Effects, Side Effects and Contraindications of Relaxation Massage during Pregnancy: A Systematic Review of Randomized Controlled Trials
Abstract
1. Introduction
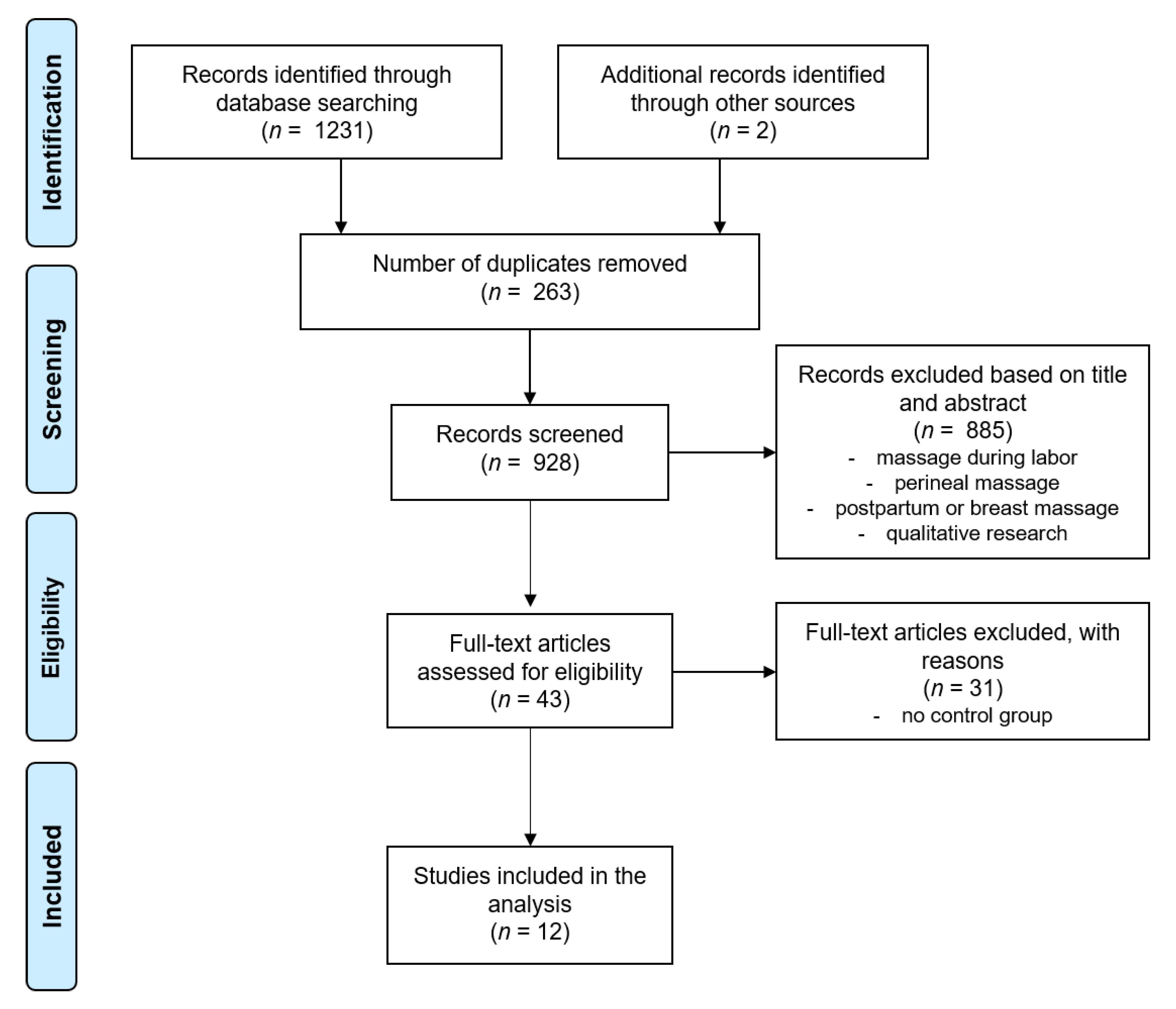
2. Methods
3. Results and Discussion
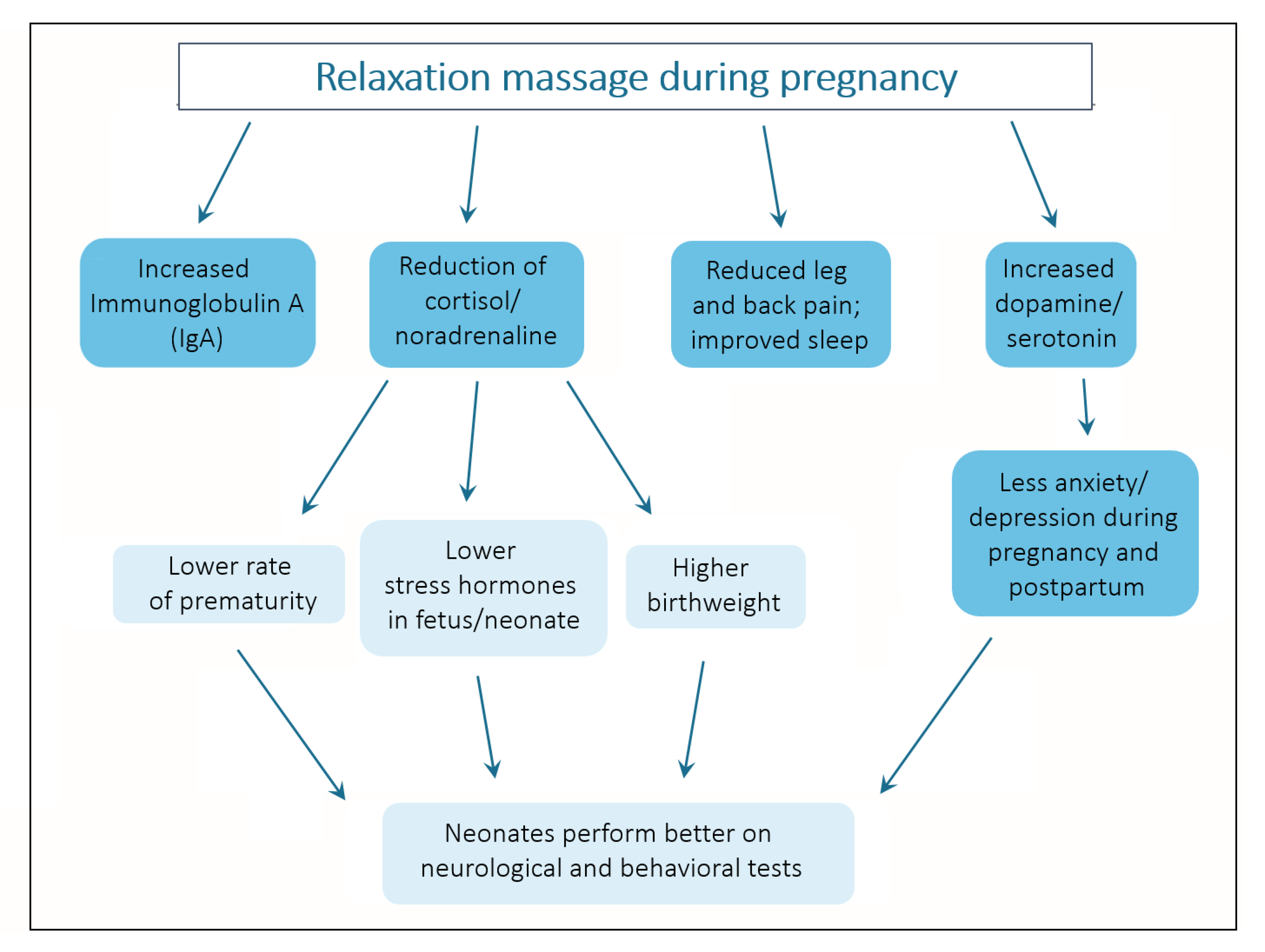
3.1. Effects of Massage during Pregnancy on Mood, Sleep, Pain and Other Pregnancy-Related Discomforts
- back pain was reduced;
- their mood improved;
- they reported calmer and deeper sleep;
- noradrenaline levels were reduced.
3.2. Effects of Massage during Pregnancy on Women with Prenatal Depression
3.3. Effects of Massage during Pregnancy on Fetal Development
3.4. Side Effects, Complications, Precautions and Contraindications
3.4.1. Risk of Thrombosis
3.4.2. Lateral Position
3.4.3. Abdominal Massage
3.4.4. Essential Oils
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Arnold, M.M.; Müller-Oerlinghausen, B.; Hemrich, N.; Bönsch, D. Effects of Psychoactive Massage in Outpatients with Depressive Disorders: A Randomized Controlled Mixed-Methods Study. Brain Sci. 2020, 10, 676. [Google Scholar] [CrossRef] [PubMed]
- Arslan, G.; Ceyhan, Ö.; Mollaoğlu, M. The influence of foot and back massage on blood pressure and sleep quality in females with essential hypertension: A randomized controlled study. J. Hum. Hypertens. 2020, 35, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Asadi, Z.; Shakibaei, F.; Mazaheri, M.; Jafari-Mianaei, S. The Effect of Foot Massage by Mother on the Severity of Attention-Deficit Hyperactivity Disorder Symptoms in Children Aged 6–12. Iran. J. Nurs. Midwifery Res. 2020, 25, 189–194. [Google Scholar] [CrossRef]
- Ashman, S.B.; Dawson, G.; Panagiotides, H.; Yamada, E.; Wilkinson, C.W. Stress hormone levels of children of depressed mothers. Dev. Psychopathol. 2002, 14, 333–349. [Google Scholar] [CrossRef]
- Hashemi, S.H.; Hajbagheri, A.; Aghajani, M. The Effect of Massage with Lavender Oil on Restless Leg Syndrome in Hemodialysis Patients: A Randomized Controlled Trial. Nurs. Midwifery Stud. 2015, 4, e29617. [Google Scholar] [CrossRef]
- Schetter, C.D.; Tanner, L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr. Opin. Psychiatry 2012, 25, 141–148. [Google Scholar] [CrossRef]
- Bonari, L.; Pinto, N.; Ahn, E.; Einarson, A.; Steiner, M.; Koren, G. Perinatal Risks of Untreated Depression During Pregnancy. Can. J. Psychiatry 2004, 49, 726–735. [Google Scholar] [CrossRef]
- Dennis, C.-L.; Dowswell, T. Interventions (other than pharmacological, psychosocial or psychological) for treating antenatal depression. Cochrane Database Syst. Rev. 2013, 7, CD006795. [Google Scholar] [CrossRef]
- Kurki, T.; Hiilesmaa, V.; Raitasalo, R.; Mattila, H.; Ylikorkala, O. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet. Gynecol. 2000, 95, 487–490. [Google Scholar]
- Dayan, J.; Creveuil, C.; Herlicoviez, M.; Herbel, C.; Baranger, E.; Savoye, C.; Thouin, A. Role of anxiety and depression in the onset of spontaneous preterm labor. Am. J. Epidemiol. 2002, 155, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Chung, T.K.; Lau, T.K.; Yip, A.S.; Chiu, H.F.; Lee, D.T. Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosom. Med. 2001, 63, 830–834. [Google Scholar] [CrossRef]
- Oberlander, T.F.; Warburton, W.; Misri, S.; Aghajanian, J.; Hertzman, C. Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population-based linked health data. Arch. Gen. Psychiatry 2006, 63, 898–906. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Melotti, R.; Heron, J.; Ramchandani, P.; Wiles, N.; Murray, L.; Stein, A. The timing of maternal depressive symptoms and child cognitive development: A longitudinal study. J. Child. Psychol. Psychiatry 2012, 53, 632–640. [Google Scholar] [CrossRef] [PubMed]
- Field, T.; Diego, M.; Hernandez-Reif, M.; Deeds, O.; Figueiredo, B. Pregnancy massage reduces prematurity, low birthweight and postpartum depression. Infant Behav. Dev. 2009, 32, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Lundy, B.L.; Jones, N.A.; Field, T.; Nearing, G.; Davalos, M.; Pietro, P.A.; Schanberg, S.; Kuhn, C. Prenatal depression effects on neonates. Infant Behav. Dev. 1999, 22, 119–129. [Google Scholar] [CrossRef]
- Luoma, I.; Tamminen, T.; Kaukonen, P.; Laippala, P.; Puura, K.; Salmelin, R.; Almqvist, F. Longitudinal study of maternal depressive symptoms and child well-being. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 1367–1374. [Google Scholar] [CrossRef]
- Beck, C.T. Predictors of postpartum depression—An update. Nurs. Res. 2001, 50, 275–285. [Google Scholar] [CrossRef]
- Auerbach, J.G.; Hans, S.L.; Marcus, J.; Maeir, S. Maternal psychotropic medication and neonatal behavior. Neurotoxicol. Teratol. 1992, 14, 399–406. [Google Scholar] [CrossRef]
- Hendrick, V.; Stowe, Z.N.; Altshuler, L.L.; Hwang, S.; Lee, E.; Haynes, D. Placental passage of antidepressant medications. Am. J. Psychiatry 2003, 160, 993–996. [Google Scholar] [CrossRef]
- Previti, G.; Pawlby, S.; Chowdhury, S.; Aguglia, E.; Pariante, C.M. Neurodevelopmental outcome for offspring of women treated for antenatal depression: A systematic review. Arch. Womens. Ment. Health 2014, 17, 471–483. [Google Scholar] [CrossRef]
- Sujan, A.C.; Rickert, M.E.; Öberg, A.S.; Quinn, P.D.; Hernández-Díaz, S.; Almqvist, C.; Lichtenstein, P.; Larsson, H.; D’Onofrio, B.M. Associations of Maternal Antidepressant Use During the First Trimester of Pregnancy With Preterm Birth, Small for Gestational Age, Autism Spectrum Disorder, and Attention-Deficit/Hyperactivity Disorder in Offspring. JAMA 2017, 317, 1553–1562. [Google Scholar] [CrossRef]
- Hall, H.; Cramer, H.; Sundberg, T.; Ward, L.; Adams, J.; Moore, C.; Sibbritt, D.; Lauche, R. The effectiveness of complementary manual therapies for pregnancy-related back and pelvic pain: A systematic review with meta-analysis. Medicine 2016, 95, e4723. [Google Scholar] [CrossRef]
- Liddle, S.D.; Pennick, V. Interventions for preventing and treating low-back and pelvic pain during pregnancy. Cochrane Database Syst. Rev. 2015, 9, CD001139. [Google Scholar] [CrossRef]
- Fogarty, S.; Barnett, R.; Hay, P. Safety and Pregnancy Massage: A Qualitative Thematic Analysis. Int. J. Ther. Massage Bodyw. 2020, 13, 4–12. [Google Scholar]
- Mueller, S.M.; Grunwald, M. Taktile Körperstimulation (Massage) in der Pränatal-und Geburtsmedizin. Man. Med. 2019, 57, 254–259. [Google Scholar] [CrossRef]
- Hall, H.G.; Cant, R.; Munk, N.; Carr, B.; Tremayne, A.; Weller, C.; Fogarty, S.; Lauche, R. The effectiveness of massage for reducing pregnant women’s anxiety and depression; systematic review and meta-analysis. Midwifery 2020, 90, 102818. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.A.; Shewamene, Z.; Galbally, M.; Schmied, V.; Dahlen, H. The effect of complementary medicines and therapies on maternal anxiety and depression in pregnancy: A systematic review and meta-analysis. J. Affect. Disord. 2019, 245, 428–439. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 29 June 2021).
- Cochrane Bias Methods Group. Using the RoB Tool to Assess Risk of Bias of Included Studies. Available online: https://methods.cochrane.org/sites/methods.cochrane.org.bias/files/public/uploads/Cochrane%20methodology%20annual%20training_ib4_0.pdf (accessed on 14 July 2021).
- Field, T.; Diego, M.A.; Hernandez-Reif, M.; Schanberg, S.; Kuhn, C. Massage therapy effects on depressed pregnant women. J. Psychosom. Obstet. Gynaecol. 2004, 25, 115–122. [Google Scholar] [CrossRef]
- Field, T.; Hernandez-Reif, M.; Hart, S.; Theakston, H.; Schanberg, S.; Kuhn, C. Pregnant women benefit from massage therapy. J. Psychosom. Obstet. Gynaecol. 1999, 20, 31–38. [Google Scholar] [CrossRef]
- Khojasteh, F.; Rezaee, N.; Safarzadeh, A.; Sahlabadi, R.; Shahrakipoor, M. Comparison of the effects of massage therapy and guided imagery on anxiety of nulliparous women during pregnancy. Depression 2016, 13, 14. [Google Scholar]
- El-Hosary, E.A.; Soliman, H.F.A.; El-Homosy, S.M. Effect of Therapeutic Massage on Relieving Pregnancy Discomforts. IOSR 2016, 5, 57–64. [Google Scholar] [CrossRef]
- Field, T.; Diego, M.; Hernandez-Reif, M.; Medina, L.; Delgado, J.; Hernandez, A. Yoga and massage therapy reduce prenatal depression and prematurity. J. Bodyw. Mov. Ther. 2012, 16, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Field, T.; Figueiredo, B.; Hernandez-Reif, M.; Diego, M.; Deeds, O.; Ascencio, A. Massage therapy reduces pain in pregnant women, alleviates prenatal depression in both parents and improves their relationships. J. Bodyw. Mov. Ther. 2008, 12, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Manber, R.; Schnyer, R.N.; Allen, J.J.B.; Rush, A.J.; Blasey, C.M. Acupuncture: A promising treatment for depression during pregnancy. J. Affect. Disord. 2004, 83, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Manber, R.; Schnyer, R.N.; Lyell, D.; Chambers, A.S.; Caughey, A.B.; Druzin, M.; Carlyle, E.; Celio, C.; Gress, J.L.; Huang, M.I.; et al. Acupuncture for depression during pregnancy: A randomized controlled trial. Obstet. Gynecol. 2010, 115, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Field, T.; Deeds, O.; Diego, M.; Hernandez-Reif, M.; Gauler, A.; Sullivan, S.; Wilson, D.; Nearing, G. Benefits of combining massage therapy with group interpersonal psychotherapy in prenatally depressed women. J. Bodyw. Mov. Ther. 2009, 13, 297–303. [Google Scholar] [CrossRef]
- Hall, H.; Munk, N.; Carr, B.; Fogarty, S.; Cant, R.; Holton, S.; Weller, C.; Lauche, R. Maternal mental health and partner-delivered massage: A pilot study. Women Birth 2021, 34, e237–e247. [Google Scholar] [CrossRef]
- Chen, P.-J.; Chou, C.-C.; Yang, L.; Tsai, Y.-L.; Chang, Y.-C.; Liaw, J.-J. Effects of Aromatherapy Massage on Pregnant Women’s Stress and Immune Function: A Longitudinal, Prospective, Randomized Controlled Trial. J. Altern. Complement. Med. 2017, 23, 778–786. [Google Scholar] [CrossRef]
- Field, T.; Diego, M.; Hernandez-Reif, M.; Schanberg, S.; Kuhn, C.; Yando, R.; Bendell, D. Pregnancy anxiety and comorbid depression and anger: Effects on the fetus and neonate. Depress. Anxiety 2003, 17, 140–151. [Google Scholar] [CrossRef]
- Verran, J.A.; Snyder-Halpern, R. Do patients sleep in the hospital? ANR 1988, 1, 95. [Google Scholar] [CrossRef]
- Huizink, A.C.; Mulder, E.J.; de Medina, P.G.R.; Visser, G.H.; Buitelaar, J.K. Is pregnancy anxiety a distinctive syndrome? Early Hum. Dev. 2004, 79, 81–91. [Google Scholar] [CrossRef]
- Field, T.; Diego, M.; Hernandez-Reif, M. Moderate pressure is essential for massage therapy effects. Int. J. Neurosci. 2010, 120, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Barr, J.S.; Taslitz, N. The influence of back massage on autonomic functions. Phys. Ther. 1970, 50, 1679–1691. [Google Scholar] [CrossRef][Green Version]
- Thomas, R.B. A Pilot Study of Partner Chair Massage Effects on Perinatal Mood, Anxiety, and Pain. Int. J. Ther. Massage Bodyw. 2019, 12, 3–11. [Google Scholar] [CrossRef]
- Field, T.; Grizzle, N.; Scafidi, F.; Schanberg, S. Massage and relaxation therapies’ effects on depressed adolescent mothers. Adolescence 1996, 31, 903–911. [Google Scholar]
- Field, T.; Hernandez-Reif, M.; Diego, M. Newborns of depressed mothers who received moderate versus light pressure massage during pregnancy. Infant Behav. Dev. 2006, 29, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Fogarty, S.; McInerney, C.; Stuart, C.; Hay, P. The side effects and mother or child related physical harm from massage during pregnancy and the postpartum period: An observational study. Complement. Ther. Med. 2019, 42, 89–94. [Google Scholar] [CrossRef]
- Torkzahrani, S.; Mahmoudikohani, F.; Saatchi, K.; Sefidkar, R.; Banaei, M. The effect of acupressure on the initiation of labor: A randomized controlled trial. Women Birth 2017, 30, 46–50. [Google Scholar] [CrossRef] [PubMed]
- McCullough, J.E.M.; Liddle, S.D.; Close, C.; Sinclair, M.; Hughes, C.M. Reflexology: A randomised controlled trial investigating the effects on beta-endorphin, cortisol and pregnancy related stress. Complement. Ther. Clin. Pract. 2018, 31, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Mollart, L. Single-blind trial addressing the differential effects of two reflexology techniques versus rest, on ankle and foot oedema in late pregnancy. Complement. Ther. Nurs. Midwifery 2003, 9, 203–208. [Google Scholar] [CrossRef]
- Shobeiri, F.; Manoucheri, B.; Parsa, P.; Roshanaei, G. Effects of Counselling and Sole Reflexology on Fatigue in Pregnant Women: A Randomized Clinical Trial. J. Clin. Diagn. Res. 2017, 11, QC01–QC04. [Google Scholar] [CrossRef] [PubMed]
- Schlegel, M.L.; Whalen, J.L.; Williamsen, P.M. Integrative Therapies for Women with a High Risk Pregnancy during Antepartum Hospitalization. MCN Am. J. Matern. Child. Nurs. 2016, 41, 356. [Google Scholar] [CrossRef]
- Devis, P.; Knuttinen, M.G. Deep venous thrombosis in pregnancy: Incidence, pathogenesis and endovascular management. Cardiovasc. Diagn. Ther. 2017, 7, S309–S319. [Google Scholar] [CrossRef] [PubMed]
- Sutham, K.; Na-Nan, S.; Paiboonsithiwong, S.; Chaksuwat, P.; Tongsong, T. Leg massage during pregnancy with unrecognized deep vein thrombosis could be life threatening: A case report. BMC Pregnancy Childbirth 2020, 20, 237. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, H.; Takagi, S.; Zhang, K.; Furui, I.; Ozaki, M. Effect of Lateral Tilt Angle on the Volume of the Abdominal Aorta and Inferior Vena Cava in Pregnant and Nonpregnant Women Determined by Magnetic Resonance Imaging. Anesthesiology 2015, 122, 286–293. [Google Scholar] [CrossRef]
- Ugboma, H.A.; Akani, C.I. Abdominal massage: Another cause of maternal mortality. Niger. J. Med. 2004, 13, 259–262. [Google Scholar]
- Dhany, A.L.; Mitchell, T.; Foy, C. Aromatherapy and massage intrapartum service impact on use of analgesia and anesthesia in women in labor: A retrospective case note analysis. J. Altern. Complement. Med. 2012, 18, 932–938. [Google Scholar] [CrossRef]
- Zahra, A.; Leila, M.S. Lavender aromatherapy massages in reducing labor pain and duration of labor: A randomized controlled trial. Afr. J. Pharm. Pharmacol. 2013, 7, 426–430. [Google Scholar] [CrossRef]
| Reference | Methodological Quality | Risk of Bias | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Quality Rating a | A | B | C | D | E | |
| [14] | + | + | ? | + | + | + | + | + | + | 8 | ? | ? | ? | ? | ? |
| [30] | + | + | ? | ? | + | ? | + | + | + | 6 | ? | ? | ? | ? | ? |
| [31] | + | − | − | ? | + | ? | + | + | + | 5 | ? | ? | ? | ? | ? |
| [32] | + | ? | + | + | + | + | + | ? | + | 7 | − | ? | ? | + | ? |
| [33] | + | ? | ? | + | + | + | ? | + | ? | 5 | ? | ? | ? | + | ? |
| [34] | + | + | ? | − | + | + | + | + | + | 7 | ? | ? | ? | − | ? |
| [35] | + | − | − | + | + | + | ? | + | + | 6 | ? | ? | ? | ? | ? |
| [36] | + | + | − | ? | ? | − | + | ? | |||||||
| [37] | + | + | − | + | + | + | + | + | − | 7 | ? | ? | − | + | ? |
| [38] | + | + | ? | ? | + | + | + | + | − | 6 | ? | ? | ? | + | ? |
| [39] | + | + | − | + | + | + | − | + | + | 7 | ? | ? | ? | ? | ? |
| [40] | + | + | − | + | + | + | + | + | − | 7 | ? | ? | ? | ? | ? |
| Reference | Sample Size Mean Age/Ethnicity | GA in Weeks at Study Start | Groups and Interventions | Assessment Tools (Anxiety, Depression, Pain, etc.) | Outcome Mothers | Outcome Neonates | Side Effects | Complications | Precautions |
|---|---|---|---|---|---|---|---|---|---|
| [14] | 200 depressed women were recruited and randomized, 149 took part (61 control, 88 intervention); Mean (SD) age: control group: 25.2 (5.8); massage group: 27.2 (6.5); USA: 57% Hispanic, 38% African American, and 5% Non-Hispanic | Between 16 and 20 weeks gestation | Two groups: massage group received 2 moderate pressure massages per week for 12 weeks by their significant other Control: standard care | Mother: SCID; CES-D; STAI; The Daily Hassles Scale [41]; Sleep Disturbance Scale [42]; back pain VAS Neonate: Saliva cortisol; birthweight; gestational age; Brazelton Neonatal Behavior Assessment Scale (BNBAS). | Long-term effects (first vs. last day of study): less depression and back pain in massage group; No diff. between groups in anxiety, sleep disturbance or daily hassles | Massage group: lower incidence of prematurity and low birthweight; neonates: lower cortisol levels; better performance on BNBAS habituation, orientation and motor scales | Not assessed | Not assessed | Only low-risk, uncomplicated pregnancies, healthy mothers |
| [30] | 84 depressed pregnant women were recruited plus 28 non-depressed women; Mean (SD) age: 28.8 (5.7); USA: 46% Caucasian, 39% Hispanic, 12% African American and 3% Asian | Between 18 and 24 weeks gestation (M = 22.9) | Four groups: massage therapy group by significant other; progressive muscle relaxation group; 20 min sessions per week for 16 weeks; two control groups (depressed/ non-depressed) standard prenatal care | STAI; Profile of Mood States Scale (POMS); CDC-D; pain VAS; Urine: cortisol, catecholamines (norepinephrine, epinephrine, dopamine) and serotonin (5-HIAA) Postnatal: Obstetric Complications (OCS) and Postnatal Factor (PNF) Scales; Brazelton Neonatal Behavior Assessment Scale (BNBAS) | Immediate effects (pre/post session): Massage: lower levels of anxiety and depressed mood, less leg and back pain. PMR: less leg pain Control groups: no change Long-term effects (first vs. last day of study): Massage: higher dopamine and serotonin levels, lower levels of cortisol and norepinephrine PMR and control groups: no change | Massage group: lower incidence of prematurity and low birthweight; better performance than depressed control on BNBAS: habituation, range of state, autonomic stability, withdrawal scales, depressed scale, motor maturity | Not assessed | Massage group had less obstetric complication than PMR or depressed control | Not reported |
| [31] | 26 pregnant women; mean (SD) age: massage 29 (3), relaxation 30 (2); range 23–35 USA: 46% Caucasian, 11% Hispanic, 38% African American and 4% other | Between 14 and 30 weeks gestation; gestational weeks Massage: 23.3 (4) PMR Relaxation: 23.6 (5) | Two groups: massage therapy by trained massage therapists; PMR relaxation therapy group at home alone; 20 min sessions twice a week for 5 weeks | STAI; Profile of Mood States Scale (POMS); CDC-D; pain VAS; The Sleep Disturbance Scale (Verran & Snyder-Halpern, 1988); urine: cortisol, catecholamines (norepinephrine, epinephrine, dopamine) and serotonin (5-HIAA) | Immediate effects (pre post session): Massage group: less STAI, POMS, less leg and back pain; relaxation group: less leg pain; Long-term effects (first session vs. last session): massage group: less sleep disturbance; less norepinephrine; more dopamine; PMR group: more dopamine | Fewer premature births in massage group | Not assessed | Fewer obstetric complications, fewer postnatal complications in massage group | Not reported |
| [32] | 75 nulliparous pregnant women; 25 per group mean (SD) age: massage: 22.76 (3.85), guided imagery: 23.76 (3.74), control: 23.92 (4.41); Iran: Persians and Baloch | GA massage: 22.12 ± 0.93 GA-guided imagery: 22.20 (0.87) GA control: 22.12 (0.93) | Three groups: massage therapy (20 min once a week, for six weeks; Guided Imagery group (once a week by experimenter; every day video CD; Control group standard care | Pregnancy-related Anxiety Questionnaire—Revised [43] | Long-term effects (first session vs. last session): Massage and guided imagery (GI): sign. less anxiety compared to control group; no diff between massage and GI; Control group: sign. more anxiety post intervention | Not assessed | Not assessed | Not assessed | Only healthy women with low-risk pregnancy included |
| [33] | 150 pregnant women, 75 per group; age mean (SD): 24.4 (4.35), Range: 19 to 33 | Between 14 and 30 weeks GA; massage group 26.3 (3.77), control group 26.6 (3.81) | Two groups: Massage by confidante at home; 10–20 min twice/week over 5 week: Control group standard care | VAS pain; VAS sleep; Pregnancy-related Anxiety Questionnaire | Massage group less pregnancy discomforts: headache, backache, muscle cramp, sleep disturbance and anxiety; no diff. between groups in joint pain | Not assessed | Not assessed | Not assessed | Excluded were women who had high risk pregnancy or abnormal fetal condition |
| [34] | 208 were screened for depression, 84 prenatally depressed women were analyzed; age: M = 26.6 years (Range 18–40); 38% Hispanic, 40% African American, and 12% Non-Hispanic White | Between 18 and 23 weeks GA | Three groups: Yoga (group sessions); professional massage therapy; standard prenatal care control group; 12 weeks twice weekly yoga or massage therapy sessions (20 min each) | SCID; Sociodemographic/Social Support Questionnaire; CES-D; STAI; STAXI; Pain VAS; Relationship Questionnaire | Long-term effects (first session vs. last session): Yoga group and massage group had greater decrease of depression, anxiety, back and leg pain and a greater increase on relationship scale than control group | Yoga and massage groups had greater gestational age and birthweight than the control group | Not assessed | Not assessed | Uncomplicated pregnancy |
| [35] | Number of participants unclear: 47 or 57 depressed (subclinical) pregnant women and their partners; between 18 and 40 years old (M = 27.9); 59% Hispanic, 32% Black and 9% Caucasian | 2nd trimester | Two groups: Massage from partner; control group standard care; two 20 min massages per week; duration unclear: 12 or 16 weeks | SCID; Sociodemographic/Social Support Questionnaire; CES-D; STAI; STAXI; Pain VAS | Long-term effects (first session vs. last session): Massaged mothers: decreased leg pain and back pain, decreased depression, anxiety and anger, improved relationship with partner; fathers who massaged their partners versus the control group fathers: decreased depression and anxiety, improved relationship with partner | Not assessed | Not assessed | Not assessed | Healthy mothers with uncomplicated pregnancies |
| [36] | 88 were screened, 61 randomized, 54 analyzed: pregnant women with major depressive disorder and a Hamilton Rating Scale for Depression score > 14; mean (SD) age: 33.3 (4.7); Caucasian 75% | Between 11 and 28 weeks GA; M = 20.0 (5.6) | Three groups: acupuncture specific for depression (ASD; n = 16), non-specific acupuncture (NASD; n = 19), massage (n = 19); 8 weeks; 12 sessions (25–30 min each) | Hamilton Rating Scale for Depression; BDI; SCID | Long-term effects (first session vs. last session): reduction in depressive symptoms in all three groups; no difference between groups | Not assessed | Not assessed | Not assessed | Not reported |
| [37] | 183 depressed women recruited, 150 randomized, 141 began treatment; 33 discontinued treatment; mean (SD) age: ASD 32.4 (4.0); NASD 33,4 (5.0); Massage 32.8 (5.6) | GA week: ASD 19.8 (6.2); NASD 21.29 (5.4); Massage 21.06 (5.6) | Three groups: Acupuncture specific for depression (ASD; n = 49); Non-specific acupuncture (NASD; n = 44); Massage (n = 48); intervention 25 min, two times per week for the first 4 weeks and weekly for 4 more weeks; | Hamilton Rating Scale for Depression; BDI; SCID | Long-term effects (first session vs. last session): reduction in depressive symptoms in all three groups, highest decrease in ASD | Not assessed | Massage: 2% of women reported side effects (tiredness after treatment); Acupuncture: almost half of participants experienced mild or transient side effects (e.g., nausea, headache or sleep disturbance after treatment) | Ten unexpected/adverse events occurred: (1) premature delivery of twins with one neonatal demise and the surviving twin receiving prolonged neonatal intensive care (ASD); (2) pregnancy loss (NASD); (3) congenital defects among two neonates (one ASD, one prenatal massage); (4) hospitalization for esophageal spasms (prenatal massage); (5) hospitalization with dehydration and low amniotic fluid (NASD); 6) hospitalization for isolated atrial fibrillation (prenatal massage); (7) hospitalization because of premature contractions (prenatal massage); (8) preeclampsia (two in NASD). The study investigators and the Data Safety and Monitoring Board classified all events as unrelated to treatment. | Complications were no exclusion criteria, but 10 women dropped out due to pregnancy complications |
| [38] | 320 were screened for depression; 112 pregnant women were diagnosed w depression and randomized; 48 were analyzed; mean (SD) age: PT: 23.71 (7.17), PT plus massage: 26.77 (5.19); 27% Hispanic, 68% Black and 5% White | Weeks GA: PT: 21.65 (4.44) PT plus massage: 19.98 (5.57) | Two groups: Inter-personal group psychotherapy (PT, n = 21); Inter-personal group psychotherapy plus massage (n = 27); PT 1 h per week; professional massage 20 min per week for 6 weeks | SCID; CES-D; STAI; STAXI; Relationship Questionnaire | PT plus massage: attended more sessions on average, and a greater percentage completed the 6-week program; Long-term effects (first session vs. last session): greater decrease in depression, depressed affect, somatic vegetative symptoms, anxiety and cortisol | No difference in birth weight or GA at birth | Not assessed | Not assessed | Not reported |
| [39] | 113 assessed; 44 randomized; 27 women/partner dyads took part; Massage: n = 14 dyads, control: n = 13 dyads; women with self-reported mild-to-moderate anxiety (0–100 VAS scale) Age 19 to 41 years (mean age 29 years) | Between 28 and 32 weeks gestation | Two groups: Partner-delivered relaxation massage; control group: self-directed stress management training; at least one 20 min session per week till birth | DASS-21 subscale scores (anxiety, depression, stress) online questionnaire, every 4 weeks; Adverse events were reported weekly in online diary | Long-term effects (first vs. last day of study): Both programs decreased women’s symptoms of anxiety, depression and stress with no significant differences identified between the two groups | No difference between groups | Massage group: only two adverse events were reported: exacerbation of anxiety and tiredness. Control group: 12 participants reported adverse events, including sleeping problems (n = 4), pain (n = 3), exhaustion (n = 2), anxiety (n = 2) | No complications occurred | Only women with low-risk pregnancy included |
| [40] | 93 screened, 62 met inclusion criteria, 52 took part; Mean (SD) age: 33.31 (4.01), range 24–43 years; Chinese | Mean 16 weeks GA | Two groups: massage (n = 24); control (n = 28); 70 min of aromatherapy massage with 2% lavender essential oil every other week (10 times in total) for 20 weeks; control group routine prenatal care | Salivary cortisol and immunoglobulin A (IgA) levels were collected before and after massage every 4 weeks (16, 20, 24, 30, 32, 36 weeks GA) | Immediate effects (pre/post session): Massage: lower cortisol and higher IgA levels at all six timepoints; no change in CO; Longitudinal: pre-test cortisol remained stable in massage group but increased successively in control group; pre-test IgA increased successively in massage group but not in control group | Not assessed | Not reported | Not reported | Healthy, low-risk, uncomplicated pregnancies |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mueller, S.M.; Grunwald, M. Effects, Side Effects and Contraindications of Relaxation Massage during Pregnancy: A Systematic Review of Randomized Controlled Trials. J. Clin. Med. 2021, 10, 3485. https://doi.org/10.3390/jcm10163485
Mueller SM, Grunwald M. Effects, Side Effects and Contraindications of Relaxation Massage during Pregnancy: A Systematic Review of Randomized Controlled Trials. Journal of Clinical Medicine. 2021; 10(16):3485. https://doi.org/10.3390/jcm10163485
Chicago/Turabian StyleMueller, Stephanie M., and Martin Grunwald. 2021. "Effects, Side Effects and Contraindications of Relaxation Massage during Pregnancy: A Systematic Review of Randomized Controlled Trials" Journal of Clinical Medicine 10, no. 16: 3485. https://doi.org/10.3390/jcm10163485
APA StyleMueller, S. M., & Grunwald, M. (2021). Effects, Side Effects and Contraindications of Relaxation Massage during Pregnancy: A Systematic Review of Randomized Controlled Trials. Journal of Clinical Medicine, 10(16), 3485. https://doi.org/10.3390/jcm10163485





