, C.; Strickland, A.; et al. Effect of Primary Tumor Side on Survival Outcomes in Untreated Patients With Metastatic Colorectal Cancer When Selective Internal Radiation Therapy Is Added to Chemotherapy: Combined Analysis of Two Randomized Controlled Studies. Clin. Colorectal Cancer 2018, 17, e617–e629. [Google Scholar] [CrossRef]
- Levillain, H.; Bagni, O.; Deroose, C.M.; Dieudonné, A.; Gnesin, S.; Grosser, O.S.; Kappadath, S.C.; Kennedy, A.; Kokabi, N.; Liu, D.M.; et al. International recommendations for personalised selective internal radiation therapy of primary and metastatic liver diseases with yttrium-90 resin microspheres. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1570–1584. [Google Scholar] [CrossRef]
- Garin, E.; Palard, X.; Rolland, Y. Personalised Dosimetry in Radioembolisation for HCC: Impact on Clinical Outcome and on Trial Design. Cancers 2020, 12, 1557. [Google Scholar] [CrossRef]
- Hermann, A.-L.; Dieudonné, A.; Ronot, M.; Sanchez, M.; Pereira, H.; Chatellier, G.; Garin, E.; Castera, L.; Lebtahi, R.; Vilgrain, V. Relationship of Tumor Radiation–absorbed Dose to Survival and Response in Hepatocellular Carcinoma Treated with Transarterial Radioembolization with 90Y in the SARAH Study. Radiology 2020, 296, 673–684. [Google Scholar] [CrossRef]
- Mikell, J.K.; Dewaraja, Y.K.; Owen, D. Transarterial Radioembolization for Hepatocellular Carcinoma and Hepatic Metastases: Clinical Aspects and Dosimetry Models. Semin. Radiat. Oncol. 2020, 30, 68–76. [Google Scholar] [CrossRef]
- Alsultan, A.A.; van Roekel, C.; Barentsz, M.W.; Smits, M.L.J.; Kunnen, B.; Koopman, M.; Bruijnen, R.C.G.; de Keizer, B.; Lam, M. Dose-response and dose-toxicity relationships for yttrium-90 glass radioembolization in patients with colorectal cancer liver metastases. J. Nucl. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Paprottka, K.J.; Schoeppe, F.; Ingrisch, M.; Rübenthaler, J.; Sommer, N.N.; De Toni, E.; Ilhan, H.; Zacherl, M.; Todica, A.; Paprottka, P.M. Pre-therapeutic factors for predicting survival after radioembolization: A single-center experience in 389 patients. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 1185–1193. [Google Scholar] [CrossRef] [PubMed]
- Ingrisch, M.; Schöppe, F.; Paprottka, K.; Fabritius, M.; Strobl, F.F.; Toni, E.N.D.; Ilhan, H.; Todica, A.; Michl, M.; Paprottka, P.M. Prediction of 90Y Radioembolization Outcome from Pretherapeutic Factors with Random Survival Forests. J. Nucl. Med. 2018, 59, 769–773. [Google Scholar] [CrossRef]
- Fabritius, M.P.; Hartmann, F.; Seidensticker, R.; Pech, M.; Powerski, M.; Grosu, S.; Maurus, S.; Todica, A.; Ilhan, H.; Omari, J.; et al. Liver Function Changes After Technetium-99m-Macroaggregated Albumin Administration and Their Predictive Value Regarding Hepatotoxicity in Patients Undergoing Yttrium-90-Radioembolization. Anticancer Res. 2021, 41, 437–444. [Google Scholar] [CrossRef]
- Denecke, T.; Rühl, R.; Hildebrandt, B.; Stelter, L.; Grieser, C.; Stiepani, H.; Werk, M.; Podrabsky, P.; Plotkin, M.; Amthauer, H.; et al. Planning transarterial radioembolization of colorectal liver metastases with Yttrium 90 microspheres: Evaluation of a sequential diagnostic approach using radiologic and nuclear medicine imaging techniques. Eur. Radiol. 2008, 18, 892–902. [Google Scholar] [CrossRef] [PubMed]
- Ishwaran, H.; Kogalur, U.B.; Blackstone, E.H.; Lauer, M.S. Random survival forests. Ann. Appl. Stat. 2008, 2, 841–860. [Google Scholar] [CrossRef]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- RC Team. R: A Language and Environment for Statistical Computing; Version 4.0.2; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Ishwaran, H.; Kogalur, U.B. Randomforestsrc: Fast Unified Random Forests for Survival, Regression, and Classification (RF-SRC), 2.9.3. 2020. Available online: http://web.ccs.miami.edu/~hishwaran/ishwaran.html (accessed on 8 July 2021).
- Therneau, T.M.; Lumley, T.; Elizabeth, A.; Cynthia, C. Survival: Survival Analysis, 3.2-7. 2020. Available online: https://github.com/therneau/survival (accessed on 13 August 2021).
- Harrell, F.E.; Califf, R.M.; Pryor, D.B.; Lee, K.L.; Rosati, R.A. Evaluating the Yield of Medical Tests. JAMA 1982, 247, 2543–2546. [Google Scholar] [CrossRef]
- Brier, G.W. Verification of Forecasts Expressed in Terms of Probability. Mon. Weather Rev. 1950, 78, 1–3. [Google Scholar] [CrossRef]
- Ishwaran, H.; Kogalur, U.B.; Gorodeski, E.Z.; Minn, A.J.; Lauer, M.S. High-Dimensional Variable Selection for Survival Data. J. Am. Stat. Assoc. 2010, 105, 205–217. [Google Scholar] [CrossRef]
- Apley, D.W.; Zhu, J. Visualizing the Effects of Predictor Variables in Black Box Supervised Learning Models. arXiv 2016, arXiv:1612.08468. [Google Scholar] [CrossRef]
- Friedman, J.H. Greedy function approximation: A gradient boosting machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Molnar, C. 5.3 Accumulated Local Effects (ALE) Plot. In Interpretable Machine Learning; Leanpub: Victoria, BC, Canada, 2019. [Google Scholar]
- Hallet, J.; Law, C.H.; Cukier, M.; Saskin, R.; Liu, N.; Singh, S. Exploring the rising incidence of neuroendocrine tumors: A population-based analysis of epidemiology, metastatic presentation, and outcomes. Cancer 2015, 121, 589–597. [Google Scholar] [CrossRef]
- Braat, M.N.; van Erpecum, K.J.; Zonnenberg, B.A.; van den Bosch, M.A.; Lam, M.G. Radioembolization-induced liver disease: A systematic review. Eur. J. Gastroenterol. Hepatol. 2017, 29, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Sangro, B.; Gil-Alzugaray, B.; Rodriguez, J.; Sola, I.; Martinez-Cuesta, A.; Viudez, A.; Chopitea, A.; Iñarrairaegui, M.; Arbizu, J.; Bilbao, J.I. Liver disease induced by radioembolization of liver tumors. Cancer 2008, 112, 1538–1546. [Google Scholar] [CrossRef] [PubMed]
- Feller, R.M.; Bitzer, M.; Zender, L.; Malek, N.P.; Plentz, R.R. Untersuchung zum Stellenwert der Cholinesterase (CHE) als prädiktiver Marker für das Therapieansprechen der transarteriellen Chemoembolisation (TACE) von Patienten mit hepatozellulärem Karzinom (HCC). Z. Gastroenterol. 2016, 54, KV299. [Google Scholar] [CrossRef]
- Takaki, S.; Fukuhara, T.; Mori, N.; Tsuji, K. High cholinesterase predicts tolerance to sorafenib treatment and improved prognosis in patients with transarterial chemoembolization refractory intermediate stage hepatocellular carcinoma. Mol. Clin. Oncol. 2020, 12, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Takeda, H.; Nishikawa, H.; Iguchi, E.; Ohara, Y.; Sakamoto, A.; Hatamaru, K.; Henmi, S.; Saito, S.; Nasu, A.; Komekado, H.; et al. Impact of pretreatment serum cholinesterase level in unresectable advanced hepatocellular carcinoma patients treated with sorafenib. Mol. Clin. Oncol. 2013, 1, 241–248. [Google Scholar] [CrossRef]
- Mendel, B.; Rudney, H. Studies on cholinesterase: 1. Cholinesterase and pseudo-cholinesterase. Biochem. J. 1943, 37, 59–63. [Google Scholar] [CrossRef]
- Ballmer, P.E. Causes and mechanisms of hypoalbuminaemia. Clin. Nutr. 2001, 20, 271–273. [Google Scholar] [CrossRef]
- Levitt, D.G.; Levitt, M.D. Human serum albumin homeostasis: A new look at the roles of synthesis, catabolism, renal and gastrointestinal excretion, and the clinical value of serum albumin measurements. Int. J. Gen. Med. 2016, 9, 229. [Google Scholar] [CrossRef]
- Meng, F.; Yin, X.; Ma, X.; Guo, X.D.; Jin, B.; Li, H. Assessment of the value of serum cholinesterase as a liver function test for cirrhotic patients. Biomed. Rep. 2013, 1, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Damm, R.; Seidensticker, R.; Ulrich, G.; Breier, L.; Steffen, I.G.; Seidensticker, M.; Garlipp, B.; Mohnike, K.; Pech, M.; Amthauer, H.; et al. Y90 Radioembolization in chemo-refractory metastastic, liver dominant colorectal cancer patients: Outcome assessment applying a predictive scoring system. BMC Cancer 2016, 16, 509. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Center 1 (n = 366) | Center 2 (n = 202) |
|---|---|---|
| Age (y) | 64 (55.7–71.0) | 66 (58.0–71.0) |
| Sex | ||
| Male | 217 (59.3) | 124 (61.4) |
| Female | 149 (40.7) | 78 (38.6) |
| Primary tumor | ||
| Colorectal cancer | 128 (35.0) | 81 (40.1) |
| Hepatocellular cancer | 57 (15.6) | 57 (28.2) |
| Neuroendocrine tumor | 51 (13.9) | 4 (2.0) |
| Metastatic breast cancer | 40 (10.9) | 28 (13.9) |
| Cholangiocarcinoma | 35 (9.6) | 5 (2.5) |
| Other | 55 (15.0) | 27 (13.4) |
| Hepatic tumor burden | ||
| 25% | 191 (52.2) | 133 (65.8) |
| 25–50% | 140 (38.3) | 53 (26.2) |
| 50% | 35 (9.6) | 16 (7.9) |
| Extrahepatic disease | ||
| Yes | 253 (69.1) | 101 (50.0) |
| No | 113 (30.9) | 101 (50.0) |
| Baseline liver function | ||
| Bilirubin (mg/dL) | 0.60 (0.50–0.90) | 0.51 (0.35–0.78) |
| Cholinesterase (U/L) | 6.35 (4.89–7.60) | 5.88 (4.34–7.50) |
| Cohort | Patients | Events | Median Survival (Months) | 95% CI |
|---|---|---|---|---|
| Center 1 | 366 | 228 | 11.41 | 9.70–14.20 |
| Center 2 | 202 | 199 | 7.91 | 7.07–9.24 |
| Model | Training | Prediction | C-index | IBS |
|---|---|---|---|---|
| RSF | Center 1 | Center 1 | 0.66 | 0.08 |
| RSF | Center 1 | Center 2 | 0.67 | 0.12 |
| RSF | Center 2 | Center 1 | 0.66 | 0.20 |
| RSF | Center 2 | Center 2 | 0.68 | 0.05 |
| CPH | Center 1 | Center 1 | 0.68 | 0.15 |
| CPH | Center 1 | Center 2 | 0.69 | 0.12 |
| CPH | Center 2 | Center 1 | 0.68 | 0.18 |
| CPH | Center 2 | Center 2 | 0.72 | 0.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fabritius, M.P.; Seidensticker, M.; Rueckel, J.; Heinze, C.; Pech, M.; Paprottka, K.J.; Paprottka, P.M.; Topalis, J.; Bender, A.; Ricke, J.; et al. Bi-Centric Independent Validation of Outcome Prediction after Radioembolization of Primary and Secondary Liver Cancer. J. Clin. Med. 2021, 10, 3668. https://doi.org/10.3390/jcm10163668
Fabritius MP, Seidensticker M, Rueckel J, Heinze C, Pech M, Paprottka KJ, Paprottka PM, Topalis J, Bender A, Ricke J, et al. Bi-Centric Independent Validation of Outcome Prediction after Radioembolization of Primary and Secondary Liver Cancer. Journal of Clinical Medicine. 2021; 10(16):3668. https://doi.org/10.3390/jcm10163668
Chicago/Turabian StyleFabritius, Matthias Philipp, Max Seidensticker, Johannes Rueckel, Constanze Heinze, Maciej Pech, Karolin Johanna Paprottka, Philipp Marius Paprottka, Johanna Topalis, Andreas Bender, Jens Ricke, and et al. 2021. "Bi-Centric Independent Validation of Outcome Prediction after Radioembolization of Primary and Secondary Liver Cancer" Journal of Clinical Medicine 10, no. 16: 3668. https://doi.org/10.3390/jcm10163668
APA StyleFabritius, M. P., Seidensticker, M., Rueckel, J., Heinze, C., Pech, M., Paprottka, K. J., Paprottka, P. M., Topalis, J., Bender, A., Ricke, J., Mittermeier, A., & Ingrisch, M. (2021). Bi-Centric Independent Validation of Outcome Prediction after Radioembolization of Primary and Secondary Liver Cancer. Journal of Clinical Medicine, 10(16), 3668. https://doi.org/10.3390/jcm10163668






