Reshaping of Italian Echocardiographic Laboratories Activities during the Second Wave of COVID-19 Pandemic and Expectations for the Post-Pandemic Era
Abstract
:1. Introduction
2. Methods
- General information: date, hospital’s name, department, name of the interviewed physician, and city and region of Italy.
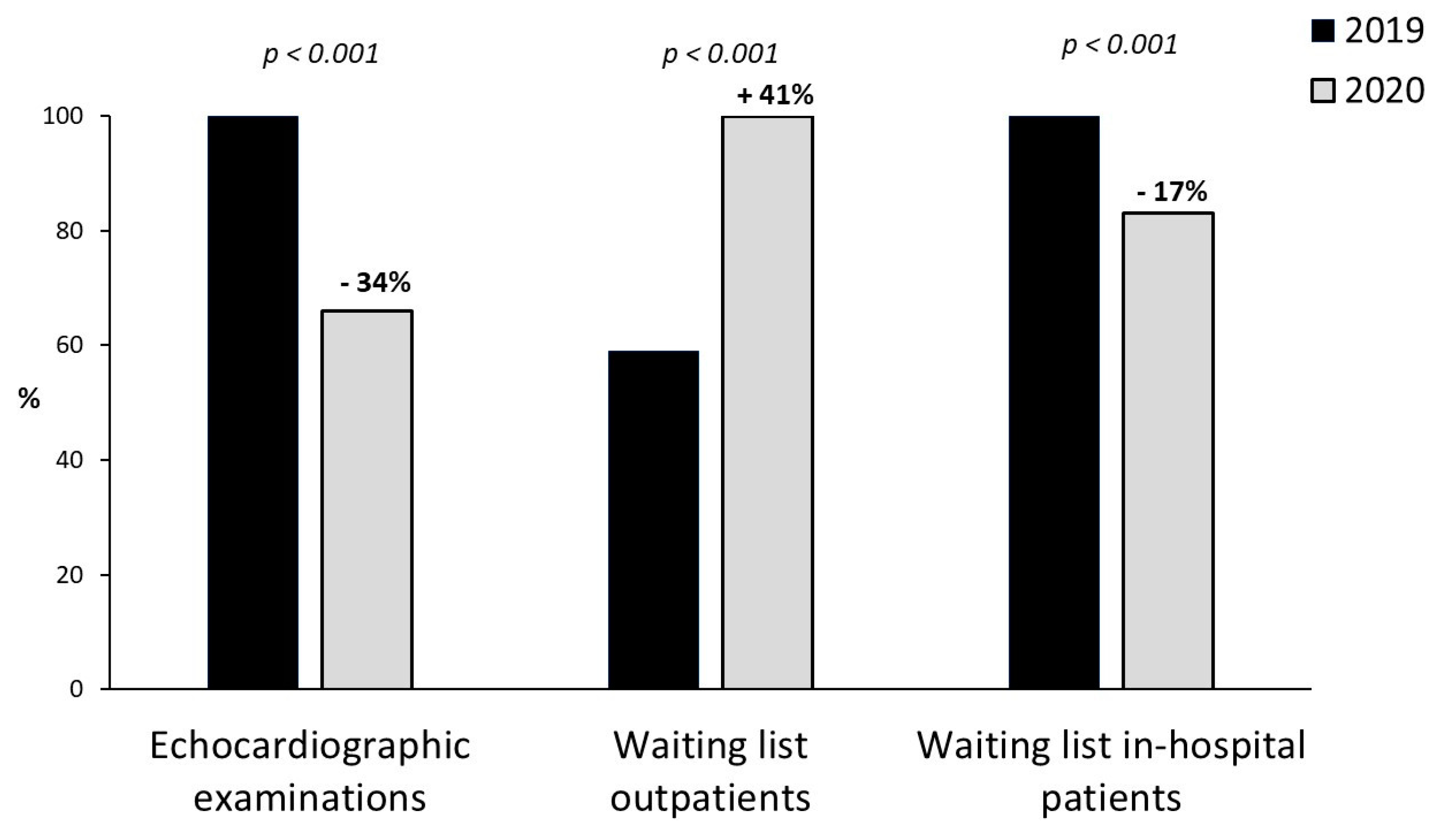
- Hospital activity and outpatient echocardiographic activity during the second wave of the COVID-19 pandemic.
- The number of echocardiographic exams and the duration of waiting in-hospital lists and for outpatients in the two analyzed periods.
- Types of activities organization in the echocardiography laboratory to reduce the operator risk: social distancing in the waiting room, limit to accompanying visitors, wearing of masks, reducing the number of exams, improvement of operators’ self-protection and nasopharyngeal swab required for patients before echocardiographic exams.
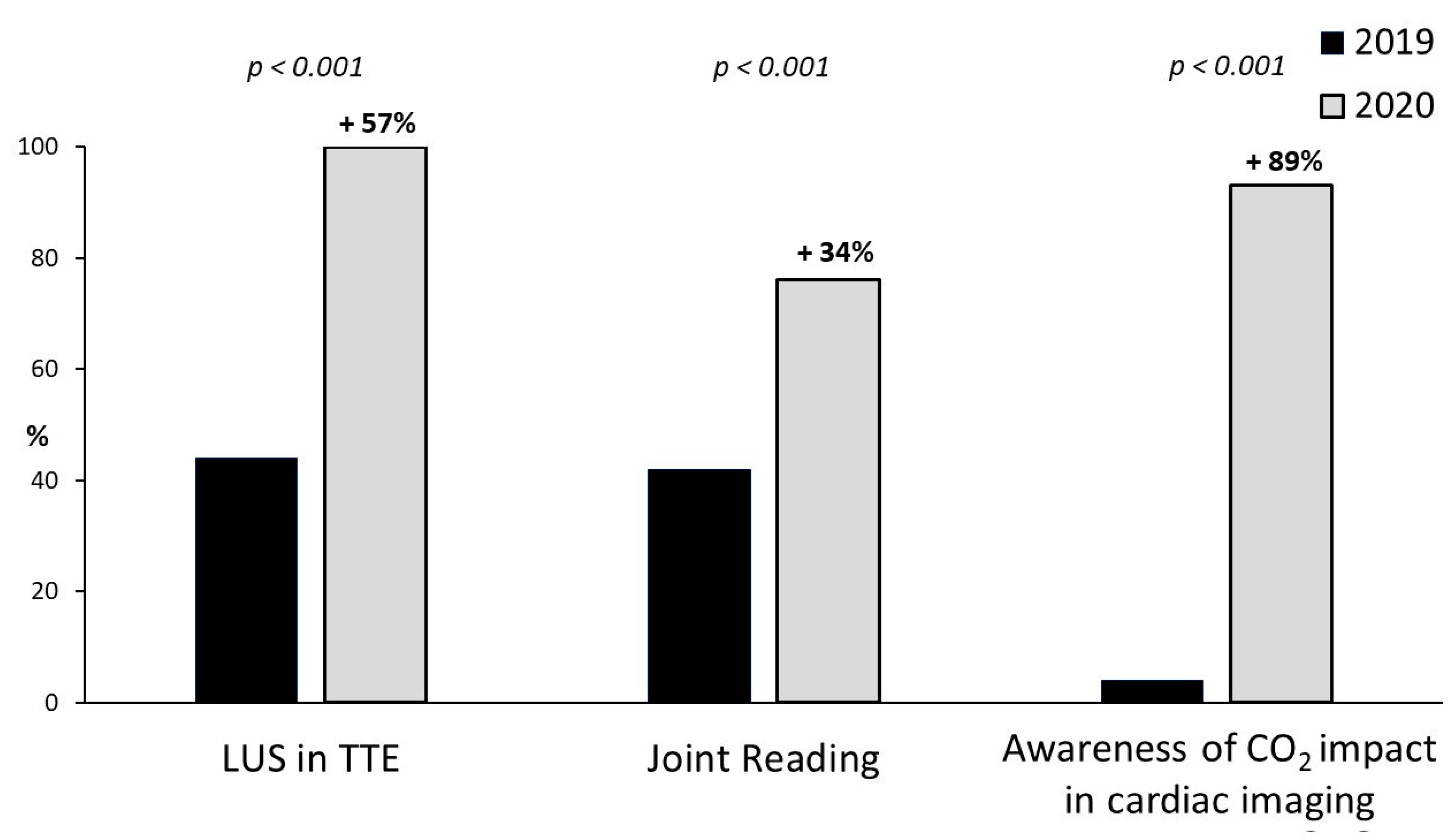
- Usage of point-of-care cardiac ultrasound by cardiologists with a joint reading assessment with other physicians.
- Use of lung ultrasound.
- Modality of analysis of echocardiographic imaging.
- Expectations for the post-COVID era regarding the echocardiographic activity.
- Role of carbon dioxide production by cardiac imaging modalities in decision-making and its importance in the future development of imaging.
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N. Engl, J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef] [PubMed]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef] [PubMed]
- Antonini-Canterin, F.; Pepi, M.; Monte, I. Document addressed to cardiovascular echography operators at the time of COVID-19: A Document by the “Società Italiana di Ecocardiografia e CardioVascular Imaging” Board 2019–2021. J. Cardiovascular Echo. 2020, 30, 2–4. [Google Scholar]
- Ciampi, Q.; Antonini-Canterin, F.; Barbieri, A.; Barchitta, A.; Benedetto, F.; Cresti, A.; Miceli, S.; Monte, I.; Picano, E.; Pepi, M. Remodeling of Activities of Italian Echocardiographic laboratories during COVID-19 Lockdown: The SIECoVId study. J. Cardiovasc. Med. 2021, 22, 600–602. [Google Scholar]
- Picano, E. Where have all myocardial infarctions gone? The answer is blowing in the less polluted wind. Eur. Heart J. 2020, 41, 2146–2147. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; DiCarli, M.F.; Blankstein, R.; Choi, A.D.; Dilsizian, V.; Flachskampf, F.A.; Geske, J.B.; Grayburn, P.A.; Jaffer, F.A.; Kwong, R.Y.; et al. Multimodality Cardiovascular Imaging in the Midst of the COVID-19 Pandemic: Ramping Up Safely to a New Normal. JACC Cardiovasc. Imaging 2020, 13, 1615–1626. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, J.N.; Mitchell, C.; Taub, C.; Kort, S.; Hung, J.; Swaminathan, M.J. ASE Statement on Protection of Patients and Echocardiography Service Providers During the 2019 Novel Coronavirus Outbreak: Endorsed by the American College of Cardiology. J. Am. Soc. Echocardiogr. 2020, 33, 648–653. [Google Scholar] [CrossRef]
- Flórez, J.M.V.; Barrios Alonso, V.; Gofin, C.F. The day after tomorrow: Echocardiography laboratories after the COVID-19 outbreak. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 1057. [Google Scholar] [CrossRef]
- Skulstad, H.; Cosyns, B.; Popescu, B.A.; Galderisi, M.; Salvo, G.D.; Donal, E.; Petersen, S.; Gimelli, A.; Haugaa, K.H.; Muraru, D.; et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J. Cardiovasc. Imaging 2020, 21, 592–598. [Google Scholar] [CrossRef]
- Ward, R.P.; Lee, L.; Ward, T.J.; Lang, R.M. Utilization and Appropriateness of Transthoracic Echocardiography in Response to the COVID-19 Pandemic. J. Am. Soc. Echocardiogr. 2020, 33, 690–691. [Google Scholar] [CrossRef]
- Moynihan, R.; Johansson, M.; Maybee, A.; Lang, E.; Légaré, F. Covid-19: An opportunity to reduce unnecessary healthcare. Recovering health systems can prioritise genuine need. BMJ 2020, 370, m2752. [Google Scholar] [CrossRef]
- Kameda, T.; Mizuma, Y.; Taniguchi, H.; Fujita, M.; Taniguchi, N. Point-of-care lung ultrasound for the assessment of pneumonia: A narrative review in the COVID-19 era. J. Med. Ultrason. 2021, 13, 1–13. [Google Scholar]
- Kirkpatrick, J.N.; Grimm, R.; Johri, A.M.; Kimura, B.J.; Kort, S.; Labovitz, A.J.; Lanspa, M.; Phillip, S.; Raza, S.; Thorson, K.; et al. Recommendations for echocardiography laboratories participating in cardiac point of care cardiac ultrasound (POCUS) and critical care echocardiography training: Report from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2020, 33, 409–422. [Google Scholar] [CrossRef] [PubMed]
- Picano, E.; Scali, M.C.; Ciampi, Q.; Lichtenstein, D. Lung Ultrasound for the Cardiologist. JACC Cardiovasc. Imaging 2018, 11, 1692–1705. [Google Scholar] [CrossRef]
- Barchitta, A.; Pepi, M.; Monte, I.P.; Trocino, G.; Barbieri, A.; Ciampi, Q.; Cresti, A.; Miceli, S.; Petrella, L.; Benedetto, F.; et al. Lung Semiotics Ultrasound in COVID-19 Infection. J. Cardiovasc. Echogr. 2020, 30, S1–S5. [Google Scholar]
- Gargani, L.; Soliman-Aboumarie, H.; Volpicelli, G.; Corradi, F.; Pastore, M.C.; Cameli, M. Why, when, and how to use lung ultrasound during the COVID-19 pandemic: Enthusiasm and cautio. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Collart, P.; Dubourg, D.; Levêque, A.; Sierra, N.B.; Coppieters, Y. Short-term effects of nitrogen dioxide on hospital admissions for cardiovascular disease in Wallonia, Belgium. Int. J. Cardiol 2018, 255, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Picano, E. Air cardiology is now on air. Eur. Heart J. 2021, 42, 961–962. [Google Scholar] [CrossRef]
- D‘Andrea, A.; Ciampi, Q.; Russo, A.; Forni, A.; Mangia, C.; Picano, E. The effects of lockdown-induced air quality changes on the results of cardiac functional stress testing in coronary artery disease and heart failure patient. Environ. Sci. Pollut. Res. Int. 2021, 30, 1–8. [Google Scholar]
- Marwick, T.H.; Buonocore, J. Environmental impact of cardiac imaging tests for the diagnosis of coronary artery disease. Heart 2011, 97, 1128–1131. [Google Scholar] [CrossRef]
- Martin, M.; Mohnke, A.; Lewis, G.M.; Dunnick, N.R.; Keoleian, G.; Maturen, K.E. Environmental Impacts of Abdominal Imaging: A Pilot Investigation. J. Am. Coll. Radiol. 2018, 15, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- Cano-Aguilar, I.; Vice-President. European Economic and Social Committee. Sustainability must be at the heart of Europe’s future. Open Access Government. Available online: https://www.openaccessgovernment.org/sustainability-must-be-at-the-heart-of-europes-future/80930/ (accessed on 20 January 2020).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciampi, Q.; Antonini-Canterin, F.; Barbieri, A.; Barchitta, A.; Benedetto, F.; Cresti, A.; Miceli, S.; Monte, I.; Petrella, L.; Trocino, G.; et al. Reshaping of Italian Echocardiographic Laboratories Activities during the Second Wave of COVID-19 Pandemic and Expectations for the Post-Pandemic Era. J. Clin. Med. 2021, 10, 3466. https://doi.org/10.3390/jcm10163466
Ciampi Q, Antonini-Canterin F, Barbieri A, Barchitta A, Benedetto F, Cresti A, Miceli S, Monte I, Petrella L, Trocino G, et al. Reshaping of Italian Echocardiographic Laboratories Activities during the Second Wave of COVID-19 Pandemic and Expectations for the Post-Pandemic Era. Journal of Clinical Medicine. 2021; 10(16):3466. https://doi.org/10.3390/jcm10163466
Chicago/Turabian StyleCiampi, Quirino, Francesco Antonini-Canterin, Andrea Barbieri, Agata Barchitta, Frank Benedetto, Alberto Cresti, Sofia Miceli, Ines Monte, Licia Petrella, Giuseppe Trocino, and et al. 2021. "Reshaping of Italian Echocardiographic Laboratories Activities during the Second Wave of COVID-19 Pandemic and Expectations for the Post-Pandemic Era" Journal of Clinical Medicine 10, no. 16: 3466. https://doi.org/10.3390/jcm10163466
APA StyleCiampi, Q., Antonini-Canterin, F., Barbieri, A., Barchitta, A., Benedetto, F., Cresti, A., Miceli, S., Monte, I., Petrella, L., Trocino, G., Aquila, I., Barbati, G., Barletta, V., Barone, D., Beraldi, M., Bergandi, G., Bilardo, G., Boriani, G., Bossone, E., ... SIECoVId Study Group, on Behalf of the Italian Society of Echocardiography and Cardiovascular Imaging (SIECVI). (2021). Reshaping of Italian Echocardiographic Laboratories Activities during the Second Wave of COVID-19 Pandemic and Expectations for the Post-Pandemic Era. Journal of Clinical Medicine, 10(16), 3466. https://doi.org/10.3390/jcm10163466














