The Use of Adipose-Derived Stem Cells (ADSCs) and Stromal Vascular Fraction (SVF) in Skin Scar Treatment—A Systematic Review of Clinical Studies
Abstract
1. Introduction
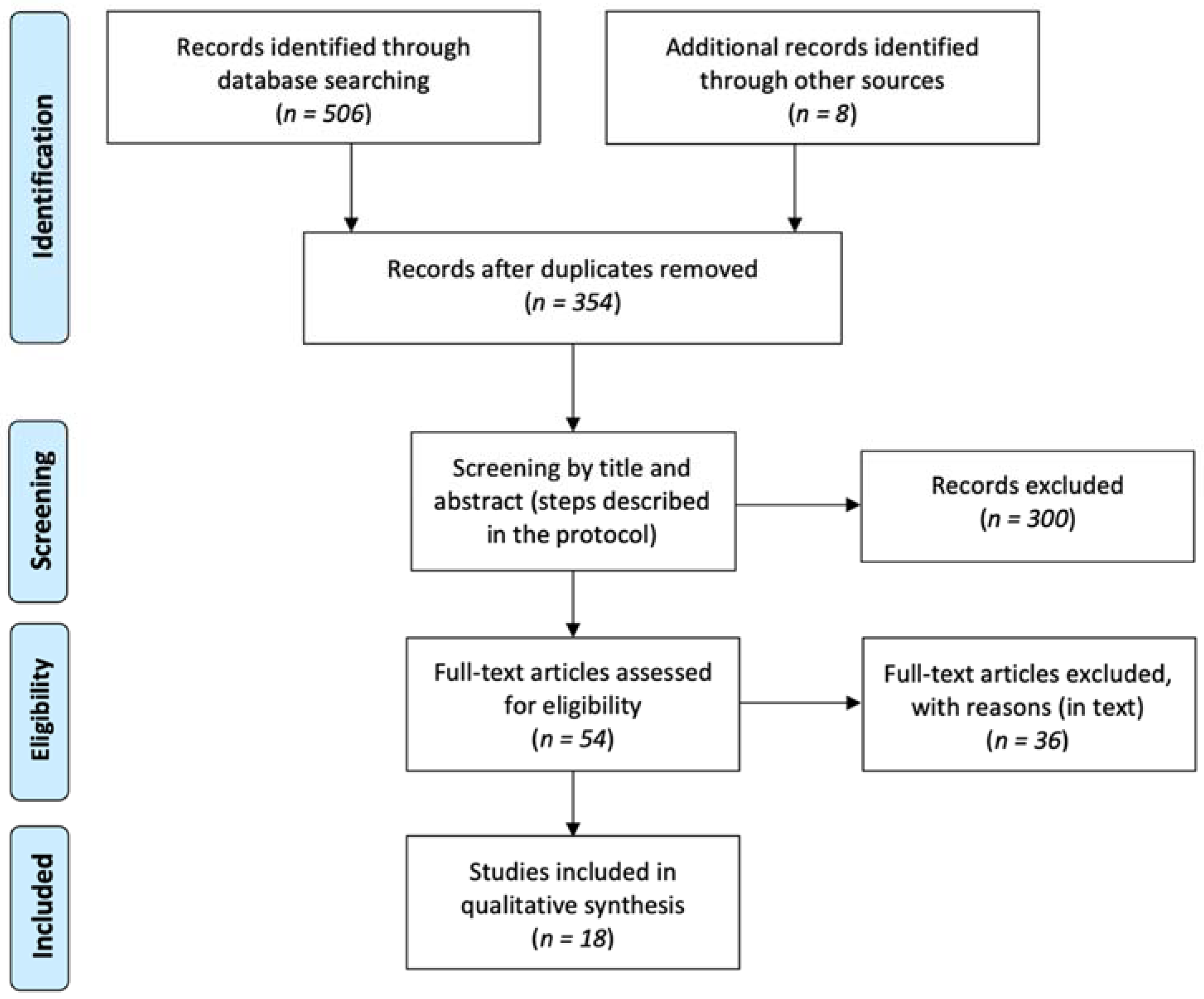
2. Materials and Methods
2.1. Study Selection
2.2. Data Extraction, Risk of Bias and Analyses
3. Results
3.1. Search Results
3.2. Case Reports
3.3. Case Series
3.4. Case-Control Studies
3.5. Prospective Cohort Studies
3.6. Randomized Controlled Trials
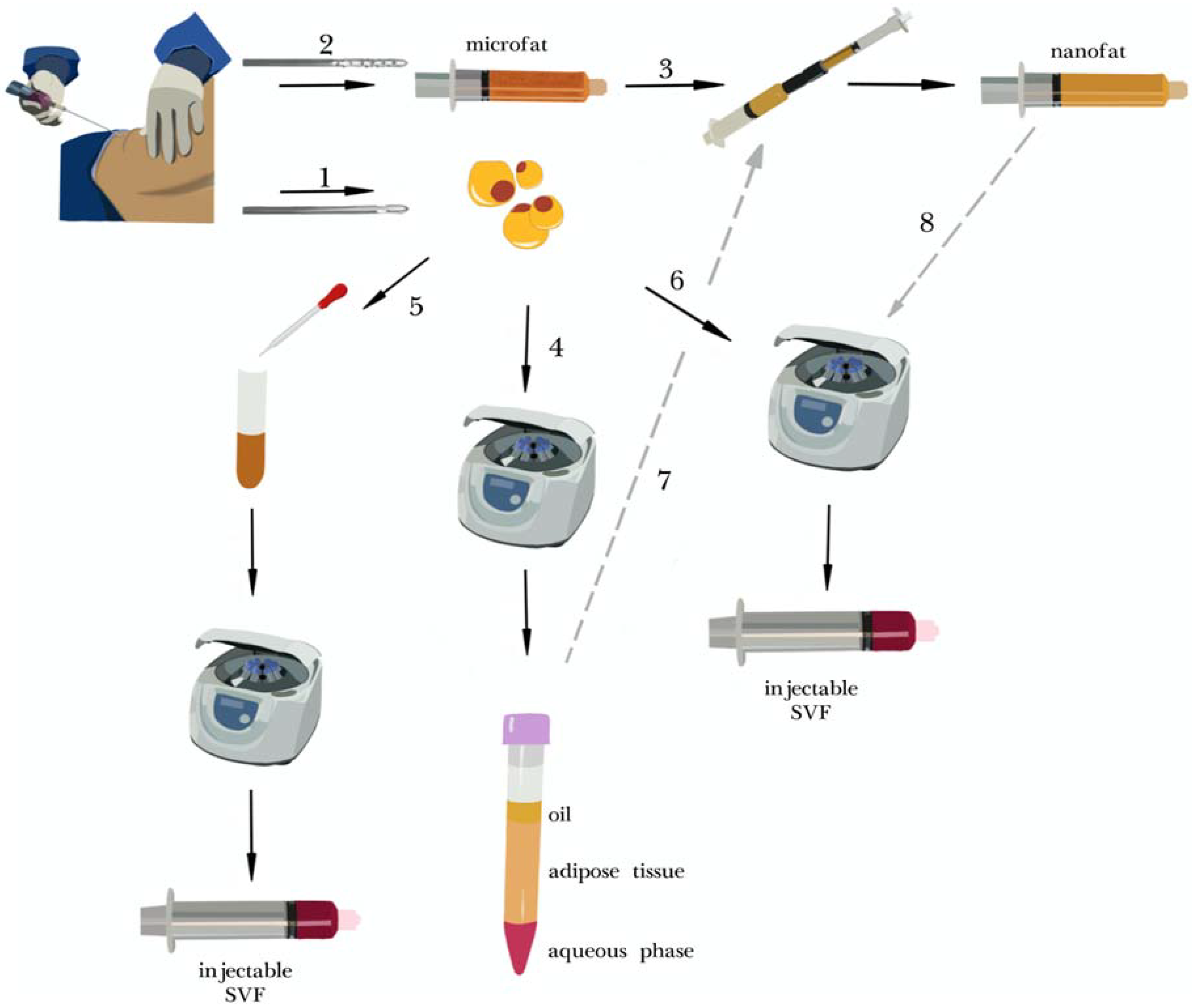
3.7. Isolation Protocols
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khansa, I.; Harrison, B.; Janis, J. Evidence-Based Scar Management. Plast. Reconstr. Surg. 2016, 138, 165S–178S. [Google Scholar] [CrossRef] [PubMed]
- Cannarozzo, G.; Silvestri, M.; Tamburi, F.; Sicilia, C.; Del Duca, E.; Scali, E.; Bennardo, L.; Nisticò, S.P. A new 675-nm laser device in the treatment of acne scars: An observational study. Lasers Med. Sci. 2021, 36, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Alser, O.H.; Goutos, I. The evidence behind the use of platelet-rich plasma (PRP) in scar management: A literature review. Scars Burn. Heal. 2018, 4, 118808773. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Shi, K.; Zhu, X.; Zhao, H.; Zhang, H.; Jones, A.; Liu, L.; Li, G. Adipose Tissue-derived Stem cells in Plastic and Re-constructive Surgery: A Bibliometric Study. Aesthetic Plast. Surg. 2020. [Google Scholar] [CrossRef]
- Rigotti, G.; Marchi, A.; Galie’, M.; Baroni, G.; Benati, D.; Krampera, M.; Pasini, A.; Sbarbati, A.; Rubin, J.P.; Marra, K.G. Clinical Treatment of Radiotherapy Tissue Damage by Lipoaspirate Transplant: A Healing Process Mediated by Adipose-Derived Adult Stem Cells. Plast. Reconstr. Surg. 2007, 119, 1409–1422. [Google Scholar] [CrossRef]
- Rehman, J.; Traktuev, D.; Li, J.; Merfeld-Clauss, S.; Temm-Grove, C.J.; Bovenkerk, J.E.; Pell, C.L.; Johnstone, B.H.; Considine, R.V.; March, K.L. Secretion of Angiogenic and Antiapoptotic Factors by Human Adipose Stromal Cells. Circulation 2004, 109, 1292–1298. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, W.; Rubin, J.P.; Marra, K.G. Adipose-derived stem cells: Implications in tissue regeneration. World J. Stem Cells 2014, 6, 312–321. [Google Scholar] [CrossRef]
- Condé-Green, A.; Marano, A.A.; Lee, E.S.; Reisler, T.; Price, L.A.; Milner, S.M.; Granick, M. Fat Grafting and Adipose-Derived Regenerative Cells in Burn Wound Healing and Scarring. Plast. Reconstr. Surg. 2016, 137, 302–312. [Google Scholar] [CrossRef]
- Negenborn, V.L.; Groen, J.-W.; Smit, J.M.; Niessen, F.B.; Mullender, M.G. The Use of Autologous Fat Grafting for Treatment of Scar Tissue and Scar-Related Conditions. Plast. Reconstr. Surg. 2016, 137, 31e–43e. [Google Scholar] [CrossRef]
- Walocko, F.M.; Eber, A.E.; Kirsner, R.S.; Badiavas, E.; Nouri, K. Systematic review of the therapeutic roles of adipose tissue in dermatology. J. Am. Acad. Dermatol. 2018, 79, 935–944. [Google Scholar] [CrossRef]
- To, K.; Crowley, C.; Lim, S.-K.; Khan, W.S. Autologous adipose tissue grafting for the management of the painful scar. Cytotherapy 2019, 21, 1151–1160. [Google Scholar] [CrossRef]
- Krastev, T.K.; Schop, S.J.; Hommes, J.; Piatkowski, A.; Van Der Hulst, R.R. Autologous fat transfer to treat fibrosis and scar-related conditions: A systematic review and meta-analysis. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 2033–2048. [Google Scholar] [CrossRef]
- Tonnard, P.; Verpaele, A.; Peeters, G.; Hamdi, M.; Cornelissen, M.; Declercq, H. Nanofat Grafting. Plast. Reconstr. Surg. 2013, 132, 1017–1026. [Google Scholar] [CrossRef]
- Sesé, B.; Sanmartín, J.M.; Ortega, B.; Matas-Palau, A.; Llull, R. Nanofat Cell Aggregates. Plast. Reconstr. Surg. 2019, 144, 1079–1088. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Almadori, A.; Bussu, F.; Parrilla, C.; Rigante, M.; Barone-Adesi, L.; Salgarello, M. Autologous fat graft as new therapeutic approach to late effect of radiotherapy in head and neck cancers. Eur. Surg. Res. 2012, 49, 131. [Google Scholar] [CrossRef]
- Tissue Engineering and Regenerative Medicine. J. Tissue Eng. Regen. Med. 2012, 6, 1–429. [CrossRef] [PubMed]
- Embaby, A.S.; El-Shaer, W.; Abdl-Hasib, A.; Korany, M. Histological study of the role of fat injection in scar remodeling following burn injury. Egypt. J. Histol. 2012, 35, 437–447. [Google Scholar] [CrossRef]
- Baptista, C.; Iniesta, A.; Nguyen, P.; Legré, R.; Gay, A.-M. Greffe de tissu adipeux autologue dans la prise en charge chirurgicale des cicatrices douloureuses: Résultats préliminaires. Chir. Main 2013, 32, 329–334. [Google Scholar] [CrossRef]
- Balkin, D.M.; Samra, S.; Steinbacher, D.M. Immediate fat grafting in primary cleft lip repair. J. Plast. Reconstr. Aesthetic Surg. 2014, 67, 1644–1650. [Google Scholar] [CrossRef]
- Lupo, F.; Ioppolo, L.M.; Pino, D.; Meduri, A.; D’Alcontres, F.S.; Colonna, M.R.; Delia, G. Lipograft in cicatricial ectropion. Ann. Ital. Chir. 2016, 87, 466–469. [Google Scholar]
- Piccolo, N.S.; Piccolo, M.S.; Piccolo, M.T.S. Fat grafting for treatment of burn and other wounds and burn scars. J. Burn. Care Res. 2016, 37, S277. [Google Scholar] [CrossRef]
- De Gast, H.; Torrensma, B.; Fitzgerald, E.; Stevens, H. The Treatment of Chronic Neuropathic Pain: Bio (Regenerative) Pain Treatment through Lipofilling. A Short Communication Case Series. Pain Physician 2016, 19, 495–498. [Google Scholar] [CrossRef]
- Jo, D.I.; Yang, H.J.; Kim, S.H.; Kim, C.K.; Park, H.J.; Choi, H.G.; Shin, D.H.; Uhm, K.I. Coverage of Skin Defects Without Skin Grafts Using Adipose-Derived Stem Cells. Aesthetic Plast. Surg. 2013, 37, 1041–1051. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Park, S.H.; Lee, B.H.; Jeong, H.S.; Yang, H.J.; Suh, I.S. Early Intervention with Highly Condensed Adipose-Derived Stem Cells for Complicated Wounds Following Filler Injections. Aesthetic Plast. Surg. 2016, 40, 428–434. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lander, E.B.; Berman, M.H.; See, J.R. Stromal Vascular Fraction Combined with Shock Wave for the Treatment of Peyronie’s Disease. Plast. Reconstr. Surg. Glob. Open 2016, 4, e631. [Google Scholar] [CrossRef] [PubMed]
- NCT. Evaluation of the Efficacy and Tolerability of Autologous Adipose Tissue Derived Stem Cells on Facial Rejuvenation. 2019. Available online: https://clinicaltrials.gov/show/NCT03928444 (accessed on 20 July 2020).
- Almadori, A.; Hansen, E.; Boyle, D.; Zenner, N.; Swale, V.; Reid, W.; MacLane, A.; Butler, P.E. Fat Grafting Improves Fibrosis and Scarring in Vulvar Lichen Sclerosus: Results from a Prospective Cohort Study. J. Low. Genit. Tract Dis. 2020, 24, 305–310. [Google Scholar] [CrossRef]
- Sung, H.M.; Suh, I.S.; Lee, H.-B.; Tak, K.S.; Moon, K.M.; Jung, M.S. Case Reports of Adipose-derived Stem Cell Therapy for Nasal Skin Necrosis after Filler Injection. Arch. Plast. Surg. 2012, 39, 51–54. [Google Scholar] [CrossRef][Green Version]
- Coban, Y.K. Application of the Stromal Vascular Fraction of Adipose Tissue to a Severe Great Toe Defect Resulting from Third-Degree Electrical Burn Injury. J. Burn. Care Res. 2019, 40, 1009–1011. [Google Scholar] [CrossRef]
- Planas, J.; Cruz, A.M. Nanofat: 5 Years Experience. Approaches Aging Control. 2019, 30–38. [Google Scholar]
- Van Dongen, J.A.; Stevens, H.P.; Parvizi, M.; Van Der Lei, B.; Harmsen, M.C. The fractionation of adipose tissue procedure to obtain stromal vascular fractions for regenerative purposes. Wound Repair Regen. 2016, 24, 994–1003. [Google Scholar] [CrossRef]
- NCT. Efficacy and Safety of a Nanofat-Seeded Biological Scaffold in Healing Lower Limb Surgical Defects. 2018. Available online: https://clinicaltrials.gov/show/NCT03548610 (accessed on 20 July 2020).
- Moon, K.-C.; Chung, H.-Y.; Han, S.-K.; Jeong, S.-H.; Dhong, E.-S. Tissue-engineered dermis grafts using stromal vascular fraction cells on the nose: A retrospective case-control study. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 965–974. [Google Scholar] [CrossRef]
- Lu, H.-J.; Chen, T.-L.; Zhang, X.-H.; Liu, J.; Bao, H.-W. Antibacterial Effects of Platelet-Rich Plasma in Promoting Facial Scars Healing in Combination with Adipose-Derived Stromal Vascular Fraction Cells. J. Craniofacial Surg. 2015, 26, e670–e672. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liao, Y.; Dong, Z.; Lu, F.; Cai, J. Treatment of Nasal Scars Caused by Skin Necrosis from Hyaluronic Acid Injections Using Stromal Vascular Fraction Gel, a Novel Fat Tissue–Derived Product. Dermatol. Surg. 2020, 46, 985–988. [Google Scholar] [CrossRef] [PubMed]
- Vinci, V.; Klinger, M.; Klinger, F.M.; Forcellini, D.; Borbon, G.; Caviggioli, F. Treatment outcomes for keloid scar management in the pediatric burn population. Burns 2013, 39, 1321–1322. [Google Scholar] [CrossRef] [PubMed]
- Ou, L.D.; Zhang, A.J.; Li, A.; Tao, S.J.; Xu, M.M.; Li, Q.; Jin, P.S. Effect of human stromal vascular fraction gel on the treat-ment of patients with skin depressed scar and its mechanism. Chin. J. Burn. 2019, 35, 859–865. [Google Scholar] [CrossRef]
- Zou, Y.L.; Tan, X.; Tian, T.; Li, L.; Li, Z.X.; Cheng, W.; Wang, Z.X. Clinical effect of nano-fat mixed granule fat transplanta-tion in the treatment of cicatricial facial depression and atrophy and the related experimental mechanism. Chin. J. Burn. 2019, 35, 266–276. [Google Scholar] [CrossRef]
- L’Orphelin, J.-M.; Garmi, R.; Labbé, D.; Benateau, H.; Dompmartin, A. Autologous fat grafting for the treatment of sclerotic lesions and scars. Ann. Dermatol. Vénéréologie 2021, 148, 40–44. [Google Scholar] [CrossRef]
- NCT. Efficacy of Adipose Derived Stromal Vascular Fraction in the Treatment of Keloids. 2020. Available online: https://clinicaltrials.gov/show/NCT04391621 (accessed on 20 July 2020).
- NCT. Scar Tissue Analysis after Intraoperative Application of Stromal Vascular Fraction Cells into Suture Line. 2020. Available online: https://clinicaltrials.gov/show/NCT04238468 (accessed on 20 July 2020).
- Kim, M.; Kim, I.; Lee, S.K.; Bang, S.I.; Lim, S.Y. Clinical Trial of Autologous Differentiated Adipocytes from Stem Cells Derived from Human Adipose Tissue. Dermatol. Surg. 2011, 37, 750–759. [Google Scholar] [CrossRef]
- Ntr. Stromal Vascular Fraction Injectable as a Preventive Treatment of Scars. 2016. Available online: http://www.who.int/trialsearch/Trial2.aspx?TrialID=NTR5719 (accessed on 20 July 2020).
- Euctr, P.L. Evaluation the Safety and Efficacy of the Treatment of Scars and Cutis Laxa Syndrome with the Use of Autologous (Fresh and Stored) Stem Cells Isolated from Adipose Tissue within the Project: ’The Therapeutic Potential of Mesenchymal Stem Cells Tested in Clinical Trials and In Vitro—A Justification for Characterized Cells Storage’. 2017. Available online: http://www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2016-004110-10-PL (accessed on 20 July 2020).
- NCT. Role of Stem Cells, Platelet Rich Plasma in Treatment of Scars. 2017. Available online: https://clinicaltrials.gov/show/NCT03264573 (accessed on 20 July 2020).
- NCT. Therapy of Scars and Cutis Laxa with Autologous Adipose Derived Mesenchymal Stem Cells. 2019. Available online: https://clinicaltrials.gov/show/NCT03887208 (accessed on 20 July 2020).
- Hamidieh, A.A. The 3rd National Festival & International Congress on Stem Cell & Regenerative Medicine. BioImpacts 2018, 8, S1–S129. [Google Scholar] [CrossRef]
- Gamal, H.; Osman, A.; Eldien, H.S.; El Oteify, M. Role of stem cells, platelet rich plasma and combination of them in treatment of scars. Cytotherapy 2018, 20, S116. [Google Scholar] [CrossRef]
- Wu, A.Y.; Morrow, D.M. Autologous fat transfer with in-situ mediation (AIM): A novel and compliant method of adult mesenchymal stem cell therapy. J. Transl. Med. 2013, 11, 136. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gentile, P.; De Angelis, B.; Pasin, M.; Cervelli, G.; Curcio, C.B.; Floris, M.; Di Pasquali, C.; Bocchini, I.; Balzani, A.; Nicoli, F.; et al. Adipose-Derived Stromal Vascular Fraction Cells and Platelet-Rich Plasma. J. Craniofacial Surg. 2014, 25, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Carstens, M.H.; Correa, D.; Llull, R.; Gomez, A.; Turner, E.; Valladares, L.S. Subcutaneous reconstruction of hand dorsum and fingers for late sequelae of burn scars using adipose-derived stromal vascular fraction (SVF). CellR4 2015, 3, e1675. [Google Scholar]
- Elkahky, H.O.; Fathy, G.; Abu-Zahra, F.A.; Afify, A.A. Autologous adipose-derived adult stem cells injection versus platelet-rich plasma injection in the treatment of rolling postacne scars. J. Egypt. Women’s Dermatol. Soc. 2016, 13, 165–172. [Google Scholar] [CrossRef]
- Zhou, B.-R.; Zhang, T.; Bin Jameel, A.A.; Xu, Y.; Guo, S.-L.; Wang, Y.; Permatasari, F.; Luo, D.; Xu, Y. The efficacy of conditioned media of adipose-derived stem cells combined with ablative carbon dioxide fractional resurfacing for atrophic acne scars and skin rejuvenation. J. Cosmet. Laser Ther. 2016, 18, 138–148. [Google Scholar] [CrossRef]
- Gentile, P.; Scioli, M.G.; Bielli, A.; Orlandi, A.; Cervelli, V. Comparing different nanofat procedures on scars: Role of the stromal vascular fraction and its clinical implications. Regen. Med. 2017, 12, 939–952. [Google Scholar] [CrossRef]
- Tenna, S.; Cogliandro, A.; Barone, M.; Panasiti, V.; Tirindelli, M.; Nobile, C.; Persichetti, P. Comparative Study Using Autologous Fat Grafts Plus Platelet-Rich Plasma with or without Fractional CO2 Laser Resurfacing in Treatment of Acne Scars: Analysis of Outcomes and Satisfaction With FACE-Q. Aesthetic Plast. Surg. 2017, 41, 661–666. [Google Scholar] [CrossRef]
- Zayed, H.M.; Ghareeb, F.; Elsakka, D.M.; Alkhateep, Y. Improving esthetic outcome of facial scars by fat grafting. Menoufia Med. J. 2017, 30, 412. [Google Scholar] [CrossRef]
- Carstens, M.H.; Pérez, M.; Briceño, H.; Valladares, S.; Correa, D. Treatment of late sequelae of burn scar fibrosis with adi-pose-derived stromal vascular fraction (SVF) cells: A case series. CellR4 2017, 5, e2404. [Google Scholar]
- Bhooshan, L.S.; Devi, M.G.; Aniraj, R.; Binod, P.; Lekshmi, M. Autologous emulsified fat injection for rejuvenation of scars: A prospective observational study. Indian J. Plast. Surg. 2018, 51, 077–083. [Google Scholar] [CrossRef] [PubMed]
- Gu, Z.; Li, Y.; Li, H. Use of Condensed Nanofat Combined with Fat Grafts to Treat Atrophic Scars. JAMA Facial Plast. Surg. 2018, 20, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Park, S.H.; Lee, S.J.; Kim, S.; Suh, I.S.; Jeong, H.S. Clinical Impact of Highly Condensed Stromal Vascular Fraction Injection in Surgical Management of Depressed and Contracted Scars. Aesthetic Plast. Surg. 2018, 42, 1689–1698. [Google Scholar] [CrossRef] [PubMed]
- Uyulmaz, S.; Sanchez-Macedo, N.; Rezaeian, F.; Giovanoli, P.; Lindenblatt, N. Nanofat Grafting for Scar Treatment and Skin Quality Improvement. Aesthetic Surg. J. 2018, 38, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Eitta, R.S.A.; Ismail, A.A.; Abdelmaksoud, R.A.; Ghezlan, N.A.; Mehanna, R.A. Evaluation of autologous adipose-derived stem cells vs. fractional carbon dioxide laser in the treatment of post acne scars: A split-face study. Int. J. Dermatol. 2019, 58, 1212–1222. [Google Scholar] [CrossRef]
- Gaba, S.; Malik, P.; Ahuja, C.; Sharma, R.; Sharma, R.; Khandelwal, N. Role of fat graft alone versus enriched fat graft with stromal vascular filtrate in painful amputation stump. Indian J. Orthop. 2019, 53, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Jan, S.N.; Bashir, M.M.; Khan, F.A.; Hidayat, Z.; Ansari, H.H.; Sohail, M.; Bajwa, A.B.; Shami, H.B.; Hanif, A.; Aziz, F.; et al. Unfiltered Nanofat Injections Rejuvenate Postburn Scars of Face. Ann. Plast. Surg. 2019, 82, 28–33. [Google Scholar] [CrossRef]
- Shalaby, M.E.-S.; Ibrahim, S.M.A.; Hassanin, M.N.A. Nanofat combined with platelet rich plasma injection versus nanofat injection alone in the treatment of atrophic scar. Al-Azhar Med. J. 2020, 49, 611–620. [Google Scholar] [CrossRef]
- Pallua, N.; Kim, B.-S. Microfat and Lipoconcentrate for the Treatment of Facial Scars. Clin. Plast. Surg. 2020, 47, 139–145. [Google Scholar] [CrossRef]
- Coleman, S.R. Structural Fat Grafting. Aesthetic Surg. J. 1998, 18, 386–388. [Google Scholar] [CrossRef]
- Fearmonti, R.; Bond, J.; Erdmann, D.; Levinson, H. A Review of Scar Scales and Scar Measuring Devices. Eplasty 2010, 10, 43. [Google Scholar]
- Mashiko, T.; Wu, S.-H.; Feng, J.; Kanayama, K.; Kinoshita, K.; Sunaga, A.; Narushima, M.; Yoshimura, K. Mechanical Mi-cronization of Lipoaspirates. Plast. Reconstr. Surg. 2017, 139, 79–90. [Google Scholar] [CrossRef]
- Pallua, N.; Grasys, J.; Kim, B.-S. Enhancement of Progenitor Cells by Two-Step Centrifugation of Emulsified Lipoaspirates. Plast. Reconstr. Surg. 2018, 142, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Prantl, L.; Eigenberger, A.; Klein, S.; Limm, K.; Oefner, P.J.; Schratzenstaller, T.; Felthaus, O. Shear Force Processing of Lipoaspirates for Stem Cell Enrichment Does Not Affect Secretome of Human Cells Detected by Mass Spectrometry In Vitro. Plast. Reconstr. Surg. 2020, 146, 749e–758e. [Google Scholar] [CrossRef]
| Reference | Study Design (Level of Evidence) | SVF/ADSC Isolation Technique | No. of Patients (Scars) | Scar Types | Treatment (Study Groups) | Clinical/Macroscopic Outcomes | Microscopic Findings |
|---|---|---|---|---|---|---|---|
| Wu et al. 2013 [51] | Case report (V) | SVF: Gravitational decanting -> Coleman’s procedure -> spectroscopy | 1 | cicatrix scar after lipoma excision on the back | PALF with SVF-enriched autologous fat transfer in conjunction with collagenase and hyaluronic acid serum with trichloroacetic acid peeling | Resolution of scar adherence against the muscle, reduced swelling, quicker epithelialization, improvement in clinical (texture, color, size) and ultrasonographic examination, and pain resolution * | None were examined due to patient’s lack of consent. |
| Gentile et al. 2014 [52] | Case-control (III) | SVF: Enzymatic isolation with a commercially available system | 30 | burn or post-traumatic scars | 1. Coleman’s fat graft (control) 2. SVF-enriched autologous fat graft 3. Coleman’s fat graft + PRP | Contour restoring and volume maintenance improvement (39%—control, 63%—SVF, 69%—PRP)†, lower fat reabsorption in facial scars in study groups vs. control *. Patients’ satisfaction with texture, softness and contour in all groups *. | None were examined. |
| Carstens et al. 2015 [53] | Case report (V) | SVF: Enzymatic digestion -> centrifugation | 1 | fibrosis of the right hand as late sequelae of a burn scar | Local injections of isolated SVF into 4 MCP joints and SVF-enriched lipofilling of the dorsum of the hand | Range of motion restoration in MCP, PIP and DIP joints, full opposition of the thumb after 6 weeks. Improvement of skin color and elasticity. Increased vascularization * | None were examined. |
| Elkahky et al. 2016 [54] | Low-quality randomized controlled trial (II) | SVF: Enzymatic digestion -> centrifugation -> filtering | 20 | atrophic rolling facial post-acne scars | 1. Intradermal injection of SVF 2. Intradermal injection of PRP underneath the scars on the entire face | Total scar surface area reduction after 1 month (no difference between groups) and 3 months (66.49 ± 12.82—SVF vs. 80.2 ± 8.9 in the PRP group †). Patients reported high satisfaction rates and good treatment tolerance *. | At 3 month follow-up, increased epidermal thickness, number and density of collagen and elastic fibers †, redevelopment of rete processes, acanthosis, spongiosis |
| Zhou et al. 2016 [55] | Prospective cohort study (II) | ADSC-CM: Enzymatic digestion -> centrifugation -> filtering -> centrifugation -> cell culture -> conditioning in hypoxia -> medium collection | 13 | Facial atrophic acne scars | Split-face study: 1. 3 × FxCR + topical DMEM (control) 2. 3 × FxCR + topical ADSC-CM | Higher patients’ satisfaction (2.35 ± 0.69 vs. 2.08 ± 0.76) and clinical improvement in the study group, measured with ECCA score (32.69 ± 18.1 vs. 26.15 ± 19.16) †. Lower melanin index and TEWL; higher elasticity and hydration in ADSC-CM-treated group †. | Semi-quantitative analysis showed increased collagen (49.9 ± 0.6% vs. 36.1 ± 0.6%) and elastin (37.6 ± 0.8 vs. 26.1 ± 0.4%) density†, more orderly alignment of fibers in ADSC-CM treated sample *. |
| Gentile et al. 2017 [56] | Low-quality randomized controlled trial (II) | Nanofat: 1. Mechanical dissociation -> filtering 2. Mechanical isolation of SVF with commercially available system + nanofat 3. Centrifugation -> mechanical fat dissociation 4. Low-speed centrifugation -> mechanical fat dissociation | 43 | burn or post-traumatic scars | Intradermal injections: 1. Nanofat (control) 2. Supercharged nanofat (SVF-enriched nanofat) 3. Centrifuged nanofat 4. Evo nanofat | Scoring of pigmentation, vascularization, pliability, thickness, itching and pain by the patients and operator showed that supercharged (means 25.6; 25.7) > evo (means 25.3; 25.2) > centrifuged (means 24; 23.8) > classic nanofat (means 22.6; 22) †. | Significant improvement of epidermal and dermal thickness in all studied groups after 6 months with no difference between them†. New collagen and vessels formation in a representative sample from the supercharged group *. |
| Tenna et al. 2017 [57] | Low-quality randomized controlled trial (II) | Nanofat: Coleman’s procedure -> mechanical emulsification | 30 | Chronic acne scars | Two treatments (6 months interval) with either (subcutaneous injections): 1. Nanofat + PRP (control) or 2. Nanofat + PRP +FxCR | Significant improvement of skin thickness 3 months after the 2nd treatment in group 2 (0.74 cm vs. 1.37 cm) †, but not in control (0.53 cm vs. 1.2 cm), compared with baseline. No difference in skin thickness increase between the groups. | None were examined. |
| Ghareeb et al. 2017 [58] | Case series (IV) | Nanofat: Coleman’s procedure -> mechanical emulsification | 30 | Facial scars—various etiology—26 were atrophic | Subcutaneous nanofat injections | Significant improvement in scar vascularity, pigmentation, pliability and pruritus as per VSS score †. Satisfaction in 76% of the patients. | None were examined. |
| Carstens et al. 2017 [59] | Case series (IV) | SVF: Washing -> enzymatic digestion -> centrifugation | 5 (35 treatment zones) | Burn scars | Subcutaneous nanofat injections | Significant improvements in VSS score, scar hardness (durometer), elasticity (cutometer) † and patients’ satisfaction *. | None were examined |
| Bhooshan et al. 2018 [60] | Case series (IV) | Classic nanofat | 34 | Post-traumatic, burn or post-inflammatory scars | Nanofat injected intralesionally | Significant improvement in POSAS—mean 27.4 ± 7.5 vs. 14 ± 14.4 (patient’s assessment) and mean 31 ± 8.5 vs. 18 ± 6.8 (observer’s assessment). Significantly better results in younger scars (<5 years) † | None were examined. |
| Gu et al. 2018 [61] | Case series (IV) | Nanofat: Coleman’s procedure -> mechanical emulsification -> centrifugation (3000 RPM × 3min) | 20 (25) | Atrophic facial scars (post-surgical, burn, post-traumatic and post-acne) | Condensed nanofat intradermal injection. One scar required additional subcutaneous lipofilling. | Significant clinical improvement both in patient’s (28.8 ± 1.02 vs. 12.2 ± 0.8) and physician’s (18 ± 0.71 vs. 9.2 ± 0.37) assessment, measured with a POSAS score†. | 6 months post-op: increased melanin density (0.671 vs. 0.844) †. Sebaceous and sweat glands visualized with CK14 and CK19 staining. |
| Lee et al. 2018 (two studies) [62] | Case series (IV)/Case-control (III) | SVF: Centrifugation -> enzymatic digestion -> multiple centrifugations | Study 1: 17 (19) Study 2: 15 | Various; restricted to face in study 2. | Study 1: SVF injection (s.c./i.d.) alone or in the course of other procedures. Study 2: Scar revision with or without SVF injection (s.c./i.d.) (2 groups) | Study 1: Improvement of OSAS (vascularity, pigmentation, hardness, flexibility), SBSES (only in overall score), VSS (vascularity, pigmentation, pliability) and VAS median scores 6 months post-op vs. baseline† Study 2: Improvement of OSAS, VSS and VAS overall median scores, as well as height and pliability in the SVF-treated group vs. control after 6 months †. | None were examined. |
| Uyulmaz et al. 2018 [63] | Case series (IV) | Classic nanofat | 40 | Various | Nanofat injection into scars or i.d. (twice in 4 cases) | Softer and less prominent scars. Good or satisfactory clinical outcome in most cases. Improved patients’ satisfaction * | None were examined. |
| Abou Eitta et al. 2019 [64] | Prospective cohort study (II) | SVF: Washing -> enzymatic digestion -> centrifugation | 10 | post-acne scars | Split-face study: 1st half—intradermal SVF injection 2nd half—3 × FxCR | At 3 month follow-up, significant reduction in scar severity and area percentage compared to baseline. TEWL, hydration, patients’ satisfaction, skin texture and homogeneity improved. No differences between the groups. | None were examined. |
| Malik et al. 2019 [65] | Low-quality randomized controlled trial (II) | SVF: Gravitational decanting -> enzymatic digestion -> centrifugation | 10 | amputation stump scars | Injection into scarred stump: 1. Fat grafting (control) 2. SVF-enriched fat graft | After 6 months, POSAS overall score (mean sum of 77 vs. 40.4 in cases and 79.2 vs. 42,4 in controls) and all its individual parameters improved over time in both groups †. Fat accumulation over stump increased in SVF-treated (mean fat area 17.9 vs. 26.8) patients †, but not in control (24.1 vs. 28.8). | None were examined. |
| Jan et al. 2019 [66] | Case series (IV) | Classic nanofat | 48 | Post-burn facial scars | Nanofat injection (subcutaneous or intradermal) | After 6 months, improvement of POSAS score in all patient-measured parameters + pigmentation and pliability, measured by observer (overall observer’s mean 7.5 ± 0.77 vs. 4.33 ± 0.48) † | None were examined. |
| Shalaby et al. 2020 [67] | Prospective cohort study (II) | Nanofat: Coleman’s procedure -> mechanical emulsification (90×) | 60 | Atrophic scars | Intradermal and subcutaneous injections of either: 1. Nanofat (control) 2. Nanofat + PRP | After 3 months—significant improvement in scar pliability, height and total VSS score (4.6 ± 1.7 vs. 2.4 ± 1.3 in nanofat + PRP; 5.2 ± 1.8 vs. 1.9 ± 1.4 in nanofat group), but no differences between the groups †. | None were examined |
| Pallua et al. 2020 [68] | Case reports (V) | Nanofat: Centrifugation -> mechanical emulsification -> cenrifugtion | 2 | Post-traumatic or post-acne facial scars | Subcutaneous microfat injection + s.c./intradermal nanofat injection ± PRP | Improvement in skin and scar quality, improved flexibility and decreased irritation. 6 months–1 year follow-up * | None were examined |
| Reference | Study Design | Strengths | Weaknesses |
|---|---|---|---|
| Wu et al., 2013 [51] | Case report | One of the first studies describing SVF use in scars Ultrasound imaging performed Innovative use of SVF | Lack of control group or statistical analysis Lack of SVF count and patient’s age |
| Carstens et al., 2015 [53] | Functional outcomes assessment Ultrasound imaging performed One of the first SVF uses in scars Adequate follow-up (24 months) | Lack of control group or statistical analysis Incomplete fat harvesting data Injection technique not specified | |
| Pallua et al., 2020 [68] | Use of condensed nanofat with increased number of ADSCs Adequate follow-up (6–12 months) | Lack of control group or statistical analysis Lack of SVF count and patients’ age | |
| Ghareeb et al., 2017 [58] | Case series | Scar assessment scale used (VSS) Sufficient statistical analysis | Lack of control group Lack of SVF count and scars’ age Scars resulting from various injuries (post-traumatic, post-burn, post-inflammatory) Heterogeneity of scars’ characteristics * |
| Carstens et al., 2017 [59] | Scar assessment scale used (VSS) Prospective design Homogenous (post-burn) scar group Multiple outcomes assessed (hardness, elasticity, range of motion) | Lack of control group Small study population (n = 5) Incomplete fat harvesting data | |
| Bhooshan et al., 2018 [60] | Scar assessment scale used (POSAS) Prospective design Sufficient statistical analysis Scar age included in the analysis (5 years cut-off) | Lack of control group Heterogeneity of scars’ characteristics* Subjective threshold for aesthetic result assessment Incomplete fat harvesting data Lack of SVF count | |
| Gu et al., 2018 [61] | Scar assessment scale used (POSAS) Homogenous (facial atrophic) scar group Prospective design Histological analysis, including various staining methods and immunohistochemistry Sufficient statistical analysis and a detailed report of used methodology | Lack of control group Scars resulting from various injuries (surgical, post-burn, traumatic) Lack of SVF count | |
| Lee et al., 2018 (1st study) [62] | Scar assessment scales used (OSAS, SBSES, VSS, VAS) Blinded outcome assessment Statistical analysis was performed | Lack of control group Heterogeneity of scars’ characteristics * Interference with additional procedures (scar revision, fat grafting etc.) No confidence interval for presented results Incomplete fat harvesting data | |
| Uyulmaz et al., 2018 [63] | Outcome assessment by three independent specialists | Lack of control group No objective clinical scores No statistical analysis | |
| Jan et al., 2019 [66] | Homogenous (post-burn facial) scar group Prospective design A significant study population (n = 48) Scar assessment scale used (POSAS) Sufficient statistical analysis and a detailed report of used methodology | Lack of control group | |
| Gentile et al., 2014 [52] | Case-control | MRI and ultrasound imaging Statistical analysis was performed Adequate follow-up (mean 60 months) Nucleated cells yield reported Novel comparison of SVF-enriched graft with PRP and normal fat grafting | Selective outcome reporting (no results of team evaluation and patient self-evaluation) No statistical analysis of baseline groups’ characteristics Incomplete fat harvesting data No information about scars’ age |
| Lee et al., 2018 (2nd study) [62] | Scar assessment scales used (OSAS, SBSES, VSS, VAS) Blinded outcome assessment Statistical analysis was performed | Heterogeneity of scars’ characteristics * Small study population (n = 15) No statistical analysis of baseline groups’ characteristics Incomplete fat harvesting data No confidence interval for presented results | |
| Zhou et al., 2016 [55] | Prospective cohort studies | Split-face study with inner control group Homogenous (facial atrophic post-acne) scar group Blinded outcome assessment by two investigators Scar assessment scale used (ECCA) Biophysical and histological analyses performed | Small study population (n = 13) P-values not reported for individual outcomes |
| Abou Eitta et al., 2019 [64] | Split-face study with inner control group Homogenous scar etiology (post-acne) SVF identification and cell count reported Blinded outcome assessment Sufficient statistical analysis Multiple clinical outcomes assessed (acne grading, skin function, scar area etc.) Comparison between SVF and FxCR | Small study population (n = 10) No information about scars’ age Ambiguous and incomplete description of injection technique | |
| Shalaby et al., 2020 [67] | Scar assessment scale used (VSS) Homogenous (atrophic facial) scar groups A significant study population (n = 60) Comparison between nanofat and nanofat + PRP Sufficient statistical analysis | Scars of various etiology Untested nanofat processing technique (90 passes between Luer-Lock syringes) Significant baseline imbalances between groups Lack of SVF count |
| Randomization Process | Deviation from the Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selective Reporting | Overall Risk of Bias | |
|---|---|---|---|---|---|---|
| Elkahky et al., 2016 [54] | ? | ? | √ | ? | ? | ? |
| Gentile et al., 2017 [56] | ? | ? | √ | × | × | × |
| Tenna et al., 2017 [57] | × | ? | √ | × | × | × |
| Malik et al., 2019 [65] | ? | ? | √ | ? | ? | ? |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stachura, A.; Paskal, W.; Pawlik, W.; Mazurek, M.J.; Jaworowski, J. The Use of Adipose-Derived Stem Cells (ADSCs) and Stromal Vascular Fraction (SVF) in Skin Scar Treatment—A Systematic Review of Clinical Studies. J. Clin. Med. 2021, 10, 3637. https://doi.org/10.3390/jcm10163637
Stachura A, Paskal W, Pawlik W, Mazurek MJ, Jaworowski J. The Use of Adipose-Derived Stem Cells (ADSCs) and Stromal Vascular Fraction (SVF) in Skin Scar Treatment—A Systematic Review of Clinical Studies. Journal of Clinical Medicine. 2021; 10(16):3637. https://doi.org/10.3390/jcm10163637
Chicago/Turabian StyleStachura, Albert, Wiktor Paskal, Weronika Pawlik, Maciej J. Mazurek, and Janusz Jaworowski. 2021. "The Use of Adipose-Derived Stem Cells (ADSCs) and Stromal Vascular Fraction (SVF) in Skin Scar Treatment—A Systematic Review of Clinical Studies" Journal of Clinical Medicine 10, no. 16: 3637. https://doi.org/10.3390/jcm10163637
APA StyleStachura, A., Paskal, W., Pawlik, W., Mazurek, M. J., & Jaworowski, J. (2021). The Use of Adipose-Derived Stem Cells (ADSCs) and Stromal Vascular Fraction (SVF) in Skin Scar Treatment—A Systematic Review of Clinical Studies. Journal of Clinical Medicine, 10(16), 3637. https://doi.org/10.3390/jcm10163637







