Preparedness of Health Care Workers and Medical Students in University Hospital in Krakow for COVID-19 Pandemic within the CRACoV Project
Abstract
:1. Introduction
2. Methods and Materials
2.1. Study Design
2.2. Setting
2.3. Study Participants
- medical doctors
- fifth-year medical students
- nurses/midwives and paramedics
- other HCWs (health care assistant, radiology technician, physiotherapist/rehabilitation specialist, dietician, psychologist, social worker, volunteer, cleaning person, diagnostic laboratory technician, registration/patient information desk worker)
- administrative staff
2.4. Methods
- (1)
- socio-demographic characteristics (age, gender, education, profession, and work experience)
- (2)
- hospital staff involvement in the training (participation in general training on the prevention and infections control (IPC); participation in the specific training in the care COVID-19 patients; duration of training on the standard precaution; the form of training in the use of PPE; self-evaluation of the respondent’s preparedness to protect themselves and other staff or patients against infection)
- (3)
- knowledge about the recommended guidance for hand hygiene in healthcare [13]
- (4)
- adherence to IPC measures (whether the respondent is able to properly apply hand hygiene, standard precaution, properly uses PPE)
2.5. Knowledge and Performance Index
- “Do you know the recommended guidance for hand hygiene in health care?” [13]
- “Do you follow IPC standard precautions when in contact with any patient?”
- “Do you wear PPE when indicated (i.e., surgical masks, goggles/face shields, aprons, coveralls, caps)?”
2.6. Statistical Analysis
Sample Size
2.7. Ethics Approval and Consent to Participate
3. Results
3.1. Descriptive Characteristics of Study Population
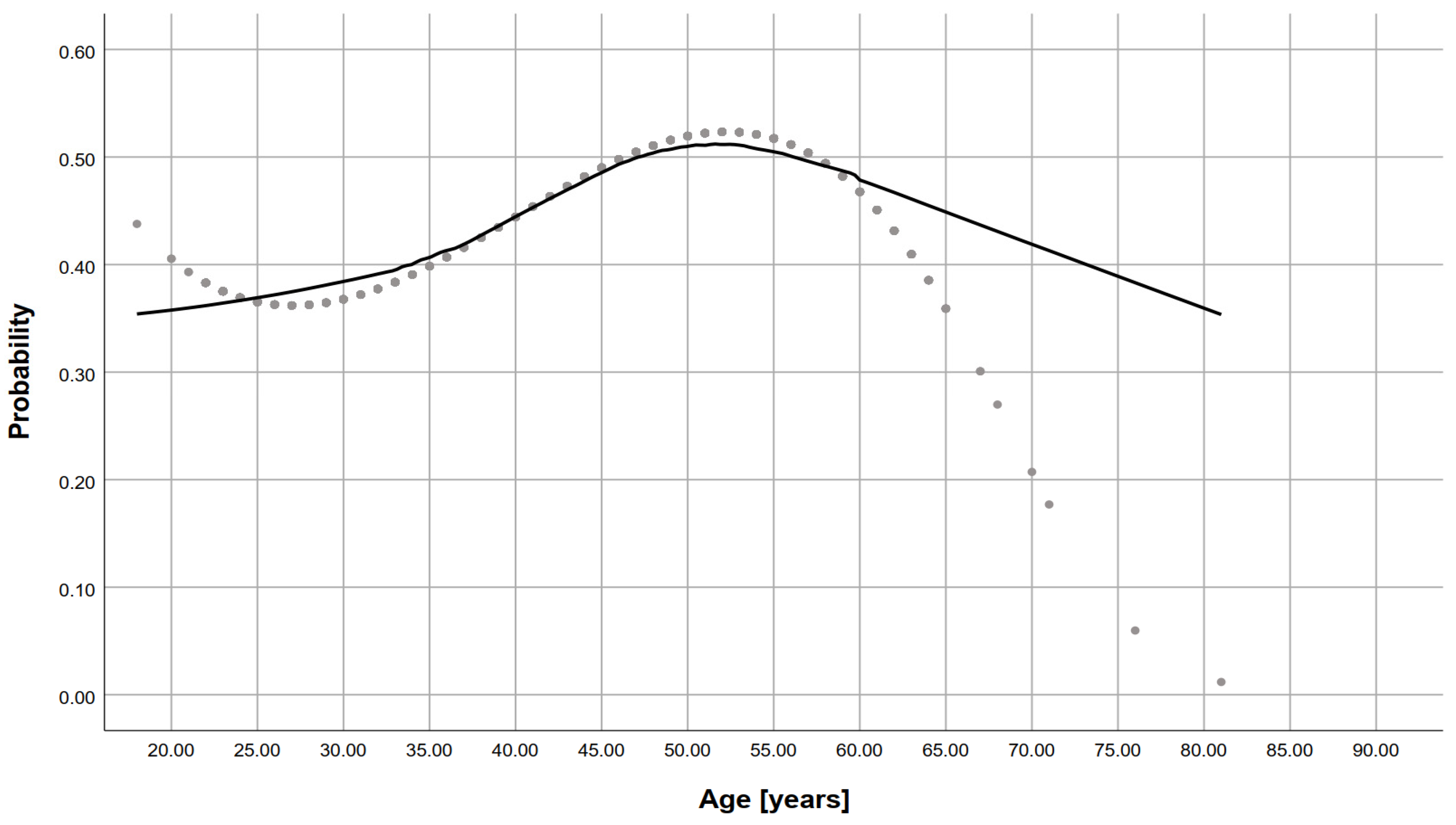
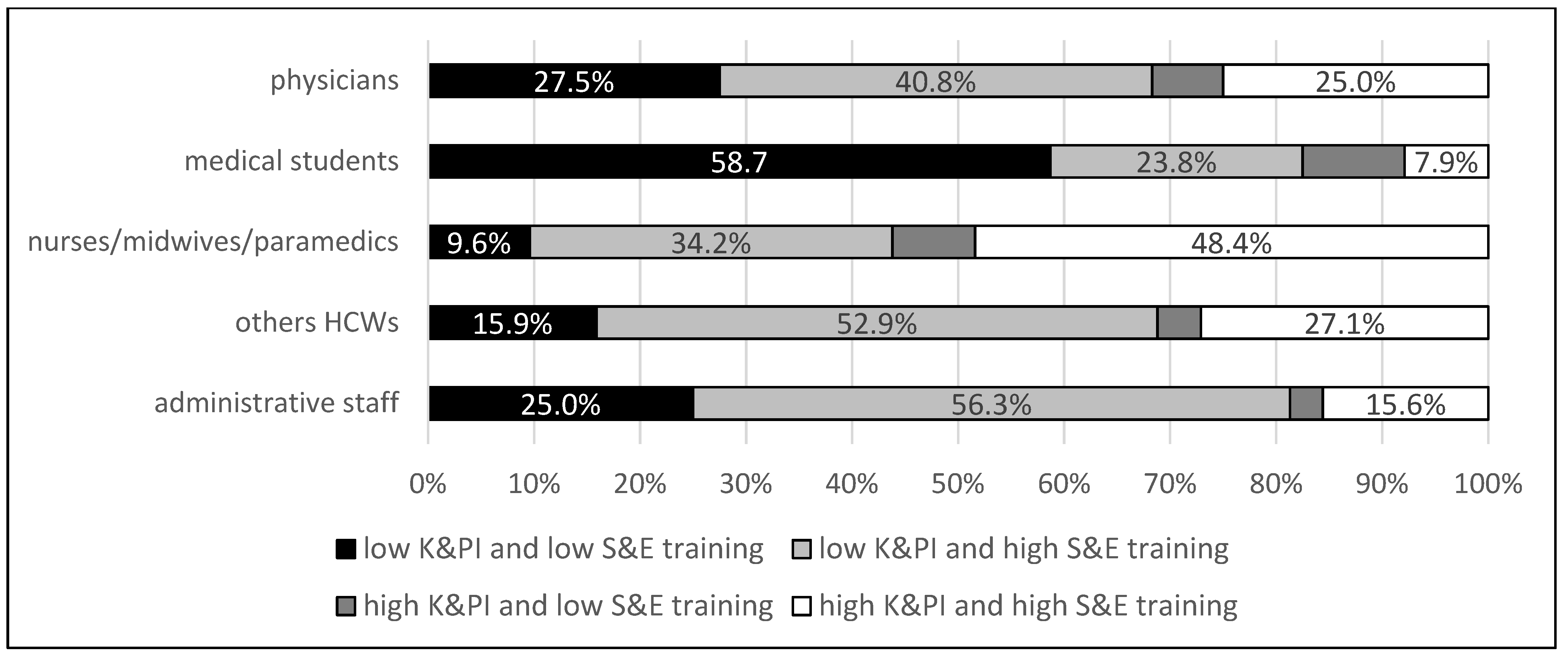
3.2. Knowledge and Performance Index
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Rapid Hospital Readiness Checklist for COVID-19. License: CC BY-NC-SA 3.0 IGO. 2020. Available online: https://apps.who.int/iris/handle/10665/332778 (accessed on 6 April 2021).
- Lietz, J.; Westermann, C.; Nienhaus, A.; Schablon, A. The Occupational Risk of Influenza A (H1N1) Infection among Healthcare Personnel during the 2009 Pandemic: A Systematic Review and Meta-Analysis of Observational Studies. PLoS ONE 2016, 11, e0162061. [Google Scholar] [CrossRef]
- Kilmarx, P.H.; Clarke, K.R.; Dietz, P.M.; Hamel, M.J.; Husain, F.; McFadden, J.D.; Park, B.J.; Sugerman, D.E.; Bresee, J.S.; Mermin, J.; et al. Ebola Virus Disease in Health Care Workers—Sierra Leone. 2014. Available online: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6349a6.htm (accessed on 6 April 2021).
- Xiao, J.; Fang, M.; Chen, Q.; He, B. SARS, MERS and COVID-19 among healthcare workers: A narrative review. J. Infect. Public Health 2020, 13, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.H.; et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Jacob, J.T.; Baker, J.M.; Fridkin, S.K.; Lopman, B.A.; Steinberg, J.P.; Christenson, R.H.; King, B.; Leekha, S.; O’Hara, L.M.; Rock, P.; et al. Risk Factors Associated With SARS-CoV-2 Seropositivity Among US Health Care Personnel. JAMA Netw. Open 2021, 4, e211283. [Google Scholar] [CrossRef] [PubMed]
- Naranbhai, V.; Chang, C.C.; Beltran, W.F.G.; Miller, T.E.; Astudillo, M.G.; Villalba, J.A.; Yang, D.; Gelfand, J.; Bernstein, B.E.; Feldman, J.; et al. High Seroprevalence of Anti-SARS-CoV-2 Antibodies in Chelsea, Massachusetts. J. Infect. Dis. 2020, 222, 1955–1959. [Google Scholar] [CrossRef]
- Baker, J.M.; Nelson, K.N.; Overton, E.; Lopman, B.A.; Lash, T.L.; Photakis, M.; Jacob, J.T.; Roback, J.; Fridkin, S.K.; Steinberg, J.P. Quantification of occupational and community risk factors for SARS-CoV-2 seroposi-tivity among healthcare workers in a large U.S. healthcare system. medRxiv 2020. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control: Infection Prevention and Control and Preparedness for COVID-19 in Healthcare Settings—Sixth Update. 9 February 2021. ECDC: Stockholm, Sweden, 2021. Available online: https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings (accessed on 6 April 2021).
- European Centre for Disease Prevention and Control: Historical Data on the Daily Number of New Reported COVID-19 Cases and Deaths Worldwide—Last Update 14 December 2020. 2020. Available online: https://www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide (accessed on 6 April 2021).
- PAP SA: The PAP Register. [In Polish]. 2021. Available online: https://www.pap.pl/aktualnosci/news%2C808786%2Cilu-lekarzy-zmarlo-z-powodu-koronawirusa-ministerstwo-zdrowia-podalo-dane (accessed on 6 April 2021).
- World Health Organization. Assessment of Risk Factors for Coronavirus Disease 2019 (COVID-19) in Health Workers: Protocol for a Case-Control Study, 26 May 2020, Version 1.0. World Health Organization License: CC BY-NC-SA 3.0 IGO. , 2020. Available online: https://apps.who.int/iris/handle/10665/332187 (accessed on 6 April 2021).
- World Health Organization. Hand hygiene: Why, How & When? World Health Organization: Geneva, Switzerland, 2009. Available online: https://www.who.int/gpsc/5may/Hand_Hygiene_Why_How_and_When_Brochure.pdf (accessed on 6 April 2021).
- Al Qadire, M.; Hani, A.M. Nurses and physicians knowledge of guidelines for preventing catheter-related blood stream infections. Nurs. Crit. Care 2020. [Google Scholar] [CrossRef]
- Chang, N.N.; Reisinger, H.S.; Schweizer, M.L.; Jones, I.; Chrischilles, E.; Chorazy, M.; Huskins, C.; Herwaldt, L. Hand Hygiene Compliance at Critical Points of Care. Clin. Infect. Dis. 2021, 72, 814–820. [Google Scholar] [CrossRef]
- Wałaszek, M.; Kołpa, M.; Wolak, Z.; Różańska, A.; Wójkowska-Mach, J. Poor Hand Hygiene Procedure Compliance among Polish Medical Students and Physicians—The Result of an Ineffective Education Basis or the Impact of Organizational Culture? Int. J. Environ. Res. Public Health 2017, 14, 1026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wałaszek, M.; Kołpa, M.; Różańska, A.; Jagiencarz-Starzec, B.; Wolak, Z. Hospital knowledge and practice of doctors and nurses regarding hand hygiene in a survey. Epidemiol. Rev. 2020, 74, 119–132. [Google Scholar]
- Zafar, N.; Jamal, Z.; Khan, M.M. Preparedness of the Healthcare Personnel against the Coronavirus Disease 2019 (COVID-19) Outbreak: An Audit Cycle. Front. Public Health 2020, 8, 502. [Google Scholar] [CrossRef]
- Różańska, A.; Wójkowska-Mach, J.; Bulanda, M. Work experience and seniority in health care vs. medical students’ knowledge of selected hand hygiene procedures. Med. Pr. 2016, 67, 623–633. (In Polish) [Google Scholar] [CrossRef] [Green Version]
- Norton, E.J.; Georgiou, I.; Fung, A.; Nazari, A.; Bandyopadhyay, S.; Saunders, K.E.A. Personal protective equipment and infection prevention and control: A national survey of UK medical students and interim foundation doctors during the COVID-19 pandemic. J. Public Health 2021, 43, 67–75. [Google Scholar] [CrossRef]
- NYS Department of Health: Key Infection Control Practices in Inpatient and Outpatient Medica Care Settings. 2008. Available online: https://www.health.ny.gov/professionals/diseases/reporting/communicable/infection/key_infection_control_practices.htm (accessed on 6 April 2021).
- Chou, R.; Dana, T.; Buckley, D.I.; Selph, S.; Fu, R.; Totten, A.M. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers. Ann. Intern. Med. 2020, 173, 120–136. [Google Scholar] [CrossRef]
- Lai, X.; Wang, X.; Yang, Q.; Xu, X.; Tang, Y.; Liu, C.; Tan, L.; Lai, R.; Wang, H.; Zhang, X.; et al. Will healthcare workers improve infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob. Resist. Infect. Control 2020, 9, 83. [Google Scholar] [CrossRef]
- Fung, M.F.-C.C. Overcoming complacency in the face of infectious disease. Nat. Med. 2021, 27, 363. [Google Scholar] [CrossRef] [PubMed]
- O’Byrne, L.; Gavin, B.; McNicholas, F. Medical students and COVID-19: The need for pandemic preparedness. J. Med. Ethics 2020, 46, 623–626. [Google Scholar] [CrossRef] [PubMed]
- John, A.; Tomas, M.E.; Hari, A.; Wilson, B.M.; Donskey, C.J. Do medical students receive training in correct use of personal protective equipment? Med Educ. Online 2017, 22, 1264125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashcroft, J.; Byrne, M.H.V.; Brennan, P.A.; Davies, R.J. Preparing medical students for a pandemic: A systematic review of student disaster training programmes. Postgrad. Med. J. 2020, 97, 368–379. [Google Scholar] [CrossRef]
- Khasawneh, A.I.; Abu Humeidan, A.; Alsulaiman, J.W.; Bloukh, S.; Ramadan, M.; Al-Shatanawi, T.N.; Awad, H.H.; Hijazi, W.Y.; Al-Kammash, K.R.; Obeidat, N.; et al. Medical Students and COVID-19: Knowledge, Attitudes, and Precautionary Measures. A Descriptive Study from Jordan. Front. Public Health 2020, 8, 253. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, J.H.; Rajamaki, B.; Ijaz, S.; Sauni, R.; Toomey, E.; Blackwood, B.; Tikka, C.; Ruotsalainen, J.H.; Balci, F.S.K. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst. Rev. 2020, 2020, CD011621. [Google Scholar] [CrossRef]
- Byrnes, Y.M.; Civantos, A.M.; Go, B.C.; McWilliams, T.L.; Rajasekaran, K. Effect of the COVID-19 pandemic on medical student career perceptions: A national survey study. Med. Educ. Online 2020, 25, 1798088. [Google Scholar] [CrossRef] [PubMed]
- O’Doherty, D.; Dromey, M.; Lougheed, J.; Hannigan, A.; Last, J.; McGrath, D. Barriers and solutions to online learning in medical education—An integrative review. BMC Med. Educ. 2018, 18, 130. [Google Scholar] [CrossRef] [Green Version]
- Rosiński, J.; Różańska, A.; Jarynowski, A.; Wójkowska-Mach, J.; Polish Society of Hospital Infections Team. Factors Shaping Attitudes of Medical Staff towards Acceptance of the Standard Precautions. Int. J. Environ. Res. Public Health 2019, 16, 1050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaur, R.; Razee, H.; Seale, H. Facilitators and barriers around teaching concepts of hand hygiene to undergraduate medical students. J. Hosp. Infect. 2014, 88, 28–33. [Google Scholar] [CrossRef]
- Polacco, M.A.; Shinkunas, L.; Perencevich, E.N.; Kaldjian, L.; Reisinger, H.S. See one, do one, teach one: Hand hygiene attitudes among medical students, interns, and faculty. Am. J. Infect. Control 2015, 43, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Abulebda, K.; Ahmed, R.A.; Auerbach, M.A.; Bona, A.M.; Falvo, L.E.; Hughes, P.G.; Gross, I.T.; Sarmiento, E.J.; Barach, P.R. National preparedness survey of pediatric intensive care units with simulation centers during the coronavirus pandemic. World J. Crit. Care Med. 2020, 9, 74–87. [Google Scholar] [CrossRef] [PubMed]
- Mahrosh, H.S.; Mustafa, G. The COVID-19 puzzle: A global nightmare. Environ. Dev. Sustain. 2021, 23, 12710–12737. [Google Scholar] [CrossRef]
| Characteristics of the Study Group/Profession | Total N = 1412 | Physicians N = 124 | Medical Students N = 129 | Nurses/Midwives and Paramedics N = 757 | Other Health Care Workers N = 233 | Administrative Staff N = 169 | p Value * |
|---|---|---|---|---|---|---|---|
| Sex, n (%) | |||||||
| Female | 1241 (87.9) | 87 (70.2) | 82 (63.6) | 734 (97.0) | 208 (89.3) | 130 (76.9) | <0.0001 |
| Age, n (%) | |||||||
| 18–36 | 524 (38.4) | 73 (58.9) | 129 (100.0) | 223 (29.5) | 72 (30.9) | 45 (26.6) | <0.0001 |
| 37–55 | 655 (46.4) | 40 (32.3) | 0 (0.0) | 402 (53.1) | 113 (48.5) | 100 (59.2) | |
| 56 or older | 215 (15.2) | 11 (8.9) | 0 (0.0) | 132 (17.4) | 48 (20.6) | 24 (14.2) | |
| Work experience, n (%) | |||||||
| Less than 12 months | 126 (8.9) | 5 (4.0) | 41 (31.8) | 46 (6.1) | 21 (9.0) | 13 (7.7) | <0.0001 |
| 1–5 Years | 334 (23.7) | 37 (29.8) | 86 (66.7) | 107 (14.1) | 54 (23.2) | 50 (29.6) | |
| 6 Years or longer | 952 (67.4) | 82 (66.1) | 2 (1.6) | 604 (79.8) | 158 (67.8) | 106 (62.7) | |
| Have you attended specific training in the care COVID-19 patients? n (%) | |||||||
| yes | 722 (57.5) | 70 (58.3) | 17 (15.3) | 520 (69.7) | 99 (51.0) | 16 (18.8) | <0.0001 |
| no | 534 (42.5) | 50 (41.7) | 94 (84.7) | 226 (30.3) | 95 (49.1) | 69 (81.2) | |
| Have you attended infection prevention and control training (all infections, not only COVID-19)? n (%) | |||||||
| yes | 1179 (83.5) | 114 (91.9) | 74 (57.4) | 729 (96.3) | 178 (76.4) | 84 (49.7) | <0.0001 |
| no | 223 (16.5) | 10 (8.1) | 55 (42.6) | 28 (3.7) | 55 (23.6) | 85 (50.3) | |
| How much cumulative IPC training to standard and additional transmission-based precautions have you received at your health care facility? n (%) | |||||||
| <2 h | 908 (64.3) | 88 (71.0) | 53 (41.1) | 580 (76.6) | 136 (58.4) | 51 (30.2) | <0.0001 |
| 2 h or more | 218 (15.4) | 22 (17.7) | 4 (3.1) | 151 (19.9) | 30 (12.9) | 11 (6.5) | |
| I don’t know what IPC standard precautions are | 286 (20.3) | 14 (11.3) | 72 (55.8) | 26 (3.4) | 67 (28.8) | 107 (63.3) | |
| Was the IPC training on standard and additional transmission-based carried out remotely or practical? n (%) | |||||||
| Only remotely | 558 (39.5) | 58 (46.8) | 47 (36.4) | 298 (39.4) | 91 (39.1) | 64 (37.9) | <0.0001 |
| Only practical | 51 (3.6) | 4 (3.2) | 6 (4.7) | 28 (3.7) | 7 (3.0) | 6 (3.6) | |
| Both, practical and remotely | 592 (41.9) | 53 (42.7) | 9 (7.0) | 420 (55.5) | 88 (37.8) | 22 (13.0) | |
| I don’t know what IPC standard precautions are | 211 (14.9) | 9 (7.3) | 67 (51.9) | 11 (1.5) | 47 (20.2) | 77 (45.6) | |
| Do you think you have received enough training to protect yourself and others from infection? n (%) | |||||||
| yes | 1021 (72.3) | 81 (65.3) | 41 (31.8) | 623 (82.3) | 185 (79.4) | 91 (53.8) | <0.0001 |
| no | 236 (16.7) | 39 (31.5) | 59 (45.8) | 97 (12.8) | 22 (9.5) | 19 (11.3) | |
| I don’t know | 155 (11.0) | 4 (3.2) | 29 (22.5) | 37 (4.9) | 26 (11.2) | 59 (34.9) | |
| Can you correctly apply IPC practices? N (%) | |||||||
| yes | 1252 (88.6) | 109 (87.9) | 70 (54.3) | 742 (98.0) | 219 (94.0) | 112 (66.3) | <0.0001 |
| no | 55 (3.9) | 6 (4.8) | 25 (19.4) | 4 (0.5) | 6 (2.6) | 14 (8.3) | |
| I don’t know | 105 (7.4) | 9 (7.3) | 34 (26.4) | 11 (1.5) | 8 (3.4) | 43 (25.4) | |
| Are you familiar with the “hand hygiene moments” recommended by WHO for daily practice in health care? n (%) | |||||||
| I don’t know them | 112 (7.9) | 9 (7.3) | 19 (14.7) | 9 (1.2) | 16 (6.9) | 59 (34.9) | <0.0001 |
| Yes, all 3 | 96 (6.8) | 8 (6.5) | 2 (1.6) | 20 (2.6) | 32 (13.7) | 34 (20.1) | |
| Yes, all 4 | 33 (2.3) | 4 (3.2) | 3 (2.3) | 6 (0.8) | 9 (3.9) | 11 (6.5) | |
| Yes, all 5 | 943 (66.8) | 87 (70.2) | 90 (69.8) | 621 (82.0) | 104 (44.6) | 41 (24.3) | |
| Yes, all 6 | 228 (16.1) | 16 (12.9) | 15 (11.6) | 101 (13.3) | 72 (30.9) | 24 (14.2) | |
| Knowledge and Performance Index n (%) | |||||||
| High n = 537 (45.1) | 537 (45.1) | 38 (31.7) | 22 (17.5) | 418 (56.3) | 53 (31.2) | 6 (18.8) | <0.0001 |
| Low n = 654 (54.9) | 654 (54.9) | 82 (68.3) | 104 (82.5) | 325 (43.7) | 117 (68.8) | 26 (81.3) | |
| Characteristics of the Study Group | Do You Think You Have Received Enough Training to Protect Yourself and Others from Infection? | p Value * | Can You Correctly Apply IPC Practices? | p Value * | ||
|---|---|---|---|---|---|---|
| No, n = 226 (20.6%) | Yes, n = 869 (79.4%) | No, n = 103 (8.3%) | Yes, n = 1140 (91.7%) | |||
| Occupation, n (%) | ||||||
| Physicians | 37 (32.5) | 77 (67.5) | <0.0001 | 15 (12.1) | 109 (87.9) | <0.0001 |
| Medical students | 43 (58.1) | 31 (41.9) | 59 (45.7) | 70 (54.3) | ||
| Nurses/midwifes and paramedics | 123 (16.9) | 606 (83.1) | 15 (2.0) | 742 (98.0) | ||
| Other HCWs | 23 (12.9) | 155 (87.1) | 14 (6.0) | 219 (94.0) | ||
| Age [year], n (%) | ||||||
| 18–36 | 136 (34.5) | 256 (65.5) | <0.0001 | 85 (17.1) | 412 (82.9) | <0.0001 |
| 37–55 | 73 (13.9) | 453 (86.1) | 14 (2.5) | 541 (97.5) | ||
| 56 or older | 17 (9.7) | 158 (90.3) | 4 (2.1) | 187 (97.9) | ||
| Sex, n (%) | ||||||
| Female | 189 (19.0) | 804 (81.0) | <0.0001 | 78 (7.0) | 1033 (93.0) | <0.0001 |
| Male | 37 (36.3) | 67 (63.7) | 25 (18.9) | 107 (81.1) | ||
| Participation in specific training in the care COVID-19 patients, n (%) | ||||||
| Yes | 80 (11.5) | 615 (88.5) | <0.0001 | 13 (1.8) | 693 (98.2) | <0.0001 |
| No | 136 (38.5) | 217 (61.5) | 76 (16.3) | 389 (83.7) | ||
| Form of general training, n (%) | ||||||
| Only remote | 130 (28.6) | 324 (71.4) | <0.0001 | 29 (5.9) | 465 (94.1) | <0.0001 |
| Practical and remote or practical | 60 (10.3) | 525 (89.7) | 17 (2.8) | 598 (97.2) | ||
| Duration of IPC training, n (%) | ||||||
| <2 h | 162 (20.0) | 648 (80.0) | <0.001 | 36 (4.2) | 6 (2.9) | <0.0001 |
| 2 h or more | 19 (9.5) | 180 (90.5) | 821 (95.8) | 201 (97.1) | ||
| Knowledge and Performance Index, n (%) | ||||||
| high | 77 (15.1) | 434 (84.9) | <0.001 | 14 (2.6) | 517 (97.4) | <0.0001 |
| low | 136 (25.9) | 389 (74.1) | 76 (12.1) | 552 (87.9) | ||
| Study Group/Profession | Self-Assessment of Preparedness for Patient Care | Use of IPC Practices | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Sex, female vs. male | 1.77 | 0.95–3.23 | 0.071 | 0.88 | 0.34–2.26 | 0.794 |
| Age | ||||||
| 18–36 | Ref | Ref | ||||
| 37–55 | 2.47 | 1.62–3.77 | <0.0001 | 1.81 | 0.68–4.79 | 0.233 |
| 56 or older | 3.19 | 1.69–6.01 | <0.0001 | 2.07 | 0.44–9.72 | 0.355 |
| Occupation | ||||||
| Physicians | Ref | Ref | ||||
| Medical students | 1.35 | 0.60–3.04 | 0.473 | 0.44 | 0.16–1.19 | 0.106 |
| Nurses/midwifes and paramedics | 1.11 | 0.63–1.94 | 0.720 | 4.22 | 1.60–11.15 | 0.004 |
| Others HCWs | 3.34 | 1.4–7.98 | 0.007 | 4.92 | 1.00–24.17 | 0.050 |
| Participation in specific training in the care COVID-19 patients, yes vs. no | 2.97 | 2.03–4.35 | <0.0001 | 3.59 | 1.55–8.33 | 0.003 |
| Form of general training, remote with practice vs. remote | 2.78 | 1.87–4.10 | <0.0001 | 1.25 | 0.57–2.75 | 0.584 |
| Duration of IPC training, 2 h or more vs. <2 h | 1.51 | 0.87–2.63 | 0.141 | 0.83 | 0.30–2.25 | 0.711 |
| Knowledge and Performance Index, high vs. low | 1.42 | 0.98–2.09 | 0.066 | 2.15 | 0.95–4.85 | 0.066 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Żółtowska, B.; Barańska, I.; Szczerbińska, K.; Różańska, A.; Mydel, K.; Sydor, W.; Heczko, P.B.; Jachowicz, E.; Wójkowska-Mach, J. Preparedness of Health Care Workers and Medical Students in University Hospital in Krakow for COVID-19 Pandemic within the CRACoV Project. J. Clin. Med. 2021, 10, 3487. https://doi.org/10.3390/jcm10163487
Żółtowska B, Barańska I, Szczerbińska K, Różańska A, Mydel K, Sydor W, Heczko PB, Jachowicz E, Wójkowska-Mach J. Preparedness of Health Care Workers and Medical Students in University Hospital in Krakow for COVID-19 Pandemic within the CRACoV Project. Journal of Clinical Medicine. 2021; 10(16):3487. https://doi.org/10.3390/jcm10163487
Chicago/Turabian StyleŻółtowska, Barbara, Ilona Barańska, Katarzyna Szczerbińska, Anna Różańska, Krzysztof Mydel, Wojciech Sydor, Piotr B. Heczko, Estera Jachowicz, and Jadwiga Wójkowska-Mach. 2021. "Preparedness of Health Care Workers and Medical Students in University Hospital in Krakow for COVID-19 Pandemic within the CRACoV Project" Journal of Clinical Medicine 10, no. 16: 3487. https://doi.org/10.3390/jcm10163487
APA StyleŻółtowska, B., Barańska, I., Szczerbińska, K., Różańska, A., Mydel, K., Sydor, W., Heczko, P. B., Jachowicz, E., & Wójkowska-Mach, J. (2021). Preparedness of Health Care Workers and Medical Students in University Hospital in Krakow for COVID-19 Pandemic within the CRACoV Project. Journal of Clinical Medicine, 10(16), 3487. https://doi.org/10.3390/jcm10163487








