Prevalence and Clinical Implications of Ascites in Gastric Cancer Patients after Curative Surgery
Abstract
1. Introduction
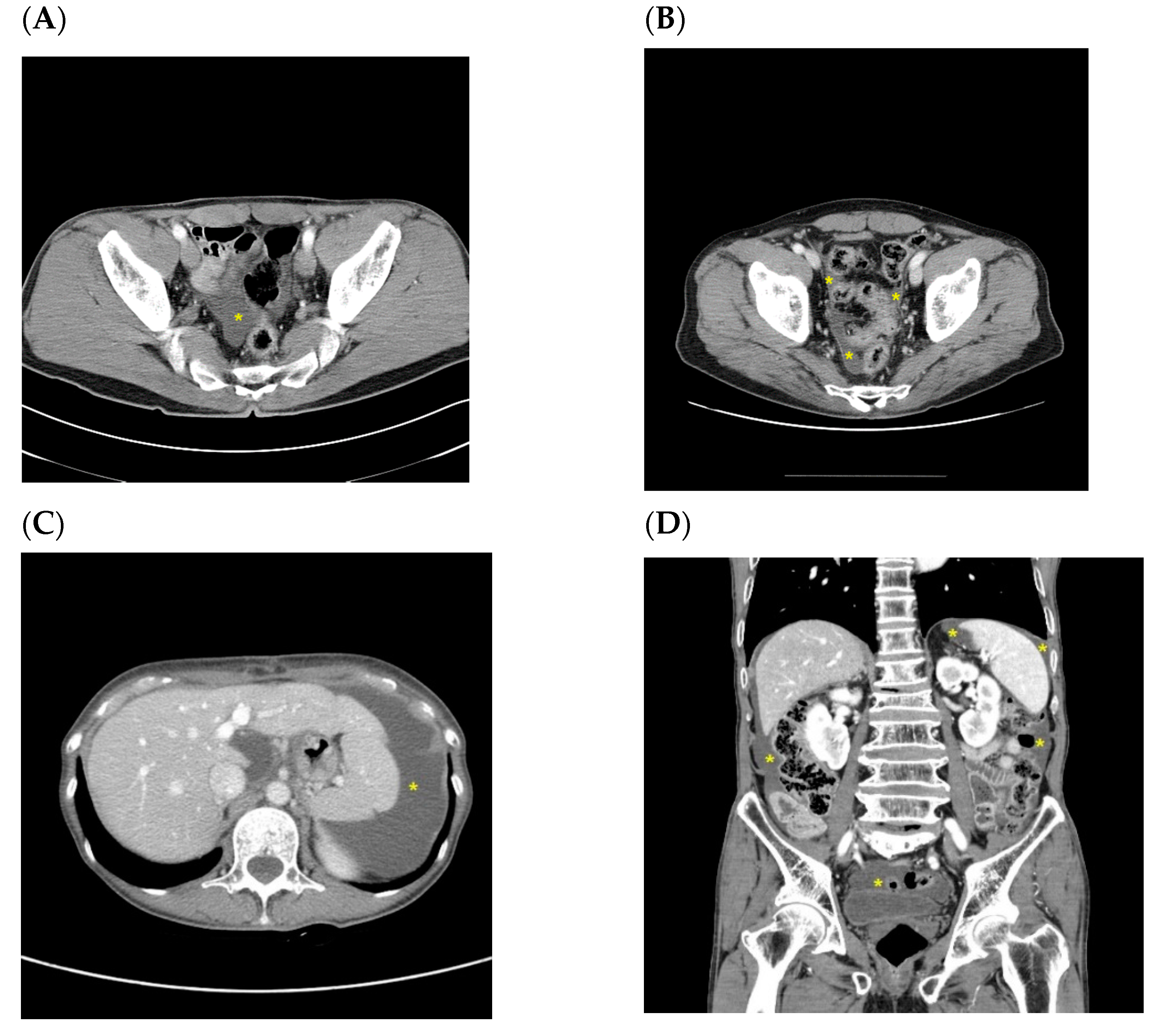
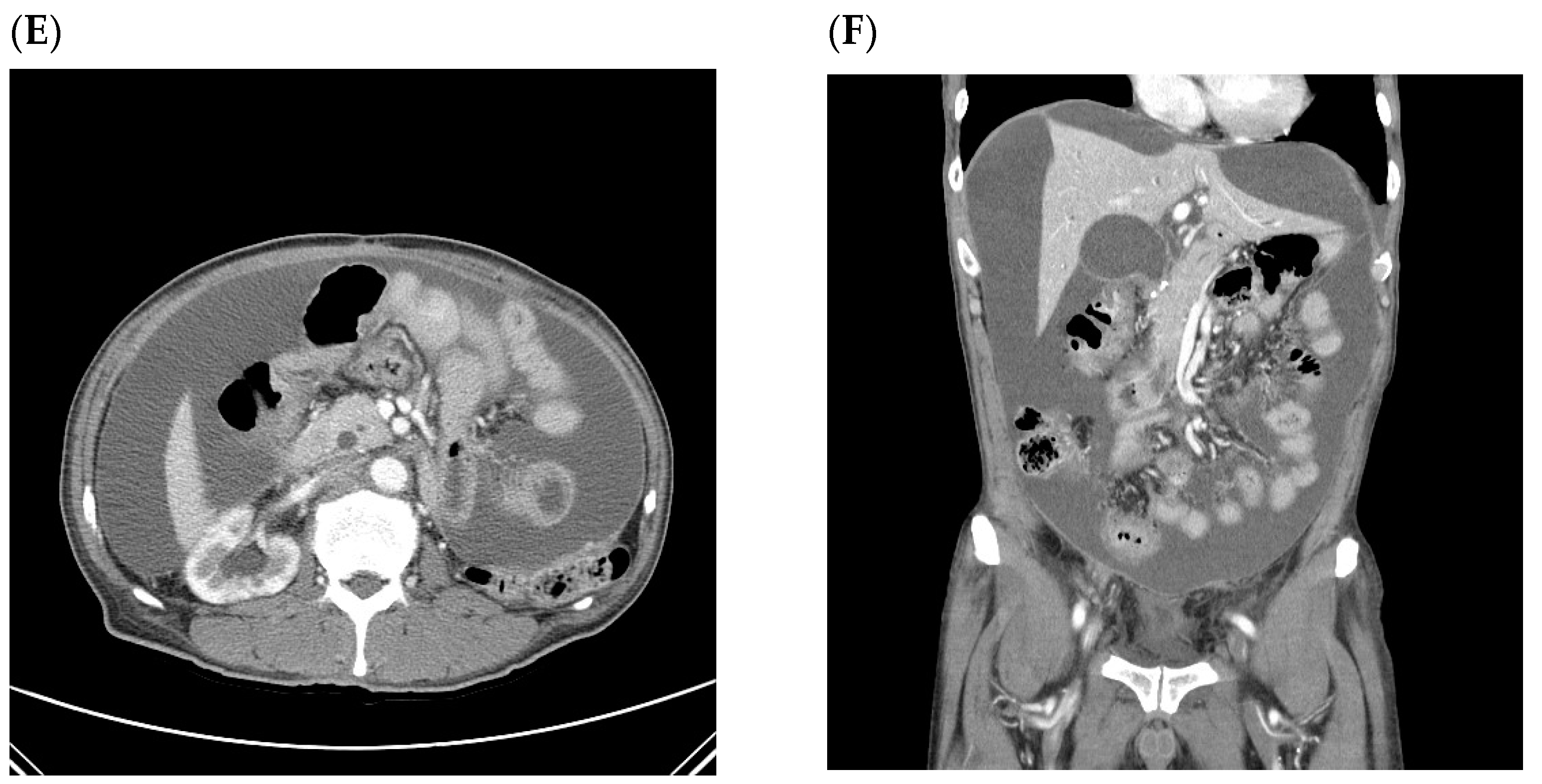
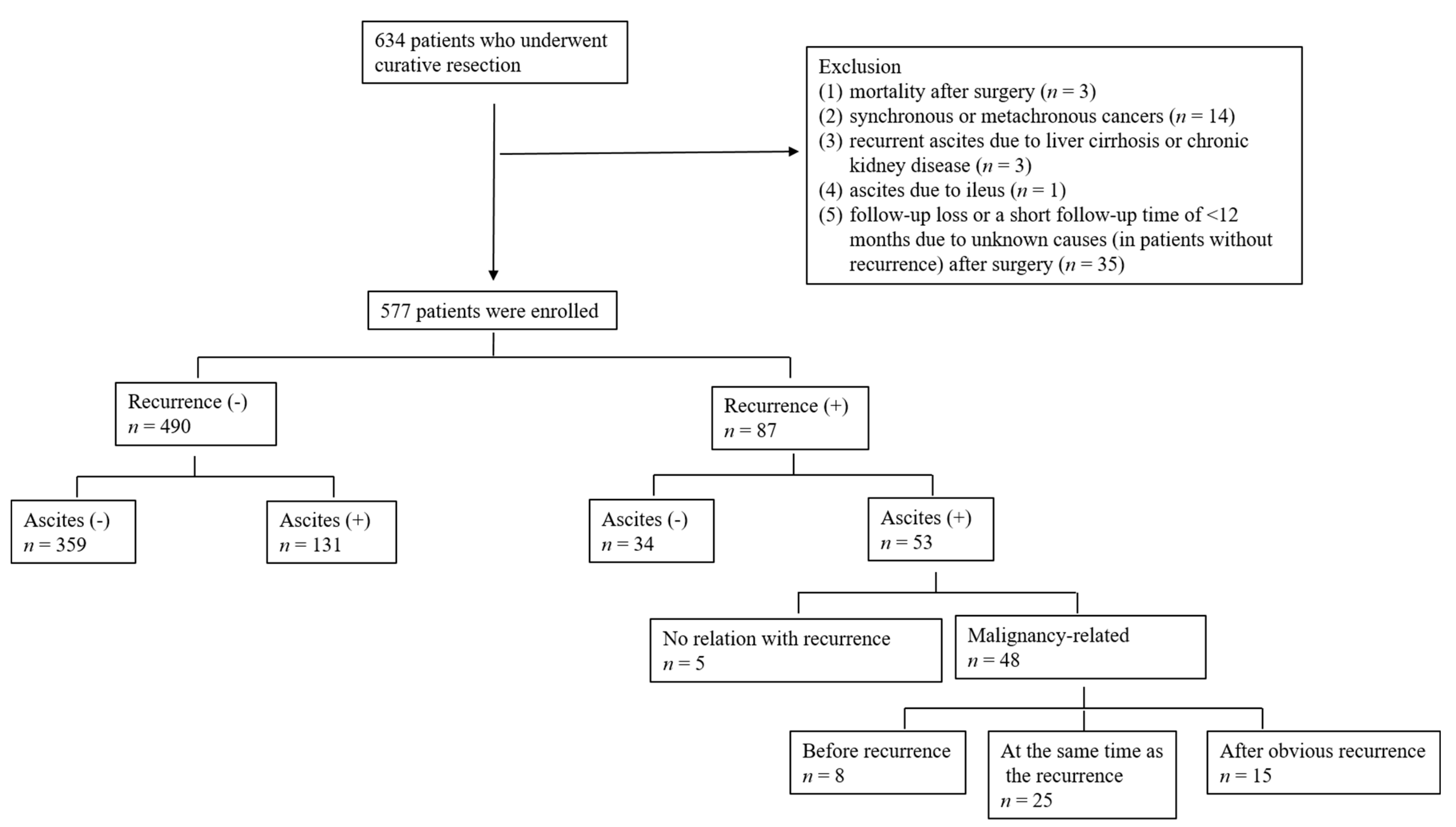
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jemal, A.; Bray, F.; Center, M.M.; Ferlay, J.; Ward, E.; Forman, D. Global cancer statistics. CA Cancer J. Clin. 2011, 61, 69–90. [Google Scholar] [CrossRef]
- Kim, C.D.; Chang, M.C.; Roh, H.R.; Chae, G.B.; Yang, D.H.; Choi, W.J. Factors influencing recurrence after curative resection for advanced gastric cancer. J. Korean Surg. Soc. 2003, 65, 301–308. [Google Scholar]
- Yoo, C.H.; Noh, S.H.; Shin, D.W.; Choi, S.H.; Min, J.S. Recurrence following curative resection for gastric carcinoma. Br. J. Surg. 2000, 87, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.Z.; Lang, N.P.; Thompson, C.; Osteen, P.K.; Westbrook, K.C. Peritoneal carcinomatosis in nongynecologic malignancy. A prospective study of prognostic factors. Cancer 1989, 63, 364–367. [Google Scholar]
- Sadeghi, B.; Arvieux, C.; Glehen, O.; Beaujard, A.C.; Rivoire, M.; Baulieux, J.; Fontaumard, E.; Brachet, A.; Caillot, J.L.; Faure, J.L.; et al. Peritoneal carcinomatosis from non-gynecologic malignancies: Results of the EVOCAPE 1 multicentric prospective study. Cancer 2000, 88, 358–363. [Google Scholar] [CrossRef]
- Raptopoulos, V.; Gourtsoyiannis, N. Peritoneal carcinomatosis. Eur. Radiol. 2001, 11, 2195–2206. [Google Scholar] [CrossRef]
- Kim, S.J.; Kim, H.H.; Kim, Y.H.; Hwang, S.H.; Lee, H.S.; Park, D.J.; Kim, S.Y.; Lee, K.H. Peritoneal metastasis: Detection with 16-or 64-detector row CT in patients undergoing surgery for gastric cancer. Radiology 2009, 253, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Friedman, A.C.; Sohotra, P.; Radecki, P.D. CT manifestations of peritoneal carcinomatosis. Am. J. Roentgenol. 1988, 150, 1035–1041. [Google Scholar]
- Lee, H.J.; Kim, M.J.; Lim, J.S.; Kim, K.W. Follow up CT findings of various types of recurrence after curative gastric surgery. J. Korean Radiol. Soc. 2007, 57, 553–562. [Google Scholar] [CrossRef][Green Version]
- Bennett, J.J.; Gonen, M.; D’Angelica, M.; Jaques, D.P.; Brennan, M.F.; Coit, D.G. Is detection of asymptomatic recurrence after curative resection associated with improved survival in patients with gastric cancer? J. Am. Coll Surg. 2005, 201, 503–510. [Google Scholar] [CrossRef]
- Kim, J.H.; Jang, Y.J.; Park, S.S.; Park, S.H.; Mok, Y.J. Benefit of post-operative surveillance for recurrence after curative resection for gastric cancer. J. Gastrointest. Surg. 2010, 14, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Lim, J.K.; Kim, M.G.; Kwon, S.J. The influence of post-operative surveillance on the prognosis after curative surgery for gastric cancer. Hepatogastroenterology 2014, 61, 2123–2132. [Google Scholar] [PubMed]
- Kim, S.H.; Choi, Y.H.; Kim, J.W.; Oh, S.; Lee, S.; Kim, B.G.; Lee, K.L. Clinical significance of computed tomography-detected ascites in gastric cancer patients with peritoneal metastases. Medicine 2018, 97, e9343. [Google Scholar] [CrossRef] [PubMed]
- Yajima, K.; Kanda, T.; Ohashi, M.; Wakai, T.; Nakagawa, S.; Sasamoto, R.; Hatakeyama, K. Clinical and diagnostic significance of preoperative computed tomography findings of ascites in patients with advanced gastric cancer. Am. J. Surg. 2006, 192, 185–190. [Google Scholar] [CrossRef]
- Chang, D.K.; Kim, J.W.; Kim, B.K.; Lee, K.L.; Song, C.S.; Han, J.K.; Song, I.S. Clinical significance of CT-defined minimal ascites in patients with gastric cancer. World J. Gastroenterol. 2005, 11, 6587–6592. [Google Scholar] [CrossRef]
- Healy, J.C.; Reznek, R.H. The peritoneum, mesenteries and omenta: Normal anatomy and pathological processes. Eur. Radiol. 1998, 8, 886–900. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, T.; Hayashi, N.; Maeda, E.; Matsuda, I.; Sasaki, H.; Ohtsu, H.; Ohtomo, K. Peritoneal fluid accumulation in healthy men and postmenopausal women: Evaluation on pelvic MRI. Am. J. Roentgenol. 2013, 200, 1181–1185. [Google Scholar] [CrossRef]
- Koninckx, P.R.; Renaer, M.; Brosens, I.A. Origin of peritoneal fluid in women: An ovarian exudation product. Br. J. Obstet. Gynaecol. 1980, 87, 177–183. [Google Scholar] [CrossRef]
- Verger, C.; Luger, A.; Moore, H.L.; Nolph, K.D. Acute changes in peritoneal morphology and transport properties with infectious peritonitis and mechanical injury. Kidney Int. 1983, 23, 823–831. [Google Scholar] [CrossRef]
- Cheon, H.J.; Ryeom, H.K.; Bae, J.H.; Jang, Y.J.; Kim, G.C.; Kim, J.H.; Shin, K.M.; Chung, H.Y. Clinical significance of a small amount of isolated pelvic free fluid at multidetector CT in male patients after curative surgery for gastric carcinoma. J. Korean Soc. Radiol. 2014, 71, 69–74. [Google Scholar] [CrossRef]
- Hwangbo, Y.; Jung, J.H.; Shim, J.; Kim, B.H.; Jung, S.H.; Lee, C.K.; Jang, J.Y.; Dong, S.H.; Kim, H.J.; Chang, Y.W.; et al. Etiologic and laboratory analyses of ascites in patients who underwent diagnostic paracentesis. Korean J. Hepatol. 2007, 13, 185–195. [Google Scholar] [PubMed]
- Runyon, B.A. Management of adult patients with ascites caused by cirrhosis. Hepatology 1998, 27, 264. [Google Scholar] [CrossRef]
- Sangisetty, S.L.; Miner, T.J. Malignant ascites: A review of prognostic factors, pathophysiology and therapeutic measures. World J. Gastrointest. Surg. 2012, 4, 87–95. [Google Scholar] [CrossRef]
- Press, O.W.; Press, N.O.; Kaufman, S.D. Evaluation and management of chylous ascites. Ann. Intern. Med. 1982, 96, 358. [Google Scholar] [CrossRef] [PubMed]
- Duarte, I.; Outerelo, C. Gastric cancer presenting as isolated ascites: A diagnostic challenge. Eur. J. Case Rep. Intern. Med. 2019, 6, 001141. [Google Scholar] [PubMed]
- Maeda, H.; Kobayashi, M.; Sakamoto, J. Evaluation and treatment of malignant ascites secondary to gastric cancer. World J. Gastroenterol. 2015, 21, 10936–10947. [Google Scholar] [CrossRef]
- Kim, K.W.; Choi, B.I.; Han, J.K.; Kim, T.K.; Kim, A.Y.; Lee, H.J.; Kim, Y.H.; Choi, J.; Do, K.; Kim, H.C.; et al. Postoperative anatomic and pathologic findings at CT following gastrectomy. Radiographics 2002, 22, 323–336. [Google Scholar] [CrossRef] [PubMed]
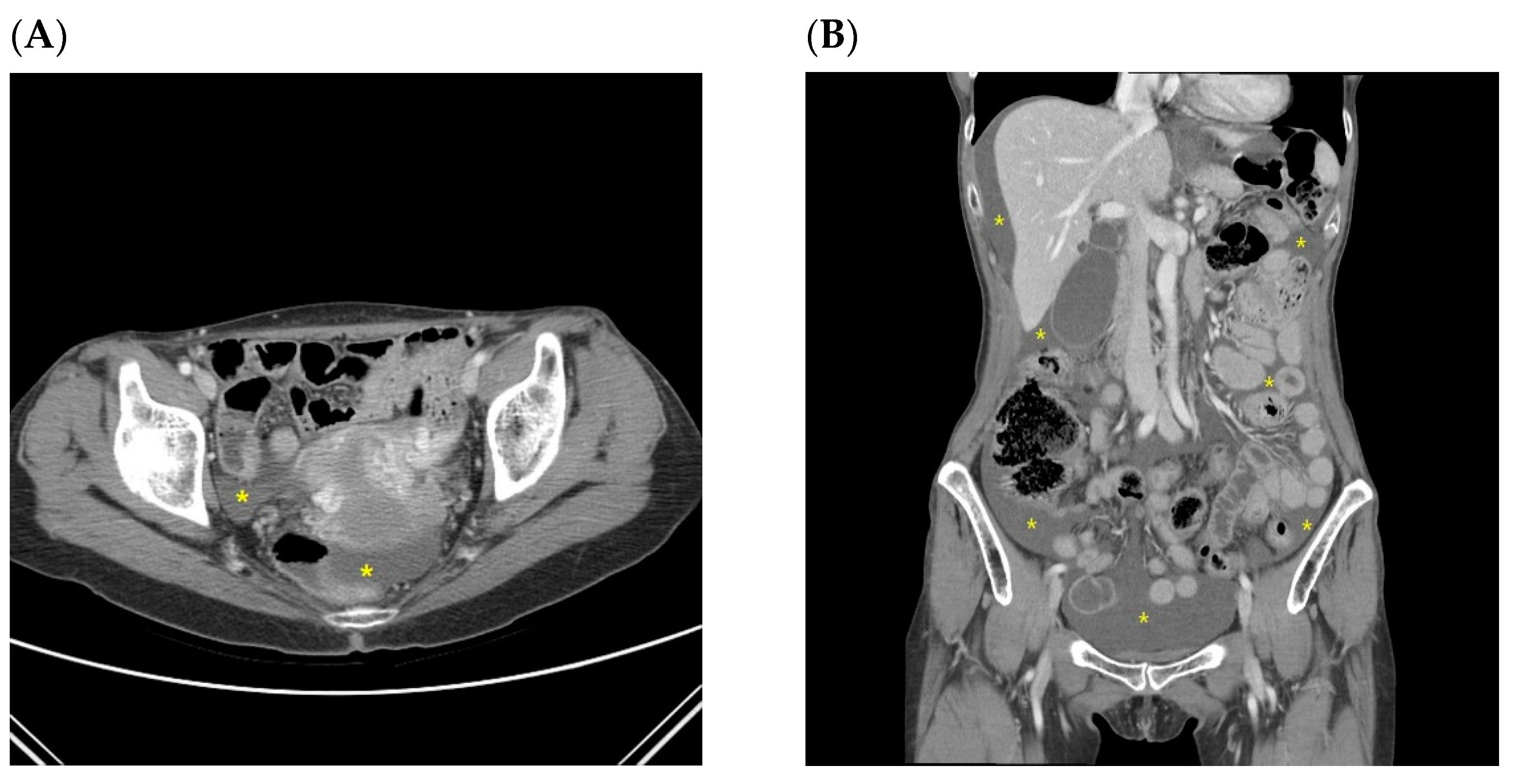
| Ascites without Recurrence | Ascites with Recurrence | p | |
|---|---|---|---|
| n (%) | n (%) | ||
| Sex | 0.869 | ||
| Male | 78 (60.3) | 31 (58.5) | |
| Female | 53 (39.7) | 22 (41.5) | |
| Age (years ± SD) | 55.9 ± 12.3 | 60.0 ± 12.1 | 0.046 |
| Type of resection | <0.001 | ||
| Partial gastrectomy | 105 (80.2) | 26 (49.1) | |
| Total gastrectomy | 26 (19.8) | 27 (50.9) | |
| Surgical approach | <0.001 | ||
| Open | 89 (67.9) | 52 (98.1) | |
| Laparoscopy | 42 (32.1) | 1 (1.9) | |
| pT stage | <0.001 | ||
| T1 | 80 (61.1) | 4 (7.5) | |
| T2 | 12 (9.2) | 4 (7.5) | |
| T3 | 18 (13.7) | 24 (45.3) | |
| T4 | 21 (16.0) | 21 (39.6) | |
| pN stage | <0.001 | ||
| N0 | 80 (61.1) | 8 (15.1) | |
| N1 | 23 (17.6) | 5 (9.4) | |
| N2 | 19 (14.5) | 7 (13.2) | |
| N3 | 9 (6.9) | 33 (62.3) | |
| Nutritional parameters | |||
| Albumin (g/dL ± SD) | 4.2 ± 0.4 | 4.0 ± 0.6 | <0.001 |
| Hemoglobin (g/dL ± SD) | 12.3 ± 1.4 | 11.4 ± 1.4 | <0.001 |
| Adjuvant chemotherapy | <0.001 | ||
| No | 80 (61.1) | 8 (15.1) | |
| Yes | 51 (38.9) | 45 (84.9) | |
| Location of ascites at first appearance | <0.001 | ||
| Pelvic cavity only | 128 (97.7) | 29 (54.7) | |
| Whole abdomen | 0 (0) | 16 (30.2) | |
| Other | 3 (2.3) | 8 (15.1) | |
| Volume of ascites at first appearance | <0.001 | ||
| Small | 130 (99.2) | 38 (71.7) | |
| Moderate | 1 (0.8) | 10 (18.9) | |
| Large | 0 (0) | 5 (9.4) | |
| Repeatability † | |||
| No | 52 (39.7) | ||
| Yes | 79 (60.3) | ||
| Timing of first appearance (months after surgery) | 9.0 (range of 3.0–108.0) | 11.5 (range of 3.0–71.0) |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Ascites (−), n (%) | Ascites (+), n (%) | p-Value | Hazard Ratio | 95% CI | p-Value | |
| Sex | 0.065 | |||||
| Male | 249 (75.9) | 79 (24.1) | 1 | |||
| Female | 110 (67.9) | 52 (32.1) | 1.436 | 0.926–2.227 | 0.106 | |
| Age (years) | <0.001 | |||||
| ≤45 | 9 (32.1) | 19 (67.9) | 6.465 | 2.803–14.915 | <0.001 | |
| >45 | 350 (75.8) | 112 (24.2) | 1 | |||
| Type of surgery | 0.211 | |||||
| Total gastrectomy | 306 (74.5) | 105 (25.5) | ||||
| Partial gastrectomy | 53 (67.1) | 26 (32.9) | ||||
| Surgical approach | 0.581 | |||||
| Open | 252 (74.0) | 89 (26.0) | ||||
| Laparoscopy | 106 (71.6) | 42 (28.4) | ||||
| Depth of invasion | 0.054 | |||||
| pT1–2 | 283 (75.5) | 92 (24.5) | 1 | |||
| pT3–4 | 76 (66.1) | 39 (33.9) | 0.889 | 0.435–1.819 | 0.748 | |
| Lymph node metastasis | ||||||
| pN0–1 | 310 (75.1) | 103 (24.9) | 0.049 | 1 | ||
| pN2–3 | 49 (63.6) | 28 (36.4) | 1.088 | 0.553–2.140 | 0.806 | |
| Adjuvant chemotherapy | 0.003 | |||||
| No | 268 (77) | 80 (23.0) | 1 | |||
| Yes | 91 (64.1) | 51 (35.9) | 2.098 | 0.985–4.470 | 0.055 | |
| Age/Sex | Type of Operation | TN Stage | Characteristic of Ascites | Timing of Malignant Ascites | Site of First Recurrence | Interval between Surgery and Recurrence (Month) | Interval between First Appearance of Benign Ascites and Recurrence (Month) | |
|---|---|---|---|---|---|---|---|---|
| Patients with ascites presumed to be benign before confirmation of recurrence (n = 8) | ||||||||
| Pt 1 | 65/M | PG | T3N3a | small pelvic cavity | Simultaneous with recurrence | T colon (increased ascites in the pelvic cavity) | 44.4 | 8.1 |
| Pt 2 | 53/F | TG | T4bN3b | small pelvic cavity | Simultaneous with recurrence | Peritoneum (increased ascites, peritoneal thickening, bowel obstruction, and Krukenberg tumors) | 18.2 | 13.2 |
| Pt 3 | 40/F | TG | T4aN3a | small pelvic cavity | Simultaneous with recurrence | Peritoneum (nodularity and increased ascites) | 73.2 | 70.3 |
| Pt 4 | 59/F | TG | T4aN3a | small pelvic cavity | Simultaneous with recurrence | Peritoneum (increased ascites and peritoneal thickening) | 25.2 | 21.7 |
| Pt 5 | 39/F | TG | T3N3b | small pelvic cavity | Simultaneous with recurrence | Peritoneum (Krukenberg tumors, nodularity, and increased ascites) | 12.1 | 9 |
| Pt 6 | 57/F | TG | T3N3a | small pelvic cavity | Simultaneous with recurrence | Peritoneum (bowel obstruction and increased ascites) | 9.8 | 4.4 |
| Pt 7 | 61/F | TG | T3N1 | small pelvic cavity | Simultaneous with recurrence | Peritoneum (increased ascites, T colon, and mesentery LNs) | 29.6 | 26 |
| Pt 8 | 68/F | PG | T4aN2 | small pelvic cavity | Simultaneous with recurrence | Peritoneum (increased ascites and peritoneal thickening) | 11.7 | 5.3 |
| A patient who first recurred with malignant ascites without other CT findings related to peritoneal seeding (later confirmed by cytology) (n = 1) | ||||||||
| Pt 9 | 49/F | TG | T3N3a | small pelvic cavity | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-H.; Kwon, S.-J.; Kim, M.; Kang, B.-K. Prevalence and Clinical Implications of Ascites in Gastric Cancer Patients after Curative Surgery. J. Clin. Med. 2021, 10, 3557. https://doi.org/10.3390/jcm10163557
Lee J-H, Kwon S-J, Kim M, Kang B-K. Prevalence and Clinical Implications of Ascites in Gastric Cancer Patients after Curative Surgery. Journal of Clinical Medicine. 2021; 10(16):3557. https://doi.org/10.3390/jcm10163557
Chicago/Turabian StyleLee, Ju-Hee, Sung-Joon Kwon, Mimi Kim, and Bo-Kyeong Kang. 2021. "Prevalence and Clinical Implications of Ascites in Gastric Cancer Patients after Curative Surgery" Journal of Clinical Medicine 10, no. 16: 3557. https://doi.org/10.3390/jcm10163557
APA StyleLee, J.-H., Kwon, S.-J., Kim, M., & Kang, B.-K. (2021). Prevalence and Clinical Implications of Ascites in Gastric Cancer Patients after Curative Surgery. Journal of Clinical Medicine, 10(16), 3557. https://doi.org/10.3390/jcm10163557






