Functional and Patient-Centered Treatment Outcomes with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants: A Randomized Clinical Trial
Abstract
:1. Introduction
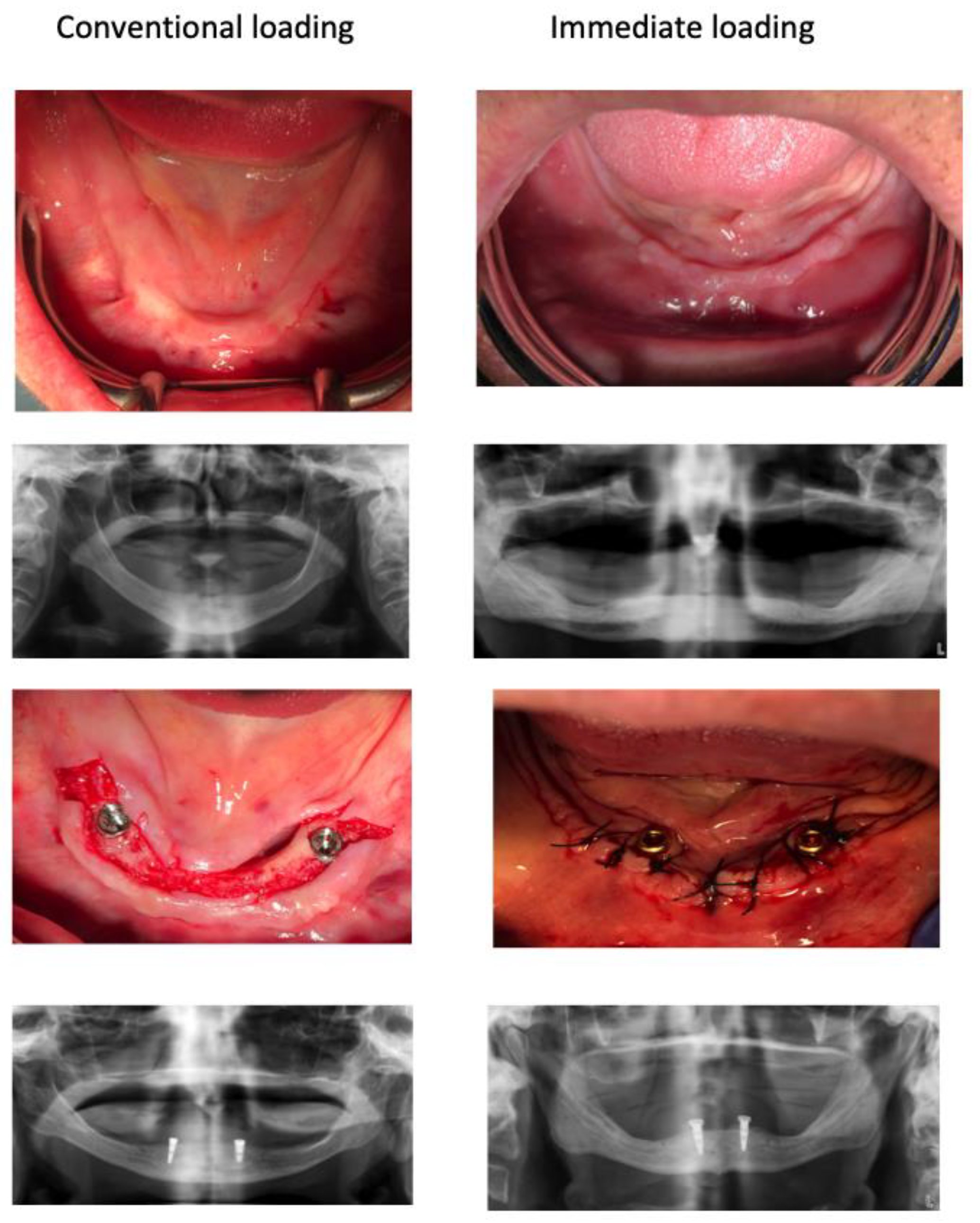
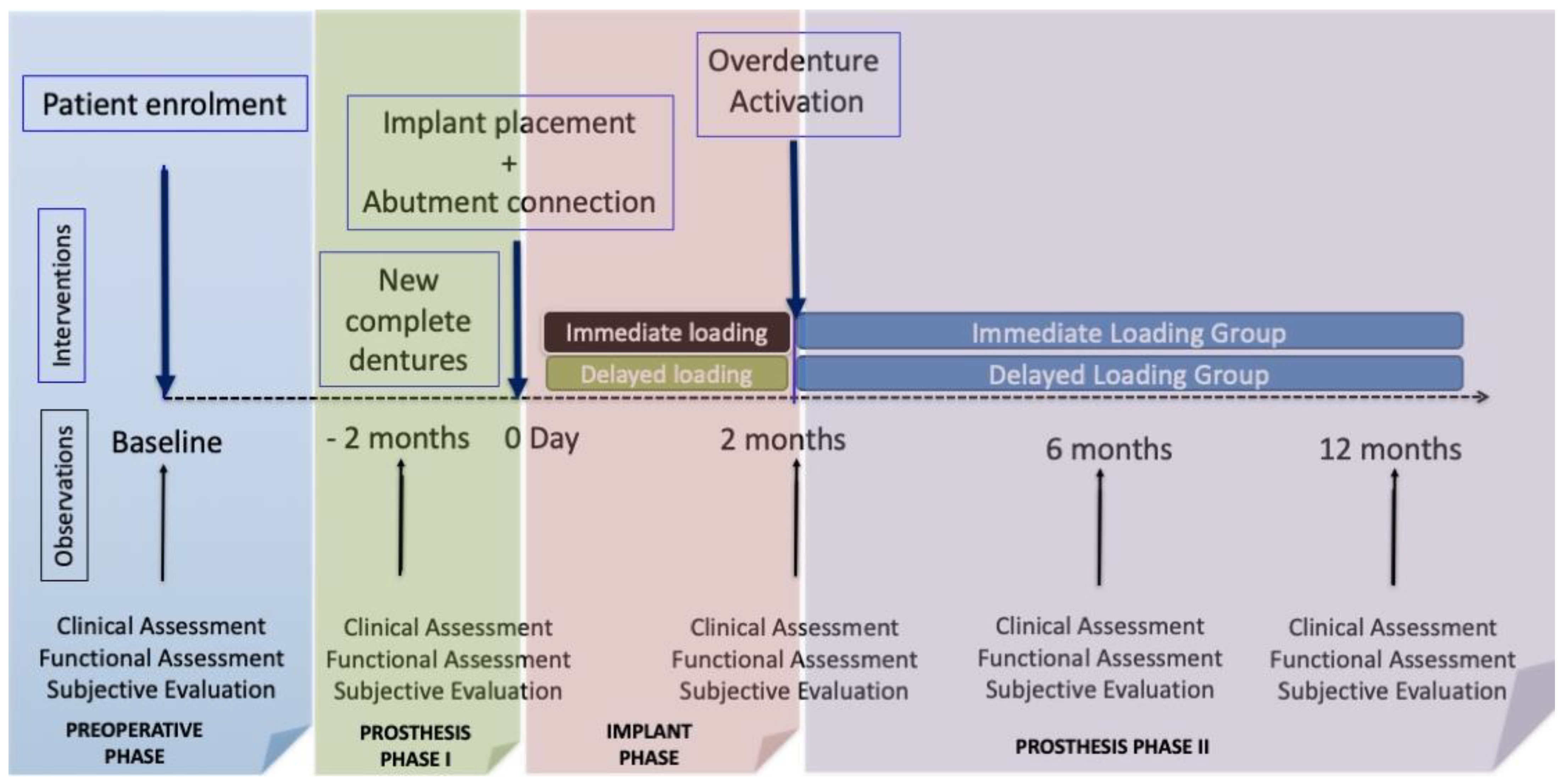
2. Materials and Methods
Data Analysis
3. Results
3.1. Sample Description
3.2. Baseline Prosthetic Status
3.3. Baseline Anatomical Conditions
3.4. Change in the Occlusal Pattern after Prosthetic Treatments
3.5. Change of the EMG Muscular Activity after Prosthetic Treatments
3.6. Change in Chewing Ability by Leake Index
3.7. Change in Self-Rated Satisfaction after Prosthetic Treatments
3.8. Change in Oral Health-Related Quality of Life after Prosthetic Treatments
3.9. Retrospective Evaluation of the Well-Being Change by Global Transitional Items
3.10. Changes in Masticatory Performance by Mixing Ability Tests
3.11. Predictors of Patient-Centered Treatment Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CD | complete denture |
| EMG | electromyography |
| GTI | Global Transitional Items |
| ISOD | implant-supported overdentures |
| ISQ | implant stability quotient |
| MID | minimally important difference |
| OHQoL | Oral Health-related Quality of Life |
| OHIP | Oral Health Impact Profile |
| OSS | Oral Satisfaction Scale |
| RCT | randomized clinical trial |
References
- Petersen, P.E.; Bourgeois, D.; Ogawa, H.; Estupinan-Day, S.; Ndiaye, C. The global burden of oral diseases and risks to oral health. Bull. World Health Organ. 2005, 83, 661–666. [Google Scholar]
- Bravo Perez, M.; Almerich Silla, J.M.; Canorea Diaz, E.; Cortes Martinicorena, F.J.; Exposito Delgado, A.J.; Gomez Santos, G.; Hidalgo Olivares, G.; Lamas Oliveira, M.; Martinez, Y.; Monger Tapies, M. Encuesta de Salud Oral en España 2020. RCOE 2020, 25, 1–29. Available online: https://rcoe.es/articulo/115/encuesta-de-salud-oral-en-espaa-2020 (accessed on 1 January 2021).
- Gerritsen, A.E.; Allen, P.F.; Witter, D.J.; Bronkhorst, E.M.; Creugers, N.H. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Qual. Life Outcomes 2010, 8, 126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The McGill consensus statement on overdentures. Quintessence Int. 2003, 34, 78–79.
- Thomason, J.M.; Feine, J.; Exley, C.; Moynihan, P.; Muller, F.; Naert, I.; Ellis, J.; Barclay, C.; Butterworth, C.; Scott, B.; et al. Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patients—The York Consensus Statement. Br. Dent. J. 2009, 207, 185–186. [Google Scholar] [CrossRef] [PubMed]
- Brånemark, P.I.; Adell, R.; Breine, U.; Hansson, B.O.; Lindström, J.; Ohlsson, A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand. J. Plast. Reconstr. Surg. 1969, 3, 81–100. [Google Scholar] [CrossRef] [PubMed]
- Laney, W. Glossary of Oral and Maxillofacial Implants. Int. J. Oral Maxillofac. Implant. 2017, 32, Gi-G200. [Google Scholar] [CrossRef]
- Antonelli, A.; Bennardo, F.; Brancaccio, Y.; Barone, S.; Femiano, F.; Nucci, L.; Minervini, G.; Fortunato, L.; Attanasio, F.; Giudice, A. Can Bone Compaction Improve Primary Implant Stability? An In Vitro Comparative Study with Osseodensification Technique. Appl. Sci. 2020, 10, 8623. [Google Scholar] [CrossRef]
- Kim, J.-H.; Lim, Y.-J.; Kim, B.; Lee, J. How Do Parameters of Implant Primary Stability Correspond with CT-Evaluated Bone Quality in the Posterior Maxilla? A Correlation Analysis. Materials 2021, 14, 270. [Google Scholar] [CrossRef]
- Kittur, N.; Oak, R.; Dekate, D.; Jadhav, S.; Dhatrak, P. Dental implant stability and its measurements to improve osseointegration at the bone-implant interface: A review. Mater. Today 2020, 43, 1064–1070. [Google Scholar] [CrossRef]
- Gapski, R.; Wang, H.L.; Mascarenhas, P.; Lang, N.P. Critical review of immediate implant loading. Clin. Oral Implant. Res. 2003, 14, 515–527. [Google Scholar] [CrossRef]
- Trisi, P.; Perfetti, G.; Baldoni, E.; Berardi, D.; Colagiovanni, M.; Scogna, G. Implant micromotion is related to peak insertion torque and bone density. Clin. Oral Implant. Res. 2009, 20, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Duyck, J.; Vandamme, K.; Geris, L.; Van Oosterwyck, H.; De Cooman, M.; Vandersloten, J.; Puers, R.; Naert, I. The influence of micro-motion on the tissue differentiation around immediately loaded cylindrical turned titanium implants. Arch. Oral Biol. 2006, 51, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Carter, D.R.; Beaupré, G.S.; Giori, N.J.; Helms, J.A. Mechanobiology of skeletal regeneration. Clin. Orthop. Relat. Res. 1998, 355, S41–S55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romanos, G.E.; Toh, C.G.; Siar, C.H.; Swaminathan, D. Histologic and histomorphometric evaluation of peri-implant bone subjected to immediate loading: An experimental study with Macaca fascicularis. Int. J. Oral Maxillofac. Implant. 2002, 17, 44–51. [Google Scholar]
- Esposito, M.; Grusovin, M.G.; Achille, H.; Coulthard, P.; Worthington, H. Interventions for replacing missing teeth: Different times for loading dental implants. Cochrane Database Syst. Rev. 2009, 28, CD003878. [Google Scholar] [CrossRef]
- Hultin, M.; Davidson, T.; Gynther, G.; Helgesson, G.; Jemt, T.; Lekholm, U.; Nilner, K.; Nordenram, G.; Norlund, A.; Rohlin, M.; et al. Oral rehabilitation of tooth loss: A systematic review of quantitative studies of OHRQoL. Int. J. Prosthodont. 2012, 25, 543–552. [Google Scholar]
- Thomason, J.M.; Kelly, S.A.M.; Bendkowski, A.; Ellis, J.S. Two implant retained overdentures––A review of the literature supporting the McGill and York consensus statements. J. Dent. 2012, 40, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Montero, J.; Dib, A.; Guadilla, Y.; Blanco, L.; Flores, J.; Gómez-Polo, C. Responsiveness of the different methods for assessing the short-term within-subject change in masticatory function after conventional prosthetic treatments. J. Prosthet. Dent. 2020, 123, 602–610. [Google Scholar] [CrossRef]
- Cannizzaro, G.; Leone, M.; Esposito, M. Immediate versus early loading of two implants placed with a flapless technique supporting mandibular bar-retained overdentures: A single-blinded, randomised controlled clinical trial. Eur. J. Oral Implant. 2008, 1, 20467642. [Google Scholar]
- Alfadda, S.A.; Attard, N.J.; David, L.A. Five-year clinical results of immediately loaded dental implants using mandibular overdentures. Int. J. Prosthodont. 2009, 22, 368–373. [Google Scholar]
- Al-Ansari, A. No difference between splinted and unsplinted implants to support overdentures. Evid. Based Dent. 2012, 13, 54–55. [Google Scholar] [CrossRef]
- Fernandez-Estevan, L.; Montero, J.; Otaolaurruchi, E.; Ruiz, M. Interventions to Maintain Locator-Retained Mandibular Overdentures on Both External Hex and Internal Connection Implants: A Retrospective Study. Int. J. Oral Maxillofac. Implant. 2018, 33, 838–846. [Google Scholar] [CrossRef] [PubMed]
- Montero, J.; Macedo, C.; López-Valverde, A.; Bravo, M. Validation of the Oral Health Impact Profile (OHIP-20sp) for edentulous Spanish patients. Med. Oral Patol. Oral Cir. Bucal. 2012, 17, e469. [Google Scholar] [CrossRef] [Green Version]
- Montero, J.; Leiva, L.A.; Martín-Quintero, I.; Rodríguez, R.B. Chewing Performance Calculator: An interactive clinical method for quantifying masticatory performance. J. Prosthet. Dent. 2021, 125, 82–88. [Google Scholar] [CrossRef]
- Leake, J.L. An Index of Chewing Ability. J. Public Health Dent. 1990, 50, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Lekholm, U.; Zarb, G.A. Patient selection and preparation. In Tissue Integrated Prostheses: Osseointegration in Clinical Dentistry; Branemark, P.I., Zarb, G.A., Albrektsson, T., Eds.; Quintessence: Chicago, IL, USA, 1985; pp. 199–209. [Google Scholar]
- Ainamo, J.; Bay, I. Problems and proposals for recording gingivitis and plaque. Int. Dent. J. 1975, 25, 229–235. [Google Scholar] [PubMed]
- Montero, J.; Bravo, M.; Albaladejo, A. Validation of two complementary oral-health related quality of life indicators (OIDP and OSS 0-10) in two qualitatively distinct samples of the Spanish population. Health Qual. Life Outcomes 2008, 6, 101. [Google Scholar] [CrossRef] [Green Version]
- Locker, D.; Jokovic, A.; Clarke, M. Assessing the responsiveness of measures of oral health-related quality of life. Community Dent. Oral Epidemiol. 2004, 32, 10–18. [Google Scholar] [CrossRef]
- Schwartz, C.E.; Sprangers, M.A. Methodological approaches for assessing response shift in longitudinal health-related quality-of-life research. Soc. Sci. Med. 1999, 48, 1531–1548. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis of the Behavioural Sciences, 2nd ed.; Lawrence Erlbaum: Hillsdadle, NJ, USA, 1988. [Google Scholar]
- Doig, G.S.; Simpson, F. Randomization and allocation concealment: A practical guide for researchers. J. Crit. Care 2005, 20, 187–191. [Google Scholar] [CrossRef]
- Harris, D.; Höfer, S.; O’Boyle, C.A.; Sheridan, S.; Marley, J.; Benington, I.C.; Clifford, T.; Houston, F.; O’Connell, B. A comparison of implant-retained mandibular overdentures and conventional dentures on quality of life in edentulous patients: A randomized, prospective, within-subject controlled clinical trial. Clin. Oral Implant. Res. 2013, 24, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, B. Standard of care for the edentulous mandible: A systematic review. J. Prosthet. Dent. 2006, 95, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Iwaki, M.; Kanazawa, M.; Sato, D.; Miyayasu, A.; Minakuchi, S. Masticatory Function of Immediately Loaded Two-Implant Mandibular Overdentures: A 5-year Prospective Study. Int. J. Oral Maxillofac. Implant. 2019, 34, 1434–1440. [Google Scholar] [CrossRef] [PubMed]
- Baca, E.; Yengin, E.; Gökçen-Röhlig, B.; Sato, S. In vivo evaluation of occlusalcontact area and maximum bite force in patients with various types of implant-supported prostheses. Acta Odontol Scand. 2013, 71, 1181–1187. [Google Scholar] [CrossRef]
- Suzuki, T.; Kumagai, H.; Yoshitomi, N.; McGlumphy, E. Occlusal contacts of edentulous patients with mandibular hybrid dentures opposing maxillary complete dentures. Int. J. Oral Maxillofac. Implant. 1999, 14, 504–509. [Google Scholar]
- Shiga, H.; Komino, M.; Uesugi, H.; Sano, M.; Yokoyama, M.; Nakajima, K.; Ishikawa, A. Comparison of two dental prescale systems used for the measurement of occlusal force. Odontology 2020, 108, 676–680. [Google Scholar] [CrossRef]
- Van der Bilt, A.; Burgers, M.; van Kampen, F.M.; Cune, M.S. Mandibular implant-supported overdentures and oral function. Clin. Oral Implant. Res. 2010, 21, 1209–1213. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Kumagai, H.; Watanabe, T.; Uchida, T.; Nagao, M. Evaluation of complete denture occlusal contacts using pressure-sensitive sheets. Int. J. Prosthodont. 1997, 10, 386–391. [Google Scholar] [PubMed]
- Komagamine, Y.; Kanazawa, M.; Sato, D.; Minakuchi, S. A preliminary comparison of masticatory performances between immediately loaded and conventionally loaded mandibular two-implant overdentures with magnetic attachments. Clin. Implant. Dent. Relat. Res. 2019, 21, 130–137. [Google Scholar] [CrossRef]
- Von der Gracht, I.; Derks, A.; Haselhuhn, K.; Wolfart, S. EMG correlations of edentulous patients with implant overdentures and fixed dental prostheses compared to conventional complete dentures and dentates: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2017, 28, 765–773. [Google Scholar] [CrossRef]
- Giannakopoulos, N.N.; Corteville, F.; Kappel, S.; Rammelsberg, P.; Schindler, H.J.; Eberhard, L. Functional adaptation of the masticatory system to implant-supported mandibular overdentures. Clin. Oral Implant. Res. 2017, 28, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Van der Bilt, A.; van Kampen, F.M.; Cune, M.S. Masticatory function with mandibular implant-supported overdentures fitted with different attachment types. Eur. J. Oral Sci. 2006, 114, 191–196. [Google Scholar] [CrossRef]
- Da Silva, R.J.; Issa, J.P.; Semprini, M.; da Silva, C.H.; de Vasconcelos, P.B.; Celino, C.A.; Siéssere, S.; Regalo, S.C. Clinical feasibility of mandibular implant overdenture retainers submitted to immediate load. Gerodontology 2011, 28, 227–232. [Google Scholar] [CrossRef]
- Boven, G.C.; Raghoebar, G.M.; Vissink, A.; Meijer, H.J. Improving masticatory performance, bite force, nutritional state and patient’s satisfaction with implant overdentures: A systematic review of the literature. J. Oral Rehabil. 2015, 42, 220–233. [Google Scholar] [CrossRef]
- Müller, F.; Duvernay, E.; Loup, A.; Vazquez, L.; Herrmann, F.R.; Schimmel, M. Implant-supported mandibular overdentures in very old adults: A randomized controlled trial. J. Dent. Res. 2013, 92 (Suppl. S12), 154S–160S. [Google Scholar] [CrossRef]
- Schuster, A.J.; Marcello-Machado, R.M.; Bielemann, A.M.; Possebon, A.P.D.R.; Chagas, O.L., Jr.; Faot, F. Immediate vs conventional loading of Facility-Equator system in mandibular overdenture wearers: 1-year RCT with clinical, biological, and functional evaluation. Clin. Implant. Dent. Relat. Res. 2020, 22, 270–280. [Google Scholar] [CrossRef]
- Jofre, J.; Castiglioni, X.; Lobos, C.A. Influence of minimally invasive implant-retained overdenture on patients’ quality of life: A randomized clinical trial. Clin. Oral Implant. Res. 2013, 24, 1173–1177. [Google Scholar] [CrossRef]
- Jabbour, Z.; Emami, E.; de Grandmont, P.; Rompre, P.H.; Feine, J.S. Is oral health-related quality of life stable following rehabilitation with mandibular two-implant overdentures? Clin. Oral Implant. Res. 2012, 23, 1205–1209. [Google Scholar] [CrossRef] [PubMed]
- Sivaramakrishnan, G.; Sridharan, K. Comparison of implant supported mandibular overdentures and conventional dentures on quality of life: A systematic review and meta-analysis of randomized controlled studies. Aust. Dent. J. 2016, 61, 482–488. [Google Scholar] [CrossRef]
- Emami, E.; Heydecke, G.; Rompré, P.H.; de Grandmont, P.; Feine, J.S. Impact of implant support for mandibular dentures on satisfaction, oral and general health-related quality of life: A meta-analysis of randomized-controlled trials. Clin. Oral Implant. Res. 2009, 20, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Allen, P.F.; O’Sullivan, M.; Locker, D. Determining the minimally important difference for the Oral Health Impact Profile-20. Eur. J. Oral Sci 2009, 117, 129–134. [Google Scholar] [CrossRef]
- Omura, Y.; Kanazawa, M.; Sato, D.; Kasugai, S.; Minakuchi, S. Comparison of patient-reported outcomes between immediately and conventionally loaded mandibular two-implant overdentures: A prelimiary study. J. Prosthodont. Res. 2016, 60, 185–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| SOCIO-DEMOGRAPHIC | ALL PATIENTS (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | |||
|---|---|---|---|---|---|---|
| Age Interval | n | % | n | % | n | % |
| 50–60 yrs | 6 | 30.0 | 3 | 30.0 | 3 | 30.0 |
| 60–70 yrs | 7 | 35.0 | 3 | 30.0 | 4 | 40.0 |
| >70 yrs | 7 | 35.0 | 4 | 40.0 | 3 | 30.0 |
| Mean | SD | Mean | SD | Mean | SD | |
| Age (average) | 66.3 | 9.1 | 67.6 | 9.6 | 65.0 | 8.9 |
| Gender | n | % | n | % | n | % |
| Female | 10 | 50.0 | 6 | 60.0 | 4 | 40.0 |
| Male | 10 | 50.0 | 4 | 40.0 | 6 | 60.0 |
| Socio-occupational class | n | % | n | % | n | % |
| Low | 15 | 75.0 | 8 | 80.0 | 7 | 70.0 |
| Medium | 5 | 25.0 | 2 | 20.0 | 3 | 30.0 |
| Place of residence | n | % | n | % | n | % |
| Urban | 13 | 65.0 | 6 | 60.0 | 7 | 70.0 |
| Peri-urban | 2 | 10.0 | 1 | 10.0 | 1 | 10.0 |
| Rural | 5 | 25.0 | 3 | 30.0 | 2 | 20.0 |
| CONDUCTUAL | ||||||
| Brushing habits * | n | % | n | % | n | % |
| 2–3 times a day | 8 | 40.0 | 4 | 40.0 | 4 | 40.0 |
| Once a day | 8 | 40.0 | 2 | 20.0 | 6 | 60.0 |
| Less than once a day | 4 | 20.0 | 4 | 40.0 | 0 | 0.0 |
| Smoking habits | n | % | n | % | n | % |
| Non-smoker | 10 | 50.0 | 5 | 50.0 | 5 | 50.0 |
| Current smoker | 5 | 25 | 2 | 20.0 | 3 | 30.0 |
| Past Smoker | 5 | 25 | 3 | 30.0 | 2 | 20.0 |
| Mean | Sd | Mean | SD | Mean | SD | |
| Cigarettes/day among smokers | 14.9 | 15.7 | 12.9 | 19.1 | 4.3 | 5.0 |
| Pattern of dental check-ups | n | % | n | % | n | % |
| regularly | 2 | 10.0 | 0 | 0 | 2 | 20.0 |
| problem-based | 18 | 90.0 | 10 | 100.0 | 8 | 80.0 |
| PROSTHETIC STATUS | ALL PATIENTS (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | |||
|---|---|---|---|---|---|---|
| Denture age (months) | Mean | Sd | Mean | Sd | Mean | Sd |
| Maxillary Denture | 115.7 | 131.3 | 135.5 | 126.7 | 93.7 | 140.3 |
| Mandibular Denture | 97.2 | 113.4 | 107.9 | 94.0 | 86.5 | 134.3 |
| MANDIBULAR DENTURE QUALITY | n | % | n | % | n | % |
| Retention Does the denture dislodge with vertical pulling on central incisors after these are dried with gauze? | ||||||
| No | 4 | 20.0 | 3 | 30.0 | 1 | 10.0 |
| Yes but difficult | 4 | 20.0 | 2 | 20.0 | 2 | 20.0 |
| Yes easily | 12 | 60.0 | 5 | 50.0 | 7 | 70.0 |
| Stability Is there movement induced by index and middle finger pressure on the first molar teeth? | ||||||
| No | 4 | 20.0 | 3 | 30.0 | 1 | 10.0 |
| Yes but difficult | 3 | 15.0 | 1 | 10.0 | 2 | 20.0 |
| Yes easily | 13 | 65.0 | 6 | 60.0 | 7 | 70.0 |
| Interocclusal distance | ||||||
| 1–4 mm | 9 | 55.0 | 4 | 40.0 | 5 | 50.0 |
| <1 OR >4 mm | 11 | 45.0 | 6 | 60.0 | 5 | 50.0 |
| Bibalanced occlusion | ||||||
| adequate | 11 | 45.0 | 6 | 60.0 | 5 | 50.0 |
| poor | 9 | 55.0 | 4 | 40.0 | 5 | 50.0 |
| ALL PATIENTS (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | ||||
|---|---|---|---|---|---|---|
| Bone Quality according to Leckholm & Zarb [24] | ||||||
| n | % | n | % | n | % | |
| Type I | 3 | 15.0 | 2 | 20.0 | 1 | 10.0 |
| Type II | 12 | 60.0 | 5 | 50.0 | 7 | 70.0 |
| Type III | 5 | 25.0 | 3 | 30.0 | 2 | 20.0 |
| Averaged ridge dimensions at canine regions | ||||||
| Mean | SD | Mean | SD | Mean | SD | |
| Length to basal bone | 16.4 | 5.3 | 18.1 | 6.5 | 14.7 | 3.1 |
| Witdth at 3 mm subcrestal | 6.9 | 2.1 | 7.3 | 2.1 | 6.5 | 2.0 |
| Gingival Biotype | n | % | n | % | n | % |
| fine | 10 | 44.0 | 6 | 60.0 | 4 | 40.0 |
| medium | 9 | 44.0 | 3 | 30.0 | 6 | 60.0 |
| thick | 1 | 12.0 | 1 | 10.0 | 0 | 0 |
| Mean | Sd | Mean | Sd | Mean | Sd | |
| Averaged attached gingiva at implant sites | 2.6 | 2.2 | 2.9 | 2.6 | 2.4 | 1.8 |
| Implant Size (n = 40) | ||||||
| Diameter | n | % | n | % | n | % |
| 3.3 mm | 7 | 17.5 | 3 | 15.0 | 4 | 20.0 |
| 3.75 mm | 23 | 57.5 | 13 | 65.0 | 10 | 50.0 |
| 4.2 mm | 10 | 25.0 | 4 | 20.0 | 6 | 30.0 |
| Length | n | % | n | % | n | % |
| 10 mm | 14 | 35.0 | 5 | 25.0 | 9 | 45.0 |
| 11.5 mm | 22 | 55.0 | 13 | 65.0 | 9 | 45.0 |
| 13 mm | 4 | 10.0 | 2 | 10.0 | 2 | 10.0 |
| BASELINE RECORDS | ALL PATIENTS (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | |||
|---|---|---|---|---|---|---|
| FULL ARCH | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) * | 11.7 a | 10.0 | 6.6 a | 5.2 | 16.7 a | 11.4 |
| Average Preasure (MPa) | 9.3 a | 3.8 | 8.4 a | 4.9 | 10.3 a | 2.2 |
| Maximal Preasure (MPa) | 30.3 a | 11.9 | 27.2 a | 15.8 | 33.4 a | 4.9 |
| Occlusal Load (Nw) * | 123.2 a | 90.8 | 74.5 a | 53.6 | 171.9 a | 96.2 |
| ANTERIOR REGION | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) | 5.1 a | 4.7 | 3.2 a | 3.5 | 6.9 a | 5.2 |
| Average Preasure (MPa) | 8.4 a | 3.9 | 7.0 a | 4.3 | 9.9 a | 2.8 |
| Maximal Preasure (MPa) | 23.4 a | 13.2 | 17.6 a | 14.0 | 29.2 a | 9.8 |
| Occlusal Load (Nw) * | 57.4 a | 57.5 | 38.1 a | 44.2 | 76.7 a | 64.8 |
| POST-OPERATIVE RECORDS: NEW COMPLETE DENTURE | ||||||
| FULL ARCH | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) | 16.3 b A | 12.4 | 16.6 b A | 14.8 | 16.0 a A | 9.1 |
| Average Preasure (MPa) | 11.8 a A | 3.6 | 12.3 a A | 4.4 | 10.9 a A | 1.9 |
| Maximal Preasure (MPa) | 35.5 a A | 5.2 | 35.4 a A | 6.0 | 35.5 a A | 4.1 |
| Occlusal Load (Nw) | 186.5 b A | 154.2 | 198.7 b A | 194.2 | 168.2 a A | 74.8 |
| ANTERIOR REGION | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) | 6.5 a A | 7.8 | 6.4 a A | 9.5 | 6.7 a A | 5.1 |
| Average Preasure (MPa) | 10.1 b A | 2.5 | 9.6 b A | 2.2 | 10.8 a A | 2.9 |
| Maximal Preasure (MPa) | 30.1 b A | 8.1 | 28.0 b A | 9.3 | 33.1 a A | 4.9 |
| Occlusal Load (Nw) | 76.4 a A | 100.4 | 79.0 a A | 125.4 | 72.5 a A | 55.0 |
| POST-OPERATIVE RECORDS: IMPLANT-RETAINED OVERDENTURE AFTER TWO MONTHS | ||||||
| FULL ARCH | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) | 21.6 b A | 21.3 | 29.6 b B | 27.9 | 13.6 a A | 6.6 |
| Average Preasure (MPa) | 10.6 b A | 1.7 | 10.3 b A | 1.7 | 10.9 a A | 1.7 |
| Maximal Preasure (MPa) | 35.3 b A | 4.7 | 35.8 b A | 4.6 | 34.7 a A | 5.0 |
| Occlusal Load (Nw) | 241.7 b A | 266.9 | 325.9 b A | 358.5 | 157.6 a A | 83.2 |
| ANTERIOR REGION | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) | 5.6 a A | 7.2 | 6.2 a A | 9.3 | 4.9 a A | 4.7 |
| Average Preasure (MPa) | 10.8 b A | 2.6 | 10.4 b A | 2.6 | 11.1 a A | 2.7 |
| Maximal Preasure (MPa) | 31.2 b A | 6.9 | 30.2 b A | 8.5 | 32.1 a A | 5.2 |
| Occlusal Load (Nw) | 68.7 a A | 93.5 | 78.6 a A | 122.6 | 58.8 a A | 57.8 |
| POST-OPERATIVE RECORDS: IMPLANT-RETAINED OVERDENTURE AFTER SIX MONTHS | ||||||
| FULL ARCH | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) * | 17.6 a A | 12.1 | 27.3 b A | 16.1 | 12.1 a A | 3.9 |
| Average Preasure (MPa) | 14.1 a A | 7.5 | 10.7 a A | 1.2 | 16.1 a A | 9.0 |
| Maximal Preasure (MPa) | 57.4 a A | 68.4 | 37.2 a A | 3.8 | 68.9 a A | 85.9 |
| Occlusal Load (Nw) * | 205.2 a A | 142.0 | 311.3 b A | 196.9 | 144.6 a A | 49.4 |
| ANTERIOR REGION | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) | 6.9 a A | 6.3 | 9.0 a A | 9.5 | 5.6 a A | 4.2 |
| Average Preasure (MPa) | 12.9 a A | 5.3 | 10.3 a A | 1.1 | 14.3 a A | 6.3 |
| Maximal Preasure (MPa) | 32.7 a A | 5.7 | 34.2 b B | 6.9 | 31.8 a A | 5.3 |
| Occlusal Load (Nw) | 70.2 a A | 75.6 | 101.0 a A | 109.7 | 52.6 a A | 50.2 |
| POST-OPERATIVE RECORDS: IMPLANT-RETAINED OVERDENTURE AFTER ONE YEAR | ||||||
| FULL ARCH | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) | 26.1 b B | 15.7 | 26.3 b B | 13.0 | 25.8 b B | 18.7 |
| Average Preasure (MPa) | 12.1 b A | 3.4 | 11.9 b A | 3.1 | 12.4 a A | 3.9 |
| Maximal Preasure (MPa) | 36.2 b A | 5.3 | 35.8 b A | 4.6 | 36.5 a A | 6.1 |
| Occlusal Load (Nw) | 292.7 b B | 163.2 | 296.4 b B | 111.1 | 288.9 b B | 209.4 |
| ANTERIOR REGION | Mean | SD | Mean | SD | Mean | SD |
| Contact Area (mm) | 9.4 b A | 7.6 | 8.2 b A | 7.8 | 10.6 b B | 7.5 |
| Average Preasure (MPa) | 10.5 b A | 1.9 | 10.2 b A | 1.5 | 10.7 a A | 2.4 |
| Maximal Preasure (MPa) | 32.1 b A | 6.4 | 31.3 b A | 3.3 | 32.9 a A | 8.7 |
| Occlusal Load (Nw) | 105.3 b A | 83.2 | 88.4 b A | 81.6 | 122.2 b B | 85.5 |
| EMG at Maximal Force (μv) | ALL PATIENTS (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | |||
|---|---|---|---|---|---|---|
| BASELINE | Mean | SD | Mean | SD | Mean | SD |
| Masseter right | 14.2 a | 14.0 | 12.8 a | 10.3 | 15.5 a | 17.4 |
| Masseter left | 10.7 a | 9.5 | 10.1 a | 8.8 | 11.3 a | 10.5 |
| Temporal right | 18.6 a | 20.8 | 12.5 a | 11.9 | 24.6 a | 26.4 |
| Temporal left | 18.9 a | 22.5 | 19.7 a | 23.5 | 18.1 a | 22.7 |
| NEW COMPLETE DENTURE | ||||||
| Masseter right | 16.4 a A | 14.9 | 12.5 a A | 9.6 | 19.9 a A | 18.3 |
| Masseter left | 11.9 a A | 9.8 | 11.4 a A | 10.1 | 12.3 a A | 10.0 |
| Temporal right * | 21.5 a A | 17.7 | 13.6 a A | 9.5 | 29.4 a A | 20.9 |
| Temporal left | 21.3 a A | 23.7 | 21.8 a A | 24.6 | 20.9 a A | 24.4 |
| OVERDENTURE TWO MONTHS | ||||||
| Masseter right | 13.9 a A | 8.3 | 13.0 a A | 5.8 | 15.0 a A | 10.8 |
| Masseter left * | 9.7 a A | 8.6 | 12.7 a A | 10.7 | 6.3 a B | 3.8 |
| Temporal right | 22.5 a A | 16.5 | 18.9 a A | 10.4 | 26.5 a A | 21.6 |
| Temporal left | 16.5 a B | 14.4 | 16.0 a A | 11.6 | 17.0 a A | 17.8 |
| OVERDENTURE SIX MONTHS | ||||||
| Masseter right | 23.3 b A | 21.9 | 21.1 a A | 19.4 | 26.0 a A | 25.9 |
| Masseter left | 22.1 b B | 20.4 | 25.5 b B | 23.2 | 17.9 a A | 16.8 |
| Temporal right | 33.9 b B | 29.4 | 24.0 b B | 17.5 | 46.3 a A | 37.3 |
| Temporal left | 28.5 a A | 31.0 | 26.3 b A | 24.4 | 31.3 a A | 39.3 |
| OVERDENTURE ONE YEAR | ||||||
| Masseter right | 23.5 b A | 20.2 | 28.1 b B | 20.3 | 18.4 a A | 19.8 |
| Masseter left | 20.0 b A | 14.8 | 22.9 b B | 16.4 | 16.8 b A | 13.0 |
| Temporal right | 26.8 b A | 16.1 | 22.5 b A | 15.9 | 31.7 a A | 15.7 |
| Temporal left | 26.2 b A | 19.9 | 25.9 a A | 23.2 | 26.4 a A | 16.9 |
| ALL PATIENTS | CARROT | SALADS | MEAT | VEGETABLES | APPLE | Number of Foods Easily Chewed | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BASELINE a | n | % | n | % | n | % | n | % | n | % | Mean | SD |
| Easy | 2 | 10.0 | 1 | 5.0 | 1 | 5.0 | 9 | 45.0 | 0 | 0.0 | 0.7 a | 0.8 |
| A bit difficult | 2 | 10.0 | 6 | 30.0 | 5 | 25.0 | 4 | 20.0 | 3 | 15.0 | ||
| Very difficult | 16 | 80.0 | 13 | 65.0 | 14 | 70.0 | 7 | 35.0 | 17 | 85.0 | ||
| Two months after new denture bA | ||||||||||||
| Easy | 3 | 15.0 | 4 | 20.0 | 4 | 20.0 | 14 | 70.0 | 0 | 0.0 | 1.3 bA | 1.0 |
| A bit difficult | 4 | 20.0 | 9 | 45.0 | 8 | 40.0 | 3 | 15.0 | 5 | 25.0 | ||
| Very difficult | 13 | 65.0 | 7 | 35.0 | 8 | 40.0 | 3 | 15.0 | 15 | 75.0 | ||
| SIX months after overdenture bB | ||||||||||||
| Easy | 7 | 35.0 | 12 | 60.0 | 11 | 55.0 | 15 | 75.0 | 5 | 25.0 | 2.5 bB | 2.0 |
| A bit difficult | 8 | 40.0 | 4 | 20.0 | 5 | 25.0 | 3 | 15.0 | 9 | 45.0 | ||
| Very difficult | 5 | 25.0 | 4 | 20.0 | 4 | 20.0 | 2 | 10.0 | 6 | 30.0 | ||
| Twelve months after overdenture bB | ||||||||||||
| Easy | 11 | 55.0 | 17 | 85.0 | 15 | 75.0 | 17 | 85.0 | 7 | 35.0 | 3.4 bB | 1.8 |
| A bit difficult | 6 | 30.0 | 1 | 5.0 | 3 | 15.0 | 1 | 5.0 | 9 | 45.0 | ||
| Very difficult | 3 | 15.0 | 2 | 10.0 | 2 | 10.0 | 2 | 10.0 | 4 | 20.0 | ||
| IMMEDIATE LOADING GROUP | ||||||||||||
| BASELINE a | n | % | n | % | n | % | n | % | n | % | Mean | SD |
| Easy | 1 | 10.0 | 1 | 10.0 | 0 | 0.0 | 5 | 50.0 | 0 | 0.0 | 0.7 a | 0.8 |
| A bit difficult | 1 | 10.0 | 3 | 30.0 | 2 | 20.0 | 2 | 20.0 | 1 | 10.0 | ||
| Very difficult | 8 | 80.0 | 6 | 60.0 | 8 | 80.0 | 3 | 30.0 | 9 | 90.0 | ||
| Two months after new denture bA | ||||||||||||
| Easy | 1 | 10.0 | 2 | 20.0 | 1 | 10.0 | 7 | 70.0 | 0 | 0.0 | 1.1 aA | 0.9 |
| A bit difficult | 2 | 20.0 | 5 | 50.0 | 5 | 50.0 | 2 | 20.0 | 2 | 20.0 | ||
| Very difficult | 7 | 70.0 | 3 | 30.0 | 4 | 40.0 | 1 | 10.0 | 8 | 80.0 | ||
| Six months after overdenture bB | ||||||||||||
| Easy | 5 | 50.0 | 8 | 80.0 | 6 | 60.0 | 9 | 90.0 | 4 | 40.0 | 3.2 bB | 1.8 |
| A bit difficult | 4 | 40.0 | 1 | 10.0 | 3 | 30.0 | 1 | 10.0 | 5 | 50.0 | ||
| Very difficult | 1 | 10.0 | 1 | 10.0 | 1 | 10.0 | 0 | 0.0 | 1 | 10.0 | ||
| Twelve months after overdenture * bB | ||||||||||||
| Easy | 7 | 70.0 | 10 | 100.0 | 9 | 90.0 | 10 | 100.0 | 6 | 60.0 | 4.2 bB | 1.1 |
| A bit difficult | 3 | 30.0 | 0 | 0.0 | 1 | 10.0 | 0 | 0.0 | 4 | 40.0 | ||
| Very difficult | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||
| CONVENTIONAL LOADING GROUP | ||||||||||||
| BASELINE a | n | % | n | % | n | % | n | % | n | % | Mean | SD |
| Easy | 1 | 10.0 | 0 | 0.0 | 1 | 10.0 | 4 | 40.0 | 0 | 0.0 | 0.6 a | 0.7 |
| A bit difficult | 1 | 10.0 | 3 | 30.0 | 3 | 30.0 | 2 | 20.0 | 2 | 20.0 | ||
| Very difficult | 8 | 80.0 | 7 | 70.0 | 6 | 60.0 | 4 | 40.0 | 8 | 80.0 | ||
| Two months after new denture bA | ||||||||||||
| Easy | 2 | 20.0 | 2 | 20.0 | 3 | 30.0 | 7 | 70.0 | 0 | 0.0 | 1.4 bA | 1.2 |
| A bit difficult | 2 | 20.0 | 4 | 40.0 | 3 | 30.0 | 1 | 10.0 | 3 | 30.0 | ||
| Very difficult | 6 | 60.0 | 4 | 40.0 | 4 | 40.0 | 2 | 20.0 | 7 | 70.0 | ||
| Six months after overdenture bA | ||||||||||||
| Easy | 2 | 20.0 | 4 | 40.0 | 5 | 50.0 | 6 | 60.0 | 1 | 10.0 | 1.8 bA | 1.9 |
| A bit difficult | 4 | 40.0 | 3 | 30.0 | 2 | 20.0 | 2 | 20.0 | 4 | 40.0 | ||
| Very difficult | 4 | 40.0 | 3 | 30.0 | 3 | 30.0 | 2 | 20.0 | 5 | 50.0 | ||
| Twelve months after overdenture * bB | ||||||||||||
| Easy | 4 | 40.0 | 7 | 70.0 | 6 | 60.0 | 7 | 70.0 | 1 | 10.0 | 2.5 bB | 1.9 |
| A bit difficult | 3 | 30.0 | 1 | 10.0 | 2 | 20.0 | 1 | 10.0 | 5 | 50.0 | ||
| Very difficult | 3 | 30.0 | 2 | 20.0 | 2 | 20.0 | 2 | 20.0 | 4 | 40.0 | ||
| SATISFACTION (0–10 Range) | ALL PATIENTS (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | |||
|---|---|---|---|---|---|---|
| PRE-OPERATIVE | Mean | SD | Mean | SD | Mean | SD |
| Global | 4.1 a | 3.2 | 3.6 a | 4.1 | 4.6 a | 2.2 |
| Aesthetic | 5.1 a | 2.8 | 5.1 a | 3.8 | 5.0 a | 1.6 |
| Chewing | 3.4 a | 2.7 | 3.6 a | 2.7 | 3.1 a | 2.8 |
| After New Dentures | Mean | SD | Mean | SD | Mean | SD |
| Global | 7.3 bA | 2.5 | 7.8 bA | 3.0 | 6.8 bA | 1.9 |
| Aesthetic * | 7.9 bA | 1.9 | 8.7 bA | 1.4 | 7.1 bA | 2.0 |
| Chewing | 6.5 bA | 2.1 | 6.6 bA | 2.1 | 6.4 bA | 2.3 |
| After Overdentures two months | Mean | SD | Mean | SD | Mean | SD |
| Global | 7.7 bA | 2.2 | 8.0 bA | 2.5 | 7.3 bA | 2.0 |
| Aesthetic * | 8.6 bB | 1.5 | 9.3 bB | 1.1 | 7.9 bA | 1.5 |
| Chewing | 7.0 bA | 2.2 | 7.1 bA | 2.4 | 6.9 bA | 2.4 |
| After Overdentures six months | Mean | SD | Mean | SD | Mean | SD |
| Global | 8.5 bB | 1.6 | 8.9 bA | 1.2 | 8.1 bB | 2.0 |
| Aesthetic * | 8.7 bB | 1.3 | 9.4 bB | 1.0 | 8.1 bA | 1.2 |
| Chewing | 7.8 bB | 2.1 | 8.2 bB | 1.7 | 7.4 bA | 2.5 |
| After Overdentures one year | Mean | SD | Mean | SD | Mean | SD |
| Global | 8.5 bB | 1.4 | 8.5 bA | 1.6 | 8.5 bB | 1.3 |
| Aesthetic | 9.0 bB | 1.1 | 9.4 bA | 0.7 | 8.6 bB | 1.3 |
| Chewing | 8.0 bB | 1.9 | 8.1 bA | 2.3 | 8.0 bB | 1.6 |
| ORAL HEALTH-RELATED QUALITY OF LIFE OHIP-20 | ALL PATIENTS (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | |||
|---|---|---|---|---|---|---|
| PRE-OPERATIVE SCORES | Mean | SD | Mean | SD | Mean | SD |
| Functional limitation | 2.6 a | 0.8 | 2.7 a | 0.5 | 2.4 a | 1.0 |
| Pain | 2.8 a | 1.1 | 2.8 a | 1.0 | 2.7 a | 1.3 |
| Psychological Discomfort | 1.6 a | 0.7 | 1.3 a | 0.7 | 1.8 a | 0.6 |
| Physical Disability | 3.3 a | 1.4 | 3.5 a | 1.1 | 3.0 a | 1.6 |
| Psychological Disability | 1.4 a | 0.9 | 1.1 a | 0.9 | 1.6 a | 0.8 |
| Social Disability | 1.4 a | 1.5 | 1.3 a | 1.4 | 1.5 a | 1.6 |
| Handicap | 0.9 a | 1.0 | 0.7 a | 1.0 | 1.0 a | 1.1 |
| TOTAL | 13.7 a | 5.1 | 13.4 a | 5.0 | 14.0 a | 5.4 |
| NEW DENTURES SCORES | Mean | SD | Mean | SD | Mean | SD |
| Functional limitation | 2.0 b A | 0.8 | 2.1 b A | 0.6 | 1.9 a A | 1.0 |
| Pain | 1.8 b A | 1.3 | 1.8 b A | 1.6 | 1.7 b A | 1.2 |
| Psychological Discomfort | 0.9 b A | 0.8 | 0.8 b A | 0.8 | 0.9 b A | 0.9 |
| Physical Disability | 2.1 b A | 1.6 | 1.6 b A | 1.7 | 2.6 a A | 1.5 |
| Psychological Disability | 0.5 b A | 0.8 | 0.6 a A | 1.0 | 0.3 b A | 0.7 |
| Social Disability | 0.6 b A | 1.2 | 0.9 a A | 1.5 | 0.2 b A | 0.6 |
| Handicap | 0.4 a A | 0.8 | 0.5 a A | 0.9 | 0.2 a A | 0.6 |
| TOTAL | 8.1 b A | 5.2 | 8.3 b A | 6.5 | 7.8 b A | 3.9 |
| OVERDENTURES SCORES | Mean | SD | Mean | SD | Mean | SD |
| Functional limitation | 1.0 b B | 1.2 | 1.1 b B | 1.1 | 0.9 b B | 1.3 |
| Pain | 0.6 b B | 0.9 | 0.5 b B | 1.0 | 0.6 b B | 0.8 |
| Psychological Discomfort | 0.5 b A | 0.8 | 0.2 b B | 0.4 | 0.7 b A | 1.0 |
| Physical Disability | 0.8 b B | 1.3 | 0.6 b A | 1.3 | 0.9 b B | 1.3 |
| Psychological Disability | 0.2 b A | 0.5 | 0.1 b A | 0.3 | 0.3 b A | 0.7 |
| Social Disability | 0.1 b B | 0.5 | 0.2 b A | 0.6 | 0.0 b A | 0.0 |
| Handicap | 0.2 b A | 0.5 | 0.2 a A | 0.6 | 0.1 b A | 0.3 |
| TOTAL | 3.2 b B | 4.1 | 2.9 b B | 4.7 | 3.5 b B | 3.6 |
| CHANGES IN ORAL HEALTH-RELATED QUALITY OF LIFE | ALL PATIENTS (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | |||
|---|---|---|---|---|---|---|
| AFTER NEW DENTURES | Mean | SD | Mean | SD | Mean | SD |
| Functional limitation | 0.5 a | 0.7 | 0.6 a | 0.5 | 0.4 a | 0.8 |
| Pain * | 0.6 a | 1.6 | 1.2 a | 1.1 | 0.0 a | 1.8 |
| Psychological Discomfort | 0.2 a | 1.1 | 0.4 a | 1.1 | −0.1 a | 1.2 |
| Physical Disability | 0.2 a | 2.4 | 0.9 a | 2.6 | −0.6 a | 2.0 |
| Psychological Disability | 0.2 a | 1.2 | 0.5 a | 1.3 | −0.1 a | 1.0 |
| Social Disability | 0.3 a | 1.5 | 0.5 a | 2.0 | 0.0 a | 0.9 |
| Handicap | 0.3 a | 1.0 | 0.6 a | 1.1 | 0.0 a | 0.9 |
| TOTAL | 2.2 a | 7.7 | 4.7 a | 7.7 | −0.4 a | 7.2 |
| GLOBAL EFFECT SIZE φ | 0.4 a | 1.3 | 0.8 a | 1.2 | 0.1 a | 1.2 |
| AFTER OVERDENTURES | Mean | SD | Mean | SD | Mean | SD |
| Functional limitation | 1.6 b | 1.5 | 1.6 b | 1.2 | 1.5 b | 1.9 |
| Pain | 2.9 b | 1.8 | 3.0 b | 1.5 | 2.7 b | 2.1 |
| Psychological Discomfort | 1.0 b | 1.2 | 1.3 b | 0.8 | 0.7 a | 1.4 |
| Physical Disability | 2.3 b | 2.1 | 3.0 b | 1.6 | 1.5 b | 2.3 |
| Psychological Disability * | 0.9 b | 1.0 | 1.5 b | 0.9 | 0.3 b | 0.7 |
| Social Disability | 1.4 b | 1.4 | 1.7 b | 1.4 | 1.0 b | 1.4 |
| Handicap * | 0.6 a | 0.9 | 1.1 a | 1.0 | 0.1 a | 0.3 |
| TOTAL | 10.5 b | 7.8 | 13.2 b | 6.8 | 7.8 b | 8.2 |
| GLOBAL EFFECT SIZE φ | 1.7 b | 1.2 | 2.1 b | 1.1 | 1.2 b | 1.3 |
| EFFECT OF NEW DENTURES | Much Worse | Worse | Equal | Better | Much Better |
|---|---|---|---|---|---|
| ALL PATIENTS (n = 20) | n(%) | n(%) | n(%) | n(%) | n(%) |
| Pronouncing words | 0(0.0) | 0(0.0) | 6(30.0) | 11(55.0) | 3(15.0) |
| Taste and smell | 0(0.0) | 0(0.0) | 12(60.0) | 8(40.0) | 0(0.0) |
| Painful aching in the mouth | 0(0.0) | 2(10.0) | 8(40.0) | 8(40.0) | 2(10.0) |
| Oral hygiene | 0(0.0) | 0(0.0) | 9(45.0) | 7(35.0) | 4(20.0) |
| Chewing Ability | 1(5.0) | 2(10.0) | 0(0.0) | 11(55.0) | 6(30.0) |
| Feeding satisfaction | 1(5.0) | 1(5.0) | 2(10.0) | 8(40.0) | 8(40.0) |
| Mouth comfortability | 0(0.0) | 0(0.0) | 5(25.0) | 8(40.0) | 7(35.0) |
| Appealing Smile | 0(0.0) | 0(0.0) | 5(25.0) | 7(35.0) | 8(40.0) |
| Social relations * | 0(0.0) | 0(0.0) | 8(40.0) | 8(40.0) | 4(20.0) |
| IMMEDIATE LOADING GROUP (n = 10) | n(%) | n(%) | n(%) | n(%) | n(%) |
| Pronouncing words | 0(0.0) | 0(0.0) | 2(20.0) | 6(60.0) | 2(20.0) |
| Taste and smell | 0(0.0) | 0(0.0) | 6(60.0) | 4(40.0) | 0(0.0) |
| Painful aching in the mouth | 0(0.0) | 1(10.0) | 4(40.0) | 4(40.0) | 1(10.0) |
| Oral hygiene | 0(0.0) | 0(0.0) | 4(40.0) | 3(30.0) | 3(30.0) |
| Chewing Ability | 1(10.0) | 1(10.0) | 0(0.0) | 4(40.0) | 4(40.0) |
| Feeding satisfaction | 1(10.0) | 0(0.0) | 1(10.0) | 3(30.0) | 5(50.0) |
| Mouth comfortability | 0(0.0) | 0(0.0) | 1(10.0) | 4(40.0) | 5(50.0) |
| Appealing Smile | 0(0.0) | 0(0.0) | 1(10.0) | 4(40.0) | 5(50.0) |
| Social relations * | 0(0.0) | 0(0.0) | 2(20.0) | 7(70.0) | 1(10.0) |
| CONVENTIONAL LOADING GROUP (n = 10) | n(%) | n(%) | n(%) | n(%) | n(%) |
| Pronouncing words | 0(0.0) | 0(0.0) | 4(40.0) | 5(50.0) | 1(10.0) |
| Taste and smell | 0(0.0) | 0(0.0) | 6(60.0) | 4(40.0) | 0(0.0) |
| Painful aching in the mouth | 0(0.0) | 1(10.0) | 4(40.0) | 4(40.0) | 1(10.0) |
| Oral hygiene | 0(0.0) | 0(0.0) | 5(50.0) | 4(40.0) | 1(10.0) |
| Chewing Ability | 0(0.0) | 1(10.0) | 0(0.0) | 7(70.0) | 2(20.0) |
| Feeding satisfaction | 0(0.0) | 1(10.0) | 1(10.0) | 5(50.0) | 3(30.0) |
| Mouth comfortability | 0(0.0) | 0(0.0) | 4(40.0) | 4(40.0) | 2(20.0) |
| Appealing Smile | 0(0.0) | 0(0.0) | 4(40.0) | 3(30.0) | 3(30.0) |
| Social relations * | 0(0.0) | 0(0.0) | 6(60.0) | 1(10.0) | 3(30.0) |
| EFFECT OF TWO-IMPLANT-RETAINED OVERDENTURES | Much Worse | Worse | Equal | Better | Much Better |
|---|---|---|---|---|---|
| ALL PATIENTS (n = 20) | n(%) | n(%) | n(%) | n(%) | n(%) |
| Pronouncing words | 0(0.0) | 1(5.0) | 6(30.0) | 8(40.0) | 5(25.0) |
| Taste and smell | 0(0.0) | 0(0.0) | 10(50.0) | 8(40.0) | 2(10.0) |
| Painful aching in the mouth | 0(0.0) | 1(5.0) | 4(20.0) | 11(55.0) | 4(20.0) |
| Oral hygiene | 0(0.0) | 0(0.0) | 9(45.0) | 7(35.0) | 4(20.0) |
| Chewing Ability * | 0(0.0) | 1(5.0) | 0(0.0) | 5(25.0) | 14(70.0) |
| Feeding satisfaction * | 0(0.0) | 0(0.0) | 2(10.0) | 5(25.0) | 13(65.0) |
| Mouth comfortability | 0(0.0) | 1(5.0) | 1(5.0) | 8(40.0) | 10(50.0) |
| Appealing Smile | 0(0.0) | 0(0.0) | 6(30.0) | 10(50.0) | 4(20.0) |
| Social relations * | 0(0.0) | 0(0.0) | 9(45.0) | 7(35.0) | 4(20.0) |
| IMMEDIATE LOADING GROUP (n = 10) | n(%) | n(%) | n(%) | n(%) | n(%) |
| Pronouncing words | 0(0.0) | 1(10.0) | 2(20.0) | 3(30.0) | 4(40.0) |
| Taste and smell | 0(0.0) | 0(0.0) | 6(60.0) | 2(20.0) | 2(20.0) |
| Painful aching in the mouth | 0(0.0) | 1(10.0) | 2(20.0) | 5(50.0) | 2(20.0) |
| Oral hygiene | 0(0.0) | 0(0.0) | 3(30.0) | 4(40.0) | 3(30.0) |
| Chewing Ability * | 0(0.0) | 1(10.0) | 0(0.0) | 0(0.0) | 9(90.0) |
| Feeding satisfaction * | 0(0.0) | 0(0.0) | 1(10.0) | 0(0.0) | 9(90.0) |
| Mouth comfortability | 0(0.0) | 1(10.0) | 0(0.0) | 2(20.0) | 7(70.0) |
| Appealing Smile | 0(0.0) | 0(0.0) | 3(30.0) | 5(50.0) | 2(20.0) |
| Social relations * | 0(0.0) | 0(0.0) | 2(20.0) | 5(50.0) | 3(30.0) |
| CONVENTIONAL LOADING GROUP (n = 10) | n(%) | n(%) | n(%) | n(%) | n(%) |
| Pronouncing words | 0(0.0) | 0(0.0) | 4(40.0) | 5(50.0) | 1(10.0) |
| Taste and smell | 0(0.0) | 0(0.0) | 4(40.0) | 6(60.0) | 0(0.0) |
| Painful aching in the mouth | 0(0.0) | 0(0.0) | 2(20.0) | 6(60.0) | 2(20.0) |
| Oral hygiene | 0(0.0) | 0(0.0) | 6(60.0) | 3(30.0) | 1(10.0) |
| Chewing Ability * | 0(0.0) | 0(0.0) | 0(0.0) | 5(50.0) | 5(50.0) |
| Feeding satisfaction * | 0(0.0) | 0(0.0) | 1(10.0) | 5(50.0) | 4(40.0) |
| Mouth comfortability | 0(0.0) | 0(0.0) | 1(10.0) | 6(60.0) | 3(30.0) |
| Appealing Smile | 0(0.0) | 0(0.0) | 3(30.0) | 5(50.0) | 2(20.0) |
| Social relations * | 0(0.0) | 0(0.0) | 7(70.0) | 2(20.0) | 1(10.0) |
| MASTICATORY PERFORMANCE by Mixing Ability Tests https://studio.chewing.app/ | ALL PATIENTS (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | |||
|---|---|---|---|---|---|---|
| PRE-OPERATIVE SCORES | Mean | SD | Mean | SD | Mean | SD |
| 5 cycles | 17.0 a A | 16.4 | 19.9 a A | 17.7 | 13.8 a A | 15.3 |
| 10 cycles | 32.6 a A | 14.3 | 33.5 a A | 13.4 | 31.6 a A | 16.1 |
| 15 cycles | 53.7 a A | 23.2 | 48.2 a A | 23.0 | 59.8 a A | 23.4 |
| After New dentures | Mean | SD | Mean | SD | Mean | SD |
| 5 cycles | 18.6 a A | 14.7 | 22.1 a A | 15.6 | 15.4 a A | 13.8 |
| 10 cycles | 35.3 a A | 20.9 | 38.7 a A | 23.2 | 32.3 a A | 19.3 |
| 15 cycles | 54.1 a A | 20.4 | 54.2 a A | 12.4 | 54.0 a A | 26.3 |
| Two months after overdentures | Mean | SD | Mean | SD | Mean | SD |
| 5 cycles | 19.3 a A | 14.1 | 22.9 a A | 14.2 | 15.6 a A | 13.8 |
| 10 cycles | 36.3 a A | 17.3 | 38.2 a A | 18.3 | 34.4 a A | 17.2 |
| 15 cycles | 54.9 a A | 16.6 | 54.9 a A | 13.6 | 54.8 a A | 20.1 |
| Six months after overdentures | Mean | SD | Mean | SD | Mean | SD |
| 5 cycles | 19.9 a A | 14.1 | 22.9 a A | 14.2 | 16.6 a A | 14.1 |
| 10 cycles | 37.9 a A | 18.3 | 38.7 a A | 16.3 | 37.1 a A | 21.3 |
| 15 cycles | 54.3 a A | 19.2 | 55.6 a A | 17.6 | 52.9 a A | 21.7 |
| One year after overdentures | Mean | SD | Mean | SD | Mean | SD |
| 5 cycles | 24.9 a A | 15.4 | 25.1 a A | 11.3 | 24.8 a A | 18.7 |
| 10 cycles | 35.2 a A | 20.7 | 35.0 a A | 19.6 | 35.4 a A | 22.7 |
| 15 cycles | 54.1 a A | 20.8 | 56.3 a A | 17.5 | 52.4 a A | 24.0 |
| DEPENDENT Predictors | β | Error | T | p-Value | Lower CI95% | Upper CI95% |
|---|---|---|---|---|---|---|
| CHEWING PERFORMANCE 5 cycles a | ||||||
| Bone quality | 15.6 | 3.0 | 5.2 | 0.001 | 8.8 | 22.5 |
| Muscular activity in right Temporalis (μv) | 0.4 | 0.2 | 2.4 | 0.04 | 0.1 | 0.7 |
| NUMBER OF FOODS CHEWED EASILY b | ||||||
| Chewing performance at 15 cycles | 0.05 | 0.01 | 3.6 | 0.002 | 0.02 | 0.08 |
| Cohort (Conventional as reference) | 1.8 | 0.6 | 3.3 | 0.005 | 0.6 | 3.0 |
| GLOBAL SATISFACTION c | ||||||
| Number of biological complications | −1.4 | 0.4 | −3.7 | 0.005 | −0.5 | −2.2 |
| Chewing performance at 5 cycles | 0.04 | 0.02 | 2.5 | 0.03 | 0.00 | 0.08 |
| FINAL IMPACT ON QUALITY OL LIFE d | ||||||
| Number of biological complications | 2.5 | 0.6 | 4.4 | 0.001 | 1.2 | 3.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montero, J.; Dib, A.; Guadilla, Y.; Flores, J.; Pardal-Peláez, B.; Quispe-López, N.; Gómez-Polo, C. Functional and Patient-Centered Treatment Outcomes with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants: A Randomized Clinical Trial. J. Clin. Med. 2021, 10, 3477. https://doi.org/10.3390/jcm10163477
Montero J, Dib A, Guadilla Y, Flores J, Pardal-Peláez B, Quispe-López N, Gómez-Polo C. Functional and Patient-Centered Treatment Outcomes with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants: A Randomized Clinical Trial. Journal of Clinical Medicine. 2021; 10(16):3477. https://doi.org/10.3390/jcm10163477
Chicago/Turabian StyleMontero, Javier, Abraham Dib, Yasmina Guadilla, Javier Flores, Beatriz Pardal-Peláez, Norberto Quispe-López, and Cristina Gómez-Polo. 2021. "Functional and Patient-Centered Treatment Outcomes with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants: A Randomized Clinical Trial" Journal of Clinical Medicine 10, no. 16: 3477. https://doi.org/10.3390/jcm10163477
APA StyleMontero, J., Dib, A., Guadilla, Y., Flores, J., Pardal-Peláez, B., Quispe-López, N., & Gómez-Polo, C. (2021). Functional and Patient-Centered Treatment Outcomes with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants: A Randomized Clinical Trial. Journal of Clinical Medicine, 10(16), 3477. https://doi.org/10.3390/jcm10163477








